Back to Journals » Clinical Ophthalmology » Volume 11
No improvement in injection frequency or in visual outcome over time in two cohorts of patients from the same Swedish county treated for wet age-related macular degeneration
Authors Schroeder M, Rung L, Lövestam-Adrian M
Received 14 December 2016
Accepted for publication 13 April 2017
Published 9 June 2017 Volume 2017:11 Pages 1105—1111
DOI https://doi.org/10.2147/OPTH.S130182
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Marion Schroeder,1 Lena Rung,2 Monica Lövestam-Adrian1
1Division of Ophthalmology, Department of Clinical Sciences Lund, Lund University, Skåne University Hospital, Lund, 2Department of Ophthalmology, Helsingborg Hospital, Helsingborg, Sweden
Background: Although ranibizumab has been used for the treatment of wet age-related macular degeneration (AMD) since 2007, real-world studies still report undertreatment resulting in a less favorable visual outcome. In this study, two different time cohorts of patients treated with ranibizumab for wet AMD in routine care were analyzed to observe whether there was a change over time regarding visual outcome, injection frequency, and quality of life (QoL).
Methods: We compared patients with treatment-naïve wet AMD in two observational follow-up cohorts 2007–2010 (n=50 patients) and 2009–2013 (n=26). After a loading dose of three intravitreal ranibizumab injections, the patients were treated under the pro re nata regimen. Visual acuity (VA) was examined by Early Treatment Diabetic Retinopathy Study (ETDRS) charts. The National Eye Institute Visual Functioning Questionnaire 25 was answered by patients at baseline and at 37±7 months (cohort 1) and at 45±4 months (cohort 2).
Results: At baseline, the cohorts were homogeneous considering mean age (76±7 vs 75±8 years), mean VA (53±14 vs 52±15 ETDRS letters), and mean self-reported symptom duration (14±11 vs 13±11 weeks). Mean VA decreased in both cohorts over time, from 53±14 to 45±24 letters (P=0.011) and from 52±15 to 46±22 letters (P=0.175), respectively. The patients received a mean of 8±5 and 9±7 injections, respectively. The mean composite score change from baseline to follow-up decreased in cohort 1 from 64±21 to 59±25 scores (P=0.04) but increased in cohort 2 from 64±28 to 67±23 scores (P=0.38).
Conclusion: We could not demonstrate any improvement in the number of injections in two different time cohorts of patients treated with ranibizumab for wet AMD in a Swedish county. Visual outcomes decreased after 3 years of follow-up, but QoL scores were divergent.
Keywords: neovascular AMD, anti-VEGF, NEI VFQ-25, clinical care
Introduction
Neovascular age-related macular degeneration (AMD) is a common disease and, in advanced stages, a key cause of visual impairment in the elderly population in Western countries.1 Since the introduction of anti-vascular endothelial growth factor (anti-VEGF) agents, a treatment that both improves and stabilizes visual acuity (VA) can be provided. This was first confirmed by the ANCHOR and MARINA clinical trials for ranibizumab and then the VIEW studies for aflibercept.2–4 These trials employed a fixed regimen with monthly or bimonthly dosing up to 12 months – a treatment regimen that has turned out to be both expensive and time consuming. Following the approval and implementation of ranibizumab and aflibercept in the clinics, it has been observed that almost no clinics have the possibility of implementing monthly or bimonthly treatment and that they have thus switched to a pro re nata (PRN) regimen instead. PRN indicates monthly visits with retreatment only in case of neovascular activity such as hemorrhage or fluid accumulation.5
However, exploration of real-life data has shown that PRN regimens give less favorable results, with the patients achieving a mean change of between −0.8 and +3 letters following 12 months of ranibizumab treatment.6,7
The National Eye Institute Visual Functioning Questionnaire 25 (NEI VFQ-25) has recently been described as corresponding well to changes in VA,8 and the influence on everyday quality of life (QoL) in patients treated with anti-VEGF for wet AMD.9 This has also been confirmed in clinical trials with an improvement in the overall composite score for the questionnaire.10 In a recent real-world study from Sweden, we could demonstrate poor visual outcomes after 3 years of follow-up due to undertreatment of wet AMD, resulting in a decrease in self-reported visual function for distance activities but, unexpectedly, an unchanged score for mental health items such as worrying.11
The purpose of this study was to observe if there was a change and improvement over time regarding visual outcomes, injection frequency, and QoL in two Swedish cohorts treated with ranibizumab during 2007–2010 and 2009–2013 under routine clinical care.
Methods
We compared two follow-up cohorts of patients with neovascular AMD from the outpatient clinic at the Department of Ophthalmology in Helsingborg Hospital. A patient consent statement was obtained from all the patients. A description of the first cohort was presented recently,11 which was having one eye per participant with primary, untreated classic or occult choroidal neovascularization (CNV) and no other retinal disease. A loading dose of three consecutive monthly intravitreal injections of ranibizumab was administered at baseline. The consultant ophthalmologists of the department decided on retreatment at each visit in a clinical setting. Reinjection was given if CNV activity was demonstrated in the form of new hemorrhages at examination or/and persistent or new fluid was seen on analysis by optical coherence tomography (OCT). Another criterion was a decrease in VA by five or more letters. If no activity signs were present, the next visit was planned after approximately 4 weeks but could be extended up to 6 weeks. This time scheduling was not often followed properly as the clinic was always overloaded and busy.
Cohort characteristics
Cohort 111 included 50 patients who were followed for 37±7 months from 2007 to 2010, and cohort 2 included 26 patients followed for 45±4 months from 2009 to 2013. The patients received a mean of 8±5 and 9±7 injections, respectively, during the follow-up period. All participants completed the NEI VFQ-25 questionnaire at baseline and at the last visit.
Ophthalmological examination
The ophthalmological examinations conducted were the same in both the cohorts and were described in detail in the first reported cohort by Rung and Lövestam-Adrian.11 In short, the baseline examination included testing of best-corrected visual acuity (BCVA) using the Early Treatment Diabetic Retinopathy Study (ETDRS) chart, near vision evaluation, biomicroscopic examination, and intraocular pressure measurement. The patients underwent fluorescein-and-indocyanine green angiography, fundus photography (Topcon TRC-50 ix camera), as well as OCT (Zeiss Humphrey Instruments, Dublin, CA, USA). All examinations were done at baseline before including the patients in the study.
NEI VFQ-25
The NEI VFQ-25 version 20008 was used as an authorized Swedish version (VFQ-25-Swedish/Sweden; vfq, S001_1). Our patients completed the test at baseline and at the last follow-up visit. The questionnaire includes 25 questions designed to measure the influence of visual function on self-reported health status in daily life. There are 12 vision-targeted subscales including general health, general vision, ocular pain, near activities, distance activities, driving, color vision, peripheral vision, vision-specific social functioning, mental health, role difficulties, and vision-specific dependency. The answers are recoded to scores with values from 0 to 100. The higher the score, the better is the vision-related function. The overall composite score evaluates the mean of the combined 11 subscales, except for general health.
Statistics
The data were analyzed using SPSS, version 23.0. The comparison of the mean values between groups was performed by applying the Student’s t-test for normally distributed data and the Mann–Whitney U-test for nonparametric data. In cases of multiple comparisons of nonparametric data, we used the Kruskal–Wallis test. Correlations between parameters were assessed with Spearman’s rho. All tests were two-sided, and P<0.05 was considered significant. The values are expressed as mean ± standard deviation.
The research procedures were performed in accordance with the institutional guidelines and the Declaration of Helsinki. Approval for the study was obtained from the Ethics Committee at Lund University, Sweden.
Results
Demographics
At baseline, the cohorts were homogeneous considering mean age (75±7 vs 75±8 years), mean VA (53±14 vs 52±15 letters), and mean self-reported symptom duration (14±11 vs 13±11 weeks). The study included 50 eyes of 50 patients (56% female) in cohort 1 and 26 eyes of 26 patients (62% female) in cohort 2.
Visual acuity
Mean VA decreased in the first cohort over time from 53±14 to 45±24 letters (P=0.01), and a similar trend was seen in cohort 2, a decrease from 52±15 to 46±22 letters (P=0.17).
We divided the VA outcome into three categories as in the analyses of MARINA and ANCHOR: gain of ≥15 letters, gain or loss (stabilization) of <15 letters, and loss of ≥15 letters.9
The results of gained or lost letters at the end of the follow-up period in cohort 1 vs cohort 2 were as follows: five (10%) vs three (11%) eyes gained at least 15 letters, 29 (58%) vs 14 (54%) eyes were stabilized (gain or loss of <15 letters), and 16 (32%) vs nine (35%) eyes lost ≥15 letters. There was no difference between the two cohorts.
Intravitreal injections
The patients received a mean of 7.8±5.0 and 8.5±7.2 (P=0.66) injections in the two cohorts, respectively.
Treatment of the better- or worse-seeing eye
A total of 9.5±5.7 injections were administered for 15 better-seeing eyes in cohort 1 and 10.9±9.4 for nine eyes in cohort 2. A total of 7.1±4.6 injections were administered for 34 worse-seeing eyes in cohort 1 and 7.3±5.6 for 17 eyes in cohort 2.
Injections in eyes with improved, stabilized, or worse visual outcome
Cohort 1
The distribution of the number of injections differed significantly between the three ETDRS groups in cohort 1 (P=0.001). The group with an improvement of ≥15 letters received a mean of 10.2±5.2 injections. Patients with a gain or loss of <15 letters received a mean of 9.3±5.3 injections. In the group with a loss of ≥15 letters, the patients received 4.2±1.6 injections.
Cohort 2
The number of injections was equally distributed between the three ETDRS groups in cohort 2 (P=0.876). The group with an improvement of ≥15 letters received a mean of 10.3±11.8 injections. Patients with a gain or loss of <15 letters received a mean of 8.7±8.2 injections. In the group with a loss of ≥15 letters, the patients received 7.7±3.8 injections.
Only the group with a loss of ≥15 letters showed a difference in the number of injections between the two cohorts: 4.2±1.6 vs 7.7±3.8 injections (P=0.021).
NEI VFQ-25
The mean composite score change from baseline to follow-up was from 64±21 to 59±25 scores in cohort 1 (P=0.04) and from 64±28 to 67±23 scores in cohort 2 (P=0.38).
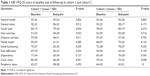
In cohort 1, also reported by Rung and Lövestam-Adrian,11 reflecting the impairment in VA at follow-up, we showed a decrease in many of the questionnaire scores, that is, in scores for general health from 57±26 to 47±24 points (P=0.004), ocular pain from 84±19 to 79±24 points (P=0.024), and distance activities from 57±28 to 46±31 points (P=0.011) (Table 1). We also showed a decrease in the vision-specific items such as color vision from 82±30 to 66±30 points (P=0.001), social functioning from 75±27 to 65±30 points (P=0.029), and role difficulties from 67±29 to 56±32 points (P=0.034) (Table 1).
In cohort 2, there was also a decrease in VA at follow-up; however, it did not influence the questionnaire results as in cohort 1. Some of the scores and also the composite scores increased at follow-up, but without reaching significant levels (Table 1).
In both cohorts, the group of patients with an increase of ≥15 letters showed a trend to gain the largest mean increase in the NEI VFQ-25 score. On the other hand, the group with a loss of ≥15 letters showed the greatest decrease in the NEI VFQ-25 scores.
We focused on the composite score and the three subscales near activities, distance activities, and vision-specific dependency from the NEI VFQ-25 questionnaire when comparing the visual outcome groups: patients with a gain of ≥15 letters to those with a gain or loss of <15 letters to those with a loss of ≥15 letters. Only the change in near activities scores in cohort 1 was significant between the three groups (P=0.044; Figure 1A–D).
Merged cohort 1 and 2
Intravitreal injections
The distribution of the number of injections differed significantly between the three ETDRS groups in the merged cohort 1 and 2 (P=0.04). The group with an improvement of ≥15 letters received a mean of 10.25±7.4 injections. Patients with a gain or loss of <15 letters received a mean of 9.12±6.3 injections. In the group with a loss of ≥15 letters, the patients received 5.5±3.1 injections.
NEI VFQ-25
We focused on the composite score and the three subscales near activities, distance activities, and vision-specific dependency from the NEI VFQ-25 questionnaire. The mean composite score for the merged cohort was 64±24 at baseline and 62±24 at follow-up. No difference was seen between any of the three ETDRS groups (Figure 2A–D). Baseline BCVA correlated to mean change in composite score (P=0.048), near activity (P=0.001), and distance activity (P=0.06) in patients with a gain or loss of <15 letters.
Discussion
In this clinical follow-up study, we found that mean VA decreased over the observed time period in both cohorts.
Our results regarding VA are worse than those reported in other clinical studies such as the COMPASS and TWIN studies,12,13 although not quite comparable because this study had a longer observational time period. However, the data of this study are comparable to a French study by Boulanger-Scemama et al,14 which showed a gain of ≥0 letter in 43% of eyes and a loss of ≥15 letters in 29% of patients after 5 years of PRN treatment. The type of treatment regimen is of importance, and one major problem in routine care of AMD patients is to keep up with the examination visits. In our study, most of the patients were not regularly examined every month. Hence, naming the regimen as “extend and treat” would have been more appropriate than “PRN”.
Today, there is limited information on the long-term outcomes of patients treated with intravitreal injections. The SEVEN-UP trial15 evaluated VA after 7–8 years of initiation of ranibizumab therapy in 65 neovascular AMD patients who were originally treated in the ANCHOR and MARINA studies2 and the open-label extension HORIZON trial.5 In the HORIZON study, the switch from a strict, monthly ranibizumab regimen to a more relaxed PRN regimen with less frequent follow-up not only resulted in worsening and progression of AMD in patients but also resulted in a decline in the VA gains achieved on the strict monthly dosing regimen. Patients from the SEVEN-UP trial have received a mean of 1.6 injections per year since the HORIZON study, which is comparable to our study. However, the mean VA of 54 letters at follow-up in the HORIZON study was higher than in this study, and almost on par with the baseline VA before treatment in this study. The low baseline VA might well partly explain the poor visual outcomes in our study, as baseline VA has been shown to be well correlated to visual outcome. Furthermore, early treatment, before a more prominent decline in VA is present, has been shown to be independently correlated to visual outcome after 3 months.16
The number of injections did not increase in cohort 2 compared to cohort 1. This was somewhat unexpected as treatment with ranibizumab was introduced in Sweden in 2007 and anti-VEGF treatment has been the standard of care of wet AMD since then. This further indicates that PRN or variations of PRN are not to be recommended, due to overloaded clinics and lack of health care resources.
Although baseline VA and the number of injections were the same in the two cohorts, we merged the two cohorts into one. As expected, more injections also resulted in a gain of more letters at follow-up. Interestingly, even eyes that gained >15 letters had fewer injections compared to other studies.5,6 This suggests that there are eyes with wet AMD lesions that do well even with a low number of injections. This is something that needs to be focused on when discussing the treat-and-extend regimen, where all eyes will be injected at every visit.
It is known that visually impaired patients experience reduced QoL with greater social dependence and higher rates of clinical depression compared to healthy individuals with normal vision.17 When analyzing the two cohorts, we did find that an impairment in VA at follow-up resulted in a decrease in many of the questionnaire scores in cohort 1 but not in cohort 2. This was not only due to the fewer patients in cohort 2, as some of the questionnaire scores even increased at follow-up, but without reaching significant levels. In agreement with other studies,9,18 we could demonstrate a trend toward higher NEI VFQ-25 scores in patients gaining more letters and the opposite in patients losing many letters, although this was only significant in the near vision scores in cohort 1. The overall absence of significance is partly due to the low number of patients included.
In conclusion, patients treated for wet AMD in routine care were undertreated and had a worse visual outcome compared to clinical trials. Although the treatment with anti-VEGF was well established by the time cohort 2 was started, no improvement in injection frequency or visual outcome was seen compared to cohort 1. This shows the difficulties in managing the time-consuming care of AMD patients in clinical routine. The NEI VFQ-25 score results were divergent but were higher in patients gaining more letters and lower in patients losing many letters.
Acknowledgments
This study was supported by grants from the Medical Faculty, Lund University and the Foundation for Visually Impaired in old Malmöhus Län.
Disclosure
Marion Schroeder has received lecturer fees from Novartis (Novartis AG) and is a grant recipient from Bayer. Monica Lövestam-Adrian is a consultant for Allergan, Novartis, and Bayer, and a grant recipient from Bayer. Lena Rung has no relevant financial or nonfinancial relationships to disclose in this work. The authors report no other conflicts of interest in this work.
References
Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam study. Arch Ophthalmol. 1998;116(5):653–658. | ||
Rosenfeld PJ, Brown DM, Heier JS, et al; MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. | ||
Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T; ANCHOR Study Group. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009;116(1):57–65.e5. | ||
Heier JS, Brown DM, Chong V, et al; VIEW 1 and VIEW 2 Study Groups. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2537–2548. | ||
Singer MA, Awh CC, Sadda S, et al. HORIZON: an open-label extension trial of ranibizumab for choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology. 2012;119(6):1175–1183. | ||
Holz FG, Amoaku W, Donate J, et al; SUSTAIN Study Group. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118(4):663–671. | ||
Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–226. | ||
Orr P, Rentz AM, Margolis MK, et al. Validation of the National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25) in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52(6):3354–3359. | ||
Suñer IJ, Kokame GT, Yu E, Ward J, Dolan C, Bressler NM. Responsiveness of NEI VFQ-25 to changes in visual acuity in neovascular AMD: validation studies from two phase 3 clinical trials. Invest Ophthalmol Vis Sci. 2009;50(8):3629–3635. | ||
Bressler NM, Chang TS, Suñer IJ, et al; MARINA and ANCHOR Research Groups. Vision-related function after ranibizumab treatment by better- or worse-seeing eye: clinical trial results from MARINA and ANCHOR. Ophthalmology. 2010;117(4):747–756.e4. | ||
Rung L, Lövestam-Adrian M. Three-year follow-up of visual outcome and quality of life in patients with age-related macular degeneration. Clin Ophthalmol. 2013;7:395–401. | ||
Souied EH, Oubraham H, Mimoun G, Cohen SY, Quere S, Derveloy A; TWIN Study Group. Changes in visual acuity in patients with wet age-related macular degeneration treated with intravitreal ranibizumab in daily clinical practice: the TWIN study. Retina. 2015;35(9):1743–1749. | ||
Wolf A, Kampik A. Efficacy of treatment with ranibizumab in patients with wet age-related macular degeneration in routine clinical care: data from the COMPASS health services research. Graefes Arch Clin Exp Ophthalmol. 2014;252(4):647–655. | ||
Boulanger-Scemama E, Sayag D, Ha Chau Tran T, et al. Ranibizumab et dégénérescence maculaire liée à l’âge exsudative: analyse multicentrique à 5 ans des résultats fonctionnels et anatomiques en pratique clinique réelle. [Ranibizumab and exudative age-related macular degeneration: 5-year multicentric functional and anatomical results in real-life practice]. J Fr Ophtalmol. 2016;39(8):668–674. French [with English abstract]. | ||
Bhisitkul RB, Mendes TS, Rofagha S, et al. Macular atrophy progression and 7-year vision outcomes in subjects from the ANCHOR, MARINA, and HORIZON studies: the SEVEN-UP study. Am J Ophthalmol. 2015;159(5):915–924.e2. | ||
Rasmussen A, Brandi S, Fuchs J, et al. Visual outcomes in relation to time to treatment in neovascular age-related macular degeneration. Acta Ophthalmol. 2015;93(7):616–620. | ||
Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes. 2006;4:97. | ||
Chang TS, Bressler NM, Fine JT, Dolan CM, Ward J, Klesert TR; MARINA Study Group. Improved vision-related function after ranibizumab treatment of neovascular age-related macular degeneration: results of a randomized clinical trial. Arch Ophthalmol. 2007;125(11):1460–1469. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.