Back to Journals » Infection and Drug Resistance » Volume 15
Multidrug-Resistant Bacteria Isolated from Blood Culture Samples in a Moroccan Tertiary Hospital: True Bacteremia or Contamination?
Authors Nachate S, Rouhi S, Ouassif H, Bennani H, Hachimi A , Mouaffak Y, Younous S, Bennaoui F, El Idrissi Slitine N, Maoulainine FMR, Lamrani Hanchi A, Soraa N
Received 7 May 2022
Accepted for publication 26 August 2022
Published 27 September 2022 Volume 2022:15 Pages 5691—5704
DOI https://doi.org/10.2147/IDR.S373065
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Soumia Nachate,1 Salma Rouhi,1 Hicham Ouassif,1 Hind Bennani,1 Abdelhamid Hachimi,2 Youssef Mouaffak,3 Said Younous,3 Fatiha Bennaoui,4 Nadia El Idrissi Slitine,4 Fadl Mrabih Rabou Maoulainine,4 Asmae Lamrani Hanchi,1 Nabila Soraa1
1Department of Microbiology, Mohamed VI University Hospital Center, Marrakech, Morocco; 2Department of Intensive Care, Mohamed VI University Hospital Center, Marrakech, Morocco; 3Pediatric Intensive Care Department, Mohamed VI University Hospital Center, Marrakech, Morocco; 4Neonatal Intensive Care Department, Mohamed VI University Hospital Center, Marrakech, Morocco
Correspondence: Soumia Nachate, Department of Microbiology, Mohamed VI University Hospital Center, BP2360 Principal, Ibn Sina Avenue, Marrakech, 40160, Morocco, Tel +212 658956312, Email [email protected]
Purpose: To demonstrate the relevance of clinico-biological correlation in the interpretation of positive blood cultures (BC) for multidrug-resistant (MDR) bacteria, among adult and pediatric patients, in order to distinguish between true bacteremia (TB) and contaminations and to evaluate the impact on patient management.
Patients and Methods: This six-month study was conducted at Mohammed VI University Hospital in Marrakech. All MDR bacteria isolated from BCs carried out on hospitalized patients during this period were included. For each positive BC to MDR microorganism, demographic and clinical characteristics, laboratory findings, therapeutic and evolution data were collected.
Results: TB was considered in 157 (94.6%) of the 166 positive-culture episodes for MDR bacteria, while 9 (5.4%) were classified as false-positive. Contamination rate was 0.2% (9/3824). TB and contaminations occurred mainly in intensive care units (ICUs), with the neonatal ICU being the most concerned (p = 0.016). Clinical signs of sepsis were present in all TB patients, with a significant difference between the two groups (p = 0.000). CRP values were higher in the TB group (p = 0.000). The most isolated true pathogens were ESBL-producing Enterobacterales (50%) and carbapenem-resistant Enterobacterales (33.3%). They also predominated in contaminated BCs. Isolation of the same microorganism from other sites was significantly associated with TB (p = 0.012). In contrast to the contaminations group, the difference in the clinical course of TB patients, according to whether or not they received appropriate probabilistic antibiotics, was statistically significant (p = 0.000). These patients had longer hospital stays and longer durations of antibiotic therapy. The overall mortality rate was 39.6%.
Conclusion: Distinguishing between MDR-positive BCs representing clinically significant bacteremia or simple contamination requires a careful clinical, biological, and microbiological confrontation of each MDR positive BC in order to avoid unnecessary overuse of broad-spectrum antibiotics and thus reduce resistance selective pressure.
Keywords: blood culture, multidrug-resistant bacteria, clinico-biological correlation, true bacteremia, contamination
Introduction
According to the World Health Organisation (WHO), antimicrobial resistance is currently the most urgent threat to global health.1 It contributes to an estimated 700,000 deaths per year and is expected to cause 10 million deaths per year by 2050 if no effective interventions are adopted.2
Multidrug-resistant (MDR) bacteria carry an arsenal of virulence factors and have acquired versatile resistance mechanisms to counteract the most effective antibiotics.3 Among MDR bacteria, the following pathogens: Enterococcus (E.) faecium, Staphylococcus (S.) aureus, Klebsiella pneumoniae, Acinetobacter (A.) baumannii, Pseudomonas (P.) aeruginosa, and Enterobacter species have been designated under the acronym “ESKAPE” because of their ability to escape the bactericidal activity of conventional antibiotics.4
In February 2017, the WHO developed a priority pathogen list where ESKAPEs and other microorganisms were stratified into three categories according to the urgency of the need for new antibiotics: critical, high, and medium priority. Vancomycin-resistant Enterococcus (VRE) faecium and methicillin-resistant Staphylococcus aureus (MRSA) were classified as high priority pathogens. Carbapenem-resistant Acinetobacter baumannii (CRAB), carbapenem-resistant Pseudomonas aeruginosa (CRPA), and carbapenem-producing or extended-spectrum beta-lactamase (ESBL)-producing strains of Enterobacterales were stratified as critical priority pathogens as they cause life-threatening infections such as pneumonia and bloodstream infections.5 However, the development of new antibiotics to control the threat of multidrug-resistance will remain insufficient in the absence of efforts focused on infection prevention and appropriate use of existing and newly developed antibiotics.
Bloodstream infections are one of the potentially life-threatening MDR infections in adults and pediatric patients. These are increasing worldwide and are associated with high morbidity, mortality, and significant costs. They represent a real challenge for clinicians in terms of patients’ management, which can even lead to therapeutic impasse. Prompt diagnosis and urgent treatment based on early, adequate, and broad-spectrum antibiotics are required.6–8
The blood culture (BC) is the gold standard for the diagnosis of bacteremia. Its execution procedures are strictly codified.9 The BC contamination rate is a commonly used indicator of BC processing quality, which needs to be continuously monitored to keep it within the international standards.9,10 The most common contaminants are coagulase-negative staphylococci, Corynebacterium spp., Bacillus spp. (other than B. anthracis), Propionibacterium acnes, Micrococcus spp. and Streptococcus viridans.11,12 This report is of particular interest because it focuses on unusual BC contamination with MDR bacteria. The microbiology team’s routine communication with clinicians when BCs are positive for MDR germs, in order to inform them about the positivity of BCs and to promptly guide the empirical antibiotic therapy in use, was in some cases unexpected as the patient’s clinical state was stable even under an inappropriate probabilistic antibiotherapy. Therefore, doubt about the possibility of contamination by MDR bacteria is raised, and the interest in correlating the clinical and biological findings of any positive BC with MDR bacteria in order to establish its true clinical significance becomes obvious. This is the first national study to assess the clinico-biologic correlation in MDR bacteremia. BC contamination can be misleading to clinicians and could have a significant impact on patient management, leading to unjustified use of broad-spectrum antibiotics, longer hospital stays, unnecessary further investigations, and therefore increased hospital charges.13,14 The aim of this study was to demonstrate the relevance of the clinico-biological correlation in the interpretation of positive BCs for MDR bacteria in order to distinguish between true bacteremia and false-positive BCs and to evaluate their impact on patient management.
Patients and Methods
Settings and Study Design
This monocentric prospective observational study was carried out in the University Hospital Center (CHU) Mohammed-VI of Marrakech, Morocco, North Africa, a public establishment of fourth resort healthcare. It is composed of four hospitals with a complete range of specialized disciplines and a haemato-oncology center (capacity of 1548 beds) and provides care to the whole population of Marrakech-Safi and the southern regions with approximately 57,096 admissions per year. Over a consecutive 6-month period from June 2019 to December 2019, all MDR strains isolated from BCs of patients hospitalized in the different departments of the CHU during the study period, without age restriction, were included.
Data Collection and Definitions
Baseline demographic characteristics, clinical details, laboratory findings, therapeutic and evolution data were collected for each MDR-positive BC from the patients’ charts and computerized medical records (Hosix software).
For therapeutic management, we collected probabilistic and definitive antibiotherapy, duration of antibiotic therapy, and hospital stay. Probabilistic and definitive antibiotherapy refer to antibiotics administered before and after receipt of the susceptibility testing results, respectively. The inappropriateness of the probabilistic regimen was judged, after analysis of the susceptibility testing data, based on comparison with the remaining active antimicrobial agents for each MDR bacteria. It was considered adequate if the isolated microorganisms exhibited in vitro sensitivity to one of the antibiotics administered to the patient and vice versa.
Among the positive BCs with MDR bacteria, TB was defined as any positive BC in a patient with clinical and biological evidence of sepsis. In adults, sepsis was defined according to the definition of the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) using the Sequential Organ Failure Assessment Score (SOFA score), calculated at the time of BC on the basis of clinical and biological criteria. A SOFA score of 2 or greater is used to define sepsis.15 Given the lack of consensus on the definition of sepsis in pediatrics, BCs were considered contaminated when the patient was clinically stable and the laboratory findings were not consistent with the BC result in the absence of any antibiotics, or when the patient had a good clinical course under empirical antibiotics not corresponding to the susceptibility pattern of the cultured isolate, or when the clinician clearly stated in the medical record that the result represented contamination. In this study, all neonates with abnormal vital signs, poor feeding, apparent change in mental status, tone, or perfusion with a positive BC and compatible biological parameters were assumed to have neonatal sepsis.16,17
The MDR bacteria included in this study were: ESBL-producing Enterobacterales, carbapenem-producing Enterobacterales (CPE), CRAB, CRPA, MRSA, and VRE.
The isolation of a single MDR microorganism from BC vials was defined as a “monomicrobial episode”. The presence of at least two different MDR bacteria in the same BC was referred to as a “polymicrobial episode”.
MDR bacteremia was considered to be nosocomial when the first positive BC was collected >48 hours after admission.
Microbiology
Bacterial Strains and Antimicrobial Susceptibility Testing
Blood samples, collected in BD BACTEC® vials (Becton Dickinson, USA), were processed by the BD BACTEC™ FX-400 (Becton Dickinson diagnostics, Sparks, USA) automated system according to the manufacturer’s recommendations. Positive samples for bacterial growth were Gram stained and subcultured on appropriate media.
The species identification was carried out using the BD Phoenix automated microbiology system (Becton–Dickinson Diagnostic Systems, Sparks, MD, USA). The antimicrobial susceptibility testing (AST) was performed using the standard disk diffusion method on Mueller–Hinton agar according to the 2019 guidelines of the Antibiogram Committee of the French Society for Microbiology/European Committee on Antimicrobial Susceptibility Testing (CA-SFM/EUCAST).18 The AST was also determined by the automated method (Phoenix BD system). The minimal inhibitory concentration (MIC) of selected antibiotics was measured using the gradient diffusion method: E-test® (BioMérieux, Marcy L’Étoile, France).
For Enterobacterales species, 16 antibiotics (bioMérieux, Marcy L’Étoile, France) were tested, namely, amoxicillin (AMX; 10 μg), amoxicillin-clavulanic acid (AMC; 20–10 μg), piperacillin (PIP; 30 μg), piperacillin-tazobactam (TZP; 75–10 µg), cefoxitin (FOX; 30 μg), ceftazidime (CAZ; 10 μg), cefotaxime (CTX; 30 μg), cefepime (CPM, 30 μg), aztreonam (ATM, 30 μg), ertapenem (ETP; 10 μg), imipenem (IPM; 10 μg), amikacin (AMK; 30 μg), gentamicin (GEN; 10 μg), nalidixic acid (NAL; 30 μg), ciprofloxacin (CIP, 5 μg) and trimethoprim-sulfamethoxazole (SXT; 1.25–23.75 μg).
The AST panel for P. aeruginosa and A. baumannii contained 11 antibiotics: ticarcillin (TIC; 75 μg), piperacillin (PIP; 30 μg), piperacillin-tazobactam (TZP; 75–10 µg), ticarcillin-clavulanic acid (TIM; 75–10 µg), ceftazidime (CAZ; 10 μg), cefepime (CPM; 30 μg), imipenem (IPM; 10 μg), amikacin (AMK; 30 μg), gentamicin (GEN; 10 μg), tobramycin (TOB; 10 μg), ciprofloxacin (CIP, 5 μg). In addition to aztreonam (ATM; 30 μg) for P. aeruginosa and trimethoprim-sulfamethoxazole (SXT; 1.25–23.75 μg) for A. baumannii.
For S. aureus, 11 antibiotics were tested: cefoxitin (FOX; 30 μg), norfloxacin (NX; 10 μg), ciprofloxacin (CIP, 5 μg), erythromycin (ERY, 15 μg) clindamycin (CLI; 2 μg), gentamicin (GEN; 10 μg), tobramycin (TOB; 10 μg), kanamycin (KAN; 30 μg), trimethoprim-sulfamethoxazole (SXT; 1.25–23.75 μg), fusidic acid (FA; 10 μg), linezolid (LZD; 10 μg).
For E. faecalis and E. faecium, the AST panel consisted of 10 antibiotics: ampicillin (AMP; 2μg), norfloxacin (NX; 10 μg), ciprofloxacin (CIP, 5 μg), erythromycin (ERY, 15 μg) clindamycin (CLI; 2 μg), gentamicin (GEN; 30 μg), trimethoprim-sulfamethoxazole (SXT; 1.25–23.75 μg), vancomycin (VAN; 5 μg), teicoplanin (TEC; 30 μg) and linezolid (LZD; 10 μg).
The following reference strains were used for routine quality control of AST: E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213 and E. faecalis ATCC 29212. All AST results were interpreted in accordance with the 2019 CA-SFM/EUCAST guidelines.18
Detection of Multidrug Resistance
Using the double-disk synergy test, the ESBL production was concluded when the inhibition zone around CTX, CAZ, CPM, and ATM (30 μg each) antibiotic discs was expanded close to AMC (20/10 μg), resulting in the appearance of a characteristic shaped-zone referred to as a “champagne cork”.19
Following detection of reduced susceptibility to carbapenems in Enterobacterales isolates (inhibition zone diameter <25 mm for 10-μg ertapenem disc or MIC > 0.5 mg/L), the imipenem MIC was determined and a phenotypic method based on the Combined Disk Test (CDT) was applied.20 Each isolate was then subjected to a lateral flow immunochromatographic test, Resist-5 O.O.K.N.V. (CORIS Bioconcept, Belgium), as per the manufacturer’s directions, to confirm the presence of one or more carbapenemases (NDM, VIM, KPC, OXA-48, and OXA-163). The Resist-5 O.O.K.N.V. test was also used for imipenem-resistant A. baumannii (MIC > 4 mg/L) and P. aeruginosa (MIC > 8 mg/L).
For S. aureus isolates, a 30-μg cefoxitin disk was used as a surrogate marker for determining mecA-mediated oxacillin resistance. An inhibition zone with a diameter ≤22 mm around the cefoxitin disk was interpreted as MRSA. S. aureus NCTC 12493 was used as a quality control for mecA positive strains.
Statistical Analysis
The data were collected using Microsoft Excel 2007 and analyzed using IBM SPSS Statistics for Windows, Version 25.0. (IBM Corp., Armonk, N.Y., USA). The TB and contamination groups were compared on the basis of the demographic characteristics, the inpatient wards, clinical details, laboratory findings, therapeutic data, and clinical course. Both groups were also compared for the main MDR bacteria isolated. Values were presented as medians (interquartile ranges [IQRs]) for quantitative variables and as percentages for qualitative variables. Comparison between the two groups was performed using the Chi-square test or two-tailed Fisher exact test for categorical variables and the Student t test or Mann–Whitney U-test for quantitative variables. p-value <0.05 was considered statistically significant for all analyses.
Results
During the six months of the study, 3824 BCs were received in the microbiology laboratory, obtained from patients hospitalized in the different departments of the Mohammed-VI University Hospital of Marrakech. Bacterial growth was detected in 1006 BCs with a positivity rate of 26.3%. In all, 166 positive-culture episodes for MDR bacteria (154 patients) were identified, giving a prevalence of 4.3% (166/3824). This prevalence was 2.9% in pediatrics and 1.4% in adults. TB was assumed in 157 episodes among 145 patients, representing 94.6% of all culture-positive episodes for MDR bacteria. Nine patients presented several bacteremic episodes with different MDR germs during the same hospitalization (two episodes for six patients and three episodes for three patients). Burn patients represented 55.5% (5/9) of these cases. Positive BCs to MDR bacteria classified as contaminated BCs accounted for 5.4% (n = 9) over this period. The rate of contamination was 0.2% (9/3824) (Figure 1).
Patients’ Characteristics
The age group of less than 1 month was the most represented in both TB (n = 67, 42.7%) and contamination groups (n = 7, 77.8%) with an average age of 7.78 and 2.86 days, respectively. Neonates with contaminated BCs were significantly younger than those with TB (7.78 days versus 2.86 days, p = 0.014). No contaminated BCs were identified in the age group >15 years (35.7% versus 0.0%, p = 0.029). Male predominance was observed in both groups (sex ratio: 1.70 versus 3.5, p = 0.490). TB (n = 129, 82.2%) and contaminations (n = 7, 77.8%) occurred mainly in intensive care units (ICUs). The neonatal intensive care unit (NICU) was significantly more concerned (p = 0.016). No significant difference was observed in terms of initial diagnosis between the two groups. In addition, 59.2% of patients had a central line in the TB group versus 0.0% in the contamination group (p = 0.000). At the time of blood sampling, clinical signs of sepsis were present in all patients who had TB, with a significant difference between the two groups (p = 0.000). Regarding biological tests, C-reactive protein (CRP) was positive in 44.4% of patients with contaminated BCs. Its values were higher in the TB group, with a median of 140.83 mg/L compared to 13.71 mg/L in the contamination group (p = 0.000). Thrombocytopenia and lymphopenia were noted in a large number of patients with TB. This difference was statistically significant (platelets (G/L): 129 versus 246, p = 0.038) and (lymphocytes (G/L): 1.62 versus 4.09, p = 0.017) (Table 1).
 |
Table 1 Baseline Characteristics of Patients with Positive BCs with MDR Bacteria (True Bacteremia and Contaminations) |
Characteristics of Positive BCs
One hundred and seventy-one (171) non-redundant MDR bacteria were isolated from 1006 positive BCs during the six-month period. A total of 162 (94.7%) were true MDR pathogens, isolated from 152 monomicrobial and 5 polymicrobial positive BCs for two MDR organisms. Nine (5.3%) were considered contaminants (Table 2). Among TB, Enterobacterales widely dominated the bacteriological profile (136/162; 83.9%), with 50% (81/162) of ESBL-producing Enterobacterales and 33.3% (54/162) of CPE. Klebsiella pneumoniae (77/136; 56.6%) and Enterobacter cloacae (37/136; 27.2%) were the most isolated MDR-Enterobacterales. MDR non-fermenting Gram-negative bacteria (GNB) represented 13.6% (22/162) of the true pathogens isolated, and MRSA was identified in 4 TB cases (2.5%). No VRE strain was found. These TB were nosocomial in 95.5% of cases. The spectrum of contaminants had the same distribution as the true pathogens, with contamination mainly by MDR-Enterobacterales (Table 2). There was no significant difference between the two groups according to the type of MDR strains identified. In 41.7% of the cases, the same MDR microorganism was isolated from other sites, which was significantly associated with TB (p = 0.012).
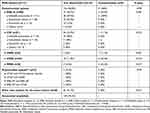 |
Table 2 Distribution of the Main Monomicrobial and Polymicrobial Causative Agents (True Pathogens and Contaminants) in Positive BCs with MDR Bacteria |
Treatments and Outcomes
Antibiotic Therapy in Patients with Contaminated BCs
Before the susceptibility testing results, eight (n = 8) patients with contaminated BCs (n = 9) were on antibiotics. Three of them were receiving “aminopenicillins and aminoglycosides”. Three were given 3rd generation cephalosporins and two were on carbapenems. According to the antibiogram, this antibiotic therapy was inappropriate in 87.5% of cases, with a good clinical course in all these patients (Table 3). It was interrupted and not substituted in two patients and carried on in five others even though it was not consistent with the sensitivity profile of the isolated microorganisms. It was also adjusted to the antibiogram in one patient with the combination “imipenem and aminoglycoside”.
 |
Table 3 Comparison of the Clinical Course of Patients According to the Appropriateness of Probabilistic Antibiotic Therapy |
Antibiotic Therapy in Patients with TB
Empirical antibiotic therapy was started in all patients with TB (n = 145), based on 3rd generation cephalosporins in 46.2% of the cases, carbapenems (31%), combination of “betalactams and glycopeptides” or colistin (1.4%), and tri-antibiotic therapy (11%). In vitro susceptibility testing revealed that the probabilistic therapy was appropriate in 35.9% (52/145) of the cases: 26.9% (39/145) were on “carbapenems and aminoglycosides”, 2.06% (3/145) on “colistin and aminoglycosides” and 5.5% (8/145) on tri-antibiotic therapy. Good clinical outcome was noted in 55.5% (29/52) of these patients, with a mortality rate of 9.6% (5/52). Of the 47 survivors who were on appropriate empirical antibiotic therapy, this was continued in 41 patients, with de-escalation to a narrower spectrum in 6 patients.
This empirical antibiotic therapy was inappropriate in 64.1% (93/145) of cases based on 3rd generation cephalosporins in 70.9% (66/145) of cases, the combination “aminopenicillins and aminoglycosides” in 11.8% (11/145) of cases, and carbapenems in 6.4% (6/145) of cases. The clinical course was unfavourable in 79.6% (74/93) of these patients, with a mortality rate of 20.4% (19/93). All survivors with an unfavourable outcome from inappropriate antibiotic therapy (n = 74) received an adjustment of the regimen according to the alternatives available on the antibiogram.
Clinical Course of Patients in the TB Group versus the Contaminations Group
The difference in the clinical course of patients in the TB group, according to whether or not they received appropriate probabilistic antibiotic therapy, was statistically significant (p = 0.000). In contrast to the contamination group, where 87.5% of patients had a favourable course despite inappropriate empirical antibiotic therapy (p = 0.882) (Table 3). Patients with TB had longer hospital stays (median: 16 days versus 10 days, P<0.008) and a prolonged duration of antibiotic therapy (median: 10 days versus 8 days, p = 0.049). The final outcome was favourable in 60.4% (93/154) of patients, with an overall mortality rate of 39.6% (61/154). This rate was significantly higher in the TB group (42.1% versus 0.0%, P = 0.009).
Discussion
The increased use of antibiotics has led to the emergence and spread of MDR bacteria globally. This multidrug-resistance is of particular concern in GNB (Enterobacterales and non-fermenting GNB) because of their broad and diversified resistome. Beyond their innate resistance, these bacteria have the potential to acquire additional resistance mechanisms through mutations in chromosomal genes or through the horizontal transfer of resistance genes carried on vectors such as plasmids, transposons, or integrons.3,21,22 Bacteria can resist antimicrobial agents by enzymatic and/or non-enzymatic mechanisms. Non-enzymatic pathways include altered membrane permeability, efflux pumps, or modifications in drug targets. Among the enzymatic mechanisms employed to inactivate or hydrolyse antibiotics, ESBLs and carbapenemases are two enzyme groups of high epidemiologic importance, involved in impairing the effectiveness of last resort antimicrobials in the treatment of life-threatening infections.3 The appropriate and judicious use of currently available antibiotics is of utmost importance.
During the six-month study period, the number of documented TB cases caused by MDR bacteria was alarming (n = 157, 15.6%). ICUs (82.2%), including NICU (51.9%), were the most affected. A marked predominance of ESBL-E (50%) and CPE (33.3%) was observed. The same trends have been reported in several studies.23–26
To our knowledge, this is the first study to examine bloodstream infections in both adult and pediatric populations, pointing out the likelihood of contamination with MDR microorganisms. This study reports a percentage of contaminated BCs of 5.4% (n = 9) among the 166 BCs positive for MDR bacteria. The Clinical and Laboratory Standards Institute (CLSI) recommends an overall BC contamination rate of <3% as the standard benchmark.9 BC contamination is a critical phenomenon with prevalence rates ranging from 0.6% to 12.5% or more among different institutions.27,28 Our contamination rate was 0.2% (9/3824). These contaminated BCs originated mainly from the pediatrics department and particularly concerned neonates hospitalized in the NICU (n = 7). Reported rates in the neonatal population range from 2.6 to 18%.29,30 This would be due to the difficulties of blood sampling in these patients; the small amount of blood taken for culture; the reduced number of vials usually drawn; and the common use of intravascular catheters instead of peripheral venipunctures as a sampling method for the patient’s comfort to minimise microtrauma and to preserve the patient’s venous capital.31–33 False-positive BC occurs when microorganisms isolated from BCs are brought from outside the patient’s bloodstream, most often from their immediate environment.27 Distinguishing contaminated BCs from clinically significant bacteremia can be challenging for clinicians and microbiologists.34,35 When the patient has clinical features requiring BCs and the contaminant is a potential pathogen, it is very likely to be considered a true bacteremia, which has serious repercussions not only for the patient but also for the healthcare resources.27 Thus, rigorous interpretation of positive BCs is imperative.
Clinical signs of sepsis were present in all patients with TB, with a significant difference between the two groups (p=0.000). In contrast to sepsis definitions in adults and children, the distinction between infection and sepsis in the NICU is actually not well defined.15 A recent case-control study established a neonatal sequential organ failure assessment (nSOFA) score that can be useful to define sepsis in this population but still needs to be validated in additional cohorts.36 Laboratory findings may help in distinguishing between true and false-positive BCs. In neonates, CRP is one of the most commonly used tests. A single positive CRP obtained at least 12 hours after the onset of symptoms has been shown to be useful in supporting the clinical suspicion of sepsis.37,38 In the current study, CRP values were higher in the TB group (p=0.000), and lymphopenia and thrombocytopenia were also noted in a large number of patients with true positive BCs with a statistically significant difference. Similarly, Chiu et al reported that elevated CRP and WBC levels were significant predictors of TB in the paediatric population.39 El-Naggari et al, found a significant association between high WBC and ANC in children with TB, whereas there was no statistically significant difference in CRP levels between the two groups.40 From a microbiological basis, several clues may be used in the interpretation of clinical significance of the positive BC: the identity of microorganism, number of positive culture sets, number of positive BC bottles within a set, and time to positivity.35,41 The identity of the microorganism was found to be the most important predictor to differentiate TB from contaminations.42 Some microorganisms, such as S. aureus, Streptococcus pneumoniae, Escherichia coli and other Enterobacterales, P. aeruginosa, should almost always be considered true pathogens when isolated from a BC.11 Nevertheless, it is not possible to interpret BC results only on the basis of the identity of isolated bacteria, infrequent exceptions are possible.43 In this report, we emphasize the importance of correlating microbiological results to the clinical condition and laboratory data of patients. Their clinical status, incompatible with bloodstream infections or the good clinical course under antibiotics that are ineffective against the MDR bacteria isolated from BCs, led us to discuss the likelihood of contamination by these MDR bacteria, despite belonging to the group of germs almost always considered as true pathogens.
In a review of 500 episodes of bacteremia, 25% of S. aureus isolates were considered contaminants. Amongst BCs positive for Enterobacterales, 2% of E. coli, 7% of Serratia marcescens, and 15% of Enterobacter aerogenes strains were of no clinical significance and represented contamination.34 A retrospective study in the United States has reported the contamination of BCs with MDR bacteria. The authors classified BCs as “probably contaminated” when the result of the BC did not require additional antibiotics, discontinuation of existing antibiotherapy did not affect the patient’s outcome, or when the result was considered by the clinician to be a ‘likely contaminant’. VRE faecalis (n = 12) and VRE faecium (n = 4) accounted for 3.5% of all probable contaminants. The rate of BC contamination in this study was significantly influenced by periods of high activity and flow in the emergency department.44 The number of positive BC sets is used to differentiate contaminated BCs from TB. However, it is not always the rule to obtain at least two sets; solitary BCs are frequent. The interpretation of a positive solitary BC as contaminated is difficult.41 At the least suspicion of contamination, a new BC set should be taken in strict aseptic conditions. Furthermore, the number of positive BC vials in a given BC batch is helpful for interpretation. As reported, if only one vial grows organisms in a given set, the likelihood of contamination is greater.35 In our setting, a single vial (BD BACTEC Peds Plus T/F culture vial) was usually collected from paediatric patients. This criterion was not useful to us in this category, especially for patients in whom bacteremia was unlikely. The presence of an identifiable source, particularly a central venous catheter, has been reported to be predictive of true bacteremia.45 Similarly, microbiological identification of the same MDR bacteria from other sites was significantly associated with TB in the present study.
Globally, none of these criteria, taken on their own, is sufficiently conclusive. A clinico-biological correlation remains the only reliable approach to determine the clinical significance of an isolated microorganism.46 Confrontation of the probabilistic antibiotic therapy with the antibiogram results is also useful.46 In this cohort, the clinical course of patients with TB was significantly associated with the appropriateness of the empirical regimen (p = 0.000), in contrast to the group of patients with contaminated BC (p = 0.882). A favourable clinical evolution under empirical antibiotics not concordant with the susceptibility profile of the isolated germ raises the question of its real presence and pathogenicity in the patient bloodstream. The first-line antibiotic therapy used in our patients was mainly 3rd generation cephalosporins in combination with an aminoglycoside. Improvement of symptoms and laboratory abnormalities leads the clinician to rule out a positive BC for MDR bacteria. This categorisation should avoid the adjustment of the current antibiotic therapy by the available alternative drugs on susceptibility testing results and thus prevent an escalation, in the case of MDR bacteria, to unnecessary broad-spectrum antibiotics. In the contamination group, we reported the case of a newborn who underwent probabilistic antibiotic therapy that was adjusted to the combination “imipenem and aminoglycoside” after receipt of the microbiology results despite the absence of clinical and biological signs of sepsis. There is a major dilemma for clinicians managing patients with comorbidities or vulnerable backgrounds, in whom some localized infections may manifest as a sepsis-like presentation. In these patients, interpreting the significance of a positive BC can be difficult, and the prescription of antibiotic therapy targeting the isolate may be of easy recourse. More prolonged hospital stays (P<0.008), longer duration of antibiotic therapy (p = 0.049) and higher mortality (P = 0.009) were noted in patients with TB. The same results were reported in a similar cohort in Oman.40 One of the major impacts of miscategorising cases of contamination, especially with MDR bacteria, is related to therapeutic management. False-positive BCs result in unjustified use of broad-spectrum antibiotics and consequently worsen the multidrug resistance crisis through increased selective pressure of new resistance mechanisms and cross-transmission of MDR strains, particularly in hospitals. Moreover, these pseudobacteremia can also be associated with additional costs due to the use of further unnecessary investigations and prolonged lengths of stay. This substantial financial impact has been demonstrated in a multivariate analysis which revealed that they were independently associated with a 20% increase in laboratory costs and a 39% increase in costs related to unnecessary intravenous antibiotics.42 Early recognition of contamination by clinicians and laboratorians is obviously important to prevent these serious negative consequences. The morbidity and mortality associated with MDR bacteremia is high and multifactorial, related to the fragility of the patient’s condition, the severity of the disease, and the inadequacy of the initial antibiotic therapy.47,48
Contamination of BCs can occur at any stage throughout the pre-analytical phase, most commonly indicating a breakdown in asepsis from BC collection to laboratory processing.27 The experience of the phlebotomist is a factor closely linked to the risk of contamination, particularly when dealing with young patients.49 An outbreak of MRSA pseudobacteremia was reported in 1984 at Boston City Hospital, resulting from cross-contamination in the automated radiometric BC analyzer (BACTEC 460) used in the microbiology department, in which bacterial growth was detected by regular automatic sampling of incubated vials, the error being due to a problem with needle decontamination.50 Current BC instruments, such as the Bactec™ FX, used in our laboratory, are based on fluorescence detection technology without vial sampling, which avoids the risk of contamination within the instrument. A cluster of Enterobacter cloacae false bacteremia has also been reported in Shiprock Hospital, Mexico. This outbreak was suspected by matching clinical and bacteriological data of patients, where 74% of BCs were obtained from patients with no clinical evidence of Gram-negative sepsis. It was attributed to the use of a new agar slant blood culturing system.51 Contamination of hospital surfaces with MDR bacteria is being increasingly described.52 Most of these microorganisms are cross-resistant to various antibiotics and antiseptic agents, which enables them to persist for long periods in the environment.27,53,54 This represents a real danger to public health as it can be a source of cross-transmission of MDR bacteria between patients, between the hospital and the community, and is also a potential reservoir for contamination of specimens, hence the necessity of strict adherence to hand hygiene and surface disinfection guidelines in hospitals.55
Limitations
This is a single-center study that reflects its own practices. The results cannot be generalised to other hospitals or patient populations. A single BC in a neonate with suspected bacteremia limits the ability to differentiate with confidence between true and false bacteremia, especially as the signs of infection in this population are not specific. As there is no gold standard for the diagnosis of bacteremia, the risk of classification bias may exist. Additional costs due to false bacteremia have not been estimated.
Conclusion
This study highlights the problem of true MDR bacteremia in the ICUs, which mainly affects neonates and is caused by ESBL-E and CPE. These true MDR bacteremias complicate the therapeutic management of these serious infections in our context and lead to the use of broad-spectrum antibiotics, prolonged hospitalization, and a high mortality rate.
The contamination of BCs with MDR is a critical and alarming phenomenon. In the era of pan-resistant bacteria, it is imperative to distinguish between MDR-positive BCs representing clinically significant bacteremia and simple contamination with no clinical threat, in order to avoid unwarranted overuse of broad-spectrum antibiotics and to reduce the delay of inappropriate antibiotic therapy and thus decrease resistance selective pressure. Only a thorough clinical, biological, and microbiological confrontation of all MDR bacteremia can ensure accurate interpretation of results. Collaboration between clinicians and microbiologists as part of a multidisciplinary approach to patient management and respect of hygiene rules and strict aseptic conditions at the time of sampling is mandatory to prevent BC contamination.
Abbreviations
WHO, World Health Organisation; BC, blood cultures; MDR, multidrug-resistant; TB, true bacteremia; ICU, intensive care unit; CRP, C-reactive protein; CHU, University Hospital Center; ESBL-E, extended-spectrum beta-lactamase producing Enterobacteriaceae; CRE, carbapenem-resistant Enterobacteriaceae; CRAB, carbapenem-resistant Acinetobacter baumannii; CRPA, carbapenem-resistant Pseudomonas aeruginosa; MRSA, Methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant Enterococcus; SOFA score, Sequential Organ Failure Assessment Score; NICU, Neonatal intensive care unit; CLSI, Clinical and Laboratory Standards Institute; WBC, White blood cells; ANC, Absolute neutrophil counts.
Ethical Considerations
The present study was approved by the Ethics Committee of the Mohammed-VI University Hospital, affiliated to the Faculty of Medicine, Cadi Ayyad University, Marrakech-Morocco (N° 2022-06). Informed consent was provided by the study participants or their legal guardian/next of kin, before study enrollment. This study complies with the Declaration of Helsinki.
Acknowledgments
The authors would like to express their sincere gratitude to all the staff of the microbiology department as well as to the staff of the different departments of Mohammed-VI University Hospital of Marrakech.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that no funding was received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Global action plan on antimicrobial resistance. [Internet]; 2015. Available from: https://apps.who.int/iris/handle/10665/193736.
2. Hoffman SJ, Outterson K, Røttingen JA, et al. An international legal framework to address antimicrobial resistance. Bull World Health Organ. 2015;93(2):66. doi:10.2471/BLT.15.152710
3. Ahmadi M, Ranjbar R, Behzadi P, Mohammadian T. Virulence factors, antibiotic resistance patterns, and molecular types of clinical isolates of Klebsiella Pneumoniae. Expert Rev Anti Infect Ther. 2022;20(3):463–472. doi:10.1080/14787210.2022.1990040
4. De Oliveira DMP, Forde BM, Kidd TJ, et al. Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev. 2020;33:e00181–19.
5. World Health Organization. Prioritization of Pathogens to Guide Discovery, Research and Development of New Antibiotics for Drug-Resistant Bacterial Infections, Including Tuberculosis. (WHO/EMP/IAU/2017.12). (Licence: CC BY-NC-SA 3.0 IGO). Geneva: World Health Organization; 2017.
6. Anderson DJ, Moehring RW, Sloane R, et al. Bloodstream infections in community hospitals in the 21st century: a multicenter cohort study. PLoS One. 2014;9(3):e91713. doi:10.1371/journal.pone.0091713
7. Wattal C, Goel N. Pediatric blood cultures and antibiotic resistance: an overview. Indian J Pediatr. 2020;87(2):125–131. doi:10.1007/s12098-019-03123-y
8. Folgori L, Livadiotti S, Carletti M, et al. Epidemiology and clinical outcomes of multidrug-resistant, gram-negative bloodstream infections in a European tertiary pediatric hospital during a 12-month period. Pediatr Infect Dis J. 2014;33(9):929–932. doi:10.1097/INF.0000000000000339
9. Clinical and Laboratory Standards Institute. M47A: principles and procedures for blood cultures: approved guideline. [Homepage on the internet]. Available from: https://clsi.org/standards/products/microbiology/documents/m47/.
10. Chukwuemeka IK, Samuel Y. Quality assurance in blood culture: a retrospective study of blood culture contamination rate in a tertiary hospital in Nigeria. Niger Med J. 2014;55(3):201–203. doi:10.4103/0300-1652.132038
11. Weinstein MP, Towns ML, Quartey SM, et al. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997;24(4):584e602. doi:10.1093/clind/24.4.584
12. Alnami AY, Aljasser AA, Almousa RM, et al. Rate of blood culture contamination in a teaching hospital: a single center study. J Taibah Univ Med Sci. 2015;10(4):432–436. doi:10.1016/j.jtumed.2015.08.002
13. Alahmadi YM, Aldeyab MA, McElnay JC, et al. Clinical and economic impact of contaminated blood cultures within the hospital setting. J Hosp Infect. 2011;77(3):233–236. doi:10.1016/j.jhin.2010.09.033
14. Thuler LC, Jenicek M, Turgeon JP, Rivard M, Lebel P. Impact of a false positive blood culture result on the management of febrile children. Pediatr Infect Dis J. 1997;16(9):846–851. doi:10.1097/00006454-199709000-00006
15. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
16. Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014;27(1):21–47. doi:10.1128/CMR.00031-13
17. Kim F, Polin RA, Hooven TA. Neonatal sepsis. BMJ. 2020;371:m3672. doi:10.1136/bmj.m3672
18. French Society for Microbiology. Internal quality control. In : CASFM / EUCAST : Société Française de Microbiologie Ed; 2019:p.16.
19. Garrec H, Drieux-Rouzet L, Golmard JL, Jarlier V, Robert J. Comparison of nine phenotypic methods for detection of extended-spectrum β-lactamase production by Enterobacteriaceae. J Clin Microbiol. 2011;49(3):1048–1057. doi:10.1128/JCM.02130-10
20. Dilagui I, Loqman S, Lamrani Hanchi A, Soraa N. Antibiotic resistance patterns of carbapenemase-producing enterobacterales in Mohammed VI University Hospital of Marrakech, Morocco. Infect Dis Now. 2022;52(6):S2666–9919. doi:10.1016/j.idnow.2022.06.001
21. Sarshar M, Behzadi P, Scribano D, Palamara AT, Ambrosi C. Acinetobacter baumannii: an ancient commensal with weapons of a pathogen. Pathogens. 2021;10(4):387. doi:10.3390/pathogens10040387
22. Behzadi P, Baráth Z, Gajdács M. It’s not easy being green: a narrative review on the microbiology, virulence and therapeutic prospects of multidrug-resistant pseudomonas aeruginosa. Antibiotics. 2021;10(1):42. doi:10.3390/antibiotics10010042
23. Oliveira PMN, Buonora SN, Souza CLP, et al. Surveillance of multidrug-resistant bacteria in pediatric and neonatal intensive care units in Rio de Janeiro State, Brazil. Rev Soc Bras Med Trop. 2019;52:e20190205. doi:10.1590/0037-8682-0205-2019
24. Nivesvivat T, Piyaraj P, Thunyaharn S, Watanaveeradej V, Suwanpakdee D. Clinical epidemiology, risk factors and treatment outcomes of extended-spectrum beta-lactamase producing Enterobacteriaceae bacteremia among children in a Tertiary Care Hospital, Bangkok, Thailand. BMC Res Notes. 2018;11(1):624. doi:10.1186/s13104-018-3729-3
25. Ndir A, Diop A, Faye PM, Cissé MF, Ndoye B. Epidemiology and burden of bloodstream infections caused by extended-spectrum beta-lactamase producing Enterobacteriaceae in a pediatric hospital in Senegal. PLoS One. 2016;11(2):e0143729. doi:10.1371/journal.pone.0143729
26. Musicha P, Cornick JE, Bar-Zeev N, et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998–2016): a surveillance study. Lancet Infect Dis. 2017;17(10):1042–1052. doi:10.1016/S1473-3099(17)30394-8
27. Jumaa PA, Chattopadhyay B. Pseudobacteraemia. J Hosp Infect. 1994;27(3):167–177. doi:10.1016/0195-6701(94)90124-4
28. Snyder SR, Favoretto AM, Baetz RA, et al. Effectiveness of practices to reduce blood culture contamination: a Laboratory Medicine Best Practices systematic review and meta-analysis. Clin Biochem. 2012;45(13–14):999–1011. doi:10.1016/j.clinbiochem.2012.06.007
29. Hamilton LF, Gillett HE, Smith-Collins A, Davis JW. A sterile collection bundle intervention reduces the recovery of bacteria from neonatal blood culture. Biomed Hub. 2018;3(1):486703. doi:10.1159/000486703
30. McLaughlin LM, Inglis GDT, Hoellering AB, Davies MW. Relationship between blood culture collection method and proportion of contaminated cultures in neonates. J Paediatr Child Health. 2013;49(2):105–108. doi:10.1111/jpc.12088
31. Lamy B, Dargère S, Arendrup MC, Parienti JJ, Tattevin P. How to optimize the use of blood cultures for the diagnosis of blood stream infections? A state-of-the art. Front Microbiol. 2016;7:697. doi:10.3389/fmicb.2016.00697
32. Norberg A, Christopher NC, Ramundo ML, Bower JR, Berman SA. Contamination rates of blood cultures obtained by dedicated phlebotomy vs intravenous catheter. JAMA. 2003;289(6):726–729. doi:10.1001/jama.289.6.726
33. Min H, Park CS, Kim DS, Kim KH. Blood culture contamination in hospitalized pediatric patients: a single institution experience. Korean J Pediatr. 2014;57(4):178–185. doi:10.3345/kjp.2014.57.4.178
34. Weinstein MP, Reller LB, Murphy JR, Lichtenstein KA. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev Infect Dis. 1983;5(1):35–53. doi:10.1093/clinids/5.1.35
35. Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19(4):788–802. doi:10.1128/CMR.00062-05
36. Wynn JL, Polin RA. A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr Res. 2020;88(1):85–90. doi:10.1038/s41390-019-0517-2
37. Hofer N, Zacharias E, Müller W, Resch B. An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology. 2012;102(1):25–36. doi:10.1159/000336629
38. Berger C, Uehlinger J, Ghelfi D, et al. Comparison of C-reactive protein and white blood cell count with differential in neonates at risk for septicaemia. Eur J Pediatr. 1995;154:138–144. doi:10.1007/BF01991918
39. Chiu YH, Chen TJ, Chen CT, Lu -C-C. Positive blood cultures in pediatric emergency department patients: epidemiological and clinical characteristics. Acta Paediatr Taiwan. 2005;46(1):11–16.
40. El-Naggari MA, Al-Mulaabed SW, Al-Muharrmi Z, Mani R, Abdelrahim R, Abdwani R. Blood culture contaminants in a paediatric population retrospective study from a tertiary hospital in Oman. Sultan Qaboos Univ Med J. 2017;17(2):e202–e208. doi:10.18295/squmj.2016.17.02.011
41. Dargère S, Cormier H. Contaminants in blood cultures: importance, implications, interpretation and prevention. Clin Microbiol Infect. 2018;24(9):964–969. doi:10.1016/j.cmi.2018.03.030
42. Bates DW, Goldman L. Contaminant blood cultures and resource utilization: the true consequences of false-positive results. JAMA. 1991;265(3):365–369. doi:10.1001/jama.1991.03460030071031
43. Chappell-Campbell L, Schwenk HT, Capdarest-Arest N, Schroeder AR. Reporting and categorization of blood culture contaminants in infants and young children: a scoping review. J Pediatric Infect Dis Soc. 2020;9(2):110–117. doi:10.1093/jpids/piy125
44. Halverson S, Malani PN, Newton DW, Habicht A, Vander Have KYJ, Younger JG. Impact of hourly emergency department patient volume on blood culture contamination and diagnostic yield. J Clin Microbiol. 2013;51(6):1721–1726. doi:10.1128/JCM.03422-12
45. Lyytikäinen O, Valtonen V, Anttila VJ, Ruutu P. Evaluation of clinical and laboratory findings in leukaemic patients with blood cultures positive for Staphylococcus epidermidis. J Hosp Infect. 1998;38(1):27–35. doi:10.1016/s0195-6701(98)90172-4
46. Société Française de Microbiologie. REMIC: Référentiel en microbiologie Médicale.
47. Murni IK, Duke T, Daley AJ, Kinney S, Soenarto Y. Antibiotic resistance and mortality in children with nosocomial bloodstream infection in a teaching hospital in Indonesia. Southeast Asian J Trop Med Public Health. 2016;47(5):983–993.
48. Rhee C, Kadri SS, Dekker JP, et al. Prevalence of antibiotic-resistant pathogens in culture-proven sepsis and outcomes associated with inadequate and broad-spectrum empiric antibiotic use. JAMA Netw Open. 2020;3(4):e202899. doi:10.1001/jamanetworkopen.2020.2899
49. Pavlovsky M, Press J, Peled NYP, Yagupsky P. Blood culture contamination in pediatric patients: young children and young doctors. Pediatr Infect Dis J. 2006;25(7):611–614. doi:10.1097/01.inf.0000220228.01382.88
50. Craven DE, Lichtenberg DA, Browne KF, Coffey DM, Treadwell TL. Pseudobacteremia traced to cross-contamination by an automated blood culture analyzer. Infect Control. 1984;5(2):75–78. doi:10.1017/s0195941700058987
51. Pearson ML, Pegues DA, Carson LA, O’Donnell R, Berger RH, Anderson RL. Cluster of Enterobacter cloacae pseudobacteremias associated with use of an agar slant blood culturing system. J Clin Microbiol. 1993;31(10):2599–2603. doi:10.1128/jcm.31.10.2599-2603.1993
52. Chaoui L, Mhand R, Mellouki F, Rhallabi N. Contamination of the surfaces of a health care environment by Multidrug-Resistant (MDR) bacteria. Int J Microbiol. 2019;2019:3236526. doi:10.1155/2019/3236526
53. Gudapuri L. Cross – resistance between antiseptic agents and antimicrobial agents. Biom Biostat Int J. 2018;7(5):429–430. doi:10.15406/bbij.2018.07.00242
54. Liu WJ, Fu L, Huang M, et al. Frequency of antiseptic resistance genes and reduced susceptibility to biocides in carbapenem-resistant Acinetobacter baumannii. J Med Microbiol. 2017;66(1):13–17. doi:10.1099/jmm.0.000403
55. Hall RT, Domenico HJ, Self WH, Hain PD. Reducing the blood culture contamination rate in a pediatric emergency department and subsequent cost savings. Pediatrics. 2013;131(1):e292–7. doi:10.1542/peds.2012-1030
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

