Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
MRI Features of Idiopathic Scrotal Calcinosis: A Case Report
Received 17 January 2023
Accepted for publication 14 March 2023
Published 27 March 2023 Volume 2023:16 Pages 743—747
DOI https://doi.org/10.2147/CCID.S405095
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Peng Huang,* Xinyu Zhu,* Li Guo
Department of Radiology, The Second Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Guo, Email [email protected]
Abstract: In this study, we report a case of idiopathic cutaneous calcium deposits in the scrotum diagnosed by imaging and pathology. A 31-year-old male presented 4 years ago with multiple nodules on the scrotal skin that had increased significantly in the past 2 years. MR showed mainly low signal nodular shadowing and diagnosed idiopathic cutaneous calcium deposits in the scrotum. To our knowledge, this is one of the rare diagnoses of the disease by imaging presentation.
idiopathic scrotal calcinosis, scrotum, MRI
Introduction
Idiopathic scrotal calcinosis (ISC) is a skin disorder caused by the restricted deposition of insoluble calcium salts in the scrotal skin of the human body. It was first described by Lewinski in 1883. It is a rare benign scrotal skin disorder that occurs in childhood or early adulthood and may not be associated with any systemic disorder of calcium and phosphorus metabolism. It presents as multiple asymptomatic skin-colored or yellow nodular plaques of variable size, single or multiple, can be scattered or fused into clusters, larger lesions can have a mild heaviness, some lesions can break down and become infected, discharging chalky contents, the disease is relatively rare. In previous clinical practice, the disease was not imaged, so it was also difficult to aid in diagnosis with specific imaging signs. Unlike in the past, in this study is a report covering clinical manifestations, MRI images and histology, and our report provides a great help in the diagnosis of this disease.
Idiopathic scrotal calcinosis (ISC) is a skin disorder caused by the restricted deposition of insoluble calcium salts in the scrotal skin of the human body. It was first described by Lewinski in 1883. It is a rare benign scrotal skin disorder that occurs in childhood or early adulthood and may not be associated with any systemic disorder of calcium and phosphorus metabolism. In previous clinical practise, the disease was not imaged, so it was also difficult to rely on specific imaging signs to aid in the diagnosis. In the present study, we report a 31-year-old man who presented 4 years ago with multiple nodules on the scrotal skin, the number of which had increased significantly in the past 2 years. MR mainly shows low signal nodal shadow, the diagnosis was idiopathic cutaneous calcium deposits in the scrotum (Written informed consent has been obtained from the patient). To our knowledge, this is one of the rare cases in which the diagnosis of the disease is made by imaging presentation.
Case
Male, 31 years old, presented to the clinic 4 years ago with multiple nodules on the scrotal skin. The patient was discovered to have multiple scrotal skin nodules by chance 4 years ago and their number had significantly increased in the past 2 years. Physical examination revealed multiple nodules of yellowish-white color scattered across the entire scrotal skin surface (Figure 1), with nodules of varying sizes, no obvious rupture, and negative tenderness. To further clarify the nature and extent of the lesions, ultrasound and MRI were performed. Ultrasound revealed many mildly hyperechoic nodules in the scrotal wall, the largest of which was about 1.2 cm×0.7 cm in diameter. Magnetic resonance imaging revealed diffuse thickening of the scrotal skin bilaterally, as well as multiple outpouching nodules with clear borders on the skin surface, the largest of which was about 1.2×0.9×0.6 cm in size and had a low signal in T1WI and T2WI, as enhancement of the well as peripheral fine line in the enhanced scan (Figures 2–4).
 |
Figure 1 Scattered yellowish-white nodules in the scrotal skin, varying in size, with clear boundaries. |
 |
Figure 2 MRI scan, transaxial position, T1WI bilateral intra-scrotal nodular shadow with low signal. |
 |
Figure 3 MRI scan, coronal position, T2WI bilateral intra-scrotal nodular shadow with low signal. |
 |
Figure 4 MRI in transaxial position with enhancement, the nodules show peripheral fine line enhancement. |
Surgery and Pathology
The patient underwent scrotal lesion excision under general anesthesia: a shuttle incision was made, the subcutaneous dartos was released, and the tumor was removed.
Postoperative Pathology
Multiple degenerative nodules with focal calcification and ossification were detected in the scrotal dermis on light microscopy, along with a minor infiltration of inflammatory cells (Figure 5). Idiopathic cutaneous calcium deposits of the scrotum are the pathological diagnosis.
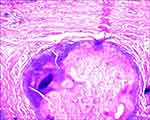 |
Figure 5 Multiple degenerative nodules with calcification and focal ossification were seen in the Microscope with a small amount of inflammatory cell infiltration (HE×200). |
Discussion
ISC is a skin disorder caused by the restricted deposition of insoluble calcium salts on the scrotal skin of the body.1 Lewinski was the first to describe it in 1883. It is a rare benign scrotal skin disease that strikes children or young adults and may not be accompanied by any systemic disorder of calcium and phosphorus metabolism.2 The etiology and pathogenesis of this disease are unknown, but it has been suggested that dystrophic, metastatic, idiopathic, medically induced, and calcific hypersensitivity are possible causes.3 The present case was considered idiopathic cutaneous calcinosis of the scrotum due to the absence of a clear etiology and a related medical history. A single or several calcified nodules of the scrotal skin, brownish or yellowish-white in color, with a sluggish progression in size and number, are the clinical manifestation of this condition. Most of them are asymptomatic, and some of the nodules cause pruritus in the corresponding areas of the skin.4
Implication
MR examination is radiation-free, non-invasive, can be multi-directional imaging, and better display of soft tissue lesions. In the present case, MRI showed multiple, well-defined nodular shadows throughout the scrotal skin with low signal on T1WI and T2WI, which corresponded to areas of subdermal calcium salt deposits in the scrotum when combined with the pathology; and fine linear enhancement shadows around the nodules on enhancement scans, which corresponded to the surrounding inflammatory areas. This suggests that MR examination can be helpful in the diagnosis of this disease and the exclusion of some lesions with a similar clinical presentation, such as steatocystoma multiplex of the scrotum (containing oily sebaceous material). Furthermore, imaging examinations can also help exclude other lesions in the scrotum and adjacent tissues and organs, thus guiding treatment.
Ethics Approval and Informed Consent
We have obtained informed patient consent and ethical approval (Ethics Committee of the Second Affiliated Hospital of Kunming Medical University).
Consent for Publication
Approval for the publication of the patient’s case details was obtained from the Second Affiliated Hospital of Kunming Medical University.
Informed Consent
The patient has signed the informed consent and agreed to publish it. He gave her consent for the publication of identifiable details, which can include photograph(s) and/or case history and/or details within the text to be published in the article. He confirmed that she have seen and been given the opportunity to read the article.
Author Contributions
All authors have the contributions:
1. Made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas.
2. Have drafted or written, or substantially revised or critically reviewed the article.
3. Have agreed on the journal to which the article will be submitted.
4. Reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage.
5. Agree to take responsibility and be accountable for the contents of the article.
Funding
This work was supported by the Medical discipline leader training project in Yunnan Province, D-2019024.
Disclosure
The authors report no competing interests in this work.
References
1. Chiummariello S, Figus A, Menichini G, et al. Scrotal calcinosis: a very rare multiple clinical presentation. Clin Exp Dermatol. 2009;34(8):e795–e797. doi:10.1111/j.1365-2230.2009.03524.x
2. Killedar MM, Shivani AA, Shinde U. Idiopathic scrotal calcinosis. Indian J Surg. 2016;78(4):329–330. doi:10.1007/s12262-016-1463-4
3. Reiter N, El-Shabrawi L, Leinweber B, et al. Calcinosis cutis: part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65(1):1–12. doi:10.1016/j.jaad.2010.08.038
4. Karaca M, Taylan G, Akan M, et al. Idiopathic scrotal calcinosis: surgical treatment and histopathologic evaluation of etiology. Urology. 2010;76(6):1493–1495. doi:10.1016/j.urology.2010.02.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
