Back to Journals » Patient Preference and Adherence » Volume 17
Non‑persistence to Oral Anticoagulation Therapy in Elderly Patients with Non‑valvular Atrial Fibrillation
Authors Cao Y, Feng YY, Du W, Li J, Fei YL, Yang H, Wang M, Li SJ, Li XJ, Han B
Received 15 August 2023
Accepted for publication 25 November 2023
Published 6 December 2023 Volume 2023:17 Pages 3185—3194
DOI https://doi.org/10.2147/PPA.S435592
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Yue Cao, Yue-Yue Feng, Wei Du, Jing Li, Ya-Lan Fei, Hao Yang, Meng Wang, Shi-Jie Li, Xian-Jin Li, Bing Han
Division of Cardiology, Xuzhou Central Hospital, Xuzhou, People’s Republic of China
Correspondence: Bing Han, Division of Cardiology, Xuzhou Central Hospital, 199 South Jiefang Road, Xuzhou, 221009, People’s Republic of China, Tel +86-516-83985069, Fax +86-516-83956012, Email [email protected]
Purpose: To investigate the reasons for elderly atrial fibrillation (AF) patients not continuing their oral anticoagulation (OAC) treatment and the factors that influence this behavior.
Methods: Elderly AF patients (aged≥ 75 years) hospitalized from December 2019 to May 2022 were consecutively enrolled. Clinical, demographic, and concomitant medication data were collected. The endpoint was defined as OAC discontinuation for more than 30 days or a switch to an alternative therapy. Predictors of OAC non-persistence were investigated using a multivariable Cox regression model.
Results: This study included 560 participants (51.1% men, mean age 80.9± 0.2 years). During a median follow-up of 20 months, medication persistence was observed in 322 patients (57.5%). Non-persistence was found to be significantly higher with warfarin than with NOAC (48.8% vs 33.6%, p = 0.006). In the multivariate analysis, OAC non-persistence was independently predicted by a history of permanent pacemaker implantation, the use of antiplatelet drugs, employee Medicare, living with children, college degree or above, and persistent AF (HR = 1.580, 1.586, 0.604, 0.668, 0.028, 0.769, p < 0.05, respectively). Treatment discontinuation within 3 months of discharge was observed in a large number of patients (81.8%). Medication discontinuation due to bleeding was more frequently observed in patients who continued for longer than 3 months (p < 0.001), while discontinuation due to patient preference was more frequent in those with shorter durations (≤ 3 months) (p = 0.049). Patient preference was the second leading cause of non-persistence in patients, regardless of whether they were taking warfarin or NOAC.
Conclusion: OAC non-persistence remains high among elderly AF patients during long-term follow-up, with a significant proportion discontinuing shortly after discharge. This pattern of non-persistence is heavily influenced by demographic factors and patient preference. Further interventions should be developed based on the reasons and risk factors to improve persistence and initiated early in the treatment process.
Keywords: atrial fibrillation, the elderly, oral anticoagulants, non-persistence
A Letter to the Editor has been published for this article.
Introduction
Atrial fibrillation (AF) stands as the most prevalent cardiac arrhythmia among elderly individuals, and its frequency escalates with age, reaching a rate of up to 12% in those aged 75 years or older.1 Ischemic stroke represents the most frequent complication associated with AF, and the incidence of ischemic stroke linked to AF is closely related to age, with rates soaring as high as 23.5% in older patients with AF aged 80–89 years, in contrast to 1.5% in those aged 50–59 years.2 Consequently, the preventative use of oral anticoagulants (OACs) to avert strokes becomes imperative,3–5 particularly for elderly AF patients who are at an elevated risk of stroke.6,7
Although the CHA2DS2-VASc scoring system and guidelines recommend OAC for individuals aged 75 and above with AF, unless contraindicated,8,9 the actual treatment situation for elderly AF patients is disheartening, marked by low prescription rates and,10 even more disconcerting, low persistence rates.11,12 A national observational study in China revealed that around 30% of patients terminated anticoagulant therapy after one year,11 while in a Dutch study, 34% and 22% of AF patients discontinued the use of novel oral anticoagulants (NOACs) and vitamin K antagonists (VKAs) at one year, a proportion that surged to nearly 64% and 34% within four years.12 The non-persistence of OAC is intertwined with adverse cardiovascular consequences, translating into a 2–6-fold elevated risk of stroke/transient ischemic attack (TIA) and an approximate twofold increase in all-cause mortality.13–15 Previous studies predominantly concentrated on the factors influencing non-persistence with OAC,12,16 but few have examined the immediate reasons behind OAC discontinuation in AF patients, particularly those who are elderly.17 Given the unique characteristics of this demographic, who constitute a significant proportion and require OAC unless contraindicated, delving into the direct causes and factors influencing drug non-persistence carries substantial significance.
This prospective study offers a protracted follow-up of patients who were prescribed OAC upon discharge and endeavors to ascertain the causes for patient non-persistence. Its aim is to comprehensively identify the predictors of non-persistence in AF patients aged 75 and above, who possess indications for anticoagulation, by considering both the patient’s perspective and clinical factors.
Methods
Participants
The study comprised elderly patients aged 75 years or older with diagnosed AF confirmed by ECG or 24-hour Holter ECG who were hospitalized at the Department of Cardiology of Xuzhou Central Hospital from December 2019 to May 2022. Exclusion criteria encompassed: (1) prior radiofrequency ablation of AF or left atrial appendage occlusion, either previously or during hospitalization; (2) in-hospital mortality; (3) contraindications for anticoagulation, specifically severe liver dysfunction (transaminases > 400 u/l) and chronic kidney disease (CKD) stage 5; (4) a history of valvular disease, defined as moderate or severe mitral stenosis, mild rheumatic mitral stenosis, or valvular surgery. Ultimately, the study comprised 322 patients who persisted with their medication (persistence group) and 238 patients who discontinued (non-persistence group) (Figure 1). The research received approval from the ethics committee of Xuzhou Center Hospital (XZXY-LJ-20190222-004) and adhered to the ethical principles outlined in the 1964 Helsinki Declaration, as well as its subsequent amendments or comparable ethical standards. All study participants provided written informed consent.
 |
Figure 1 Patients’ selection flowchart. Abbreviations: AF, atrial fibrillation; NOAC, novel oral anticoagulant. |
Data Collection
Data collection included demographic details (eg, age, gender, medical insurance, educational attainment, residence, and current residential situation), clinical history data (eg, AF type, onset time of AF, history of previous pacemaker implantation, prior instances of bleeding, and previous stroke), comorbid conditions (eg, hypertension, coronary heart disease, diabetes mellitus, congestive heart failure, chronic obstructive pulmonary disease, and cancer), laboratory test results (eg, serum creatinine levels), concomitant medication (eg, antiplatelet drugs, medication to control ventricular rate, and proton pump inhibitors), stroke risk assessment (CHA2DS2-VASc score), and bleeding risk evaluation (HAS-BLED score).
Follow-Up and Endpoint Event
Patients underwent post-hospitalization follow-up conducted by a team of specialized electrophysiologists either through outpatient visits or telephone consultations at intervals of 3, 6, and 12 months, and subsequently every 6 months until December 2022. The primary endpoint event of interest was non-persistence with therapy during follow-up, which was defined as either discontinuation with a lapse of more than 30 days or a switch to an alternative treatment.16 The follow-up assessments included determining whether the patient had ceased taking the prescribed medication, the timing of discontinuation, the primary reason for non-persistence, occurrences of stroke, hemorrhage, and mortality. Patient-reported reasons for non-persistence included: (1) experiencing bleeding complications; (2) perceiving anticoagulation therapy as overly cumbersome; (3) being unable to afford the excessive cost of anticoagulation therapy; (4) patient preference toward discontinuation due to a fear of bleeding or the absence of AF-related symptoms; (5) being compelled to discontinue anticoagulant treatment due to other diseases, trauma, or surgery.
Statistical Analysis
The Kolmogorov–Smirnov test was employed to assess whether continuous variables adhered to a normal distribution. Continuous variables not conforming to normal distribution were expressed as median (Q1, Q3), and comparisons between groups were made using the Mann–Whitney U-test. Categorical variables were presented as raw counts and percentages, and group comparisons were performed using the Chi-square test or the Fisher exact probability method if the frequency was less than 5 in either of the two groups. A time-to-event analysis was used to evaluate patient persistence with OAC, and survival curves were depicted using the Kaplan-Meier method. The survival distributions of persistence between the warfarin group and the NOAC group were compared using the Log rank test. Cox multivariate proportional hazards regression analysis was conducted to identify factors associated with non-persistence. Additionally, a sensitivity analysis was performed, excluding patients who remained adherent to their medication at the time of death during follow-up, ensuring that this subgroup of patients did not unduly influence the results. Statistical analyses were carried out using SPSS statistical software version 26.0 (IBM Co., Armonk, NY, USA). All P-values were two-tailed, and significance was determined at a threshold of P < 0.05.
Results
Baseline Characteristics
In total, 560 patients were enrolled, with 328 patients demonstrating persistence with their medication and 238 patients exhibiting non-persistence at the conclusion of the follow-up period. Of these patients, 51.1% were male, and the mean age was 80.9±0.2 years. In comparison to the persistence group, the non-persistence group had higher percentages of resident or rural Medicare recipients (53.8% and 20.8%), individuals residing in rural areas (38.2% and 16.1%), those living alone or with a spouse (31.5% and 13.7%), and individuals with lower educational levels (83.6% and 40.7%), as well as higher rates of paroxysmal AF (31.5% and 16.5%), previous permanent pacemaker implantation (13.4% and 7.1%), a higher HAS-BLED score, and concurrent use of antiplatelet drugs (21.4% and 8.1%) (all P < 0.05). However, medications to control ventricular rate (50.0% and 62.4%) and proton pump inhibitors (5.5% and 13.4%) were less frequently employed (all P < 0.05). No significant differences were observed between the two groups in terms of CHA2DS2-VASc scores and other clinical indicators (all P > 0.05) (Table 1).
 |
Table 1 Baseline Characteristics of Participants in Two Groups |
Follow-Up Outcomes
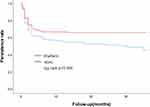
The median follow-up period spanned 20 months (ranging from 6 to 36 months). Out of the total patient cohort, 322 individuals (57.5%) remained persistent with their medication. This included 168 patients (52.2%) using warfarin and 154 patients (47.8%) taking NOAC, with a statistically higher rate of treatment persistence for NOAC compared to warfarin (P = 0.006) (Figure 2). In contrast, 238 patients (42.5%) discontinued their treatment, comprising 160 patients (67.2%) on warfarin and 78 patients (32.8%) on NOAC. Additionally, six patients initially on warfarin switched to NOAC, while ten patients originally on NOAC switched to warfarin. Forty patients opted for antiplatelet agents alone after discontinuing OAC. Throughout the follow-up period, a total of 39 patients experienced acute ischemic strokes, 86 patients had hemorrhages, and 91 patients passed away.
Predictors of OAC Non-Persistence
In the multivariate analysis, several factors were identified as independent predictors of OAC non-persistence, including a history of permanent pacemaker implantation (HR = 1.580, 95% CI 1.056–2.362, P = 0.026), the use of antiplatelet drugs (HR = 1.586, 95% CI 1.107–2.271, P = 0.012), being covered by employee Medicare (HR = 0.604, 95% CI 0.422–0.863, P = 0.006), living with children (HR = 0.668, 95% CI 0.503–0.888, P = 0.005), having a college degree or above (HR = 0.028, 95% CI 0.004–0.201, P < 0.001), and having persistent AF (HR = 0.769, 95% CI 0.664–0.891, P < 0.001) (Table 2).
 |
Table 2 Main Predictors of OAC Non-Persistence in the Elderly Patients with AF |
Reasons of Patients with Non-Persistence
The principal reasons for non-persistence, as determined through detailed patient interviews, were as follows: (1) In 72 cases,(30.3%),patients perceived anticoagulation therapy as overly cumbersome. (2) 65 cases,(27.3%) discontinued medication due to patient preference,including 27 cases who feared bleeding and 38 cases who did not experience AF-related symptoms. (3) 35 cases (14.7%) reported that they were unable to afford the excessive cost of anticoagulation therapy. (4) In 34 cases (14.3%),patients experienced bleeding complications. (5) 32 cases (13.4%) were compelled to discontinue anticoagulant treatment due to other diseases,trauma,or surgery. Figure 3 illustrates that the most common reason for discontinuation among patients using warfarin was the perception of therapy as being overly cumbersome,whereas the excessive cost was the primary reason for patients discontinuing NOAC. Patient preference was the second leading cause of non-persistence in patients,regardless of whether they were taking warfarin or NOAC.
 |
Figure 3 The reasons of patients with non-persistence in OAC, Warfarin and NOAC groups. Abbreviations: OAC, oral anticoagulant; NOAC, novel oral anticoagulant. |
The data presented in Table 3 highlights the distinctions between patients who discontinued anticoagulation for various reasons, including the duration of use and the type of anticoagulant employed. A substantial proportion of patients discontinued their treatment within 3 months following discharge, totaling 81.8%. Patients who continued for longer durations (>3 months) more frequently ceased medication due to bleeding (P < 0.001). In contrast, patients who continued for shorter durations (≤3 months) were more likely to discontinue due to patient preference (P = 0.049). Additionally, patients taking warfarin were more prone to discontinue due to the perceived cumbersomeness of the therapy (P < 0.001), while those using NOAC discontinued primarily due to the excessive costs (P < 0.001).
 |
Table 3 The Distinctions Between Patients Who Discontinued Anticoagulation for Various Reasons, Including the Duration of Use and the Type of Anticoagulant Employed |
Discussion
In this prospective study, we made the following observations. First, the rate of non-persistence among elderly AF patients with indications for anticoagulation remained notably high (40%). The majority (81%) of patients discontinued their anticoagulant treatment within a short period (≤3 months) after being discharged from the hospital. Second, our study unveiled that non-persistence was influenced by a combination of demographic factors (such as Medicare insurance, current living situation, and education level), clinical variables (including the type of AF and history of permanent pacemaker implantation), and the use of antiplatelet drugs. Third, the most common reason for non-persistence among patients taking warfarin was the medication being too complicated, while patients on NOACs cited excessive costs as the primary issue. Regardless of whether they were taking warfarin or NOACs, patient preference played a significant role in medication non-persistence, making it the primary reason for early drug discontinuation.
Our study indicated that approximately 60% of patients maintained their medication adherence at the end of the follow-up period, which was lower than the results of previous domestic studies.11,18 This disparity can be explained by differences in patient characteristics and the longer follow-up time. In this study, the rate of NOAC use was comparable to warfarin, but the rate of non-persistence was much lower (33.6% vs 48.8%).
We found that clinical factors, such as the type of AF, history of permanent pacemaker implantation, and the use of antiplatelet drugs, were independent predictors of OAC non-persistence in elderly patients with AF. These factors were associated with an increased risk of bleeding and the alleviation of clinical symptoms, contributing to OAC non-persistence. This observation was also consistent with the reasons for discontinuation among patients we interviewed, where we found that patient preference for discontinuation due to fear of bleeding or the absence of AF-related symptoms was the second leading cause of non-persistence in patients, regardless of whether they were taking warfarin or NOACs. AF and coronary artery disease (CAD) are closely related, with a reported prevalence as high as 70% in recent studies.19 Current guidelines recommend a combination of antiplatelet drugs and OAC shortly after acute coronary syndrome or PCI for patients with AF at high risk of thrombosis, whereas anticoagulants are recommended for patients with stable coronary artery disease, and antiplatelet drugs are not recommended for thrombosis prevention.9 However, our study revealed that CAD patients less commonly used OAC, mainly due to knowledge gaps and the fear of bleeding.19 Therefore, there is an urgent need to educate people and raise awareness about this significant association, as well as promote the appropriate use of antithrombotic agents. Additionally, with the global population aging, more patients will undergo permanent pacemaker implantation,20,21 and the high discontinuation of OAC in elderly patients with AF should receive considerable attention.
It’s worth noting that demographic factors also play a significant role in influencing patient medication status. Our study found that Medicare insurance, educational level, and current residence were independently associated with OAC non-persistence. An analysis of the reasons for this association revealed the following: (1) Patients with higher levels of education tended to have better knowledge about their medical condition. Madrid22 found that patients with college or higher education levels had a greater understanding of anticoagulation and were more likely to engage in frequent monitoring and dose adjustments when using warfarin. Another previous study18 also demonstrated that patients with higher education levels exhibited better adherence to anticoagulation treatment. (2) The living situation of patients also played a role. In our study, 78.7% of patients who lived with their children received better care compared to those who lived alone or with their spouses. (3) Medicare payment policies with higher reimbursement proportions influenced patient behavior. In our study, 85.8% of patients who used NOACs were insured through employee Medicare, and a higher reimbursement proportion was associated with reduced rates of patient non-persistence.
In a Japanese study,23 drug adverse events were the most common reason for medication discontinuation. However, in our study, we found that patients themselves were the primary contributors to discontinuation. Instances of needing to discontinue due to factors like bleeding or surgery were rare (27.7%), whereas 72.3% of patients discontinued due to personal reasons, especially the fear of bleeding and the absence of AF-related symptoms, accounting for up to 27.3%, similar to the findings of Wu,17 who confirmed that patient preference was the most common reason for discontinuation. Therefore, mitigating factors related to individual preferences is pivotal in enhancing medication adherence.
We also explored the relationship between the reasons for non-persistence in patients and the type of anticoagulant used. Warfarin had a high discontinuation rate due to the frequent monitoring of coagulation.24,25 However, one study confirmed that the effective time spent within the therapeutic range (TTR>60%) is comparable to the efficacy of NOACs in patients with AF.26 On the other hand, the most common reason for non-persistence with NOACs was the users unable to afford the excessive cost of anticoagulation therapy. This may be related to the incomplete coverage of Medicare in China and the low proportion of reimbursement.
Furthermore, we delved deeper into the relationship between the reasons for non-persistence and the time of discontinuation in patients. Our study revealed that the non-persistence rate was notably high during the initial phase of OAC medication, followed by a lower rate of discontinuation as time progressed. This trend aligns with the findings of Beyer,27 who reported that approximately 40% of patients prescribed OAC discontinued at 6 months, and 50% at 1 year. What stood out in our study was that a significant majority of patients discontinued within 3 months of hospital discharge, with most of them attributing their discontinuation to personal reasons, mainly the fear of bleeding or the absence of AF-related symptoms, particularly when compared to those discontinuing after 3 months. Relevant research has demonstrated that effective publicity and education about anticoagulant therapy can increase adherence and enhance clinical outcomes.28,29 Our study suggests that such efforts may be particularly impactful, especially during the early stages of anticoagulation therapy in elderly patients with AF.
However, there are certain limitations to our study. Firstly, it is a single-center study. Although we enrolled patients from four provinces, being one of the largest hospitals in northern China, our findings may not be fully representative of the entire Chinese population. Secondly, in our multivariate Cox regression analysis, we examined the factors influencing OAC non-persistence as a whole, rather than separately exploring the factors affecting NOAC and warfarin discontinuation due to the small sample size. This may have influenced the results.
Conclusions
In conclusion, the rate of non-persistence with OAC remains notably high among elderly AF patients over long-term follow-up, with a significant proportion discontinuing shortly after hospital discharge. This non-persistence pattern is strongly influenced by demographic factors and patient preference. It is crucial to develop interventions based on the identified reasons and risk factors to enhance persistence, especially during the early phases of treatment.
Data Sharing Statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Funding
This study received the support of the National Natural Science Foundation of China (grant number: 82370329); and the Jiangsu Research Project of Cadre Health Care (grant number: BJ19007); and the Xuzhou Medical leading Talents Project (grant number: XWRCHT20210032).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fitzmaurice DA, Hobbs FD, Jowett S, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ. 2007;335(7616):383. doi:10.1136/bmj.39280.660567.55
2. Wang TJ, Massaro JM, Levy D, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290(8):1049–1056. doi:10.1001/jama.290.8.1049
3. Andersen LV, Vestergaard P, Deichgraeber P, et al. Warfarin for the prevention of systemic embolism in patients with non-valvular atrial fibrillation: a meta-analysis. Heart. 2008;94(12):1607–1613. doi:10.1136/hrt.2007.135657
4. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–962. doi:10.1016/S0140-6736(13)62343-0
5. Hirschl M, Kundi M. Safety and efficacy of direct acting oral anticoagulants and vitamin K antagonists in nonvalvular atrial fibrillation - a network meta-analysis of real-world data. Vasa. 2019;48(2):134–147. doi:10.1024/0301-1526/a000746
6. Krittayaphong R, Boonyapiphat T, Wongvipaporn C, Sairat P; COOL-AF Investigators. Age-related clinical outcomes of patients with non-valvular atrial fibrillation: insights from the COOL-AF Registry. Clin Interv Aging. 2021;16:707–719. doi:10.2147/CIA.S302389
7. Wehling M, Collins R, Gil VM, et al. Appropriateness of oral anticoagulants for the long-term treatment of atrial fibrillation in older people: results of an Evidence-Based Review and International Consensus Validation Process (OAC-FORTA 2016). Drugs Aging. 2017;34(7):499–507. doi:10.1007/s40266-017-0466-6
8. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
9. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2020;42:ehaa612.
10. Hsu JC, Maddox TM, Kennedy K, et al. Aspirin instead of oral anticoagulant prescription in atrial fibrillation patients at risk for stroke. J Am Coll Cardiol. 2016;67(25):2913–2923. doi:10.1016/j.jacc.2016.03.581
11. Guo Y, Wang H, Kotalczyk A, Wang Y, Lip GYH; ChiOTEAF Registry Investigators. One-year follow-up results of the optimal thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. J Arrhythm. 2021;37(5):1227–1239. doi:10.1002/joa3.12608
12. Zielinski GD, van Rein N, Teichert M, et al. Persistence of oral anticoagulant treatment for atrial fibrillation in the Netherlands: a surveillance study. Res Pract Thromb Haemost. 2019;4(1):141–153. doi:10.1002/rth2.12261
13. Dhamane AD, Hernandez I, Di Fusco M, et al. Non-persistence to oral anticoagulation treatment in patients with non-valvular atrial fibrillation in the USA. Am J Cardiovasc Drugs. 2022;22(3):333–343. doi:10.1007/s40256-021-00501-w
14. Sherwood MW, Douketis JD, Patel MR, et al. Outcomes of temporary interruption of rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: results from the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF). Circulation. 2014;129(18):1850–1859. doi:10.1161/CIRCULATIONAHA.113.005754
15. García Rodríguez LA, Cea Soriano L, Munk Hald S, et al. Discontinuation of oral anticoagulation in atrial fibrillation and risk of ischaemic stroke. Heart. 2020;107(7):542–548. doi:10.1136/heartjnl-2020-317887
16. Kozieł M, Mazurek M, Teutsch C, et al. Persistence with anticoagulation for atrial fibrillation: report from the GLORIA-AF Phase III 1-year follow-up. J Clin Med. 2020;9(6):1969. doi:10.3390/jcm9061969
17. Wu S, Xie S, Xu Y, et al. Persistence and outcomes of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with non-valvular atrial fibrillation. J Clin Nurs. 2019;28(9–10):1839–1846. doi:10.1111/jocn.14797
18. Liu C, Du X, Jiang C, et al. Long-term persistence with newly-initiated warfarin or Non-VKA Oral Anticoagulant (NOAC) in patients with non-valvular atrial fibrillation: insights from the prospective China-AF Registry. Med Sci Monit. 2019;25:2649–2657. doi:10.12659/MSM.915875
19. Batta A, Hatwal J, Batta A, Verma S, Sharma YP. Atrial fibrillation and coronary artery disease: an integrative review focusing on therapeutic implications of this relationship. World J Cardiol. 2023;15(5):229–243. doi:10.4330/wjc.v15.i5.229
20. Kowalewski M, Pasierski M, Finke J, et al. Permanent pacemaker implantation after valve and arrhythmia surgery in patients with preoperative atrial fibrillation. Heart Rhythm. 2022;19(9):1442–1449. doi:10.1016/j.hrthm.2022.04.007
21. Greenspon AJ, Patel JD, Lau E, et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. J Am Coll Cardiol. 2012;60(16):1540–1545. doi:10.1016/j.jacc.2012.07.017
22. Hernández Madrid A, Potpara TS, Dagres N, et al. Differences in attitude, education, and knowledge about oral anticoagulation therapy among patients with atrial fibrillation in Europe: result of a self-assessment patient survey conducted by the European Heart Rhythm Association. Europace. 2016;18(3):463–467. doi:10.1093/europace/euv448
23. Shiga T, Naganuma M, Nagao T, et al. Persistence of non-vitamin K antagonist oral anticoagulant use in Japanese patients with atrial fibrillation: a single-center observational study. J Arrhythm. 2015;31(6):339–344. doi:10.1016/j.joa.2015.04.004
24. Wang ZZ, Du X, Wang W, et al. Long-term persistence of newly initiated warfarin therapy in Chinese Patients With Nonvalvular Atrial Fibrillation. Circ Cardiovasc Qual Outcomes. 2016;9(4):380–387. doi:10.1161/CIRCOUTCOMES.115.002337
25. Gallagher AM, Rietbrock S, Plumb J, et al. Initiation and persistence of warfarin or aspirin in patients with chronic atrial fibrillation in general practice: do the appropriate patients receive stroke prophylaxis? J Thromb Haemost. 2008;6(9):1500–1506. doi:10.1111/j.1538-7836.2008.03059.x
26. Aktan A, Güzel T, Aslan B, et al. Comparison of the real-life clinical outcomes of warfarin with effective time in therapeutic range and non-vitamin K antagonist oral anticoagulants: insight from the AFTER-2 trial. Kardiol Pol. 2023;81(2):132–140. doi:10.33963/KP.a2022.0287
27. Beyer-Westendorf J, Ehlken B, Evers T. Real-world persistence and adherence to oral anticoagulation for stroke risk reduction in patients with atrial fibrillation. Europace. 2016;18(8):1150–1157. doi:10.1093/europace/euv421
28. Márquez-Contreras E, Martell-Claros N, Márquez-Rivero S, et al. Strategies for improving dabigatran adherence for stroke prevention in patients with non-valvular atrial fibrillation: education and drug intake reminders (FACILITA study). Curr Med Res Opin. 2018;34(7):1301–1308. doi:10.1080/03007995.2018.1435519
29. Clarkesmith DE, Pattison HM, Lip GY, et al. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013;8(9):e74037. doi:10.1371/journal.pone.0074037
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.