Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Nodular Elastoidosis with Cysts and Acne: A Case Report
Received 21 July 2023
Accepted for publication 3 September 2023
Published 8 September 2023 Volume 2023:16 Pages 2453—2456
DOI https://doi.org/10.2147/CCID.S426880
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Shicheng Jiao,1,* Mu Niu,2,* Jie Yang2
1Jiao Shicheng Medical Beauty Clinic, Haikou, Hainan, People’s Republic of China; 2Department of Dermatology, The Fifth People’s Hospital of Hainan Province, Haikou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jie Yang, Department of Dermatology, The Fifth People’s Hospital of Hainan Province, Haikou, People’s Republic of China, Email [email protected]
Abstract: A 53-year-old male presented to the clinic for “bilateral temporal dark yellow plaques with pruritus for 8 years.” The patient had bilateral temporal dark yellow plaques without obvious inducement 8 years ago and did not see doctors at that time. Five years ago, bilateral temporal skin lesions gradually increased and were accompanied by severe itching. On top of them, there were several blackheads and pimples with the size of needle tips up to the size of rice grains. After compression, lipid substances could be excreted and there was a clear odor. The patient sought medical attention at a local hospital, but the diagnosis and medication were unknown, and the symptoms did not improve. In the past month, due to the aggravation of skin lesions and itching that affected sleep, he visited the outpatient clinic of our hospital again. The patient was diagnosed with nodular elastoidosis with cysts and acne and was given 5% peroxybenzoyl gel and 0.1% tretinoin cream for topical use. After 2 weeks, the itching symptoms of the patient were significantly reduced.
Keywords: nodular elastoidosis, cysts, acne
Case Introduction
The patient denied a history of chronic diseases such as hypertension and diabetes, denied a history of infectious diseases such as tuberculosis and malaria, and denied a history of major trauma, surgery, and blood transfusion. He also denied any medication or food allergy. There were no patients with similar diseases in the family. His vaccination history was consistent with local. The patient was married with children. The patient was a local fisherman in Hainan province, a long-term smoker, 1 pack/day.
Dermatological examination concluded that the patient had diffuse thickening of facial skin, thickening of skin lines and furrow deepening. Clustered dark yellow plaques can be seen on both sides of the temporal region, with dozens of blackheads and cysts in rice to soybean size scattered on the plaques. After some cysts are compressed, white lipid substances can be seen to be excreted (Figure 1A–1C).
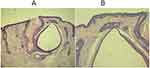
Laboratory and auxiliary examinations showed that routine blood, urine, and feces tests, as well as liver and kidney function tests, were normal. The thickened part of the left-cheek skin was taken for a histopathological examination of the skin lesions, which showed that the epidermis became thinner, the collagen fibers in the superficial layer of the dermis became basophilic with the formation of cysts, and the pilosebaceous orifice expanded in a cystic manner, containing keratin plugs, extending to the deep layer of the dermis. The superficial layers of the dermis have scattered lymphocytic infiltrates (Figure 2A and B). Skin ultrasound examination showed that multiple mixed-echo structures can be seen in the subcutaneous soft tissue, with raised skin surface, regular shape, circular shape, and uneven internal echoes. Strong echo structures can be seen in the rear, and some openings can be seen on the epidermis. CDFI: Small blood flow signal is visible (Figure 3A and B).
The doctor diagnosed the patient with nodular elastoidosis with cysts and acne. The doctor asked the patient to avoid sun exposure and take sun protection measures during daytime work. There was no specific treatment for this disease. 5% peroxybenzoyl gel was used to apply skin lesions during the day and 0.1% tretinoin cream was applied at night. Because both drugs had certain irritation, the patient’s medication was supervised by a specialist dermatology nurse. After 2 weeks, the patient complaint of pruritus was significantly reduced, and some skin lesions were significantly smaller than before. A month later, the patient returned to the hospital, and he was advised to remove the larger epidermal cyst through surgery, but the patient refused.
Discussion
Nodular elastosis is also known as Favre Racouchot disease (FRD), senile acne, solar acne, and so on, easily happening to people with lighter skin color.1 The cause of the disease is still unclear, and patients with this disease often have excessive smoking, prolonged sun exposure, ionizing radiation, harsh environment, and other related factors.2,3 With the high incidence among fishermen, farmers, drivers, and the low incidence in women, the disease may be related to its occupational characteristics.4 It usually occurs in the temporal, periorbital, neck, back of the hand and other exposure areas, with clinical manifestations of blackhead, cyst and elastic fiber nodules as the main features.5 Typical clinical characteristics are crucial to the diagnosis of the disease. Histopathology contributes to the diagnosis of the disease, such as enlargement of pilosebaceous orifice, keratin filling, formation of follicular cyst and basophilic of superficial dermis collagen fibers.6 This disease can also exist at the same time with other degenerative diseases. As patients do not pay enough attention, the disease continues to progress. In addition, secondary infection or degeneration after long-term extrusion stimulation also causes misdiagnosis or missed diagnosis, which may also be the reason for the few reports in China. For treatment, sun protection is the most basic measure. Outdoor work should take strict sun protection measures. Skin lesion treatment is similar to acne treatment, topical or oral tretinoin cream is recognized as an effective treatment.7 For large skin lesions, resection, grinding and CO2 laser can be used. In this case, the patient was a local fisherman in Hainan, who had been working at sea for a long time and had a history of smoking, which may be the cause of the disease. Tretinoin cream was applied, and the patient’s symptoms were significantly improved. For large skin lesions, surgical resection was planned, but the patient refused and is still in follow-up.
Conclusion
In summary, the clinical manifestations of this patient were mainly blackhead and cyst, and the treatment was similar to acne. However, due to the older age of the patient, the pursuit of facial beauty is low, and refuse further treatment, so the external drug treatment is the main method, and the effect is remarkable. Due to the nature of the patient’s work, there are many factors that can cause the disease, and the cause of the patient cannot be clarified. Subsequently, we can continue to collect relevant cases and explore the risk factors of the disease.
Ethical Statement
We have already got approval from the Ethics Committee of The Fifth People’s Hospital of Hainan Province. It is okay to publish the case details without his name being published.
Informed Consent
A written informed consent form was obtained from the patient. In the form, the patient agreed that his case details can be used by our doctors or hospital in the professional field without his name being published, namely he gave consent for the publication of his case details as well as any accompanying images.
Acknowledgment
Shicheng Jiao and Mu Niu should be considered as co-first authors.
Funding
This work was supported by Hainan Province Clinical Medical Center.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Friedman SJ, Su WP. Favre-Racouchot syndrome associated with radiation therapy. Cutis. 1983;31:306–310.
2. Sutherland AE, Green PJ. Favre-Racouchot syndrome in a 39-year old female following radiation therapy. J Cutan Med Surg. 2014;18(1):72–74. doi:10.2310/7750.2013.13011
3. Vogel S, Muhlstadt M, Molin S, Ruzicka T, Schneider J, Herzinger T. Unilateral favre-racouchot disease: evidence for the etiological role of chronic solar damage. Dermatology. 2013;226:32–34.
4. Leeuwis-Fedorovich NE, Starink M, van der Wal AC. Multifocal squamous cell carcinoma arising in a favre-racouchot lesion - report of two cases and review of the literature. J Dermatol Case Rep. 2015;9:103–106.
5. Patterson WM, Fox MD, Schwartz RA. Favre-Racouchot disease. Int J Dermatol. 2004;43:167–169.
6. Platsidaki E, Markantoni V, Balamoti E, Kouris A, Rigopoulos D, Kontochristopoulos G. Combination of 30% salicylic acid peels and mechanical comedo extraction for the treatment of favre-racouchot syndrome. Acta Dermatovenerol Croat. 2019;27:42–43.
7. Paganelli A, Mandel VD, Kaleci S, Pellacani G, Rossi E. Favre-Racouchot disease: systematic review and possible therapeutic strategies. J Eur Acad Dermatol Venereol. 2019;33:32–41. doi:10.1111/jdv.15184
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.