Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
New Users of Herbal Medicine Containing Aristolochic Acids and the Risk of Dementia in the Elderly: A Nationwide, Population-Based Study in Taiwan
Authors Chiou YE , Chien WC , Chung CH , Chang HA, Kao YC, Tsay PK , Tzeng NS
Received 20 February 2020
Accepted for publication 22 May 2020
Published 12 June 2020 Volume 2020:16 Pages 1493—1504
DOI https://doi.org/10.2147/NDT.S250659
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Yuping Ning
Yueh-Er Chiou,1,2 Wu-Chien Chien,3– 5,* Chi-Hsiang Chung,3,4,6 Hsin-An Chang,7,8 Yu-Chen Kao,7,9 Pei-Kwei Tsay,10,* Nian-Sheng Tzeng7,8,*
1Department of Nursing, College of Medicine, Fu Jen Catholic University, New Taipei City, Taiwan; 2Graduate Institute of Clinical Medical Sciences, College of Medicine, Chang Gung University, Tao-Yuan, Taiwan; 3Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan; 4School of Public Health, National Defense Medical Center, Taipei, Taiwan; 5Graduate Institute of Life Sciences, National Defense Medical Center, Taipei, Taiwan; 6Taiwanese Injury Prevention and Safety Promotion Association, Taipei, Taiwan; 7Department of Psychiatry, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taipei, Taiwan; 8Student Counseling Center, National Defense Medical Center, Taipei, Taiwan; 9Department of Psychiatry, Tri-Service General Hospital, Song-Shan Branch, National Defense Medical Center, Taipei, Taiwan; 10Department of Public Health and Center of Biostatistics, College of Medicine, Chang Gung University, Tao-Yuan 333, Taiwan
*These authors contributed equally to this work
Correspondence: Pei-Kwei Tsay
Department of Public Health and Center of Biostatistics, College of Medicine, Chang Gung University, Tao-Yuan 333, Taiwan
Tel +886-3-211-8800 # 5068 (PKT)
Email [email protected]
Nian-Sheng Tzeng
Joint Program for Geriatric Psychiatry and Psychosomatic Medicine, Department of Psychiatry, School of Medicine, Tri-Service General Hospital, National Defense Medical Center, 325, Section 2, Cheng-Gung Road, Nei-Hu District, Taipei, Taiwan, Republic of China
Tel +886-2-87923311, Ext 17484
Fax +886-2-87927221
Email [email protected]
Background: Herbal medicine containing aristolochic acids (HMCAA) was used for inflammatory and infectious diseases. This study aimed to investigate the association between the usage of HMCAA and the risk of dementia.
Methods: A total of 199 new users of HMCAA were enrolled, along with 597 controls without the usage of HMCAA, at a ratio of 1:3 – matched by age, sex, and comorbidity, between 2000 and 2003 – from the National Health Research Institutes Database (NHRID) of Taiwan, which contains two million randomly sampled subjects, in this cohort study. We used Fine and Gray’s survival analysis (competing with mortality) to compare the risk of developing dementia during a 15-year follow-up period (2000– 2015).
Results: In general, HMCAA was not significantly associated with dementia (adjusted subdistribution hazard ratio [SHR] = 0.861, 95% confidence interval [CI] = 0.484– 1.532, p = 0.611) for the HMCAA-cohort, although differential risk was observed among the groups at risk. The patients with usage of HMCAA aged ≧ 85 years were associated with a higher risk in dementia (adjusted SHR: 6.243, 95% CI=1.258– 21.084, p = 0.001), in comparison to those aged 50– 54 years. Furthermore, the patients with usage of HMCAA that had cerebrovascular accidents were associated with an increased risk of dementia.
Conclusion: The usage of HMCAA was associated with the risk of developing dementia in the patients aged ≧ 85 years.
Keywords: herbal medicine containing aristolochic acids, traditional Chinese herbal medicines, dementia
Introduction
Dementia is a global public health problem,1 and it has been estimated that the prevalence was of 2–5% for the population aged ≥65 years in Taiwan’s community studies.2–4 Dementia causes a significant increase in the cognitive and functional impairment; therefore, it is considered as a heavy burden to the caregivers and the society of these patients.5–8 Injuries on the brain such as traumatic brain injury,9 stroke,10 or carbon monoxide intoxication,11,12 could also contribute to the development of dementia. Further study is therefore needed to evaluate other toxic chemicals and the risk of dementia.
Herbal medicine containing aristolochic acids (HMCAA) have been widely used in traditional Chinese medicine.13–15 However, the Committee on Chinese Medicine and the Pharmacy of the Department of Health in Taiwan has banned HMCAA since 2003,14 because of its nephrotoxicity.16–18 HMCAA is an inhibitor of phospholipase A2, and even an apoptosis inducer.19 In addition, phospholipases serve as mediators of the amyloid-beta peptide neurotoxicity, as an early event contributing to the neurodegeneration characteristic of Alzheimer’s disease.20 On the other hand, previous studies have found that other traditional medicines, such as Jia-Wei-Xiao-Yao-San, were associated with a lower risk of dementia.21,22 However, the association between HMCAA and dementia has not, as yet, been studied. We have therefore conducted this study to investigate as to whether HMCAA was associated with the risk of dementia, by using a nationwide, population-based database in Taiwan, the National Health Insurance Research Database (NHIRD).
Methods
Data Sources
We used the Longitudinal Health Insurance Database (LHID), a subset of two million randomly sampled patients from the NHIRD, during a 15-year period (2000–2015) in this study. Taiwan’s National Health Insurance (NHI) Program was launched in 1995, and had contracts with 97% of the medical providers and enrolled more than 99% of the 23 million population, as of June, 2009.23 The details of the program have been documented in previous studies.24–36
Ethics Approval
This study was conducted according to the Code of Ethics of the World Medical Association (Declaration of Helsinki). This study was approved by the Institutional Review Board (IRB) of the Tri-Service General Hospital (TSGH). The TSGH IRB waived the need of individual consents since all the identification data were encrypted in the NHIRD (IRB No. 2-107-05-026).
Study Design and Participants
The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)37 diagnostic codes were used in the NHIRD. Each diagnosis of dementia was made by a board-certified psychiatrist or neurologist according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), and its Text-revised edition (DSM-IV-TR).38,39 The records of ambulatory care visits and inpatient claims by the NHI Administration are randomly reviewed, to verify the accuracy of the diagnoses.40 Therefore, using the NHIRD is considered as being suitable to study the association between HMCAA and the risk of development of dementia.
This is a retrospective cohort study. Patients who first started to use HMCAA from January 1, 2000, to December 31, 2003, were identified. The exclusion criteria were those using HMCAA before 2000, those diagnosed with dementia before 2000, and patients with kidney disease, liver disease, and hepatoma. A total of 199 patients who used HMCAA were enrolled, and another 597 patients who had not used HMCAA were enrolled as the control group, at a ratio of 1:3, propensity score-matched by age, sex, and index year, from the NHRID (Figure 1).
 |
Figure 1 The flowchart of study sample selection. |
The HMCAA Medications
The records of HMCAA were retrieved from the NHIRD. We also calculated the estimated cumulative dosage of aristolochic acid for each subject using an estimated average dosage of aristolochic acid per 1 g. For Guan Mu Tong, Guang Fang Ji, Ma Dou Ling, Qing Mu Xiang, Tian Xian Teng, and Xi Xin, this was 2.59, 2.04, 0.63, 0.009, 0.026, and 0.042 mg, respectively, with the reference from one previous study on HMCAA.41 We also analyzed the cumulative dosage as 1–250, 251–500, 501–1000, >1000 mg of HMCAA and the risk of dementia.
Covariates
Covariates included sex, age (50–54, 55–64, 65–74, 75–84, ≧85), geographical area of residence (northern, central, southern, and eastern Taiwan), urbanization level (levels 1 to 4, as described below), seasons for medical help, monthly insured premiums (in New Taiwan dollars (NT$): <18,000, 18,000–34,999, ≥35,000), and levels of medical care (medical center, regional hospital, and local hospital). For indexing comorbidity, we used the Charlson comorbidity index (CCI, scores of 0, 1, 2, 3, ≧4), which is the most widely used comorbidity index in the literature.13,42 Other comorbidities were diabetes mellitus, hypertension, hyperlipidemia, obesity, chronic kidney disease (CKD), atrial fibrillation, and cerebrovascular accidents (CVA). We also included the common indications of the usage of HMCAA as hepatitis, UTI, dysuria, urolithiasis, vaginitis, scrotum swelling, inguinal hernia, dysmenorrhea, oral ulcer, upper respiratory tract infection (URI), bronchitis, pneumonia, cough, allergy, eczema, headache, arthralgia, pain, neuralgia, heart failure, edema, CVA (Table S1). 41
Major Outcome
All of the study participants were followed from the index year until the onset of dementia, death, withdrawal from the NHI program, or the end of 2015. Patients with dementia were identified by the ICD-9-CM codes of 290.0, 290.10, 290.11, 290.12, 290.13, 290.20, 290.21, 290.3, 290.41, 290.42, 290.43, 290.8, 290.9, and 331.0, and the types of dementia are grouped as follows: Alzheimer dementia (AD), vascular dementia (VaD), and other dementia (Table S1).
Statistical Analysis
All analyses were performed using the SPSS software version 22.0 for Windows (IBM Corp., Armonk, NY). χ2 and t-tests were used to evaluate the distribution of the categorical and continuous variables between the patients who did and did not use HMCAA. In addition, the Fisher exact test for categorical variables was used to statistically examine the differences between the two cohorts, while the sample size was < 5. For the analysis of the non-normally distributed variables between the cohorts, the U-test was used. Fine and Gray’s survival analysis and regression analysis were used to determine the risk of dementia (competing with mortality), and the results were presented as a subdistribution hazard ratio (SHR) with a 95% confidence interval (CI).43 The Value-added module, including the Competing Risks Survival Analysis, in the SPSS, was used to conduct the Fine and Gray’s survival analysis (https://www.asia-analytics.com.tw/en/product/p-asia-analytics-2.jsp). Differences in the risk of dementia between the two groups were estimated using the Kaplan–Meier method with the Log-rank test. A 2-tailed p value <0.05 was considered to be statistically significant.
Results
Baseline Characteristics of the Study Population
Table 1 depicts the baseline characteristics of the study population. There were 199 subjects in the HMCAA usage group and 597 in the non-HMCAA controls, with a similar distribution of sex, age, insured premiums, CCI scores, comorbidities, medical indications, seasons, geographical area of residence, urbanization levels, and levels of medical care.
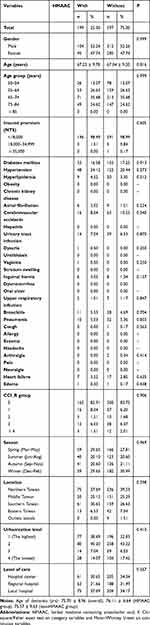 |
Table 1 Characteristics of Study at the Baseline |
The Association Between HMCAA and Dementia in the Patients Aged ≧ 85 Years
Of the HMCAA usage group, 18 (674.29 per 100,000 person-years) developed dementia when compared to 57 (706.82 per 100,000 person-years) in the control group, after the 15-year follow-up. The Kaplan–Meier analysis was used for the dementia-free survival in the HMCAA-users and user controls (Log-rank test, p = 0.909) in Figure 2. In addition, the overall mean ages at the beginning of the dementia were: 75.70 (Standard deviations [SD] ± 8.96) years for), 76.11 (SD ± 6.64) years for the HMAAC group, and 75.57 (SD± 9.63) years for the non-HMAAC group.
 |
Figure 2 Dementia-free survival for patients with HMCAA users and non-users during the 15-year follow-up period in Taiwan from the index year. |
Table 2 depicts that Fine and Gray’s survival analysis revealed that the adjusted SHR for dementia was 0.861 (95% CI = 0.484–1.532, p = 0.611), when compared with the controls, after adjusting for age, sex, CCI scores, and all the covariates. There were multicollinearities between the urbanization levels and regions, thus we only analyzed the urbanization levels. The adjusted SHR for patients aged ≧85 years was adjusted SHR: was 6.243 (95% CI=1.258–21.084, p = 0.001) in contrast to patients with age 50–55. Furthermore, the patients with usage of HMCAA with cerebrovascular accidents were associated with the risk of dementia (adjusted SHR as 6.096, 95% CI=3.466–9.720, p<0.001). But the patients with medical help from the medical center (adjusted SHR as 0.562, 95% CI=0.262–0.996, p=0.044) and the regional hospital were associated with a lower risk of dementia (adjusted SHR as 0.534 as 95% CI=0.290–0.984, p<0.039).
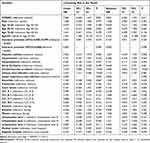 |
Table 2 Factors of Dementia by Using Cox Regression |
Table S2 depicts that the Cox regression model revealed that the adjusted HR for dementia was 0.929 (95% CI = 0.528–1.634, p = 0.797), when compared with the controls, after adjusting for age, sex, CCI scores, and all the covariates. There were multicollinearities between the urbanization levels and regions, thus, we only analyzed the urbanization levels. The adjusted HR for the patients aged ≧85 years was 8.996 (95% CI=1.813–31.020, p = 0.001) in contrast to the patients aged 50–55 years. Furthermore, the patients with usage of HMCAA with urinary tract infection (adjusted HR as 6.157, 95% CI=3.563–10.640, p<0.001) were associated with the risk of dementia. The patients who resided in the urbanization level 1 area (adjusted HR as 1.990, 95% CI=1.032–3.835, p=0.040) were also associated with the risk of dementia. But the patients with the CCI 1 (adjusted HR as 0.128, 95% CI=0.017–0.968, p=0.046) were associated with a lower risk of dementia.
Table S3 reveals that the other type of dementia was found to be proportionately higher than AD and VaD, in both HMCAA and non-HMCAA groups. For example, there were 11.11% of AD in the HMCAA group. In addition, the adjusted SHR of AD, VaD, and other dementia were 2.601 (p = 0.189), 0.606 (p = 0.772), and 0.834 (p = 0.420), respectively.
Table S4 reveals the mortality information of this study, including the mean age of mortality and the leading causes of mortality in the HMCAA-users or non-user controls. The mean ages of the mortality of the HMCAA users were 75.99 (SD ± 7.72) years and 76.37 (SD ± 9.55) years. Table S5 depicts the sensitivity analysis for the risk of dementia by excluding the dementia diagnosis in the first, first two, and first 5 years.
Table S6 shows the subgroup analysis for the factors of dementia using the Cox regression and Fine and Gray’s competing risk model. The p-values of the interaction term analysis of Age × HMAAC were 0.019 in the non-competing risk model and0.013 in the competing risk model.
For the adjustment of the different covariates, we conducted all the seven models, from no adjustment (Model 0) to adjustment with all the covariates (Model 6). All the models of adjustment were not statistically significant (Table S7).
The Cumulative Dosage of HMCAA and the Risk of Dementia
The HMCAA was not associated with the increased risk of dementia in different cumulative dosages. After 2005, no usage of HMCAA was found in the participants from this study (Table 3).
 |
Table 3 Factors of Dementia in Different Model by Using Cox Regression and Fine and Gray’s Competing Risk Model |
Discussion
The Association Between HMCAA and the Risk of Dementia
After adjusting for the covariates, the overall adjusted SHR was 0.861 (95% CI = 0.484–1.532, p = 0.611), when compared with the controls. HMCAA was not significantly associated with the risk of different types of dementia. The Kaplan-Meier analysis revealed that the 15-year cumulative incidence rate between the HMCAA-cohort and the controls was not significant (p=0.909). The adjusted SHR for patients aged ≧ 85 years was 6.243 (95% CI=1.258–21.084, p = 0.001), in contrast to the patients aged 50–55 years. In other words, the patients in the HMCAA-cohort aged ≧ 85 years had a nearly sixfold increased risk of developing dementia. In addition, the Fine and Gray’s model benefits from the use of the inclusion of the actual mortality data to study the usage of HMCAA as a risk factor for dementia.44,45
To our best knowledge, this is the first study on the topic of the association between the usage of HMCAA and the risk of dementia. Since HMCAA was widely used in Taiwan before 2003, the long-term effects could not be overlooked. Several countries have banned the usage of HMCAA,14,46 and the Food and Drug Administration (FDA) has issued a warning about consuming HMCAA.47 However, this fact does not detract from the relevance of the results for clinical practice: HMCAA-containing herbal medicine are still used in several countries such as China,48 Korea,49 and some Asian and Balkan countries.50 In addition, HMCAA could also be detected in some raw herbal medicine.51 This finding could serve as a reminder for the clinicians caring for those exposed to HMCAA, as to the potential risk of dementia in the elderly.
Comparison to Previous Literature
Several researchers have found the HMCAA-induced nephrotoxicity since 2002.16,17,52–55 Some studies have also found that HMCAA are associated with the risk of urothelial carcinoma,18,56–58 hepatocellular carcinoma,41 small intestine cancers,59 and renal cell carcinoma.59 Furthermore, Chinese herbalists exposed to HMCAA also were associated with an increased risk of renal failure60 and urothelial carcinoma.61 The present study is the first on the topic of the association between HMCAA and the risk of dementia.
Potential Mechanisms for HMCAA and Dementia
Aristolochic acids could inhibit phospholipase A2, and thus, decrease the production of prostaglandins.62 This mechanism could be a double-edged sword: Previous studies have shown that chemicals from Aristolochia arcuata, consisting of HMCAA, have neurotrophic and neuroprotective effects by decreasing the neuroinflammation.63,64 As some prostaglandins could also be neuroprotective, this mechanism could decrease the levels of these prostaglandins. In addition, there is an aging-shifted prostaglandin profile in the endothelium,65 and this might also play a role in the brain, and not only in the cardiovascular system. We hypothesize that a decrease of neuroprotective prostaglandins might as well contribute to the risk of dementia in patients, especially in the elderly patients, in the present study. However, the underlying mechanisms for the association between HMCAA and dementia in the elderly needs more detailed studies.
Furthermore, in the present study, patients who used HMCAA with CVA were also associated with the risk of dementia (adjusted SHR as 6.096, 95% CI=3.466–9.720, p<0.001). Previous studies have shown that CVA was also associated with the risk of dementia.66,67 The association between the patients with medical help from the medical centers (adjusted SHR as 0.562, 95% CI=0.262–0.996, p=0.044) and regional hospital (adjusted SHR as 0.534 as 95% CI=0.290–0.984, p<0.039) and the lower risk of dementia might reflect the impact of socio-economic levels on the risk of dementia.
Issues on the Validity of Dementia Diagnosis and Prescriptions
In the present study, using a claims database for dementia diagnosis and medications, the missed or wrong classification in the dementia cases and medication users would be a crucial issue. Although there is not yet a study to validate the dementia diagnosis in the NHIRD, previous studies have shown that most of the validated diagnosis codes are for diseases with the modest to high sensitivity and positive predictive values.68 Among these diseases, high sensitivity and positive predictive values were modest to high in several central nervous diseases, such as acute ischemic stroke69 (sensitivity as 94.5% and positive predictive values as 97.9%) and epilepsy (sensitivity as 81.4% and positive predictive values as 76.8%).70 One study have found that the medication dispensing error is 0.01% in Taiwan,71 which is low and comparable to other developed countries, such as the United States (0.08%),72 the United Kingdom (0.04),73 and Slovenia (0.02%).74 However, further studies are needed to validate the dementia diagnosis and the dispensing error rates in Taiwan’s NHIRD and the hospitals or clinics.
Interactions Between Age and the HMCAA Effects
The elder age is also a risk for the development of dementia.2–4,75 Table S6 revealed that the p-values of the interaction term analysis of Age × HMAAC were 0.019 in the non-competing risk model and 0.013 in the competing risk model for the patients aged ≧ 85 years. Therefore, there was interaction in the age of the HMCAA usage in the patients aged ≧ 85 years.
Limitations
The present study has several limitations that warrant consideration. First, like previous studies using the NHIRD, the data regarding severity, staging, and the caregiver burden of dementia, genetic, psychosocial, laboratory parameters, and environmental factors, were not reported in this claims database. Second, over the counter (OTC) HMCAA for inflammatory diseases was not included in the NHIRD. In addition, HMCAA could also be detected in the dietary supplements used as slimming regimens.76 However, most of the people would ask for help from the NHI-contracted hospital or clinics for their inflammatory diseases due to the high coverage of medical providers (97%) and beneficiaries (more than 99%) of the NHI system in Taiwan. Furthermore, it is possible that OTC HMCAA could have been used by both groups in this study before the enrollment of the two cohorts. However, it is likely that these two groups, the HMCAA-cohort and the control, have had the same opportunity to have used OTC HMCAA in 2000. Third, there could be differences between the physicians’ prescriptions and the patients’ intake, for example, 47.5% of the patients toward hypertension showed non-adherence with antihypertensive medications.77 However, we could estimate that the patients’ intake of medications may well be in a reasonable proportion from the physicians’ prescriptions. Fourth, Taiwan’s prevalence rate of dementia is 2–5%, which is low compared with international estimates, ranging from 4.6% in Central Europe, 8.7% in North Africa and the Middle East, and 5.6% to 7.6%, in other regions.78 Therefore, there is an under-ascertainment limitation in this study. Fifth, there could be several residual confounding factors in this study, although we have divided as non-modifiable factors, such as sex and age, and modifiable factors, such as comorbidities, geographical area of residence, urbanization level, seasons for medical help, monthly insured premiums, and levels of medical care. Sixth, in our study, other type of dementia was found to be proportionately higher than AD and VaD. However, in Taiwan, several community studies revealed that Alzheimer-type dementia is the most common cause of dementia (40–60% in all dementias), followed by vascular dementia (20–30% in all dementias), and mixed or other dementias (7–15%).2,3,79 One possible explanation for this disparity is that some subjects were classified as other degenerative type of dementia, similar to the findings of previous studies.80,81 Seventh, we failed to identify the factors, such as selective purchase or cultural differences, that could distinguish the HMCAA-users from the non-users by the characteristics at the study baseline (Table 1). Nonetheless, several previous studies have found individuals that are female, aged 35–59 years, in higher socioeconomic levels, with unhealthy lifestyles, and living in the areas of higher density of practicing traditional Chinese herbal medicine physicians, tend to use more Chinese herbal medicine products.82–84 Eighth, in the present study, the HMCAA users were matched with the non-users by sex, age, and index year, not including other covariates. This could be a limitation in the lack of population-based weights and propensity matching. However, a matching that included all the covariates could result in a problem that there were no enough non-users as the control group with an exact matching. In addition, even a 1:4 case-control ratio is one way to achieve higher statistical power,85 however, in the present study, we adopted a practical ratio as 1:3 matching, for obtaining enough controls for the study.
Conclusion
In general, the HMCAA-cohort was not associated with the risk of dementia. However, the usage of HMCAA in patients aged ≧ 85 years was associated with a nearly sixfold higher risk of dementia, in comparison to the controls. This finding could serve as a reminder for clinicians in charge of care for the patients who have used HMCAA, as to the potential risk of dementia in patients aged ≧ 85 years.
Data Sharing Statement
Data are available from the National Health Insurance Research Database (NHIRD) published by Taiwan National Health Insurance (NHI) Administration. Due to legal restrictions imposed by the government of Taiwan in relation to the “Personal Information Protection Act”, data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (http://www.mohw.gov.tw/cht/DOS/DM1.aspx?f_list_no=812).
Acknowledgments
This work was supported by the Medical Affairs Bureau, the Ministry of Defense of Taiwan (MAB-107-084), and the Tri-Service General Hospital Research Foundation (TSGH-C108-003, TSGHC108-027, TSGH-C108-151, and TSGH-B-109-010). These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript. We also appreciate Taiwan’s Health and Welfare Data Science Center and Ministry of Health and Welfare (HWDC, MOHW) for providing the National Health Research Database.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wortmann M. Dementia: a global health priority – highlights from an ADI and World Health Organization report. Alzheimers Res Ther. 2012;4(5):40. doi:10.1186/alzrt143
2. Liu HC, Lin KN, Teng EL, et al. Prevalence and subtypes of dementia in Taiwan: a community survey of 5297 individuals. J Am Geriatr Soc. 1995;43(2):144–149. doi:10.1111/j.1532-5415.1995.tb06379.x
3. Liu CK, Lai CL, Tai CT, Lin RT, Yen YY, Howng SL. Incidence and subtypes of dementia in southern Taiwan: impact of socio-demographic factors. Neurology. 1998;50(6):1572–1579. doi:10.1212/WNL.50.6.1572
4. Sun Y, Lee HJ, Yang SC, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS One. 2014;9(6):e100303. doi:10.1371/journal.pone.0100303
5. Tzeng NS, Chang CW, Hsu JY, Chou YC, Chang HA, Kao YC. Caregiver burden for patients with dementia with or without hiring foreign health aides: a cross-sectional study in a northern Taiwan memory clinic. J Med Sci. 2015;35(6):239–247. doi:10.4103/1011-4564.172999
6. Tzeng NS, Chiang WS, Chen SY, et al. The impact of pharmacological treatments on cognitive function and severity of behavioral symptoms in geriatric elder patients with dementia: pharmacological treatments on in elder patients with dementia. Taiwan J Psychiatry. 2017;31(1):69–79.
7. Wang HY, Chen JH, Huang SY, et al. Forensic evaluations for offenders with dementia in Taiwan’s criminal courts. J Am Acad Psychiatry Law. 2018;46(1):45–51.
8. Yeh TC, Chou YC, Weng JP, et al. Detection of malingering in the memory of patients with dementia: a pilot study on coin-in-the-hand test in a Northern Taiwan Memory Clinic. J Med Sci. 2019;39(2):81–89. doi:10.4103/jmedsci.jmedsci_100_18
9. Lee YK, Hou SW, Lee CC, Hsu CY, Huang YS, Su YC. Increased risk of dementia in patients with mild traumatic brain injury: a nationwide cohort study. PLoS One. 2013;8(5):e62422. doi:10.1371/journal.pone.0062422
10. Huang CY, Li YC, Wang HK, et al. Stroke suggests increased risk of dementia. Curr Alzheimer Res. 2015;12(3):287–295. doi:10.2174/1567205012666150302155536
11. Lai CY, Huang YW, Tseng CH, Lin CL, Sung FC, Kao CH. Patients with carbon monoxide poisoning and subsequent dementia: a population-based cohort study. Medicine. 2016;95(1):e2418. doi:10.1097/MD.0000000000002418
12. Wong CS, Lin YC, Hong LY, et al. Increased long-term risk of dementia in patients with carbon monoxide poisoning: a population-based study. Medicine. 2016;95(3):e2549. doi:10.1097/MD.0000000000002549
13. de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–229. doi:10.1016/S0895-4356(02)00585-1
14. Ministry of Health and Welfare. The department of health of the executive yuan completely banned Chinese herbal medicines containing aristolochic acid and its preparations and follow-up management measures; 2003. Available from: https://www.mohw.gov.tw/dl-10393-c2193812-7a43-4a6c-9eff-e39c8cab4a50.html.
15. Ng AWT, Poon SL, Huang MN, et al. Aristolochic acids and their derivatives are widely implicated in liver cancers in Taiwan and throughout Asia. Sci Transl Med. 2017;9(412):eaan6446. doi:10.1126/scitranslmed.aan6446
16. Hong YT, Fu LS, Chung LH, Hung SC, Huang YT, Chi CS. Fanconi’s syndrome, interstitial fibrosis and renal failure by aristolochic acid in Chinese herbs. Pediatr Nephrol (Berlin, Germany). 2006;21(4):577–579. doi:10.1007/s00467-006-0017-6
17. Kong PI, Chiu YW, Kuo MC, et al. Aristolochic acid nephropathy due to herbal drug intake manifested differently as Fanconi’s syndrome and end-stage renal failure–a 7-year follow-up. Clin Nephrol. 2008;70(6):537–541. doi:10.5414/CNP70537
18. Yang HY, Chen PC, Wang JD. Chinese herbs containing aristolochic acid associated with renal failure and urothelial carcinoma: a review from epidemiologic observations to causal inference. Biomed Res Int. 2014;2014:569325. doi:10.1155/2014/569325
19. Gardiner J, Andreeva Z, Barton D, Ritchie A, Overall R, Marc J. The phospholipase A inhibitor, aristolochic acid, disrupts cortical microtubule arrays and root growth in Arabidopsis. Plant Biol (Stuttgart, Germany). 2008;10(6):725–731. doi:10.1111/j.1438-8677.2008.00090.x
20. Kanfer JN, Sorrentino G, Sitar DS. Phospholipases as mediators of amyloid beta peptide neurotoxicity: an early event contributing to neurodegeneration characteristic of Alzheimer’s disease. Neurosci Lett. 1998;257(2):93–96. doi:10.1016/S0304-3940(98)00806-4
21. Chen KH, Yeh MH, Livneh H, et al. Association of traditional Chinese medicine therapy and the risk of dementia in patients with hypertension: a nationwide population-based cohort study. BMC Complement Altern Med. 2017;17(1):178. doi:10.1186/s12906-017-1677-4
22. Liu CT, Wu BY, Hung YC, et al. Decreased risk of dementia in migraine patients with traditional Chinese medicine use: a population-based cohort study. Oncotarget. 2017;8(45):79680–79692. doi:10.18632/oncotarget.19094
23. Ho Chan WS. Taiwan’s healthcare report 2010. EPMA J. 2010;1(4):563–585. doi:10.1007/s13167-010-0056-8
24. Huang HL, Ho SY, Li CH, et al. Bronchial asthma is associated with increased risk of chronic kidney disease. BMC Pulm Med. 2014;14:80. doi:10.1186/1471-2466-14-80
25. Yang CW, Tzeng NS, Yin YJ, et al. Angiotensin receptor blockers decrease the risk of major adverse cardiovascular events in patients with end-stage renal disease on maintenance dialysis: a nationwide matched-cohort study. PLoS One. 2015;10(10):e0140633. doi:10.1371/journal.pone.0140633
26. Chien W-C, Chung C-H, Lin F-H, Chang H-A, Kao Y-C, Tzeng N-S. Is weight control surgery associated with increased risk of newly onset psychiatric disorders? A population-based, matched cohort study in Taiwan. J Med Sci. 2017;37(4):137–149. doi:10.4103/jmedsci.jmedsci_94_16
27. Kao LC, Chien WC, Chung CH, et al. The newly diagnosed amnestic disorders and dementia: a nationwide, cohort study in Taiwan. Taiwan J Psychiatry. 2018;32(1):18–28.
28. Yang CC, Chien WC, Chung CH, et al. No association between human immunodeficiency virus infections and dementia: a nationwide cohort study in Taiwan. Neuropsychiatr Dis Treat. 2019;15:3155–3166. doi:10.2147/NDT.S225584
29. Chen TY, Huang CH, Chung CH, et al. Sex and age differences in the association between anxiety disorders and narcolepsy: a nationwide population-based case control study. J Affect Disord. 2020;264:130–137. doi:10.1016/j.jad.2019.12.010
30. Lin YC, Chen TY, Chien WC, et al. Stimulants associated with reduced risk of hospitalization for motor vehicle accident injury in patients with obstructive sleep apnea-a nationwide cohort study. BMC Pulm Med. 2020;20(1). doi:10.1186/s12890-019-1041-1
31. Liu YP, Chien WC, Chung CH, Chang HA, Kao YC, Tzeng NS. Are anticholinergic medications associated with increased risk of dementia and behavioral and psychological symptoms of dementia? A nationwide 15-year follow-up cohort study in Taiwan. Front Pharmacol. 2020;11:30.
32. Wan FJ, Chien WC, Chung CH, Yang YJ, Tzeng NS. Association between traumatic spinal cord injury and affective and other psychiatric disorders – a nationwide cohort study and effects of rehabilitation therapies. J Affect Disord. 2020;265:381–388. doi:10.1016/j.jad.2020.01.063
33. Wang DS, Chung CH, Chang HA, et al. Association between child abuse exposure and the risk of psychiatric disorders: a nationwide cohort study in Taiwan. Child Abuse Negl. 2020;101:104362. doi:10.1016/j.chiabu.2020.104362
34. Lin CH, Chien WC, Chung CH, et al. Increased risk of dementia in patients with genital warts: a nationwide cohort study in Taiwan. J Dermatol. 2020;47(5). doi:10.1111/1346-8138.15277
35. Yeh TC, Chien WC, Chung CH, et al. Psychiatric disorders after traumatic brain injury: a nationwide population-based cohort study and the effects of rehabilitation therapies. Arch Phys Med Rehab. 2020;101(5):822–831. doi: 10.1016/j.apmr.2019.12.005
36. Tzeng NS, Hsu YH, Ho SY, et al. Is schizophrenia associated with an increased risk of chronic kidney disease? A nationwide matched-cohort study. BMJ Open. 2015;5(1):e006777. doi:10.1136/bmjopen-2014-006777
37. Chinese Hospital Association. ICD-9-CM English-Chinese Dictionary. Taipei, Taiwan: Chinese Hospital Association Press; 2000.
38. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
39. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
40. National Health Insurance Administration. National health insurance reimbursement audit guidelines and notes; 2015. Available from: http://www.nhi.gov.tw/webdata/webdata.aspx?menu=20&menu_id=710&webdata_id=2889.
41. Chen CJ, Yang YH, Lin MH, et al. Herbal medicine containing aristolochic acid and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. Int J Cancer. 2018;143(7):1578–87.
42. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
43. Latouche A, Allignol A, Beyersmann J, Labopin M, Fine JP. A competing risks analysis should report results on all cause-specific hazards and cumulative incidence functions. J Clin Epidemiol. 2013;66(6):648–653. doi:10.1016/j.jclinepi.2012.09.017
44. Santabarbara J, Lopez-Anton R, de la Camara C, et al. Clinically significant anxiety as a risk factor for dementia in the elderly community. Acta Psychiatr Scand. 2019;139(1):6–14. doi:10.1111/acps.12966
45. Santabarbara J, Villagrasa B, Lopez-Anton R, et al. Clinically relevant anxiety and risk of Alzheimer’s disease in an elderly community sample: 4.5 years of follow-up. J Affect Disord. 2019;250:16–20. doi:10.1016/j.jad.2019.02.050
46. Martena MJ, van der Wielen JC, van de Laak LF, Konings EJ, de Groot HN, Rietjens IM. Enforcement of the ban on aristolochic acids in Chinese traditional herbal preparations on the Dutch market. Anal Bioanal Chem. 2007;389(1):263–275. doi:10.1007/s00216-007-1310-3
47. Food and Drug Administration. FDA warning regarding aristolochic acid; 2001. Available from: https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/herbs/news-alerts/fda-warning-regarding-aristolochic-acid.
48. IARC. Working group on the evaluation of carcinogenic risk to humans. 1.1. Identification of the agent, plants containing aristolochic acid. In: Humans IWGotEoCRt, editor. Pharmaceuticals: IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. 100A2010.
49. Ban TH, Min JW, Seo C, et al. Update of aristolochic acid nephropathy in Korea. Korean J Intern Med. 2018;33(5):961–969. doi:10.3904/kjim.2016.288
50. Han J, Xian Z, Zhang Y, Liu J, Liang A. Systematic overview of aristolochic acids: nephrotoxicity, carcinogenicity, and underlying mechanisms. Front Pharmacol. 2019;10:648. doi:10.3389/fphar.2019.00648
51. Cheung TP, Xue C, Leung K, Chan K, Li CG. Aristolochic acids detected in some raw Chinese medicinal herbs and manufactured herbal products – a consequence of inappropriate nomenclature and imprecise labelling? Clin Toxicol (Philadelphia, Pa). 2006;44(4):371–378. doi:10.1080/15563650600671712
52. Lai MN, Lai JN, Chen PC, et al. Increased risks of chronic kidney disease associated with prescribed Chinese herbal products suspected to contain aristolochic acid. Nephrology (Carlton, Vic). 2009;14(2):227–234. doi:10.1111/j.1440-1797.2008.01061.x
53. Tsai CS, Chen YC, Chen HH, Cheng CJ, Lin SH. An unusual cause of hypokalemic paralysis: aristolochic acid nephropathy with Fanconi syndrome. Am J Med Sci. 2005;330(3):153–155. doi:10.1097/00000441-200509000-00012
54. Yang HY, Lin JL, Chen KH, Yu CC, Hsu PY, Lin CL. Aristolochic acid-related nephropathy associated with the popular Chinese herb Xi Xin. J Nephrol. 2006;19(1):111–114.
55. Yang SS, Chu P, Lin YF, Chen A, Lin SH. Aristolochic acid-induced Fanconi’s syndrome and nephropathy presenting as hypokalemic paralysis. Am J Kidney Dis. 2002;39(3):E14. doi:10.1053/ajkd.2002.31425
56. Chen CH, Dickman KG, Huang CY, et al. Aristolochic acid-induced upper tract urothelial carcinoma in Taiwan: clinical characteristics and outcomes. Int J Cancer. 2013;133(1):14–20. doi:10.1002/ijc.28013
57. Wang SM, Lai MN, Wei A, et al. Increased risk of urinary tract cancer in ESRD patients associated with usage of Chinese herbal products suspected of containing aristolochic acid. PLoS One. 2014;9(8):e105218. doi:10.1371/journal.pone.0105218
58. Chen CH, Dickman KG, Moriya M, et al. Aristolochic acid-associated urothelial cancer in Taiwan. Proc Natl Acad Sci U S A. 2012;109(21):8241–8246. doi:10.1073/pnas.1119920109
59. Bara T
60. Yang HY, Wang JD, Lo TC, Chen PC. Occupational kidney disease among Chinese herbalists exposed to herbs containing aristolochic acids. Occup Environ Med. 2011;68(4):286–290. doi:10.1136/oem.2010.058594
61. Yang HY, Wang JD, Lo TC, Chen PC. Increased risks of upper tract urothelial carcinoma in male and female chinese herbalists. J Formos Med Assoc. 2011;110(3):161–168. doi:10.1016/S0929-6646(11)60026-0
62. Vishwanath BS, Gowda TV. Interaction of aristolochic acid with Vipera russelli phospholipase A2: its effect on enzymatic and pathological activities. Toxicon. 1987;25(9):929–937. doi:10.1016/0041-0101(87)90155-3
63. Zhai H, Inoue T, Moriyama M, Esumi T, Mitsumoto Y, Fukuyama Y. Neuroprotective effects of 2,5-diaryl-3,4-dimethyltetrahydrofuran neolignans. Biol Pharm Bull. 2005;28(2):289–293. doi:10.1248/bpb.28.289
64. Zhai H, Nakatsukasa M, Mitsumoto Y, Fukuyama Y. Neurotrophic effects of talaumidin, a neolignan from Aristolochia arcuata, in primary cultured rat cortical neurons. Planta Med. 2004;70(7):598–602. doi:10.1055/s-2004-827179
65. Qian H, Luo N, Chi Y. Aging-shifted prostaglandin profile in endothelium as a factor in cardiovascular disorders. J Aging Res. 2012;2012:121390. doi:10.1155/2012/121390
66. Kalaria RN, Akinyemi R, Ihara M. Stroke injury, cognitive impairment and vascular dementia. Biochim Biophys Acta. 2016;1862(5):915–925. doi:10.1016/j.bbadis.2016.01.015
67. Li CH, Chang YH, Chou MC, et al. Factors of post-stroke dementia: a nationwide cohort study in Taiwan. Geriatr Gerontol Int. 2019;19(8):815–822. doi:10.1111/ggi.13725
68. Hsieh CY, Su CC, Shao SC, et al. Taiwan’s national health insurance research database: past and future. Clin Epidemiol. 2019;11:349–358. doi:10.2147/CLEP.S196293
69. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20(3):236–242. doi:10.1002/pds.2087
70. Chen CC, Chen LS, Yen MF, Chen HH, Liou HH. Geographic variation in the age- and gender-specific prevalence and incidence of epilepsy: analysis of Taiwanese national health insurance-based data. Epilepsia. 2012;53(2):283–290. doi:10.1111/j.1528-1167.2011.03332.x
71. Chen CI, Liu CT, Chen C-I, Li Y-C, Chao CC. Medical errors in a hospital in Taiwan: incidence, aetiology and proposed solutions. J Inf Technol Healthcare. 2004;2:11–18.
72. Teagarden JR, Nagle B, Aubert RE, Wasdyke C, Courtney P, Epstein RS. Dispensing error rate in a highly automated mail-service pharmacy practice. Pharmacotherapy. 2005;25(11):1629–1635. doi:10.1592/phco.2005.25.11.1629
73. Ashcroft DM, Quinlan P, Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf. 2005;14(5):327–332. doi:10.1002/pds.1012
74. Beso A, Franklin BD, Barber N. The frequency and potential causes of dispensing errors in a hospital pharmacy. Pharm World Sci. 2005;27(3):182–190. doi:10.1007/s11096-004-2270-8
75. Liu HC, Fuh JL, Wang SJ, et al. Prevalence and subtypes of dementia in a rural Chinese population. Alzheimer Dis Assoc Disord. 1998;12(3):127–134. doi:10.1097/00002093-199809000-00002
76. Ioset JR, Raoelison GE, Hostettmann K. Detection of aristolochic acid in Chinese phytomedicines and dietary supplements used as slimming regimens. Food Chem Toxicol. 2003;41(1):29–36. doi:10.1016/S0278-6915(02)00219-3
77. Li WW, Kuo CT, Hwang SL, Hsu HT. Factors related to medication non-adherence for patients with hypertension in Taiwan. J Clin Nurs. 2012;21(13–14):1816–1824. doi:10.1111/j.1365-2702.2012.04088.x
78. Alzheimer’s Disease International. World alzheimer report 2015; 2015. Available from: https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf.
79. Lin RT, Lai CL, Tai CT, Liu CK, Yen YY, Howng SL. Prevalence and subtypes of dementia in southern Taiwan: impact of age, sex, education, and urbanization. J Neurol Sci. 1998;160(1):67–75. doi:10.1016/S0022-510X(98)00225-1
80. Tzeng NS, Chung CH, Yeh CB, et al. Are chronic periodontitis and gingivitis associated with dementia? A nationwide, retrospective, matched-cohort study in Taiwan. Neuroepidemiology. 2016;47(2):82–93. doi:10.1159/000449166
81. Tzeng NS, Chung CH, Lin FH, et al. Magnesium oxide use and reduced risk of dementia: a retrospective, nationwide cohort study in Taiwan. Curr Med Res Opin. 2018;34(1):163–169. doi:10.1080/03007995.2017.1385449
82. Yeh YH, Chou YJ, Huang N, Pu C, Chou P. The trends of utilization in traditional Chinese medicine in Taiwan from 2000 to 2010: a population-based study. Medicine. 2016;95(27):e4115. doi:10.1097/MD.0000000000004115
83. Shih CC, Huang LH, Lane HL, et al. Use of folk therapy in Taiwan: a nationwide cross-sectional survey of prevalence and associated factors. Evid Based Complement Alternat Med. 2015;2015:649265. doi:10.1155/2015/649265
84. Chen FP, Chen TJ, Kung YY, et al. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv Res. 2007;7(1):26. doi:10.1186/1472-6963-7-26
85. Hong EP, Park JW. Sample size and statistical power calculation in genetic association studies. Genomics Inform. 2012;10(2):117–122. doi:10.5808/GI.2012.10.2.117
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
