Back to Journals » Patient Preference and Adherence » Volume 17
Navigating the Challenges: Predictors of Non-Adherence to Psychotropic Medications Among Patients with Severe Mental Illnesses in Ethiopia
Authors Zeleke TK , Birhane W, Gubae K, Kebede B, Abebe RB
Received 17 June 2023
Accepted for publication 31 October 2023
Published 9 November 2023 Volume 2023:17 Pages 2877—2890
DOI https://doi.org/10.2147/PPA.S422659
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Tirsit Ketsela Zeleke,1 Worku Birhane,1 Kale Gubae,1 Bekalu Kebede,1 Rahel Belete Abebe2
1Department of Pharmacy, College of Medicine and Health Sciences, Debre Markos University, Debre Markos, Ethiopia; 2Department of Clinical Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Tirsit Ketsela Zeleke, Tel +251919187613, Email [email protected]; [email protected]
Background: Psychotropic medications, consisting of antidepressants, mood stabilizers, antipsychotics, and anxiolytics, are the pillars of managing mental illnesses. Since there is impairment in judgment, attitude, and stability in patients with severe mental conditions, they are vulnerable to non-adherence, which compromises treatment outcome. Nevertheless, a lack of studies investigating medication non-adherence and its predictors in severe mental illnesses patients in Ethiopia has been noticed. The purpose of this study was to evaluate the extent of non-adherence to psychotropic medication and its predictors in patients with severe mental illnesses in Ethiopia.
Patients and Methods: A cross-sectional study was carried out among severely ill mental patients attending outpatient psychiatry department at Debre Markos Comprehensive Specialized Hospital. Stratified sampling strategy was used to enroll patients with a variety of mental diseases. The determinants of non-adherence were identified using logistic regression analysis. Statistical significance was determined by a p-value of < 0.05 and a 95% confidence range.
Results: The prevalence of non-adherence to psychotropic medication was 50.9%. Missing regular follow-up [AOR (95% CI): 2.36 (1.24– 4.47)], current substance use [AOR (95% CI): 2.48 (1.44– 4.27)], negative attitude towards treatment [AOR (95% CI); 3.87 (2.26– 6.62)], experience of side effects [AOR (95% CI); 4.84 (2.74– 8.54)], medication use for more than 3 years [AOR (95% CI); 7.16 (3.93– 13.06)], and no family support [AOR (95% CI); 2.07 (1.19– 3.58)] were predictors of psychotropic medication non-adherence.
Conclusion: This study generalized that most of the patients were non-adherent to their medications. Missing regular follow-up, current substance use, negative attitude towards treatment, experience of side effects, Medication use for more than 3 years and absence of family support were found to influence medication adherence of the patients. In order to correct patients’, caregivers’, and societal misconceptions regarding the significance of treatment adherence, we recommend the need to implement psycho-educational programs.
Keywords: severe mental illness, psychotropic medication, non-adherence, Ethiopia
Introduction
Severe mental illnesses (SMIs) have been defined by a chronic and occasionally variable disorders along with consequential impairment of daily activities.1,2 Psychotropic medications, consisting of psycho stimulants, antidepressants, mood stabilizers, antipsychotics, and anxiolytics, are the pillars in the management of these SMIs.3,4 The effective management of people with SMIs requires a complete approach that helps to control their symptoms.5 According to the World Health Organization medication adherence is the degree to which a person follows the generally recognized recommendations of a healthcare professional by following a diet, taking prescription medication, and/or making lifestyle modifications.6,7 Since there is impairment in judgment, attitude, and stability in patients with SMIs, they are vulnerable to non-adherence.8–11 Previous studies have also shown that disruptions in reward processing and motivation-related brain circuits may lead to reduced motivation to adhere to medication regimens; therefore, impairments in executive functions, such as working memory and cognitive control, as well as neural substrate alterations, emotional dysregulation and altered stress response systems may hinder the ability of patients with SMIs to remember and follow prescribed medication schedules.12,13 Lack of adherence to treatment compromises effectiveness and It has detrimental effects on patients, their families, and society as a whole.14 In addition worsening symptoms, frequently causing increased chances of relapse, poor prognosis, high costs, and higher hospitalization resulting in a significant cost burden on the healthcare.15,16 Moreover, non-adherence is a complex set of behaviors with both unintentional and intentional non-adherences that could affect psychiatric patients. Fortunately, non-adherence to medications is one of the primary preventable causes of relapses and treatment failures among psychiatric illnesses; for this reason, when assessing patients with serious mental health conditions, it is important to look into the potential causes of non-adherence.17–19 Previous studies on medication non-adherence and predicts, usually address a single diagnosis group. To the best of our knowledge, there are insufficient studies that compared patients with severe mental illness from various diagnosis groups in terms of medication non-adherence in Ethiopia. Hence, the purpose of this study is to explore the magnitude of non-adherence to psychotropic medication and its predictors among patients with severe mental illnesses in Ethiopia.
Methods and Materials
Study Setting
The study was done at Debre Markos Comprehensive Specialized Hospital (DMCSH) located in the northwestern part of Ethiopia, and in East Gojjam Zone, it serves as the sole comprehensive hospital. A distinct unit inside the hospital delivers mixed ambulatory and hospitalized psychiatric care.16
Study Period and Design
An institution-based, cross-sectional, study was conducted at DMCSH psychiatric outpatient department from September 25, 2022, to January 25, 2023.
Source and Study Population
The source population consisted of the patients who visited the DMCSH psychiatric outpatient unit for follow-up treatment, while the study population comprises all severely mentally ill patients who visited for follow-up care throughout the data collection period.
Eligibility Criteria
Patients who came to the psychiatric outpatient clinic for follow-up and were above the age of 18, patients with a diagnosis of severe mental illnesses, as evidenced by their medical records, and patients who had been calm and on psychotropic medications for at least 3 months were enrolled in the study. Patients with serious physical or health problems, as well as those who were unable to express themselves due to their disease, were not included in the study.
Study Variables
Non-adherence to psychotropic medication was a dependent variable. Whereas independent variables included sociodemographic characteristics such as age, sex, residence, religion, educational background, and occupation, clinical- and medication-related variables including presence of comorbid conditions, diagnosis, duration of illness, number of inpatient admission, frequency and type of medications prescribed, lifestyle and socio-behavioral-related characteristics including attitude towards treatment, regular follow-up, current substance use, stigma, family support, and social support.
Operational Definitions
Severe mental illnesses: is defined as mental illness with the diagnosis of major depressive disorder, schizophrenia, Bipolar disorders, and anxiety.1
Psychotropic medication: is defined as medication consisting of antidepressants, anxiolytics, antipsychotics, psycho stimulants, and/or mood stabilizers.3
Sample Size Determination
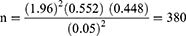
A single population proportion formula was used to estimate the sample size: considering the assumptions of a 95% confidence interval, the prevalence of non-adherence in a previous study at Felege Hiwot Hospital was 55.2% (0.552).20 The desired margin of error of 5% is calculated as follows:
Lastly, we add a 10% non-response rate which made our final sample size to be 418.
Sampling Technique
The stratified sampling method was applied. Based on the four diagnoses, schizophrenia, generalized anxiety disorder, bipolar disorder, and major depressive disorder, proportional allocation was carried out. Based on the number of patients under each stratum, the samples to be studied were determined by the proportional allocation method. Likewise, the number of patients from each diagnosis under the stratum was determined by proportional allocation. Finally, the study participants from each stratum were selected by systematic random sampling method. The sampling interval was determined by dividing the total population who had follow-up during the data collection period in psychiatry outpatient department divided by the sample size by using the formula k=N/n (where K is sampling frame, N is total population units and n is sample size). Then, the data collectors collected data from every fourth interval of patients. The first patient was selected by lottery method.
Data Collection Procedure
Data were collected using a pre-tested data-abstracting checklist that was designed by the authors after reviewing different literature and modified to correspond to local circumstances.1,20–23 The checklist included four sections that contained patient socio-demographic characteristics, medication and clinical-related variables, lifestyle and socio-behavioral-related variables, and self-reported adherence to medication characteristics. The patient’s sociodemographic characteristics were obtained by asking them while the number, type, and frequency of psychotropic medications, clinical parameters such as diagnosis, presence of comorbid conditions taken from the patient’s medical chart. Three psychiatry nurses participated in the data collection process. The principal and co-investigators provided supervision during the data collection period. Family support and social support were assessed by evaluating the presence of encouraging patients to take medications properly, treatment follow-up, reassurance or listening to the patient talk about his/ her illness, and financial by their family and or society.24,25 Attending regular follow-up appointments which are arranged by the hospital at set intervals were also assessed.26 Patient attitude towards medication were assessed by using drug attitude inventory scale which contains 10 true/false items. A correct response got a score of +1, whereas an incorrect response got a score of −1. The total of the pluses and minuses determines the drug attitude inventory score. A positive overall score denotes a positive attitude toward the course of treatment, and a negative total score, a negative attitude.27 Finally, medication non-adherence was assessed using the four-item version of the Morisky Medication Adherence Rating Scale.28 The Morisky scale rates a patient’s carelessness and forgetfulness about taking medications, discontinuing medication when feeling better, and stopping medication when they are feel worse. Answers to questions got one point if they were “yes” and got zero points if they were “no”. Scores were added up to make a final score between 0 and 4. Patients must score 1 or below to be adherent, and a score of 2 or more is considered non-adherence.28–31
Data Quality Assurance
The questionnaire was initially created by the investigator in English, and then Amharic and English-speaking staff translated it both forward and backward to maintain uniformity. Based on the translation, the instrument needed to be modified. The study’s principal investigator provided supervisors and data collectors with training on the study’s goals, methodology, and ethical considerations. For the purpose of evaluating the questionnaire’s clarification and sociocultural appropriateness, a pretest was conducted at the comprehensive and specialized hospital of the University of Gondar among 21 patients with severe mental illness (5% of the overall sample size). Additionally, the investigator evaluated and verified the collected data for completeness and consistency, while the supervisors provided on-site supervision during the whole data collection period.
Data Processing and Analysis
The data were examined for accuracy and consistency, coded, and entered into Epi-data 4.6 before being exported to SPSS 26 for additional analysis. Percentages and frequencies were used in descriptive statistics for categorical variables. Bi-variable and multivariable logistic regressions were fitted to examine the impact of independent variables on medication non-adherence, with the Hosmer and Lemeshow test for goodness of fit being performed to assess the model fit of each variable employed in the logistic regression model. In order to account for confounder effects, variables with a p-value <0.2 in the bivariate analysis were moved to multiple logistic regression models. In the final model, variables with a p-value <0.05 were considered statistically associated. The adjusted odds ratio (AOR) was calculated and interpreted using a 95% confidence interval (CI). To further identify and prevent redundant factors that could have an impact on our estimate, the variance inflation factor (VIF) was used to analyze the multicollinearity of the explanatory variables. The VIF fell within a reasonable range (1–5).32 The study’s findings were then presented utilizing texts, tables, and figures depending on the findings.
Ethical Considerations
Ethical approval was received from the Research and Ethical Review Committee of DebreMarkos University College of Health Sciences, pharmacy department on September 13, 2022 (SN: DOP/204/01/22) and an official letter was submitted to Debre Markos Comprehensive Specialized Hospital, and respective official permission was obtained. Furthermore: The study was carried out in line with the Helsinki Declaration. All participants provided written informed consent; every technique was used in compliance with the rules and regulations. To safeguard the confidentiality of the responses, no personal identifier has been requested for on the questionnaire. Patients identified as non-adherent were counseled to take their medication as directed, and members of the family were given health information.
Result
Sociodemographic Characteristics of Study Participants
The current study recruited 407 participants in total, with a response rate of 97.4%. The majority of the respondents (40.0%) were within the range of 25–34 years; with a mean age of 34.7 (±11.2) years. Males made up over half of the participants [234 (57.5%)], and 223 (54.8%) participants were from urban areas, whereas most of the participant’s marital status was single [294 (72.2%)]. The majority of participants were followers of the Orthodox religion 237 (58.2%). Regarding education, more than a quarter (26.5%) of the participants had a higher education level, while more than one-third of them had no job (38.1%). In addition, 65.1% of the participants made less than 2500 Ethiopian Birr (ETB) per month (Table 1).
 |
Table 1 Frequency of Sociodemographic Characteristics in Patients with Severe Mental Illness at Outpatient Psychiatric Department of DMCSH, Amhara, Ethiopia |
Clinical- and Treatment-Related Characteristics of Study Participants
Regarding specific diagnoses, almost half of the participants (48.2%) had a diagnosis of schizophrenia. Additionally, the majority of participants (51.8%) had illnesses that lasted less than 3 years, while 36.1% of the patients had comorbid diseases. Most of the patients (48.2%) were prescribed with antipsychotics. Moreover, 42.8% of the patients had been taking their medications for a maximum of 6 months and 74% of the participants reported were missing their routine follow-up. Regarding attitude towards medication, 39.8% of the participants had negative attitude. Most of participants had no family support (62.2%) and social support ((65.4%), while stigma was faced by 23.6% of the participants (Table 2).
 |
Table 2 Frequency of Clinical- and Treatment-Related Characteristics of Patients with Mental Illness at Outpatient Psychiatric Department of DMCSH, Amhara, Ethiopia |
Concerning medication-related side effects, 40.3% of the total participants experienced one or more side effects, and 29.8% of the patients reported gastro-intestinal complaints (Figure 1).
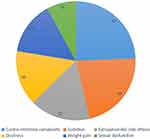 |
Figure 1 Frequency of perceived side effects among patients with severe mental illness at outpatient. Psychiatric department of DMCSH, Amhara, Ethiopia, 2023. |
Prevalence of Non-Adherence to Psychotropic Medications and Reasons for Non-Adherence
The prevalence of non-adherence to psychotropic medications was 50.9%. Common justifications for not being adherent mentioned by the respondents were the belief that medication was not helping in 51.6% of the patients and the shift to religion or traditional alternatives in 41.5% of the patients (Table 3).
 |
Table 3 Frequency of Reasons for Non-Adherence to Medication Among Patients with Severe Mental Illness at Outpatient Psychiatric Department of DMCSH, Amhara, Ethiopia |
Predictors for Non-Adherence to Psychotropic Medications
Multiple logistic regression analysis findings showed that experience of side effects, long duration of medication taking, lack of family support or encouragement, current substance use, attitude towards treatment, and irregular follow-up were predictors psychotropic medication non-adherence. Accordingly, patients who missed their regular follow-up had about twice the risk of non-adherence to psychotropic medications than those who had regular follow-up [AOR (95% CI): 2.36 (1.24–4.47)]. Patients who used substance had two times the likelihood of taking their medications as prescribed than those who did not [AOR (95% CI): 2.48 (1.44–4.27)]. Patients with a negative attitude regarding their treatment appeared 3.8 times more likely to exhibit medication non-adherence than those with a positive attitude [AOR (95% CI); 3.87 (2.26–6.62)]. Patients who had experienced side effect were five times the risk of non-adherence [AOR (95% CI); 4.84 (2.74–8.54)]. Moreover, patients who had been taking their medication for more than 3 years were prone to become non-adherent [AOR (95% CI); 7.16 (3.93–13.06)], whereas patients who had no family support or encouragement had a two-fold higher risk of being non-adherent compared to those with family support [AOR (95% CI); 2.07 (1.19–3.58)] (Table 4).
Discussion
The current study assessed the extent of non-adherence to psychotropic medication and its predictors in patients with severe mental illnesses. Based on the outcomes of the current study, there was an overall 50.9% non-adherence rate, which was consistent with rates of non-adherence worldwide, which were between 30% and 65%.33,34 Our result was less than study outcomes done in Jimma, Mekele, Egypt, Nigeria, India, Pakistan, and Bulgaria1,22,35–40 which was quite encouraging, but these differences might be because of the variation in socio-demography of the study population and, variation in tools used for assessing adherence. Likewise, differences in sample size, eligibility requirements, and methodological discrepancies could explain the disparity. As an example, a convenience sample method was employed in the Egypt study with a smaller sample size was taken. In studies done in Pakistan and Bulgaria, 128 and 226 psychiatric patients were enrolled, respectively, suggesting an explanation for the disparity that was noticed. However, a higher non-adherence was observed compared to studies conducted in the USA and Germany.41,42 This variance may be brought on by variations in healthcare environments or the degree of training in drug adherence that healthcare professionals have; hence, their care is crucial for drug compliance. The most frequent reasons reported for non-adherence were that medication was not helping and shift to religion or traditional options which was similar to the finding in Jimma and Pakistan.22,38 This might be due to inadequate communication between medical professionals and patients regarding their illness status, the delay in treatment response, the advantages of medications, and potential side effects, whereas feeling well and forgetting to take medication have been pointed out as causes in Canada and India.37,43 Medication-related side effects were also mentioned by patients as the reason for non-adherence. Notably, typical side effects experienced by patients were extrapyramidal complications, sedation, and gastrointestinal complaints.
Non-adherence to psychiatric treatment was significantly correlated with a variety of variables. The duration of medication taking, side effects experienced, missing regular follow-up, substance use, negative attitude towards treatment, and lack of family support or encouragement were predictors. In this study, participants undergoing inconsistent follow-up were more likely to have been non-adherent, which was similar to research from Jimma and Nigeria.22,44 Patients who attend regular follow-ups can be more informed about the advantages of drug compliance.45,46 Patients who had negative attitude towards treatment were at increased likelihood of non-adherence to medication. This outcome is also consistent with research done in Nigeria, the USA, and Germany.41,42,47 The presence of knowledge and positive attitude about the disease and towards its treatment, which is a key factor in drug adherence, may be one explanation for this. Due to the fact that adherence is positively correlated with health seeking, the relevance of any form of treatment for a patient is determined by their attitude.24,48
It was additionally determined that the absence of involvement from family members predicted failure to adhere to psychotropic medications. Research from the United States and Nigeria agreed up this finding.49–51 Patients with serious mental diseases quality of life suffered greatly by those who have not family support.52 This could be as a result of the family encouraging or serving as an alert for those who have mental illness to take their medication as prescribed. Furthermore, patients who used substances did not take their medications as prescribed, which is consistent with other studies.53–56 One explanation is that substance abuse can negatively affect a person’s internal environment, leading to greater mental disorders and unpleasant withdrawal effects.57 In addition to the immediate physical effects, substance use has a number of long-term social and therapeutic effects. These include a higher risk of social marginalization and homelessness, which can result in non-adherence to medicine.58,59 Moreover, patients who were on treatment for longer duration were more prone to be non-adherent, which is comparable with findings from studies conducted in Addis Ababa and Nigeria.1,56 Boredom, low motivation, and hopelessness due to a perceived lack of efficacy, might be present when patients take medications for an extended period of time. Concerning occurrence of side effects patients who experience side effect were more likely being non-adherent the possible explanation might be due to the fact that patients who encounter side effects tend to be less prone to be inspired to comply with such treatments and have a more unfavorable attitude toward medication.60,61 Moreover, prior studies show that increased medical costs as well as making SMIs to be managed and controlled in a less than optimal manner as potential consequences of non-adherence to psychotropic medication in Ethiopia.20,22,38,62 Based on the findings of the current study, we would like to recommend health care professionals and policymakers in Ethiopia to address the factors contributing to non-adherence in the country by using psycho-educational programs and to focus on the behavioral theory of adherence based on the operant conditioning such as reinforcement of action that leads to adherence.
Limitation
Self-report methods were used to measure the lack of medication adherence in this study, which has the tendency to understate drug non-adherence and poses concerns about the patient’s memory of events. Additionally, the degree of failure to adhere has not been taken into account in the study. This study’s cross-sectional design makes it impossible to pinpoint the precise cause.
Strength
Trained professionals collected the data, relevant language unit experts translated the questions, and when the outcome had been determined, non-adherent patients were provided with health education.
Conclusion
In accordance with the study’s findings, patients with severe mental illnesses had an elevated level of non-adherence. Therefore, we advocate psycho-educational initiatives that target patients’ and society’s beliefs with regard to the illness and its management. Furthermore, healthcare professionals should emphasize the need for substance abuse assessment for patients and offer quick encouragement for those who are in search of rehabilitation programs, which could boost adherence to medications.
Data Sharing Statement
There are all of the necessary data in the document. The corresponding author can provide you with additional data that has been used to support the results of the research on enquiry.
Acknowledgments
We want to forward our deepest appreciation to the data collectors and the employees of the psychiatric department for their efforts put forth in the completion of this study. Additionally, we would like to thank the study participants sincerely for their willing participation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ibrahim AW, Yahya S, Pindar SK, Wakil MA, Garkuwa A, Sale S. Prevalence and predictors of sub-optimal medication adherence among patients with severe mental illnesses in a tertiary psychiatric facility in Maiduguri, North-eastern Nigeria. Pan Afr Med J. 2015;21(1). doi:10.11604/pamj.2015.21.39.6664
2. Swartz JA, Jantz I. Association between nonspecific severe psychological distress as an indicator of serious mental illness and increasing levels of medical multimorbidity. Am J Public Health. 2014;104(12):2350–2358. doi:10.2105/AJPH.2014.302165
3. Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279(7):526–531. doi:10.1001/jama.279.7.526
4. George E, Engel L. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137(5):535–544.
5. Citrome L, Yeomans D. Do guidelines for severe mental illness promote physical health and well-being? J Psychopharmacol. 2005;19(6):102–109. doi:10.1177/0269881105059505
6. Saag KG, Bhatia S, Mugavero MJ, Singh JA. Taking an Interdisciplinary Approach to Understanding and Improving Medication Adherence. Springer; 2018:136–138.
7. Miller NH. Adherence behavior in the prevention and treatment of cardiovascular disease. J Cardiopulm Rehabil Prev. 2012;32(2):63–70. doi:10.1097/HCR.0b013e318235c729
8. Perlick D, Rosenheck R, Kaczynski R, Kosma L. Medication non-adherence in bipolar disorder: a patient-centered review of research findings. Clin Approach Bipolar Disorder. 2004;3:56–64.
9. Pomykacz B, Mao M, Weiss RD, Teter CJ. A review of brief medication-adherence instruments used in patients with schizophrenia and bipolar disorder. Harv Rev Psychiatry. 2007;15(5):259–263. doi:10.1080/10673220701650383
10. Mert DG, Turgut NH, Kelleci M, Semiz M. Perspectives on reasons of medication nonadherence in psychiatric patients. Patient Prefer Adherence. 2015:87–93. doi:10.2147/PPA.S75013
11. Maan C, Munnawar Hussain M, Heramani N, Lenin R. Factors affecting non-compliance among psychiatric patients in the Regional Institute of Medical Sciences, Imphal. IOSR J Pharm. 2015;5(1):1–5.
12. Tanaka M, Á S, Vécsei L, Giménez-Llort L. Emerging translational research in neurological and psychiatric diseases: from in vitro to in vivo models.
13. August SM. Medication Adherence Among the Elderly: A Test of the Effects of the Liberty 6000. technology: University of North Texas; 2005.
14. Sin J, Gamble C. Managing side‐effects to the optimum: valuing a client’s experience. J Psychiatr Ment Health Nurs. 2003;10(2):147–153. doi:10.1046/j.1365-2850.2003.00564.x
15. Crowe M, Wilson L, Inder M. Patients’ reports of the factors influencing medication adherence in bipolar disorder–an integrative review of the literature. Int J Nurs Stud. 2011;48(7):894–903. doi:10.1016/j.ijnurstu.2011.03.008
16. Amha H, Denekew B, Asnakew S. 2022. Depressive Symptoms and Associated Factors Among Adults Attending Antiretroviral Therapy Clinic in Debre Markos Comprehensive Specialized Hospital. Amhara, Ethiopia: SAGE Open Medicine, 10:20503121221100992.
17. Horne R, Weinman J, Barber N, et al. Concordance, adherence and compliance in medicine taking. London: NCCSDO. 2005;2005(40):6.
18. Chan AHY, Horne R, Hankins M, Chisari C. The medication adherence report scale: a measurement tool for eliciting patients’ reports of nonadherence. Br J Clin Pharmacol. 2020;86(7):1281–1288. doi:10.1111/bcp.14193
19. Weret ZS, Mukherjee R. Prevalence of relapse and associated factors in patient with schizophrenia at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: institution based cross sectional study. Int J Interdiscip Multidiscip Stud. 2014;2(1):184–192.
20. Gebeyehu DA, Mulat H, Bekana L, et al. Psychotropic medication non-adherence among patients with severe mental disorder attending at Bahir Dar FelegeHiwote Referral Hospital, north west Ethiopia, 2017. BMC Res Notes. 2019;12(1):1–6. doi:10.1186/s13104-019-4126-2
21. Tareke M, Tesfaye S, Amare D, Belete T, Abate A. Antipsychotic medication non-adherence among schizophrenia patients in Central Ethiopia. S Afr J Psychiatr. 2018;24. doi:10.4102/sajpsychiatry.v24i0.1124
22. Tesfay K, Girma E, Negash A, Tesfaye M, Dehning S. Medication non-adherence among adult psychiatric out-patients in Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop J Health Sci. 2013;23(3):227–236. doi:10.4314/ejhs.v23i3.5
23. Gudeta DB, Leta K, Alemu B, Kandula UR. Medication adherence and associated factors among psychiatry patients at Asella Referral and Teaching Hospital in Oromia, Ethiopia: institution based cross sectional study. PLoS One. 2023;18(4):e0283829. doi:10.1371/journal.pone.0283829
24. Kasahun AE, Sendekie AK, Mekonnen GA, Sema FD, Kemal LK, Abebe RB. Impact of personal, cultural and religious beliefs on medication adherence among patients with chronic diseases at university hospital in Northwest Ethiopia. Patient Prefer Adherence. 2022:1787–1803. doi:10.2147/PPA.S370178
25. Kamaryati NP, Malathum P. Family support: a concept analysis. Pac Rim Int J Nurs Res. 2020;24(3):403–411.
26. Pang A, Lum F, Ungvari G, Wong C, Leung Y. A prospective outcome study of patients missing regular psychiatric outpatient appointments. Soc Psychiatry Psychiatr Epidemiol. 1996;31(5):299–302. doi:10.1007/BF00787924
27. Hogan TP, Awad A, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13(1):177–183. doi:10.1017/S0033291700050182
28. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986:67–74.
29. Bates JA, Whitehead R, Bolge SC, Kim E. Correlates of medication adherence among patients with bipolar disorder: results of the bipolar evaluation of satisfaction and tolerability (BEST) study: a nationwide cross-sectional survey. Prim Care Companion CNS Disord. 2010;12(5):26157.
30. Vik SA, Maxwell CJ, Hogan DB, Patten SB, Johnson JA, Romonko-Slack L. Assessing medication adherence among older persons in community settings. J Popul Ther Clin Pharmacol. 2005;12(1).
31. Morisky DE, Ang A, Krousel‐Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–54. doi:10.1111/j.1751-7176.2008.07572.x
32. Daoud JI, editor. Multicollinearity and regression analysis.
33. Yang J, Y-H K, Paik J-W, et al. Symptom severity and attitudes toward medication: impacts on adherence in outpatients with schizophrenia. Schizophr Res. 2012;134(2–3):226–31. doi:10.1016/j.schres.2011.11.008
34. Kassis IT, Ghuloum S, Mousa H, Bener A. Treatment non-compliance of psychiatric patients and associated factors: are patients satisfied from their psychiatrist? Br J Med Med Res. 2014;4(2):785.
35. Amr M, El-Mogy A, El-Masry R. Adherence in Egyptian patients with schizophrenia: the role of insight, medication beliefs and spirituality. Arab JPsychiatr. 2013;24: 60–8.
36. Ibrahim A, Pindar S, Yerima M, et al. Medication-related factors of non adherence among patients with schizophrenia and bipolar disorder: outcome of a cross-sectional survey in Maiduguri, North-eastern Nigeria. J NeurosciBehav Health. 2015;7(5):31–39.
37. Roy R, Jahan M, Kumari S, Chakraborty P. Reasons for drug non-compliance of psychiatric patients: a centre based study. J Indian Acad Appl Psychol. 2005;31(1–2):24–28.
38. Taj F, Tanwir M, Aly Z, et al. Factors associated with non-adherence among psychiatric patients at a tertiary care hospital, Karachi, Pakistan: a questionnaire based cross-sectional study. J Pak Med Assoc. 2008;58(8):432.
39. Vassileva I, Milanova V, Asan T. Predictors of medication non-adherence in Bulgarian outpatients with schizophrenia. Community Ment Health J. 2014;50(7):854–861. doi:10.1007/s10597-014-9697-8
40. Eticha T, Teklu A, Ali D, Solomon G, Alemayehu A, Laks J. Factors associated with medication adherence among patients with schizophrenia in Mekelle, Northern Ethiopia. PLoS One. 2015;10(3):e0120560. doi:10.1371/journal.pone.0120560
41. Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness; 2009.
42. Rummel-Kluge C, Schuster T, Peters S, Kissling W. Partial compliance with antipsychotic medication is common in patients with schizophrenia. Aust N Z J Psychiatry. 2008;42(5):382–388. doi:10.1080/00048670801961107
43. Lacro JP, Dunn LB, Dolder CR, Jeste DV, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):15489. doi:10.4088/JCP.v63n1007
44. Adeponle AB, Thombs BD, Adelekan ML, Kirmayer LJ. Family participation in treatment, post-discharge appointment and medication adherence at a Nigerian psychiatric hospital. Br J Psychiatry. 2009;194(1):86–87. doi:10.1192/bjp.bp.108.052217
45. Berk L, Hallam KT, Colom F, et al. Enhancing medication adherence in patients with bipolar disorder. Hum Psychopharmacol Clin Exp. 2010;25(1):1–16. doi:10.1002/hup.1081
46. Biadgilign S, Deribew A, Amberbir A, Deribe K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: a qualitative study. SAHARA J Soc Asp HIV/AIDS. 2009;6(4):148–154. doi:10.1080/17290376.2009.9724943
47. Chukwujekwu CD, Adesokun OK. Prevalence of medication non-adherence among psychiatric patients in a tertiary hospital in Nigeria. J Biosci. 2017;5(04):1. doi:10.4236/jbm.2017.54001
48. Sluijs EM, Kok GJ, Van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;73(11):771–782. doi:10.1093/ptj/73.11.771
49. Adewuya AO, Owoeye OA, Erinfolami AR, et al. Prevalence and correlates of poor medication adherence amongst psychiatric outpatients in southwestern Nigeria. Gen Hosp Psychiatry. 2009;31(2):167–174. doi:10.1016/j.genhosppsych.2008.12.005
50. Thrush CR, Han X, Pyne JM, Thapa P, Sullivan G. A pilot study of barriers to medication adherence in schizophrenia. J Clin Psychiatry. 2004;65(2):211–216. doi:10.4088/JCP.v65n0211
51. Wilk JE, West JC, Marcus SC, Countis L, Regier DA, Olfson M. Family contact and the management of medication non-adherence in schizophrenia. Community Ment Health J. 2008;44(5):377–380. doi:10.1007/s10597-008-9139-6
52. Corrigan PW, River LP, Lundin RK, et al. Three strategies for changing attributions about severe mental illness. Schizophr Bull. 2001;27(2):187–195. doi:10.1093/oxfordjournals.schbul.a006865
53. Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3(4):200–218. doi:10.1177/2045125312474019
54. Teferra S, Hanlon C, Beyero T, Jacobsson L, Shibre T. Perspectives on reasons for non-adherence to medication in persons with schizophrenia in Ethiopia: a qualitative study of patients, caregivers and health workers. BMC Psychiatry. 2013;13(1):1–9. doi:10.1186/1471-244X-13-168
55. Misdrahi D, Petit M, Blanc O, Bayle F, Llorca P-M. The influence of therapeutic alliance and insight on medication adherence in schizophrenia. Nord J Psychiatry. 2012;66(1):49–54. doi:10.3109/08039488.2011.598556
56. Girma S, Abdisa E, Fikadu T. Prevalence of antipsychotic drug non adherence and associated factors among patients with schizophrenia attending at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: institutional based cross sectional study. Health Sci J. 2017;11(4). doi:10.21767/1791-809X.1000520
57. Janssen B, Gaebel W, Haerter M, Komaharadi F, Lindel B, Weinmann S. Evaluation of factors influencing medication compliance in inpatient treatment of psychotic disorders. Psychopharmacology. 2006;187(2):229–236. doi:10.1007/s00213-006-0413-4
58. de Bragança FC. Treatment in Schizophrenia: Factors for Adherence; 2020.
59. Digaffe T, Weldegebreal F, Motuma A 10 assessment of level of adherence and its risk factors to anti-tuberculosis treatment among tuberculosis patients in selected public health facilities, Harar Town, Eastern Ethiopia.
60. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415–422. doi:10.1016/j.eurpsy.2004.06.031
61. DiBonaventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry. 2012;12(1):1–7. doi:10.1186/1471-244X-12-20
62. Kaplan RM, Sallis JF, Patterson TL. Health and Human Behavior. Mcgraw-Hill Book Company; 1993.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.