Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Nasal Prongs: Risks, Injuries Incidence and Preventive Approaches Associated with Their Use in Newborns
Authors Ribeiro DFC , Barros FS , Fernandes BL , Nakato AM , Nohama P
Received 1 March 2020
Accepted for publication 14 May 2020
Published 19 June 2020 Volume 2020:13 Pages 527—537
DOI https://doi.org/10.2147/JMDH.S252017
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Débora de Fátima Camillo Ribeiro,1– 3 Frieda Saicla Barros,2 Beatriz Luci Fernandes,3 Adriane Muller Nakato,3 Percy Nohama2,3
1Neonatal Services, Waldemar Monastier Hospital, Campo Largo, Paraná, Brazil; 2Graduate Program on Biomedical Engineering, Universidade Tecnológica Federal do Paraná, Curitiba, Paraná, Brazil; 3Graduate Program on Health Technology, Pontifícia Universidade Católica do Paraná, Curitiba, Paraná, Brazil
Correspondence: Percy Nohama
Graduate Program on Health Technology, Pontifícia Universidade Católica do Paraná, Rua Imaculada Conceição 1155, Curitiba, Paraná CEP 80215-901, Brazil
Tel +55 41 3271-1357
Email [email protected]
Purpose: To assess the incidence of nasal injury in newborns submitted to non-invasive ventilation (NIV) via binasal prongs, to identify risks that come with using this interface, and to present actions for nasal injury prevention.
Patients and Methods: Observational and descriptive study performed in neonatal intensive care unit (NICU) of a public hospital in the south of Brazil. This research was divided into three stages. In the first one, nasal injury incidence was assessed in 148 newborns, using data collection from medical records. In the second stage, injury incidence, severity and a preliminary analysis of risks associated with the prescription of binasal prongs were analyzed in 33 newborns who required NIV. In the third stage. recommendations were presented to prevent nasal injury during NIV with short binasal prong.
Results: The incidence of nasal injury in the first stage was 37.16%, and 63.64% in the second one. As for severity, 68.42% of the injuries showed Stage I severity, and 31.58% Stage II. The main risks associated with the use of binasal prongs were inappropriate prong size, inappropriate prong model, interface reuse, prolonged NIV use exclusively with binasal prongs, incorrect prong position and NIV circuit pulled. A total of 17 preventive approaches were recommended: 13 related to newborns care and not dependent on prior investment. Among them: to choose appropriate prong size; to keep the prong and the NIV circuit well positioned and periodically massages with circular movements in the nasal septum and columella.
Conclusion: The inappropriate prong size, interface reuse, prong model, prolonged NIV use with binasal prong and incorrect prong and NIV circuit position may be associated with the high occurrence of injury in the NICU studied. Simple approaches concerning clinical staff care actions towards the newborn in NIV, which do not require a financial investment, can prevent nasal injury.
Keywords: neonatal intensive care units, non-invasive ventilation, prevention, risk factors, wound and injuries
Introduction
The non-invasive ventilation (NIV) provides ventilatory support without artificial airways such as endotracheal tube or tracheostomy.1 In neonatology, binasal prong is the most frequently interface used at neonatal intensive care units (NICUs) because it is easy to use, has a lower cost and is less invasive. Also, it provides relatively constant pressure allowing good access to the patient.2,3 Furthermore, binasal prong offers less flow resistance to the airflow and are effective in preventing reintubation.4
Despite all the advantages mentioned above, the nasal prongs can cause nasal injury, an adverse event that is increasingly present in NICUs.5 The nasal injury is a consequence of the pressure and friction caused by the prongs on the columella and the nasal septum, thus reducing local blood circulation, with consequent tissue perfusion and ischemia.6,7
Nasal injuries are initially characterized by hyperemia (stage I), but may evolve to superficial ulceration (stage II), and necrosis and total nasal tissue loss (stage III).8 They can limit the use of NIV in newborns (NBs) who need this ventilatory support and may be the cause of septicemia.9 The nasal injury may be a source of discomfort for patients.8,9 Since it is painful, it leads to crying episodes, increasing blood pressure and intracranial pressure, which may increase the risk of interventricular hemorrhage and, consequently, affects the motor development of the NBs.10
Given the adverse consequences that nasal injury may cause, and because nasal injury is an avoidable problem most of the time, prevention is deemed fundamental. To prevent injuries, it is necessary to identify the individuals who are at a greater risk of developing injuries and triggering factors.11 In this way, identifying and characterizing the problem leads to preventive measures.
The prevention of nasal injury is the best strategy for NBs submitted to NIV. Injury can be prevented employing an adequately sized interface, changing between prongs and masks, and using nasal protection and Velcro to keep the prongs properly positioned.12,13
Considering this scenario, the objectives of the present study were: to assess the incidence of nasal injury in NBs submitted to NIV with the use of short binasal prongs; to identify risks due to the use of this interface, and; to indicate procedures aimed to prevent nasal injury at the NICU studied herein.
Materials and Methods
We carried out an observational study in the NICU of Waldemar Monastier Children’s Hospital [Hospital Infantil Waldemar Monastier] (HIWM), located in the metropolitan area of Curitiba, Paraná, Brazil.
Waldemar Monastier Hospital’s NICU is equipped with 20 beds and its healthcare service is provided through the Brazilian Unified Health System (SUS), uniquely to NBs aged from 0 to 28 days, that come from all of Paraná State - Brazil, through the hospital’s beds center. The NBs assisted are premature babies ranging from extreme to late preterm, full-term and post-term NBs, with or without the necessity of invasive or non-invasive ventilatory support.
We conducted the research in three stages according to its three main goals.
First Stage
In the first stage, the incidence of nasal injury was assessed in 148 NBs who required NIV with binasal prongs between January 2013 to December 2014.
We collected data from the GSUS’ Health Care Management System involved in electronic medical records and developments reported by health professionals. We considered the following information: gender, gestational age, birth weight and total NIV use time.
In addition to these elements, we consulted the developments reported by physicians, nurses, and physiotherapists for notifications on nasal injury and information about the need for NIV suspension due to the observed injury.
Data were arranged in a Microsoft Office Excel spreadsheet and underwent statistical analysis. For quantitative variables, we determined means and standard deviations, and for nominal variables, absolute and percentage frequencies.
We excluded newborns who presented extreme length of permanence in NIV. To do so, we considered those with values above the 3rd quartile plus three times the interquartile range as outliers. Fisher’s exact test (for nominal variables) and the Mann–Whitney test (for ordinal or non-normal quantitative variables) were applied to assess differences between NBs with and without nasal injury. We analyzed the normality of the quantitative variables with the Shapiro–Wilk test. For variables of interest, we estimated the relative risk from its Odd Ratio and confidence interval (95% CI).
Statistical analyses were performed using the statistical package GraphPad PRISM with the level of significance set at 5% (α = 0.05).
Second Stage
In the second stage, the incidence and severity of the nasal injury were assessed in 33 NBs who needed NIV with short binasal prongs between January 2015 to April 2016 and possible risks associated with the use of short binasal prongs were identified from daily clinical nasal evaluations.
Newborns of both genders were part of this stage, with no distinctions for ethnicity, class, or social group, with the gestational age of fewer than 38 weeks, subjected to NIV with binasal prongs as initial ventilatory support or as weaning, for a minimum of 24 hours.
The NBs received NIV using Inter® Neo mechanical ventilators. The interfaces used were short binasal prongs from three different brands (A, B, and C), either new or sterilized, selected according to the availability of the material at the time of NIV implementation.
We had applied an assessment protocol to all NBs, consisting of a collection of neonatal data and visual inspection. Neonatal data collected were: gender, gestational age, birth weight, and time of permanence in NIV.
In the clinical inspection, we had verified the presence of cutaneous alterations in the nostrils, and we had categorized the injuries according to the classification proposed by Fischer et al:8 Stage I - intact skin with unbleached erythema; Stage II - partial loss of dermis thickness, evidenced as a superficial wound with a crustless red bed; and Stage III - necrosis and total tissue loss.
Such assessments were performed before NIV implementation, and every 24 hours until the medical suspension of that support, always by the same assessor. We recorded the stage of the nasal injury daily.
Neonatal data and assessment results on the nasal injury stage were tabulated and underwent statistical analysis. We evaluated the quantitative variables through means and standard deviations, and the nominal ones (categorical) through absolute and percentage frequencies.
The possible risks associated with the use of short binasal prongs were identified through unsystematic observations of the neonatal intensive care provided to the 33 NBs that needed NIV. This evaluation was performed by a physiotherapist specialized in intensive care, that before each daily nasal evaluation, checked for possible risks that could be associated with nasal injury in the NICU studied. This professional has previously worked in assessment and reduction of nasal injury in newborns in other investigations. From the survey of possible risks associated to nasal injury, the team achieved an analysis of these risks, looking for correlating the risks with their possible causes, effects, severity categories and procedures to minimize them.
Third Stage
In the third stage, through the improvements studied on the risk analysis stage, this research team proposed preventive actions to minimize the risks and consequently to reduce nasal injury in the NBs treated in the NICU studied. However, it was not the scope of the study described in this article to check if the proposed recommendations effectively have reduced the nasal injuries in this NICU. These preventive actions were based on the NICU’s physiotherapy team experience, and in the risk reducing strategies studied and described in the literature.
Results
First Stage
During the study period, 369 NBs were admitted to HIWM’s NICU. Of those, 158 needed non-invasive ventilatory support (NIV). We excluded 10 NBs from the total that used NIV since they presented extreme values as to the length of permanence under this ventilatory support.
Concerning the 148 NBs who had used NIV, 63 (42.57%) were girls, and 85 were boys (57.43%). The mean gestational age was 34.27 ± 4.60 weeks, and their mean birth weight was 2212.49g ± 937.54g. The length in this ventilatory support was 104h ± 108 hours. Fifty-five NBs (37.16%) developed nasal injury while using non-invasive ventilatory support.
Table 1 displays the characteristics of NBs with and without nasal injury who used NIV during the study period.
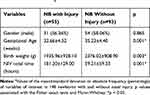 |
Table 1 Characteristics of Newborns with and Without Nasal Injuries That Used NIVa |
Logistic regression showed that the relative risk for nasal injury development increased significantly when gestational age was lower than 37 weeks (2.50 OR; 95% CI: 1.21–5.13) and decreased significantly when birth weight was greater than 2500 g (0.19 OR; 95% CI: 0.06 −0.53).
Due to the severity of the injury, the ventilatory support was suspended in 9 NBs who presented a nasal injury. Of those, six were subjected to oxygen therapy using an oxygen hood, one was reintubated, and two NBs had alternating periods of NIV and hood to reduce said injury.
Second Stage
During the assessment period of the second stage, 210 NBs were admitted to HIWM’s NICU. Of those, 83 required NIV. Among the newborns who had used NIV, 49 were born with a gestational age of fewer than 38 weeks. Of those, we excluded 16 from the study for not meeting the inclusion criteria.
Of the 33 NBs who participated in this study, 18 (54.55%) were girls, and 15 (45.55%) were boys. The mean gestational age was 32.03 ± 3.93 weeks, and the mean birth weight reached 1760.00 g ± 818.86 g. The mean time of permanence in NIV was 91h ± 72h. We found that 21 NBs (63.64%) developed nasal injury while using non-invasive ventilatory support.
Table 2 presents the frequency and severity of the nasal injury of the 33 studied NBs regarding gestational age, birth weight, and NIV time.
 |
Table 2 Frequency and Severity Nasal Injury in the Evaluated Newborns in the Second Stage of This Study |
Table 3 presents the preliminary risk analysis. We were able to relate six of them to the use of prongs that may result in nasal injury. For each risk factor, we suggested its respective causes, effects, the category of severity, and improvements.
 |
Table 3 Preliminary Risk Analysis of the Prong Use in the Newborn |
Figure 1 shows the use of inappropriate binasal prong size in a neonate. It is possible to visualize the compression that this material causes on the newborn skin. Also, it shows the newborn submitted to NIV through a reused but sterilized short binasal prong. It is possible observe that the prong is inappropriately sized, since the insertion catheters are small and clamp the nasal septum. Besides, the reused prong does not adapt properly in the circuit connectors, hampering the correct prong positioning. Due to connection difficulties, the healthcare staff uses adhesive tape to keep the circuit connected. The prong used in the newborn has straight line insertion catheters, and it is not anatomical, making it even harder for proper prong positioning.
 |
Figure 1 Photo of a newborn submitted to NIV through a used but sterilized short binasal prong. Note: Consent to use the image was obtained by the newborn’s caretaker. |
Figure 2 shows 17 nasal injury preventive actions proposed to the NICU studied, based on the improvements found on the preliminary risk analysis. We have indicated 17 preventive actions for reducing the risks associated to nasal injury according to the NICU studied. Thirteen of them do not require financial investments, for instance: it is possible to prevent nasal injuries by changing how the procedures are performed regardless of NICU’s financial conditions.
 |
Figure 2 The preventive approaches for nasal injury. |
The recommendations were divided into three stages: pre-implementation of NIV, during the implementation of NIV, and during permanence in NIV.
NIV Pre-Installation Recommendations
Adequate prong size prevents injury.5,6,14-19 Thus, choosing prong size according to the NB’s body weight is recommended. If the service has a specific device that correlates nostril dimensions and prong size, it should be used in the selecting process. In both selection forms, it is necessary to follow the instructions of the manufacturer.
The correct size of the cap used to attach the NIV circuit also contributes to minimizing the occurrence of nasal injury.12–14,17 In this way, is important to select the cap size according to the manufacturer’s recommendations. If the service does not have a cap, it is necessary to make a handmade tubular-knit cap that fits the NB’s cephalic dimensions to attach the NIV circuit and fix it with an elastic band and safety pin or with Velcro.
Recommendations During NIV Implementation
During NIV implementation, it is necessary to make sure that the chosen prong is the appropriate one for the NB in treatment. It should be emphasized that sometimes the prong will not adapt to the NB’s anatomical characteristics, and it is necessary to choose the best size that fits the NB’s anatomy, that is, without pinching the septum or causes blanching.
The recommendation involves the lubrication of the prong with water or saline solution before insertion of the catheters into the nostrils to facilitate insertion and minimize the risk of trauma to the nasal mucosa.13,15,17,19
To fix the NIV circuit it is necessary to use Velcro or safety pins and rubber band on both sides of the tubing cap.19,20
Velcro around the prong and on the upper lip is also recommended to keep the prong well positioned. To prevent damaging the upper lip, it is necessary to use hydrocolloids under the Velcro. Also, two professionals must perform the procedure to ensure that the device is correctly positioned and to facilitate the adaptation of the NB to the NIV, making this procedure less traumatic.13
Recommendations During Permanence in NIV
During the entire period of permanence in NIV, it is necessary to monitor the positioning of the prong, NIV circuit, and the NB.
The prong should stay at least 2 mm away from the nasal columella.13 The trachea circuit should not be pulled.17 The NB should be comfortably positioned, as to allow natural movements.13
During the implementation and permanence of the NB in NIV, it is essential to ensure the correct humidification and gas temperature of 37ºC,20 because non-humidification and incorrect temperature may dry out the mucosa and cause nasal injury.18
Regular inspection of the integrity of the nasal septum and constant inspection of the positioning of the prong can prevent the occurrence of nasal damages.13 The inspection of the integrity of the nasal septum should be performed at each work shift, and inspection of the position should be checked every hour.16
If the NB remains agitated during the application of NIV, comfort maneuvers such as non-nutritive suction and restraint is recommended13,21 to reduce the friction between the prong and the nose.
During the permanence of the NB in NIV, massages with circular movements in the nasal septum and columella every 3 hours is indicated to increase skin perfusion, thus preventing nasal injury.12,13,22
All these actions depend on the training and commitment of the professionals involved in supportive care. Training and collective involvement in optimizing NIV use is key to provide the best performance of the ventilatory support.23 Constant awareness and training programs on the proper care for NBs using NIV with nasal prong are important in preventing or minimizing the occurrence of nasal injury.
Discussion
The incidence of nasal injury in the first stage was 37.16% and, in the second one, 63.64%. In the first stage, we assessed the injury incidence retrospectively using developments reported by physicians, nurses, and physiotherapists. During that period, daily evaluations of the nasal septum in NBs subjected to NIV are not routine in the studied NICU; for this reason, some NBs may have developed nasal injury without notification by the medical staff.
When assessed prospectively, incidence reached a rate of over 60%. These findings are similar to those of other studies,6,22,23 which assessed similar incidence. Regular evaluation of the nasal septum allows for accurate knowledge about the occurrence of nasal injury, indicates the importance of developing preventive actions, and acts as a feedback to verify whether these actions are indeed effective in preventing nasal injury. Additionally, in the case of injury, it is possible to assess the injury stage, thus guiding therapeutic actions.
In stage I, it was possible to identify which NBs were at greater risk for developing injuries and triggering factors, which are important aspects to develop preventive procedures. We observed that preterm NBs with low birth weight and NBs who stay for long periods under NIV have a high susceptibility to nasal injury, as reported in the literature.6,8,22
Preterm and low-birth-weight NBs are prone to develop nasal injury due to the immaturity of their integumentary system.24 They have a poorly developed epidermal barrier, which leads to injury when the skin is compressed.25
In this stage, we could not assess the severity of the injury, since the reports of the clinical staff did not present a description of the injuries’ stages. In the second stage, when the nasal injury was daily evaluated, we found that 71.43% of nasal injuries were in stage I severity and 28.57% in stage II. None were in stage III.
All NBs evaluated in the first stage had used hydrocolloid as nasal protection. In the second stage, the NBs used hydrocolloid or silicone gel nasal protection on their nasal base. This practice could have contributed to the prevention of severe injury stages. Nasal protections reduce the friction between the prong surface and the newborn’s skin.13,26 In other studies6,22,23 in which nasal protections were used during permanence in NIV stage I and II injuries were observed in larger proportions than stage III injury, the latter being of minimal incidence.
In the second stage of the present study we presented a preliminary analysis of risks associated with the use of nasal prongs. Possible risks are: inappropriate prong size, prong reuse, prolonged NIV use exclusively with binasal prong, incorrect prong positioning, NIV circuit traction, and prong model.
The prong size for each NB is selected based on body weight at the time of NIV implementation.15 However, in clinical practice, the relationship between prong size and body weight does not always guarantee that the NB will receive a prong of appropriate size.
Some manufacturers offer NIV circuit devices that measure nostrils’ size and indicate their respective prong sizes.13 However, this practice is not common in the studied NICU since prongs are chosen based on the NB’s body weight, on the availability of the material at the time of NIV implementation, and the clinical staff’s common sense.
In the NICU studied, it is the physiotherapist who evaluates if the prong’s size used on the NB is appropriate or inappropriate. Prong’s size is considered inappropriate to the NB when it forces the septum, and when a bigger prong is selected, the insertion catheter does not fit in the nostrils; in other words, when available sizes do not satisfy the NB anatomical characteristics.
Small-caliber prongs, when inserted in the NB, can move inside the nostrils and, due to friction, can cause injury.17 Prongs with a caliber greater than the diameter of the NB’s nostrils may enlarge and damage them with the increased pressure on the nasal mucosa.9
The pressure yielded by NIV interface, besides causing nasal injury, can provoke edema, facial and cephalic deformity.13 Pandita et al27 reported three cases of idiopathic unilateral facial nerve palsies in NBs associated to the pressure caused by the NIV interface. They found that NIV interfaces that compress the facial nerve near the exit from the stylomastoid foramen results in facial palsy.
Regarding the reused prong, the continuous sterilization process causes degradation on the plastic material, turning the device rigid, increasing the risk of a nasal injury.17 Nasal prongs are manufactured to be disposable, but their reuse has been observed in the practice of Brazilian NICUs.6 For economic reasons, on the studied NICU, prongs are reused. However, attempting to reduce costs by using reprocessed materials is a mistake. In addition to cause adverse sequelae in the NB,8,28 the nasal injury may extend the length of hospitalization29 due to the need for antibiotic therapy as a result of the infection caused by nasal wound or reintubation.
The longer the length in NIV, the higher the risk of developing skin damage.6,8,22 Studies28,30 have proved that switching between interfaces decrease the incidence of nasal injury. In this study’s NICU, there are no switches because they only offer short binasal prongs.
Concerning the improper prong positioning and the pulling force of the NIV circuit, both increase the pressure on nasal structures, reduce local blood flow, and may result in nasal damage. Moreover, inappropriate prong and incorrect NIV circuit positioning may cause discomfort in the NB.13 The painful episodes provoke negative effects on the sleep and wakefulness state, increasing agitation of the NB that, in turn, increases the prong movement, intensifying the risk of lesions caused by friction.18
In the NICU studied, the NIV circuit is fixed in NBs through tubular mesh caps with adhesive taps. According to Nascimento et al,17 large caps in relation to the newborns’ heads cause mobility of the tracheas and contribute to increase the pressure or friction of the prongs on the nasal region. Very small caps can put pressure on the cephalic region and cause pain and positional plagiocephaly.13
In the third stage, we introduce a flowchart with 17 preventive procedures for nasal injury. Thirteen of them are related to care actions towards newborns and do not require investments for their application, namely: appropriate prong size,5,6,13-19 and correct prong positioning;13,14,18,22 proper NIV circuit placement;5,6,13,17 suitable NB positioning,13,14,17,19,23 and appropriate cap size;12–14,17 adequate heated and humidified gas flow;13,17,18,20 regular clinical evaluation of the nasal septum;12,13,15,16,18,26 regular inspection of the NB and the NIV circuit;5,13,22,23,31 prong lubrication before insertion into the NB;13,15,17,19 regular massage of the nasal septum;12,13,22 training and commitment of the care team;5,13,17,23 comfort actions for agitated NBs;5,13 and four-hand care.13
The other preventive procedures, namely single-use prong, use of Velcro, nasal protection and switching interfaces demand financial resources and require the team to be aware that the healing of the injuries is more expensive than its prevention.
The switching between prongs and masks every 4 to 6 hours helps to avoid excessive pressure on nasal structures and allows the blood flow’s return to the pressed areas, thus preventing the development of nasal damages.28,30
The use of Velcro to attach the prong is encouraged in NBs as it helps to keep the prong properly positioned, preventing pressure on the septum.12,13,15,20 Also, it prevents excessive prong motion, reducing friction on the nasal septum.
Such procedures can be introduced into care protocols for NBs that require NIV and must be disseminated to clinical staff through training and updating courses, to improve the assistance provided to these NBs and prevent nasal injury in NICUs.
This study’s strength is its data survey in real environment, showing the reality of a Brazilian NICU about the incidence and nasal injury severity in NBs submitted to NIV with short binasal prong. At first, it may seem that the recommendations indicated to prevent nasal injuries are exclusive to the NICU studied, since they were based on the risk analysis for Waldemar Monastier Children’s Hospital. However, the findings can be generalized because the consulted literature indicates, in part, similar recommendations to treat these kind of nasal injury risks in other parts of the world.
The major limitation of this study was the small sample size. Even so, it was possible to verify the occurrence and severity by means of periodic assessment of the nasal septum and inventory of the associated injury risks in the researched NICU.
Other limitation refers to inventorying the related risks of nasal injury development. The risks were determined by only one professional and lack of a healthcare team to monitor risks full time or video strategies that could record the NB during NIV permanence. The considered risks during daily assessment of the nasal septum were specific for the study’s scenario, which is not a multicenter research yet. Although each NICU has its particularities in terms of NIV using, the data provided may help other similar NICUs to the comprehension about the related nasal injury causes and which actions could be adopted to prevent nasal injury.
This study was limited to evaluate the incidence and severity of the nasal injury, and the risks associated to its occurrence. It has also presented specific preventive actions, which were based on the risk analysis of the studied NICU and on the consulted literature.
Using these data, we may implement recommendations as preventive approaches in the NICU studied and in other NICUs. In the future, it is intended to turn this into a multicenter study.
Conclusion
The incidence of injury in NBs subjected to NIV with binasal prongs was high in this study.
Gestational age, birth weight, and length in NIV are risk factors for the development of nasal injuries in NBs who required non-invasive ventilatory support with the use of binasal prongs.
The risks associated with the use of binasal prongs in NICU studied were: inappropriate prong size, prong reuse, prolonged NIV use exclusively with nasal prongs, incorrect positioning, NIV circuit pulling force, and prong model.
Through the preliminary risk analysis, it was possible to indicate preventive actions to nasal injury for the NICU. Altogether 17 recommendations were presented, 13 of them do not require investments to be implemented, in other words, it is possible to prevent the nasal injury regardless of the NICUs financial conditions.
The results of this study may help other similar NICUs to the comprehension about the risks associated to nasal injury and which actions could be adopted to reduce them and prevent nasal injury.
Abbreviations
NB, newborn; NICU, neonatal intensive care unit; NIV, non-invasive ventilation.
Ethics Approval and Informed Consent
The development of this study complied with national and international requirements that conduct ethics in research involving human beings and it is accordance with the Declaration of Helsinki, having been approved by the Ethics Committee on Research Involving Human Beings of the Universidade Tecnológica Federal do Paraná - UTFPR (CEP/CONEP), under Protocol number 42,718,915.4.0000.5547. The parents of the newborns were informed about the study and provided written informed consent.
Acknowledgments
We thank Fundação Araucária, Secretaria de Estado da Ciência, Tecnologia e Ensino Superior do Paraná (SETI), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and the Waldemar Monastier Children’s Hospital directy for allowing the study to be performed on the NICU’s premises.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Morley SL. Non-invasive ventilation in paediatric critical care. Paediatr Respir Rev. 2016;20:24–31. doi:10.1016/j.prrv.2016.03.001
2. Greenough A, Lingam I. Invasive and non-invasive ventilation for prematurely born infants - current practice in neonatal ventilation. Expert Rev Respir Med. 2016;10(2):185–192. doi:10.1586/17476348.2016.1135741
3. Gupta N, Saini SS, Murki S, Kumar P, Deorari A. Continuous positive airway pressure in preterm neonates: an update of current evidence and implications for developing countries. Indian Pediatr. 2015;52(4):319–328. doi:10.1007/s13312-015-0632-z
4. De Paoli AG, Davis PG, Faber B, Morley CJ. Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev. 2008;(1):CD002977.
5. McCoskey L. Nursing care guidelines for prevention of nasal breakdown in neonates receiving nasal CPAP. Adv Neonatal Care. 2008;8(2):116–124. doi:10.1097/01.ANC.0000317260.99072.ae
6. Bonfim SFSF, Vasconcelos MGL, Sousa NFC, Silva DVC, Leal LP. Nasal septum injury in preterm infants using nasal prongs. Rev Lat Am Enfermagem. 2014;22(5):826–833. doi:10.1590/0104-1169.3451.2486
7. Visscher MO, Adam R, Brink S, Odio M. Newborn infant skin: physiology, development, and care. Clin Dermatol. 2015;33(3):271–280. doi:10.1016/j.clindermatol.2014.12.003
8. Fischer C, Bertelle V, Hohlfeld J, Forcada-Guex M, Stadelmann-Diaw C, Tolsa JF. Nasal trauma due to continuous positive airway pressure in neonates. Arch Dis Child Fetal Neonatal Ed. 2010;95(6):F447–451. doi:10.1136/adc.2009.179416
9. Imbulana DI, Manley BJ, Dawson JA, Davis PG, Owen LS. Nasal injury in preterm infants receiving non-invasive respiratory support: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2018;103(1):F29–F35. doi:10.1136/archdischild-2017-313418
10. Bouza H. The impact of pain in the immature brain. J Matern Fetal Neonatal Med. 2009;22(9):722–732. doi:10.3109/14767050902926962
11. Coyer F, Tayyib N. Risk factors for pressure injury development in critically ill patients in the intensive care unit: a systematic review protocol. Syst Rev. 2017;6(1):1–6. doi:10.1186/s13643-017-0451-5
12. Alessi S. Evidence regarding the use of bubble continuous positive airway pressure in the extremely low birth-weight infant: benefits, challenges, and implications for nursing practice. Adv Neonatal Care. 2018;18(3):199–207. doi:10.1097/ANC.0000000000000509
13. Squires AJ, Hyndman M. Prevention of nasal injuries secondary to NCPAP application in the ELBW infant. Neonatal Netw. 2009;28(1):13–27. doi:10.1891/0730-0832.28.1.13
14. Casey JL, Newberry D, Jnah A. Early bubble continuous positive airway pressure: investigating interprofessional best practices for the NICU team. Neonatal Netw. 2016;35(3):125–134. doi:10.1891/0730-0832.35.3.125
15. Chen C-Y, Chou A-K, Chen Y-L, Chou H-C, Tsao P-N, Hsieh W-S. Quality improvement of nasal continuous positive airway pressure therapy in neonatal intensive care unit. Pediatr Neonatol. 2017;58(3):229–235. doi:10.1016/j.pedneo.2016.04.005
16. Milligan PS, Goldstein MR. Implementation of an evidence-based non-invasive respiratory support (NIRS) bundle in the NICU to decrease nasal injury complications. J Neonatal Nurs. 2017;23(2):89–98. doi:10.1016/j.jnn.2016.05.003
17. Nascimento RM, Ferreira ALC, Coutinho ACFP, Veríssimo RCSS. The frequency of nasal injury in newborns due to the use of continuous positive airway pressure with prongs. Rev Lat Am Enfermagem. 2009;17(4):489–494. doi:10.1590/S0104-11692009000400009
18. Rego MA, Martinez FE. Clinical and laboratorial repercussions of the nasal CPAP in preterm newborns. J Pediatr (Rio J). 2000;76(5):339–348. doi:10.2223/jped.125
19. Sahni R, Schiaratura M, Polin RA. Strategies for the prevention of continuous positive airway pressure failure. Semin Fetal Neonatal Med. 2016;21(3):196–203. doi:10.1016/j.siny.2016.02.008
20. Bonner KM, Mainous RO. The nursing care of the infant receiving bubble CPAP therapy. Adv Neonatal Care. 2008;8(2):78–95. doi:10.1097/01.ANC.0000317256.76201.72
21. Mangat AK, Oei JL, Chen K, Quah-Smith I, Schmolzer GM. A review of non-pharmacological treatments for pain management in newborn infants. Children. 2018;5(10):1–12.
22. Sousa NFC, Bonfim SFSF, Vasconcelos MGL, Bezerra JLO, Silva DVC, Leal LP. Prevalence of nasal septum injury in premature infants using nasal prongs. Rev Esc Enferm USP. 2013;47(6):1285–1290. doi:10.1590/S0080-623420130000600005
23. Ota NT, Davidson J, Guinsburg R. Early nasal injury resulting from the use of nasal prongs in preterm infants with very low birth weight: a pilot study. Rev Bras Ter Intensiva. 2013;25(3):245–250. doi:10.5935/0103-507X.20130042
24. Robertson NJ, McCarthy LS, Hamilton PA, Moss AL. Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 1996;75(3):F209–212. doi:10.1136/fn.75.3.F209
25. Fox MD. Wound care in the neonatal intensive care unit. Neonatal Netw. 2011;30(5):291–303. doi:10.1891/0730-0832.30.5.291
26. Gunlemez A, Isken T, Gokalp AS, Turker G, Arisoy EA. Effect of silicon gel sheeting in nasal injury associated with nasal CPAP in preterm infants. Indian Pediatr. 2010;47(3):265–267. doi:10.1007/s13312-010-0047-9
27. Pandita A, Mishra N, Gupta G, Shukla A. Neonatal facial palsy, a case series: is CPAP the culprit? BMJ Case Rep. 2018;
28. Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child Fetal Neonatal Ed. 2005;90(6):F480–483. doi:10.1136/adc.2004.069351
29. Galetto SGS, Nascimento ERP, Hermida PMV, Malfussi LBH. Medical device-related pressure injuries: an integrative literature review. Rev Bras Enferm. 2019;72(2):505–512. doi:10.1590/0034-7167-2018-0530
30. Newnam KM, McGrath JM, Salyer J, Estes T, Jallo N, Bass WT. A comparative effectiveness study of continuous positive airway pressure-related skin breakdown when using different nasal interfaces in the extremely low birth weight neonate. Appl Nurs Res. 2015;28(1):36–41. doi:10.1016/j.apnr.2014.05.005
31. Davis PG, Morley CJ, Owen LS. Non-invasive respiratory support of preterm neonates with respiratory distress: continuous positive airway pressure and nasal intermittent positive pressure ventilation. Semin Fetal Neonatal Med. 2009;14(1):14–20. doi:10.1016/j.siny.2008.08.003
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
