Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
No-Shave Long Hair Follicular Unit Excision Using an All-Purpose Skin-Responsive Device
Authors Umar S , Khanna R, Gonzalez A , Chouhan K, Maldonado JC , Oguzoglu OT, Nusbaum A
Received 24 October 2023
Accepted for publication 17 December 2023
Published 21 December 2023 Volume 2023:16 Pages 3681—3691
DOI https://doi.org/10.2147/CCID.S442822
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Video abstract presented by Umar.
Views: 374
Sanusi Umar,1– 3 Raveena Khanna,3,4 Alejandro Gonzalez,5 Kavish Chouhan,6 Juan Carlos Maldonado,7 Osman Tayfun Oguzoglu,8 Aron Nusbaum9
1Department of Medicine, Dermatology Division, University of California, Los Angeles, CA, USA; 2Division of Dermatology, Harbor-UCLA Medical Center, Torrance, CA, USA; 3Dr. U Hair and Skin Clinic, Manhattan Beach, CA, USA; 4Department of Dermatology, Howard University College of Medicine, Washington, DC, USA; 5Mxcapilar Clinic, Chulavista, Sonora, Mexico; 6Department of Dermatology, DermaClinix, New Delhi, India; 7Hair Evolution Robotics, Medellin, Colombia; 8Dr. T Hair Transplant, Istanbul, Turkey; 9Hair Transplant Institute, Miami, Coral Gables, FL, USA
Correspondence: Sanusi Umar, Dr. U Hair and Skin Clinic, 2121 N Sepulveda Blvd, Suite 200, Manhattan Beach, CA, 90266, USA, Tel +1-310-480-0490, Fax +1-310-318-1590, Email [email protected]
Background: Current no-shave long hair-follicular unit excision (LH-FUE) techniques employ recesses (slots, notches, or grooves) in punch tips to reduce the long-hair shaft break rate (SBR) and graft transection rate (GTR). However, these methods demand advanced skills and extended procedure time.
Objective: We aimed to evaluate a skin-responsive FUE technique without the use of recess-tipped punches, accommodating diverse hair and skin types in LH-FUE procedures.
Methods and Materials: We retrospectively analyzed patients who underwent this technique using a UGraft Zeus device at five multinational clinics (Mexico, Colombia, India, United States, and Türkiye) from August 9, 2021, to April 11, 2023. Donor zones were pre-operatively graded for expected difficulty using the Sanusi FUE Scoring (SFS) Scale, ranging from class I (low difficulty) to V (high difficulty).
Results: Among 152 patients (mean age, 46 years; 146 straight-wavy, 6 curly-coiled hair), most (n=107) were class I donors. The GTR ranged 2.2%– 4.3%, and was highest in class IV donors and those with thick-firm scalps. The SBR was 12.2%, and the average graft excision rate (GER; speed) was 440 grafts/h. Only 19G and 18G punches were used. All patients were satisfied with the procedure, with 57.4% reporting that they were “very happy”. Surgeon willingness to perform no-shave LH-FUE significantly increased from 1.25 to 4.20 (on a scale of 1– 5) after adopting this device. SFS class, skin thickness, and firmness, more than hair curliness, influenced the GTR, SBR, torque, and punch movement duration.
Conclusion: Our findings reveal consistent success in conducting no-shave LH-FUE using this skin-responsive device across diverse patients. Notably, success was achieved without recess-tipped punches, resulting in low GTR and SBR, along with a high GER and increased patient satisfaction. These outcomes suggest enhanced procedure speed and ease of use, contributing to a greater willingness among surgeons to adopt this technique.
Plain Language Summary: Despite the increasing popularity of no-shave long-hair follicular unit excision (FUE) as a hair transplant technique for its advantages in preserving the donor area and immediately assessing results after implanting long hairs, its adoption by surgeons has been slow due to its demanding nature. It is time-consuming and skill-intensive because it requires specialized punches with recesses (slots, notches, or grooves) on their tips that must align to accommodate and protect the long hair shafts from breakage during each extraction.
Our study reports a novel skin-responsive FUE device for performing nonshaven long-hair FUE called the UGraft Zeus, whose recess-free punch (The intelligent Punch) features a minimal-assist-navigation capability to simplify the procedure and enhances performance parameters, including speed, graft transection rate, hair shaft break rate, and its easy adoption rate by surgeons, including novices. Additionally, patient satisfaction is high.
Additionally, skin characteristics, specifically thickness and firmness, play a more critical role than the degree of hair curliness. Thicker and firmer skin requires increased torque and a longer punch movement duration during surgery. Furthermore, the skin-responsive FUE device was successful in performing no-shave long hair FUE in patients with Afro-textured hair, a population typically considered to be a hair transplant challenge.
Keywords: follicular unit extraction, nonshaven FUE, unshaven FUE, long-hair FUE, hair transplantation, hair restoration surgery
Introduction
No-shave long-hair follicular unit excision (LH-FUE) is an FUE hair transplant technique in which hair grafts are harvested from the donor area without the need to shave or trim the hair. This method aims to retrieve intact grafts while preserving the natural hair shaft length.1–5 The procedure’s growing popularity stems from its advantages, notably the immediate visualization of expected transplant results and the ability to precisely determine the optimal angle for graft placement. An end-result preview is especially beneficial when transplanting areas such as the hairline, eyebrows, eyelashes, and beard. Implanting long-hair shafted grafts also allows the camouflaging of recipient and donor areas, limiting signs of surgical intervention for patients desiring fast reintegration into social and professional activities.1–5 The procedure aims to directly harvest intact hair follicles by FUE at their natural length while keeping hair shafts from wrapping around the device’s punch tip or being cut. Despite these benefits and increasing popularity, no-shave LH-FUE is unpopular with hair surgeons because it is time-consuming and technically challenging, with one study reporting a harvesting rate of 157 grafts/h by an expert practitioner.5 A major cause of inefficiency with published no-shave LH-FUE techniques is the use of recesses (open slots, notches, or grooves; see Figure 1A–C) on the cutting end of their punches.1–5 With these devices, the long hair shaft of the follicle slides into a recess to avoid being cut.1–5 This requires a reorientation to the punch recesses to capture the target graft’s follicular shaft, in an effort to minimize the risk of breaking the shaft. Thus, the process is technically challenging, requiring meticulous eye-hand synchronization, and is time-consuming,1–5 resulting in a higher patient cost and decreased appeal to FUE surgeons. Here, we report an all-purpose skin-responsive FUE technique designed to improve the efficiency of no-shave LH-FUE using a recess-free punch (Figure 1D). Further, we report the influence of skin and hair type on no-shave LH-FUE.
Materials and Methods
All patients provided written informed consent for surgery; where applicable, consent to publish photographs was obtained. All procedures were conducted following the Declaration of Helsinki (as revised in 2013). An institutional review board exemption was obtained from the Western Institutional Review Board (IRB) Copernicus Group.
Deidentified patient data were retrospectively obtained from five independent hair restoration clinics that performed no-shave LH-FUE procedures in the United States, Mexico, India, Colombia, and Turkiye. All five treating physicians had ≥5 years of experience performing FUE on shaved donors and approximately 6 months of LH-FUE experience, with one practitioner having >2 years of experience. Data from the lead author, who developed the technology and donor scoring method, was excluded from the analysis to minimize bias. All patients underwent scalp-hair-only FUE of 100 grafts or more between August 9, 2021, and April 11, 2023, using an all-purpose skin-responsive FUE device (SRFD) called UGraft Zeus (Dr. U Devices Inc., Manhattan Beach, CA, USA)6 (Figure 2). The all-purpose designation was derived from its capability across all FUE scenarios using the same punch and punch driver.6
Preoperative Assessment of FUE Donor
Donor area assessment for expected procedural difficulty level was conducted according to the Sanusi FUE Scoring (SFS) scale, with the class (I–V) of the scalp donor zone based on a combination of skin and hair characteristics.7,8 The highest class (V) denoted the thickest, firmest skin in combination with the curliest hair type, predicting the highest difficulty and a high-to-very-high graft attrition rate.7,8
SRFD Device
The device (Figure 1) consists of a punch and punch driver, both of which have been previously described.6,8
SRFD Punch
The device has three punch sizes: 20 gauge (G), 19G, and 18G, based on the universal sizing of hypodermic needles. The SRFD punch (Figures 1D, 2, 3A and B) (Intelligent Punch®, Dr. U Devices Inc.) is a proprietarily flared, textured, and volumized punch.6,8 The circumferences of the cutting tips and edges of the punch are smooth and recess-free. Flaring of the tip presents a blunt surface toward the graft and a sharp cutting edge facing away from the graft, thereby minimizing transection. Punch texturing drives the long hair shaft into the punch lumen in a corkscrew manner, which prevents long hair from bunching and being cut (Figure 2B).6 Additionally, a see-saw oscillatory movement rolls the hair shaft over the blunt cutting edge of the punch instead of cutting it (Figure 3B).
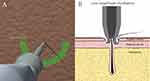 |
Figure 3 Drawing of the preferred semicircular zone; hair should be approached at any point of the circumference of the cutting edge of the punch of the skin-responsive FUE device (A). Drawing of the hair shaft contacting the semi-blunt cutting edge of the punch of the skin-responsive FUE device, which glides over it rather than cutting it. The pulling action of the punch design aids the gliding. Deep to the dermis, the shaft glides against the cutting edge of the punch, with the subcutaneous fat layer providing a soft board, reducing the risk of cutting. Copyright ©2021. Dove Medical Press. Adapted from Umar S, Lohlun B, Ogozuglu T, Carter MJ. A novel follicular unit excision device for all-purpose hair graft harvesting. Clin Cosmet Investig Dermatol. 2021;14:1657–16746 (B). Abbreviation: FUE, follicular unit excision. |
SRFD Punch Driver
The SRFD dashboard is adjustable to skin thickness or firmness with a preset for LH-FUE (Figure 1), calibrated to a set of torque settings (UForce on the dashboard) and three compound movement settings (all oscillatory) of adjustable durations (250–1000 ms/score) that are optimal for no-shave LH-FUE.6,8
Torque
The torque setting reflects the rotational force of the punch, which directly influences its skin-penetrating power. It is denoted as UForce on the dashboard (range, 1–15) and is adjustable according to skin thickness and firmness to determine the required settings for optimal skin penetration and graft release.6,8
Compound Movement
The default preset for LH-FUE comprised three-phase oscillatory movements of varying durations. The operator can adjust the duration (up or down) to influence the amount of time given to the punch to complete a scoring action, with longer durations resulting in a deeper skin-penetration effect.
Method of Use
Preoperatively, a local anesthetic (lidocaine 2% and epinephrine 1:1,000,000) was injected into scalp donor areas without causing tumescent turgor. The recommended method is to engulf the hair exit point with the punch tip pressed onto the hair shaft at any point on the circumference of the punch tip. However, for optimum performance, the punch should approach the hair follicle from any direction along a semicircular line drawn from the 3- to the 6- and 9-o’clock positions relative to the hair’s long axis (Figure 3A, Supplemental Video 1 demonstrates the preferred points of the punch-hair approach). The surgeon then holds the handpiece 45–90 degrees to the skin along the long axis of the exiting hair and lets the scoring continue under the weight of the equipment with minimal control (Supplemental Video 2 demonstrates the method of use for the SRFD in no-shave LH-FUE). Because of its minimal assist navigational (MAN) ability, the punch self-navigates the course of the hair deep into the skin, correcting punch hair misalignments within 40–60 degrees without transecting it.6,8 Thus, the surgeon does not need to guess the hair exit angle and align it exactly with the punch (Supplemental Video 2). This procedure results in long-shafted grafts and well-camouflaged donor areas (Figure 4).
Implantation was performed using conventional methods with either forceps or implanters. If previewing results was not a goal, some surgeons cut hair shafts to simplify the graft insertion process. Postoperative care was provided using previously described methods.1–3
Outcome Measures
Outcome measures included the horizontal graft transection rate (GTR); shaft breakage rate (SBR), defined as the percentage of long hair shafts broken during no-shave LH-FUE among the untransected grafts; graft excision rate (GER), which was the time taken to score and pull out grafts expressed as the number of grafts excised per hour; and patient and surgeon feedback.
Surgeons were asked to rate patient feedback starting 6 months postoperatively as “Very Happy”, “Satisfactory”, or ”Unhappy”. Surgeons were asked to compare their willingness to perform no-shave LH-FUE before and after using the SRFD, scored on a scale of 1–5 (1=not at all willing; 2, somewhat unwilling; 3, neutral; 4, somewhat willing; and 5=very willing).
Statistical Methods
We conducted univariate analyses to determine significant differences in the mean values for SRFD settings, maximum GTR, and SBR across FUE classes, sex, and skin and hair types. For non-normally distributed variables, the results of t-tests and analyses of variance were confirmed and reported using nonparametric tests. Spearman correlation coefficients were determined to evaluate significant differences in settings and outcomes across age groups. P values of <0.05 denoted statistical significance.
Results
Patient Characteristics
Overall, 152 patients (107 men; 45 women), with a mean age of 46 years (range, 25–71 years) underwent no-shave LH-FUE procedures, including 146 with straight-wavy hair and 6 African-descended Black patients with curly-coiled hair. Demographic characteristics and results of preoperative FUE donor area assessments are summarized in Table 1. Eighty-eight patients underwent hairline correction surgery: 31 received eyebrow hair transplantation, 24 underwent long hair transplantation to either the frontal or vertex scalp, and 9 received beard hair restoration. The five surgeons harvested 128,057 grafts, with a mean (SD) of 842 (691.5) grafts and GER of 440 (192.1) grafts/h.
 |
Table 1 Demographics and Preoperative Findings |
SRFD Settings
Table 2 summarizes the settings used in this study.
 |
Table 2 Procedural Data Stratified by FUE Class (Sanusi FUE Score Scale),8 Donor Site Location, and Skin Type |
Torque (UForce) Effect
The mean required torque settings were significantly lower in FUE class I patients than in class III (p=0.017) and IV (p<0.001) patients. Patients with medium-thickness firm skin required a significantly greater UForce than those with soft (p=0.008) or hard (p<0.001) skin. However, the level of torque required was not significantly affected by hair type, age, or sex.
Compound Movement Effect
Movement duration differed significantly among classes, skin types, and ages. The movement duration was significantly shorter in class I patients than in class IV patients (p<0.001) and was significantly longer with thick-firm skin than with medium-thick-firm skin (p<0.001) and with curled hair than with straight hair (p=0.001). As age increased, the mean movement duration decreased (r=−0.25, p=0.005).
GTR and Influencing Factors
The overall mean GTR range was 2.2%–4.3%, with significantly higher GTRs in FUE class IV (p<0.001) and III (p=0.04) patients than in class I patients. This correlated well with our finding of significantly greater GTRs with thick-firm skin than medium-firm skin (p<0.001). There was no significant difference in GTRs between curly-coiled-haired (n=14) and straight-wavy-haired patients (n=135). A few patients with coiled hair (n=3) registered a mean GTR of 4, well within the general GTR range. No significant correlation was observed between GTR and age or sex.
SBR and Influencing Factors
The overall mean SBR was 12%, indicating that long-hair-shafted grafts were retrieved 88% of the time. SBRs were greater with thick-firm skin than with medium-thick-firm skin (p=0.018). There was no significant difference in SBRs across classes, hair types, sexes, or ages.
Punch Size
All patients in this study required 19G and 18G punch sizes or their combination, with 18G (65%) used twice as frequently as 19G (33%). The distribution of punch size usage is summarized in Table 3. An 18G punch resulted in a significantly higher GER (578/h vs 439, p=0.02) and higher GTR (3.8% vs 5.1%, p=0.003) than a 19G punch. Punch size did not influence the SBR.
 |
Table 3 Procedural Data According to Surgeon |
Black African-Descended Patients
Six patients (mean age, 30.3 years, range 28–35 years) were African-descended Black males with Afro-textured (curly-coiled) hair. Among these, 4 were SFS class I donors, while the remaining two were class IV donors. All six patients had a maximum mean (SD) GTR of 2 (0)% and SBR of 5.7 (3.6)% using an 18G punch. Mean (SD) SRFD settings comprised an UForce of 10 (1.10) and total movement duration of 1733 (51.6) milliseconds. Notably, a preview of the results for Afro-textured hair was not possible in the immediate postoperative period, as the hair shafts laid flat, stuck to the scalp (Figure 5A and B), but became noticeable a few days after the hair was dry and unstruck from the scalp (Figure 5C).
Patient Feedback
Of 152 patients, 129 were evaluated by surgeons at a minimum of 6 months of follow up. Seventy-four (57.4%) and 55 (42.6%) patients reported being “Very happy” and “Satisfactory”, respectively, while no patient reported being “Unhappy” (Figures 6–9).
 |
Figure 6 A 36-year-old Caucasian man before long-hair FUE using a skin-responsive FUE device (A). Forty-eight hours after the implantation of 3289 long-shafted grafts to the frontal scalp. Copyright ©2021. Dove Medical Press. Adapted from Umar S, Lohlun B, Ogozuglu T, Carter MJ. A novel follicular unit excision device for all-purpose hair graft harvesting. Clin Cosmet Investig Dermatol. 2021;14:1657–16746 (B). Three years after surgery (C). Abbreviation: FUE, follicular unit excision. |
Surgeon Performance and Feedback
Table 3 summarizes the procedural data of the five surgeons. There was a significant difference in the mean number of grafts harvested between surgeons (p<0.001). Although there were significant differences between surgeons in the GTR (p<0.001), SBR (p=0.003), and GER (p<0.001), the mean GTR, SBR, and GER of all surgeons were individually within the reported performance range of the overall group. Of the five surgeons, only one had prior experience in performing no-shave LH-FUE. The mean value of willingness to perform no-shave LH-FUE changed from 1.25 to 4.20 after adopting the SRFD.
Discussion
We report a new skin-responsive FUE technique for performing no-shave LH-FUE using a recess-free punch across a diversity of patients, with notable improvements in the GTR, SBR, GER, ease of use, and surgeon adoption rates. Our 4.6% GTR compares favorably with that for recess-tipped-punch-based techniques, with previously reported higher mean GTRs of 5.6%5 and 9.2%.1 Furthermore, the long-hair harvesting speed of 440 grafts/h with our SRFD reflects a significant improvement over that in a previous study of the use of a recess-tipped punch-based unshaven LH-FUE device by an expert user (157 grafts/h).5 Two key factors contribute to the speed advantage of our SRFD over previously reported devices. First, our SRFD eliminates the technically challenging and time-consuming process of repositioning recess-tipped punches used in previous devices to capture and protect hair shafts in LH-FUE.1–4,5 Second, when long hair is pathed in preparation for unshaven LH-FUE harvesting, the visual clues of the exit angle typically used in shaved-FUE to gauge the orientation of the graft axis and subcutaneous angulation, which guides the surgeon in optimally aligning their punch, is lost. The ability of the all-purpose SRFD punch to navigate the course of the hair via its MAN6,8 is beneficial in this situation, because the operator only needs to align the punch at any point between 20 and 40 degrees of the hair shaft axis (Supplemental Video 2).6,8 The noted speed advantage of the SRFD is significant, considering that most of our surgeons had <6 months of experience in performing no-shave LH-FUE, with all but one performing no-shave LH-FUE for the first time only after acquiring the SRFD. Furthermore, the MAN effect and previously published design benefits6,8 of the SRFD may explain the success of no-shave LH-FUE in Black patients of African descent, which has not been previously reported, despite a small cohort (n=6).
In no-shave LH-FUE, the objectives of camouflaging the signs of surgery in the recipient and previewing its final result are best achieved by implanting a greater number of long-shafted grafts, which would be aided by lower SBRs. Our study is the first to report data on the SBR, an important parameter in no-shave LH-FUE, since more unbroken long-hair-shafted grafts would better achieve the objective of previewing the final result and camouflaging the surgerized bald zone. Furthermore, we have observed that all types of FUE punches can perform unshaven LH-FUE with varying degrees of success, with blunter punches performing better than their sharper counterparts. However, apart from a higher GTR, the SBR is typically high, inconsistent, and widely ranging (25–75%). Thus, SBRs should be reported alongside GTRs as standard in no-shave LH-FUE studies. Finally, there was no significant difference in SBRs between SFS classes or between 19G and 18G SRFD punches. However, the later result might be related to the fact that 36% of the time, we used both 19 and 18G punches in the same patient.
SFS is valuable as it captures the combined influence of skin and hair characteristics on procedural settings and outcomes.7 Not surprisingly, higher SFS-classified donor areas (denoting thicker, firmer skin combined with curlier hair) had relatively higher GTRs and required higher torque and longer movement durations to complete follicle separation from tissue attachments compared to those in lower SFS classes. Skin thickness influenced the SBR more significantly than the SFS class, with thicker and firmer skin resulting in higher SBRs. During punch scoring, the subcutaneous fat in the surrounding tissue at a shallow depth helps avoid long hair shaft breakage by serving as a soft board onto which the hair rolls over on the cutting edge of the punch, with less risk of being cut6 (Figure 2B). However, in thick skin, due to a naturally thicker dermis (seen in SFS classes IV and V) or a scarred donor environment, the punch-cutting tip travels through a longer dermal/fibrous path, whereby the hair shaft rolls onto the punch’s cutting edge against a more rigid tissue surface composed of the fibrous dermis, thereby resulting in a higher SBR. This study is also the first to report success with no-shave LH-FUE across skin and hair types, including African-descended Black patients with curly-coiled hair, a population considered challenging to conventional (ie, shaved) FUE due to their curled hair.8–10
The variability observed among surgeons in the total number of grafts harvested may reflect different levels of popularity of no-shave LH-FUE among locations. Differences in the GTR and GER may be explained by variations in patient demographics influencing the SFS class and skin types. Other factors influencing variability in GTRs and GERs include variations in the level of experience, methods of donor area preparation for unshaven LH-FUE (eg, clearing the surgical field of hair and blood), and choreography of the staff regarding scoring and graft removal. Notwithstanding these differences, all five surgeons reported favorable GTRs and SBRs, four of whom reported GER values falling within the range of the overall group. As more surgeons adopt unshaven LH-FUE due to its improved ease of use and efficiency, informed consent must emphasize the shedding of implanted long-shafted grafts, which patients can expect to occur at 2–8 weeks after surgery.
The strengths of this study include its multinational nature, with diverse patient demographics, skin and hair types, and a range of surgeon experiences. The limitations of this investigation include its small sample size and differences in unshaven LH-FUE expertise among FUE practitioners and staff. Future studies should evaluate procedural outcomes using larger sample sizes and standardized procedures across diverse patient populations.
Conclusion
No-shave LH-FUE is limited by the requirement of recess-tipped punches to minimize graft attrition and long hair shaft breakage, contributing to a slower and technically more challenging process. We report consistent success across patients with different skin and hair types using no-shave LH-FUE with a recess-free punch-tipped all-purpose SRFD, resulting in low GTR and SBR, and high procedure speed, patient satisfaction, and surgeon adoption rate.
Data Sharing Statement
Source data is available on request to the corresponding author.
Ethics and Consent
All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from patients, including consent for publication and use of photographs. An institutional review board exemption was obtained from the Western IRB Copernicus Group.
Acknowledgments
We are particularly grateful to our patients and dermatology staff.
Funding
There is no funding to report.
Disclosure
The first author owned shares in and issued patents and patent applications for FineTouch Dr. U Devices, Inc. at the time of this work. The other authors declare that they have no conflicts of interest.
References
1. Park JH, You SH, Kim NR, Ho YH. Long hair follicular unit excision: personal experience. Int J Dermatol. 2021;60(10):1288–1295. doi:10.1111/ijd.15648
2. Trivellini R, Perez-Meza D, Renaud HJ, Gupta AK. Preview long hair follicular unit excision: an up-and-coming technique. J Cosmet Dermatol. 2021;20(11):3422–3426. doi:10.1111/jocd.14026
3. Boaventura O. Long hair FUE and the donor area preview. Hair Transpl Forum Int. 2016;26(5):200–202. doi:10.33589/26.5.0200
4. Erdogan K Apparatus with needle for the extraction of hair follicles in long form. US Patent No. 0282260; 2019. Available from: https://www.freepatentsonline.com/20190282260.pdf.
5. Schambach MA. Shaved FUE vs long hair FUE: a comparative study during excision, extraction, and placement. Hair Transpl Forum Int. 2020;30(4):117–126. doi:10.33589/30.4.117
6. Umar S, Lohlun B, Ogozuglu T, Carter MJ. A novel follicular unit excision device for all-purpose hair graft harvesting. Clin Cosmet Invest Dermatol. 2021;14:1657–1674. doi:10.2147/CCID.S333353
7. Umar S, Shitabata P, Rose P, et al. A new universal follicular unit excision classification system for hair transplantation difficulty and patient outcome. Clin Cosmet Invest Dermatol. 2022;15:1133–1147. doi:10.2147/CCID.S369346
8. Umar S, Khanna R, Lohlun B, et al. Follicular unit excision in patients of african descent: a skin-responsive technique. Dermatol Surg. 2023;49(10):949–955. doi:10.1097/DSS.0000000000003881
9. Singh MK, Avram MR. Technical considerations for follicular unit extraction in African-American hair. Dermatol Surg. 2013;39(8):1282–1284. doi:10.1111/dsu.12229
10. Umar S. Comparative study of a novel tool for follicular unit extraction for individuals with afro-textured hair. Plast Recontr Surg Glob Open. 2016;4:e1069.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







