Back to Journals » Patient Preference and Adherence » Volume 10
Naltrexone HCI/bupropion HCI for chronic weight management in obese adults: patient selection and perspectives
Authors Cenk Tek C
Received 5 October 2015
Accepted for publication 29 February 2016
Published 4 May 2016 Volume 2016:10 Pages 751—759
DOI https://doi.org/10.2147/PPA.S84778
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Cenk Tek
Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA
Abstract: Naltrexone, an opiate antagonist, and bupropion, a noradrenergic/dopaminergic antidepressant, have many effects on the reward systems of the brain. These medications impact eating behavior, presumably via their impact on food reward. However, only bupropion induces weight loss in obese individuals, while naltrexone does not have any appreciable effect. The combination of 32 mg of naltrexone and 360 mg of bupropion in a sustained-release combination pill form has been recently approved for obesity treatment. Studies have shown that the combination of these two medications is more effective in inducing weight loss, when combined with lifestyle intervention and calorie reduction, than each individual medicine alone. The naltrexone–bupropion combination, when combined with lifestyle intervention and modest calorie reduction, seems to be quite effective for 6-month and 1-year outcomes for clinically significant weight loss (over 5% of total body weight). These medications are not devoid of serious side effects, however, and careful patient selection can reduce dramatic complications and increase positive outcomes. This paper reviews existing weight loss clinical trials with bupropion and the bupropion–naltrexone combination. Additionally, the rationale for the suggested patient selection and clinical strategies for special patient populations are discussed.
Keywords: naltrexone, bupropion, obesity treatment, lifestyle intervention, calorie reduction
Introduction
Obesity is a disease that is characterized by excess body fat that results from an energy imbalance resulting from excess consumption of calories relative to energy expenditure of the body. Obesity is strongly associated with increased mortality and morbidity in combination with a host of other diseases, primarily diabetes and cardiovascular disease.1,2 Rates of both obesity and these associated diseases are increasing around the world, which has since led to the recognition of obesity as a disease rather than an expression of a normal human condition.
Treatment of obesity is, naturally, weight loss. This enables the body to expend energy stores, namely, the adipose tissue in the human body. To lose weight, patients, simply put, need to decrease their calorie intake and increase their energy consumption through expanded physical activity. Various forms of extreme calorie reduction and extreme exercising have been found to be very effective. The problem is that very few obese/overweight people can adequately follow these diets and exercise routines, and even fewer people can sustain them over long periods of time. Thus, extreme dieting and exercise are efficacious in study conditions, but are not necessarily effective in practice or at the population level.
Research has shown that lifestyle interventions that prescribe moderate calorie restriction (typically 500 calories per day) and behavior change, which promotes small changes in daily life, lead to a moderate increase in activity and a moderate decrease in the consumption of unnecessary calories.3 Both of these strategies appear efficacious in research conditions and are additionally effective at the clinic and population level, as exemplified in many commercialized weight-loss programs.3 Behavior change focuses on cognition and behavior regarding eating and movement, such as portion control, control of nonhunger eating, sedentary life, increasing daily activities, etc. Most people can join these courses in clinics or commercial programs in their communities and successfully lose weight. However, some individuals are unable to participate in lifestyle interventions due to financial, motivational, or other reasons. Also, a high proportion of people who can manage to lose weight through lifestyle interventions eventually revert back to old behaviors once the intervention is over and, ultimately, regain the weight.4 Since obesity affects not only how one thinks about food and activity, but also the brain physiology that is connected to energy regulation, pharmacological support for lifestyle interventions may be useful. For this particular reason, many pharmacological agents have been developed or repurposed. These medications are mostly psychoactive substances that directly target various receptors in the brain and aim at helping with appetite control and maintaining participation in lifestyle programs. This paper centers on the recently approved, repurposed medication combination of naltrexone and bupropion, with a focus on specific patient populations and correct patient selection to maximize the utility of this promising pharmacological intervention.
Naltrexone
Naltrexone is an antagonist of μ, δ, and κ opiate receptors, although its actions are most pronounced on μ opiate receptors.5 It does not have any other known actions in the brain. It is available in a 50 mg generic oral preparation and a 380 mg brand-name depot injectable form. The oral form is approved by the US Food and Drug Administration (FDA) for alcohol dependence and is shown to decrease cravings for alcohol. The injectable form is approved for alcohol dependence as well as opiate addiction. In both forms it completely blocks opiate receptors, which may cause dramatic opiate withdrawal in ongoing opiate users, while also completely negating both euphoric and therapeutic antinociceptive effects of opioids for nonusers. The oral form is well studied and has been widely used in clinics for over 2 decades; it is inexpensive and very well tolerated.
Naltrexone may also affect food intake through various mechanisms.6 Its nonspecific blockade of opiate receptors also blocks endogenous opioid (ie, endorphin) action. First, craving is a form of anticipatory reward which is regulated through endogenous opioid and mesolimbic dopaminergic systems. Naltrexone attenuation of alcohol craving may be explained by its blockade of anticipatory reward, and so it could be hypothesized that it would reduce food cravings, which induce nonhunger eating. Second, food intake is a very rewarding process in itself. Food consumption is pleasurable, since it induces endorphin release, which is in relative proportion to fat and sugar content of the consumed food. Thus, naltrexone blocks the rewarding aspects of the food and is shown to decrease food consumption in rodents.7 Finally, hypothalamic pro-opiomelanocortin (POMC) cells are important in appetite regulation since they send a “stop-eating” signal to the brain by secreting melanocyte-stimulating hormone (MSH). MSH is cosecreted with β endorphin, which does not have any effect on appetite but provides a feedback inhibition to POMC cells. Since naltrexone blocks this feedback inhibition, it could provide continued MSH release, resulting in appetite reduction.8 While all of these have the making of an excellent obesity medication, surprisingly, studies of naltrexone as a weight loss agent in normal obese patients are uniformly negative.9,10
Bupropion
Bupropion is a well-studied antidepressant which has been widely used for over 25 years. It is marketed in various generic oral doses in immediate-release, sustained-release, and extended-release formulations. It is inexpensive and generally well tolerated when attention is paid to its side effects and precautions. Bupropion inhibits dopamine and noradrenalin reuptake, thus, increasing the level of these neurotransmitters in the synapse. It is also a nicotine antagonist and is approved for smoking cessation. Its major side effects include seizures, tachycardia, glaucoma, increased blood pressure, rash, and in rare cases, Stevens–Johnson syndrome, anxiety/agitation, and in even rarer cases, psychosis. Like other antidepressants, it carries a warning for increased suicidal ideation. It increases blood levels of a range of medications through its inhibition of hepatic P450 cytochrome 2D6 enzyme. This list includes antidepressants, antipsychotics, β-blockers, and tamoxifen. It also interacts with monoamine oxidase (MAO) inhibitors to create a potentially fatal reaction. Monoamine oxidase inhibiting antidepressants are not currently widely used, but weaker inhibitors, such as the antibiotic linezolid and the antituberculosis agent isoniazid, still have the potential to create the interaction.11,12
Bupropion is chemically related to amphetamines. All amphetamines and their congeners reduce appetite. The mechanism is not clear, however, it is possibly related to their action in central noradrenergic and dopaminergic systems, which may impact the food reward. They may possibly have direct effect on the appetite regulation in hypothalamus, but this action is not well described. Amphetamine congeners phentermine and diethylpropion are approved for obesity treatment and are quite effective.13,14 Bupropion, similar to its chemical cousins and unlike naltrexone, does have a weight loss effect, although it is thought to be weaker than phentermine and diethylpropion. For obese patients who are given lifestyle intervention and caloric restriction, the clinically significant weight loss (defined as 5% of total body weight [TBW]) is roughly twice the rate of placebo.10,15,16 Summary findings are presented in a “number needed to treat” (NNT) format in Figures 1 and 2 for easy comparison. NNT is a summary statistic that denotes the number of patients needed to be treated to get one positive clinically significant outcome compared to placebo.17 Lower numbers correlate with better outcomes and most effective medications in medicine have an NNT between 2 and 4.
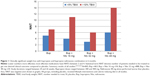  | Figure 1 Clinically significant weight loss with bupropion and bupropion naltrexone combination in 6 months. |
  | Figure 2 Clinically significant weight loss with bupropion and bupropion naltrexone combination in 1 year. |
Naltrexone bupropion combination
The naltrexone–bupropion combination pill was recently approved for obesity treatment in the USA and Europe. This is a sustained-release combination of 8 mg of naltrexone and 90 mg bupropion. At this time, the recommended dose is a total of 32 mg naltrexone and 360 mg bupropion. The manufacturer has evaluated various doses of naltrexone combined with fixed doses of bupropion and found that 32 mg of naltrexone is the optimum dose.10,18 The mechanism of action is thought to be through a combination of both medications’ action on food reward. The medications, in this instance, appear to have a synergistic effect by providing more weight loss than each medication alone. Studies showed a yearly weight loss of nearly 8% TBW with the combination medication in combination with lifestyle intervention and a 500-calorie reduction compared to approximately 1.5% TBW lost in the placebo arm.19 When intensive lifestyle intervention is applied, the weight loss approaches 11% TBW compared to about 7% with placebo.20 Diabetic patients appear to lose less weight with the combo drug, about 6% versus 2% with placebo.21 It is not clear why diabetic patients lose less weight with the drug. In a previous study, we also have found naltrexone not to be very efficacious in a group of antipsychotic-using obese patients as opposed to nondiabetic patients, thus, this area requires further study.22 Results of the studies with different combinations of the two drugs are presented in an easy-to-compare NNT format in Figures 1 and 2.
There are several caveats with the naltrexone–bupropion combination studies. First, all of the studies are sponsored by the manufacturer of the combination pill. They are, nevertheless, well-conducted studies by experienced investigators. Confirmation studies by independent funding do not exist as of this point. Second, these are all efficacy studies that are conducted under careful experimental conditions with carefully selected ideal patients. Effectiveness studies, which would demonstrate real-life performance of the drug, have not been done to date. It is possible that study performance may not reflect real-life results. Third, most study reports have been analyzed by utilizing last observation carried forward strategy. Weight loss studies typically have high dropout rates; in the naltrexone–bupropion studies this was as high as about half of the subjects. Subjects who dropped out may or may not maintain the results that are recorded at the dropout point. The last observation carried forward strategy typically favors the intervention versus the control. Finally, perhaps since the US Food and Drugs Administration requires this for approval of obesity drugs, all studies include a prescription of calorie reduction and lifestyle change recommendations. This limits the result interpretation to the motivated patients and gives us little information on how the drug will perform without diet/lifestyle change. Bupropion by itself for example, induces much more weight loss in obesity treatment studies compared to analysis in depression studies, where weight loss is not the primary aim.23 Thus, results presented in Figures 1 and 2 should be interpreted by clinicians with these caveats in mind.
Use and dosage
The naltrexone–bupropion combination pill is marketed in a sustained-release tablet consisting of 8 mg of naltrexone and 90 mg of bupropion. Due to seizure and elevated blood pressure risk with sudden increase in bupropion, the manufacturer recommends starting with one tablet a day and gradually increasing over a period of 1 month to 2 tablets twice daily.24 During the studies, the drug was well tolerated, and the most frequent reported side effect was nausea, which is not surprising as this is the most common side effect for both drugs separately. Nausea is usually time-limited with both drugs and is more pronounced in the beginning of the therapy. Other side effects observed appear to be generated mostly by the bupropion component and most importantly, although rare, seizures and myocardial infarction were observed.24
For budgetary or dosing flexibility purposes, similar dosing can be achieved by utilizing generic naltrexone and sustained-/extended-release bupropion tablets. In this case, it is possible to start the naltrexone at the targeted dose and gradually add and increase bupropion to the desired dose based on patient tolerability. It should be considered that both weight-loss effect and serious side effect risks of bupropion appear to be dose related.15
The aim of the treatment is clinically significant weight loss. This is by convention defined as 5% of TBW. This level of weight loss, although modest, is shown to improve medical outcomes if maintained in the long term. Naturally, as the weight loss increases, the morbidity decreases, as exemplified in bariatric surgery, which routinely provides a loss of 30% or more TBW.
Medication treatment with naltrexone–bupropion combination needs to be coupled with a lifestyle intervention and caloric restriction, to be successful. Lifestyle interventions are behavioral interventions that can be delivered in office, via group or individual format; alternately, patients can sign up for commercial programs or internet delivery. It appears the medication effect is more pronounced if the lifestyle program is more intensive.20 These programs prescribe easy-to-implement small changes to patient’s lifestyle, aimed at decreasing unnecessary caloric intake and increasing daily activities such as walking, climbing stairs, etc. It is possible to find manuals for these interventions on the internet or at bookstores, and, with some preparation, professionals with basic nutrition knowledge can deliver these. One example for such a manual, is a 16-week lifestyle program we have created and tested previously (Simplified Intervention to Modify Physical activity, Lifestyle, and Eating behavior – SIMPLE); this can be downloaded free of charge and has been effective for people with cognitive impairment, low education, and mental illness and can be used for a wide selection of patients (http://www.simpleprogram.org/home/manual). A diet and exercise program coupled with lifestyle intervention would be very useful, however, and, at the very least, a modest calorie reduction in the daily diet, such as 500 calories per day, should be prescribed. This can usually be achieved by eliminating or decreasing some empty calories that do not serve any purpose, such as sugary drinks, sweets, or chips. This medication combination without any lifestyle recommendations and calorie reduction has not been tested for obesity treatment. It should be noted that actimeter wristbands and smartphone-based activity and food diary apps are now widely available at a low cost and have great potential to improve weight loss outcomes.
Patient expectations
Patient expectations for weight loss are often unrealistic. Most people want to lose weight for cosmetic reasons and desire maximum weight loss in a minimal amount of time with the least effort necessary. Weight loss is difficult and often takes many attempts. Therefore, patient expectations need to be well managed. Medical indications for weight loss are primarily to prevent morbidity and mortality, to decrease the impact of already existing obesity-related illnesses such as high blood pressure and type 2 diabetes, and to increase quality of life. This can often be achieved by modest levels of weight loss, if the weight loss is sustained.25
Patient selection
Level of obesity for treatment
The naltrexone–bupropion combination is studied and approved for patients who have a body mass index (BMI) of 30 and over (obese), or people who have a BMI over 27 (overweight) and have one or more obesity-related conditions such as type 2 diabetes.18–20 It should be noted that BMI here is used as a proxy measure for adiposity. For muscular people, the BMI cutoffs should be adjusted up. Also, for people of Asian ethnic origin, BMI cutoffs should be lowered by 2 or 3 points.26,27 Furthermore, this writer is of the opinion that healthy overweight people with a BMI over 27 should be treated if their weight over the past few years has been consistently trending up.
The ideal patient
The ideal obese/overweight patient for naltrexone–bupropion supplementation of a behavioral and caloric program is relatively young, has no cardiac disease or seizure history, no eating disorders, is not yet diabetic, and has tried behavioral intervention and dieting in the past, but either could not achieve desired results or could not sustain their achieved weight loss. Since the indications are similar with bariatric surgery, medication treatment can be attempted as a last resort before surgery.28 For patients who have never tried behavioral intervention and dieting, an effort should be made first with these interventions before medication is started, since some people will never need the medication support.29
Special patient populations
The unwilling patient
A group of patients does exist that need to lose weight, have already high cardiac risk or obesity-related diseases, and are either not motivated to change their diet/lifestyle, or cannot comprehend the link between their obesity and medical problems. Some of these patients will refuse obesity interventions but may be willing to take a medication. Naltrexone–bupropion combination may not be appropriate for this group. Orlistat may be a better option, since it will block the absorption of the lipids at the intestinal level.30 Another strategy, albeit riskier from a cardiac and/or psychiatric stand point, is to utilize direct appetite-reducing medications. In this case, phentermine, diethylpropion, or topiramate may be better options.13,14,31 Amphetamine use, due to addictive properties, is not advisable.
Patients with diabetes
Individuals with either type 1 or 2 diabetes, but especially type 2, will benefit from weight reduction. The naltrexone–bupropion combination is shown to be effective in this population, but somewhat less so than in nondiabetics. Regardless, significant improvements in hemoglobin A1c levels were observed.21 Some diabetes medications are associated with some weight gain (eg, sulfonylureas) and others with modest (eg, metformin) or moderate (GLP-1 agonists) weight loss.32–34 Of the latter, the GLP-1 analog liraglutide has recently been approved for weight loss in diabetic patients.35–37 It makes sense to examine the diabetic obese patients’ medications first to see if a switch of the antidiabetic medication makes sense from a weight loss perspective. Another special point for this population is to be mindful for hypoglycemia resulting from weight loss by any treatment, including behavioral interventions.38
Hypertensive patients
Bupropion raises blood pressure, as does the naltrexone–bupropion combination.10,39 This increase sometimes may be offset by the reduction in blood pressure through weight loss; however, clinically significant weight loss will occur much later than the institution of full dose bupropion. Thus, blood pressure needs to be well-controlled before initiating therapy and should be monitored closely by the patient and the treating physician throughout the use of the combination.24
Patients with cardiac disease
During trials, myocardial infarction was observed.40 Bupropion has the potential to increase heart rate, which in turn may provoke arrhythmias.41 The naltrexone–bupropion combination should be used with great caution in this group of patients.
Patients with seizure history
Naltrexone–bupropion combination or bupropion alone should not be used in this group of people.24,42 If a seizure develops during treatment of a patient who did not experience prior seizures, treatment should be stopped immediately.24 Since bupropion lowers seizure thresholds, caution is required when it is used alongside other medications that lower seizure threshold.43 Similarly, caffeine intake should be reduced during treatment due to caffeine-induced decrease in seizure threshold.44,45
Smokers
Obese/overweight patients who smoke cigarettes present a unique challenge. From a cardiovascular risk reduction perspective, smoking needs to be targeted first. The 10-year cardiovascular risk is reduced by half following smoking cessation for an obese smoker.46 Nicotine has a unique effect on POMC cells and lowers appetite.47 Thus, smoking cessation is usually associated with weight gain. Bupropion is approved for smoking cessation, and naltrexone is shown to reduce the weight gain following smoking cessation.48 Thus naltrexone–bupropion combination is uniquely suitable for use in this population. Weight loss may be slightly less; however, in this situation, absence of weight gain and cessation of smoking are the desired results rather than clinically significant weight loss to reduce cardiovascular risk.49
Patients with hepatic disease
Naltrexone has the potential to cause drug-induced hepatic damage and frequently elevates hepatic transaminases, which may or may not be clinically significant.50 Patients with hepatic disease were excluded from the abovementioned studies, and similarly, we do not recommend use of naltrexone–bupropion combination in this patient population.
Patients with renal disease
Dose reductions are recommended in patients with renal disease, and it is not clear how this will affect the amount of weight loss achieved in this population.24
Patients with depression
Depression is highly comorbid with obesity and is universally undertreated.51 Bupropion is an excellent antidepressant, while naltrexone is not reported to have a mood effect. Thus, the naltrexone–bupropion combination, which includes an effective antidepressant dose of bupropion, may be the ideal weight loss drug for this population. Indeed, a recent pilot study had reported improvement in both depression and weight profile among obese/overweight and depressed patients.52 The usual caveats with antidepressant treatment continue to apply, including suicidal ideation and intent, which should be closely monitored. Furthermore, all antidepressants have the ability to induce mania, including in patients with previously unknown bipolar disease.53,54 It might be beneficial to collaborate with a psychiatrist in the care of such patients.
Patients with bipolar disorder
The naltrexone–bupropion combination should not be used in bipolar patients due to the risk of mania induction.54
Patients with psychosis
Most patients with schizophrenia are obese due to the appetite-increasing effects of antipsychotic medications.55 While bupropion and naltrexone separately have been used safely in schizophrenia patients, bupropion has a documented side effect of psychosis in nonpsychotic patients.22,56,57 For schizophrenia spectrum patients, we recommend expert consultation and care.
Patients with chronic pain
Naltrexone will induce opiate withdrawal in the setting of opiate analgesic use, a severe but nonfatal condition that still may require hospitalization.58 Chronic pain patients should be carefully screened for opiate pain medication use, prescribed or otherwise. If the patients are not on an opiate pain medication, the combination drug can be used with the caveat that it will block antinociceptive effects of opiates if they are required in future. The clearance of the sustained-release combination pill may take longer than immediate-release naltrexone in this case. Regardless, several weeks may be required after the cessation of the naltrexone–bupropion combination before starting an opiate pain medication.
Patients with substance and/or alcohol abuse
Substance abusing patients are clearly another unique challenge. Other than opiate abusers, there is no absolute contraindication. The naltrexone–bupropion combination could be beneficial as it decreases craving.59–63 Cocaine and bupropion have similar cardiovascular toxicity, and therefore should not be used together.64 Cannabis is an orexigenic substance and, as such, will counteract weight loss efforts. The author would urge caution and objective drug screening in this group of patients.
Patients who receive excessive calories from alcohol
All alcohol-containing drinks are very calorically dense. Social drinkers, who do not abuse alcohol but regardless consume large amounts on occasion, may not realize alcohol as a source of their obesity.65 The naltrexone–bupropion combination may actually be an ideal weight-loss drug for this population due to naltrexone’s anticraving effect.66 Alcohol education in this case should be incorporated into the lifestyle intervention.
Patients with eating disorders
There are several eating disorders, which are associated with obesity, predominantly bulimia nervosa, binge eating disorder, and sleep-related eating disorder.67–69 For these patients, we recommend expert care. The naltrexone–bupropion combination’s effects in eating disorders are not well known at this time. Bupropion alone is not effective for binge eating disorder.70
Patients with anxiety
The naltrexone–bupropion combination may cause anxiety and agitation.24 Caution is required in this patient population.
Patients with insomnia
Insomnia is highly prevalent and is associated with obesity.71 Additionally, sleep apnea is associated with obesity.72 The daytime aftereffects of inadequate sleep, such as lack of energy, may cause patients to overeat. It might also interfere with their participation in lifestyle weight interventions. Sleep apnea is a condition with high morbidity and mortality, and thus, clearly needs to be screened for and treated. In addition, insomnia is a potential side effect of the bupropion–naltrexone combination.52 For these patients, we would recommend resolving the sleep problem by behavioral and/or pharmacological interventions and then attempting nonpharmaceutical weight-loss strategies again. If these options fail, then the naltrexone–bupropion combination may be supplemented to the weight loss effort.
Patients who are scheduled for bariatric surgery
When all else fails, there is still bariatric surgery, which is very effective in producing lasting weight loss.73 Over the years, bariatric surgery techniques have developed to the point that it has become safer. If a patient decides to go the bariatric surgery route, it should be remembered that the naltrexone–bupropion combination should be discontinued several weeks before any type of surgery is performed, as opiate use may be necessary postsurgery for pain control.
Conclusion
The naltrexone–bupropion combination is a relatively safe and effective adjunct to lifestyle interventions and diet for the treatment of obesity. Both medications have been used for other purposes for over 2 decades, and so their side effect profiles are well known. Their weight-reducing effect is shown to be more pronounced together than with each individual medication on its own, and this effect is sustained over 1 year. With some care to appropriate patient selection and with adequate knowledge of side effects and potential complications, the naltrexone–bupropion combination can be an effective tool for treatment of the obese patient.
Acknowledgment
The author thanks Ms Erin Sullivan and Ms Katherine Lucas for editorial assistance.
Funding
This research was supported by grant number 1R01 DK093924 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the U.S. National Institutes of Health (NIH).
Disclosure
The author reports no conflicts of interest in this work.
References
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–1200. | ||
Flegal KM, Kalantar-Zadeh K. Overweight, mortality and survival. Obesity (Silver Spring). 2013;21(9):1744–1745. | ||
Wadden T, Butryn M, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132(6):2226–2238. | ||
Kraschnewski JL, Boan J, Esposito J, et al. Long-term weight loss maintenance in the United States. Int J Obes (Lond). 2010;34(11):1644–1654. | ||
Froehlich J, O’Malley S, Hyytia P, Davidson D, Farren C. Preclinical and clinical studies on naltrexone: what have they taught each other? Alcohol Clin Exp Res. 2003;27(3):533–539. | ||
Bodnar RJ. Endogenous opioids and feeding behavior: a 30-year historical perspective. Peptides. 2004;25(4):697–725. | ||
Levine AS, Billington CJ. Opioids as agents of reward-related feeding: a consideration of the evidence. Physiol Behav. 2004;82(1):57–61. | ||
Greenway FL, Whitehouse MJ, Guttadauria M, et al. Rational design of a combination medication for the treatment of obesity. Obesity (Silver Spring). 2009;17(1):30–39. | ||
Atkinson RL, Berke LK, Drake CR, Bibbs ML, Williams FL, Kaiser DL. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38(4):419–422. | ||
Greenway FL, Dunayevich E, Tollefson G, et al. Comparison of combined bupropion and naltrexone therapy for obesity with monotherapy and placebo. J Clin Endocrinol Metab. 2009;94(12):4898–4906. | ||
Lawrence KR, Adra M, Gillman PK. Serotonin toxicity associated with the use of linezolid: a review of postmarketing data. Clin Infect Dis. 2006;42(11):1578–1583. | ||
DiMartini A. Isoniazid, tricyclics and the “cheese reaction”. Int Clin Psychopharmacol. 1995;10(3):197–198. | ||
Cercato C, Roizenblatt VA, Leanca CC, et al. A randomized double-blind placebo-controlled study of the long-term efficacy and safety of diethylpropion in the treatment of obese subjects. Int J Obes (Lond). 2009;33(8):857–865. | ||
Langlois KJ, Forbes JA, Bell GW, Grant GF Jr. A double-blind clinical evaluation of the safety and efficacy of phentermine hydrochloride (Fastin) in the treatment of exogenous obesity. Curr Ther Res Clin Exp. 1974;16(4):289–296. | ||
Anderson JW, Greenway FL, Fujioka K, Gadde KM, McKenney J, O’Neil PM. Bupropion SR enhances weight loss: a 48-week double-blind, placebo-controlled trial. Obes Res. 2002;10(7):633–641. | ||
Jain AK, Kaplan RA, Gadde KM, et al. Bupropion SR vs placebo for weight loss in obese patients with depressive symptoms. Obes Res. 2002;10(10):1049–1056. | ||
Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ. 1995;310(6977):452–454. | ||
Apovian CM, Aronne L, Rubino D, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring). 2013;21(5):935–943. | ||
Greenway FL, Fujioka K, Plodkowski RA, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376(9741):595–605. | ||
Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity (Silver Spring). 2011;19(1):110–120. | ||
Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36(12):4022–4029. | ||
Tek C, Ratliff J, Reutenauer E, Ganguli R, O’Malley SS. A randomized, double-blind, placebo-controlled pilot study of naltrexone to counteract antipsychotic-associated weight gain: proof of concept. J Clin Psychopharmacol. 2014;34(5):608–612. | ||
Croft H, Houser TL, Jamerson BD, et al. Effect on body weight of bupropion sustained-release in patients with major depression treated for 52 weeks. Clin Ther. 2002;24(4):662–672. | ||
Contrave®[prescription information]. Deerfield, IL: Takeda Pharmaceuticals America I; 2014. Available from: http://general.takedapharm.com/content/file.aspx?filetypecode=CONTRAVEPI&CountryCode=US&LanguageCode=EN&cacheRandomizer=cecb72e0-e3b9-44c7-80a1-3534965d5e61. Accessed February 2, 2016. | ||
Wadden TA, Stunkard AJ. Handbook of Obesity Treatment. New York, NY: Guilford Press; 2002. | ||
Hsu WC, Araneta MR, Kanaya AM, Chiang JL, Fujimoto W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care. 2015;38(1):150–158. | ||
Shiwaku K, Anuurad E, Enkhmaa B, Kitajima K, Yamane Y. Appropriate BMI for Asian populations. Lancet. 2004;363(9414):1077. | ||
Zundel N, Ikramuddin S, Rosenthal R. Optimizing outcomes in bariatric surgery: a primer in patient selection. J Obes. 2012;2012:837216. | ||
Behary P, Cegla J, Tan TM, Bloom SR. Obesity: lifestyle management, bariatric surgery, drugs, and the therapeutic exploitation of gut hormones. Postgrad Med. 2015;127(5):494–502. | ||
McClendon KS, Riche DM, Uwaifo GI. Orlistat: current status in clinical therapeutics. Expert Opin Drug Saf. 2009;8(6):727–744. | ||
Sweeting AN, Tabet E, Caterson ID, Markovic TP. Management of obesity and cardiometabolic risk – role of phentermine/extended release topiramate. Diabetes Metab Syndr Obes. 2014;7:35–44. | ||
Zhong X, Zhang T, Liu Y, et al. Effects of three injectable antidiabetic agents on glycaemic control, weight change and drop-out in type 2 diabetes suboptimally controlled with metformin and/or a sulfonylurea: a network meta-analysis. Diabetes Res Clin Pract. 2015;109(3):451–460. | ||
Campbell IW. Comparing the actions of older and newer therapies on body weight: to what extent should these effects guide the selection of antidiabetic therapy? Int J Clin Pract. 2010;64(6):791–801. | ||
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. | ||
Astrup A, Carraro R, Finer N, et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond). 2012;36(6):843–854. | ||
Tsai AG. Randomised controlled trial: liraglutide for weight loss: more research is needed. Evid Based Med. 2010;15(2):46–47. | ||
Marre M, Shaw J, Brandle M, et al. Liraglutide, a once-daily human GLP-1 analogue, added to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight control compared with adding rosiglitazone or placebo in subjects with type 2 diabetes (LEAD-1 SU). Diabet Med. 2009;26(3):268–278. | ||
Prelipcean MS, O’Neil PJ, Bell DS. Hyperinsulinemic hypoglycemia precipitated by weight loss. South Med J. 2005;98(7):726–728. | ||
Thase ME, Haight BR, Johnson MC, et al. A randomized, double-blind, placebo-controlled study of the effect of sustained-release bupropion on blood pressure in individuals with mild untreated hypertension. J Clin Psychopharmacol. 2008;28(3):302–307. | ||
Patterson RN, Herity NA. Acute myocardial infarction following bupropion (Zyban). QJM. 2002;95(1):58–59. | ||
Caillier B, Pilote S, Castonguay A, et al. QRS widening and QT prolongation under bupropion: a unique cardiac electrophysiological profile. Fundam Clin Pharmacol. 2012;26(5):599–608. | ||
Tripp AC. Bupropion, a brief history of seizure risk. Gen Hosp Psychiatry. 2010;32(2):216–217. | ||
Johnston JA, Lineberry CG, Ascher JA, et al. A 102-center prospective study of seizure in association with bupropion. J Clin Psychiatry. 1991;52(11):450–456. | ||
Rosenquist PB, McCall WV, Farah A, Reboussin DM. Effects of caffeine pretreatment on measures of seizure impact. Convuls Ther. 1994;10(2):181–185. | ||
Carrillo JA, Benitez J. Clinically significant pharmacokinetic interactions between dietary caffeine and medications. Clin Pharmacokinet. 2000;39(2):127–153. | ||
Morris PB, Ference BA, Jahangir E, et al. Cardiovascular effects of exposure to cigarette smoke and electronic cigarettes: clinical perspectives from the Prevention of Cardiovascular Disease Section Leadership Council and Early Career Councils of the American College of Cardiology. J Am Coll Cardiol. 2015;66(12):1378–1391. | ||
Picciotto MR, Mineur YS. Nicotine, food intake, and activation of POMC neurons. Neuropsychopharmacology. 2013;38(1):245. | ||
Toll BA, Leary V, Wu R, Salovey P, Meandzija B, O’Malley SS. A preliminary investigation of naltrexone augmentation of bupropion to stop smoking with less weight gain. Addict Behav. 2008;33(1):173–179. | ||
Wilcox CS, Oskooilar N, Erickson JS, et al. An open-label study of naltrexone and bupropion combination therapy for smoking cessation in overweight and obese subjects. Addict Behav. 2010;35(3):229–234. | ||
Kim SW, Grant JE, Yoon G, Williams KA, Remmel RP. Safety of high-dose naltrexone treatment: hepatic transaminase profiles among outpatients. Clin Neuropharmacol. 2006;29(2):77–79. | ||
Xiang X, An R. Obesity and onset of depression among U.S. middle-aged and older adults. J Psychosom Res. 2015;78(3):242–248. | ||
McElroy SL, Guerdjikova AI, Kim DD, et al. Naltrexone/bupropion combination therapy in overweight or obese patients with major depressive disorder: results of a pilot study. Prim Care Companion CNS Disord. 2013;15(3):12m01494. | ||
Patel R, Reiss P, Shetty H, et al. Do antidepressants increase the risk of mania and bipolar disorder in people with depression? A retrospective electronic case register cohort study. BMJ Open. 2015;5(12):e008341. | ||
Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163(2):232–239. | ||
Tek C, Kucukgoncu S, Guloksuz S, Woods SW, Srihari VH, Annamalai A. Antipsychotic-induced weight gain in first-episode psychosis patients: a meta-analysis of differential effects of antipsychotic medications. Early Interv Psychiatry. Epub May 12, 2015. | ||
George TP, Vessicchio JC, Termine A, et al. A placebo controlled trial of bupropion for smoking cessation in schizophrenia. Biol Psychiatry. 2002;52(1):53–61. | ||
Kumar S, Kodela S, Detweiler JG, Kim KY, Detweiler MB. Bupropion-induced psychosis: folklore or a fact? A systematic review of the literature. Gen Hosp Psychiatry. 2011;33(6):612–617. | ||
Hassanian-Moghaddam H, Afzali S, Pooya A. Withdrawal syndrome caused by naltrexone in opioid abusers. Hum Exp Toxicol. 2014;33(6):561–567. | ||
Haney M, Ramesh D, Glass A, Pavlicova M, Bedi G, Cooper ZD. Naltrexone maintenance decreases cannabis self-administration and subjective effects in daily cannabis smokers. Neuropsychopharmacology. 2015;40(11):2489–2498. | ||
Mannelli P, Peindl K, Patkar AA, Wu LT, Pae CU, Gorelick DA. Reduced cannabis use after low-dose naltrexone addition to opioid detoxification. J Clin Psychopharmacol. 2010;30(4):476–478. | ||
Comer SD, Mogali S, Saccone PA, et al. Effects of acute oral naltrexone on the subjective and physiological effects of oral d-amphetamine and smoked cocaine in cocaine abusers. Neuropsychopharmacology. 2013;38(12):2427–2438. | ||
Cordery SF, Taverner A, Ridzwan IE, et al. A non-rewarding, non-aversive buprenorphine/naltrexone combination attenuates drug-primed reinstatement to cocaine and morphine in rats in a conditioned place preference paradigm. Addict Biol. 2014;19(4):575–586. | ||
Wee S, Vendruscolo LF, Misra KK, Schlosburg JE, Koob GF. A combination of buprenorphine and naltrexone blocks compulsive cocaine intake in rodents without producing dependence. Sci Transl Med. 2012;4(146):146ra110. | ||
Killian LM, Docherty JR. Cardiovascular stimulant actions of bupropion in comparison to cocaine in the rat. Eur J Pharmacol. 2014;735:32–37. | ||
Liangpunsakul S. Relationship between alcohol intake and dietary pattern: findings from NHANES III. World J Gastroenterol. 2010;16(32):4055–4060. | ||
Anton RF, Oroszi G, O’Malley S, et al. An evaluation of mu-opioid receptor (OPRM1) as a predictor of naltrexone response in the treatment of alcohol dependence: results from the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) study. Arch Gen Psychiatry. 2008;65(2):135–144. | ||
de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 2001;25(Suppl 1):S51–S55. | ||
Palavras MA, Hay P, Touyz S, et al. Comparing cognitive behavioural therapy for eating disorders integrated with behavioural weight loss therapy to cognitive behavioural therapy-enhanced alone in overweight or obese people with bulimia nervosa or binge eating disorder: study protocol for a randomised controlled trial. Trials. 2015;16:578. | ||
Auger RR. Sleep-related eating disorders. Psychiatry (Edgmont). 2006;3(11):64–70. | ||
White MA, Grilo CM. Bupropion for overweight women with binge-eating disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2013;74(4):400–406. | ||
Nedeltcheva AV, Scheer FA. Metabolic effects of sleep disruption, links to obesity and diabetes. Curr Opin Endocrinol Diabetes Obes. 2014;21(4):293–298. | ||
Alam I, Lewis K, Stephens JW, Baxter JN. Obesity, metabolic syndrome and sleep apnoea: all pro-inflammatory states. Obes Rev. 2007;8(2):119–127. | ||
Sethi M, Parikh M. Bariatric surgery versus intensive medical weight management for type 2 diabetes. Adv Surg. 2015;49(1):157–171. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
