Back to Journals » Psychology Research and Behavior Management » Volume 17
Motivational Interviewing as a Tool to Increase Motivation and Adherence to a Long COVID Telerehabilitation Intervention: Secondary Data Analysis from a Randomized Clinical Trial
Authors León-Herrera S , Oliván-Blázquez B, Samper-Pardo M, Aguilar-Latorre A , Sánchez Arizcuren R
Received 4 August 2023
Accepted for publication 26 November 2023
Published 13 January 2024 Volume 2024:17 Pages 157—169
DOI https://doi.org/10.2147/PRBM.S433950
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Sandra León-Herrera,1,2 Bárbara Oliván-Blázquez,1,2 Mario Samper-Pardo,3 Alejandra Aguilar-Latorre,1,2 Rafael Sánchez Arizcuren4
1Institute for Health Research Aragón (IIS Aragón), Zaragoza, Spain; 2Department of Psychology and Sociology, University of Zaragoza, Zaragoza, Spain; 3Department of Health Sciences, University of Zaragoza, Zaragoza, Spain; 4Department of Physiatry and Nursing, University of Zaragoza, Zaragoza, Spain
Correspondence: Bárbara Oliván-Blázquez, C. Violante de Hungría, 23, Zaragoza, 50009, Spain, Tel +34 622719759, Email [email protected]
Background: Although motivational interviewing was originally developed to address abuse disorders, scientific evidence confirms that it is an increasingly used and effective approach in a wide range of therapeutic interventions. To date, however, no studies have analyzed the use of this tool in patients with persistent symptoms following coronavirus disease 2019, a condition known as Long COVID.
Purpose: To analyze the effectiveness of motivational interviewing with regard to the adherence to telerehabilitation for Long COVID using a mobile application. As a secondary objective, factors related to greater motivation before and after the motivational interviewing techniques were analyzed.
Patients and Methods: This longitudinal design substudy used a sample of 52 adult patients with Long COVID participating in the intervention group of a randomized clinical trial. This trial examined the effectiveness of a telerehabilitation program for this population using a mobile application. This program included three motivational interviews to achieve maximum treatment adherence. In this study, the main variables were motivation and adherence to application use. Sociodemographic and clinical data, personal constructs, and affective state were also collected. Subsequently, a descriptive, correlational, and regression statistical analysis was performed using the SPSS Statistics program.
Results: The median motivation prior to the first motivational interview was 8 (IQR 2), the median at the end of the last motivational interview was 8.5 (IQR 2.75), and the change in motivation levels after the three motivational interviews was 0.5 (IQR 1). Affective state and final motivation scores were predictors of greater adherence to telerehabilitation treatment.
Conclusion: A high level of motivation after participating in motivational interviewing appears to be related to higher levels of adherence to telerehabilitation in patients with Long COVID. This suggests that motivational interviewing may be an effective tool in the treatment of this disease.
Keywords: motivational interviewing, Long COVID, telerehabilitation, motivation, personal constructs, affective state
Background
As the global coronavirus disease 2019 (COVID-19) pandemic has progressed, evidence has emerged showing that while most people infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) return to their pre-illness baseline within several weeks, some people suffer long-lasting and persistent multi-organ COVID symptoms, which could range from mildly distressing to significantly interfering with essential daily activities.1,2 The term Long COVID (or post-COVID syndrome or Long-haul COVID-19) has begun to gain recognition in the scientific and medical community, with various descriptions of the same having been proposed, the most common of which being “symptoms that last more than three months after the disease onset”.1 The diverse clinical spectrum of Long COVID includes respiratory, physical, neurocognitive, and psychological symptoms.2,3
Medical experts are making every possible effort to manage Long COVID patients. Although several guidelines have been published on the management of this disease, a large practical gap remains and treatment options are limited.4–6 Like all long-term conditions, it impacts numerous aspects of life and is best managed holistically, considering physical, psychological, and social factors.7 Therefore, treatment requires a multidisciplinary approach.8 The multisystemic damages suffered by these individuals may lead to health conditions causing major functional deterioration, notable affectation of emotional well-being, and a decreased quality of life. For this reason, although there is currently no established treatment for this syndrome, adequate patient support and the creation of a positive relationship are essential for recovery.2,5,9
Medical care increasingly focuses on addressing long-term conditions such as Long COVID syndrome. In this type of intervention, motivational aspects are an essential factor, since oftentimes, patients face lifestyle changes in an attempt to modify risk factors and optimize adherence to medical advice.10,11 Adherence has been defined as the degree to which a person’s behavior (in terms of taking medications, exercising, following a diet, and other lifestyle changes) is consistent with health or medical advice.12 In other words, it refers to how the patient follows the treatment plan prescribed by their healthcare provider.13
Promotion of treatment adherence is difficult to achieve,14 with certain factors such as emotional problems (eg, depression and anxiety) or those related to personal constructs (poor health literacy, limited patient activation, or low perceived self-efficacy) increasing this difficulty.15–18 Health literacy (HL), defined as the degree to which patients are able to acquire, process, and understand the necessary information to make appropriate decisions about their health, is an important determinant of adherence since a low HL level predicts poor clinical outcomes.19–21 However, while HL plays a relevant role, other factors should also be considered when addressing non-adherence, such as patient activation.22 An activated patient has the necessary skills, knowledge, and motivation to manage their own health.23,24 Highly activated patients consider their role in managing their own health to be crucial and have the confidence and knowledge to act appropriately to maintain and improve their health.25 Furthermore, the patient’s perception of self-efficacy, defined as one’s self-belief in the ability and confidence to successfully perform a task or change behavior, is an important factor explaining adherence to health behaviors.26,27
A lack of adherence may result in a reduction in treatment effectiveness and, therefore, more serious health problems, as well as financial and social costs.28 Traditional counseling and education-based intervention alone are not sufficiently effective in increasing patient adherence to evidence-based lifestyle modifications. There is an urgent need for an innovative approach that promotes health-related behavioral changes at an individual level, reducing the development of a disease or improving the management and control of other diseases.29
Motivational Interviewing (MI) is a tool used with increasing frequency to elicit motivation for change from the individuals themselves, as opposed to change imposed by healthcare providers.30 The MI approach was created by William Miller in 1983 help people with alcohol problems to modify their behavior.31 This concept was further advanced in the 1990s, being described as “a collaborative conversation style for strengthening a person’s own motivation and commitment to change”.32
Miller and Rollnick outlined five basic principles to guide MI: express empathy, develop discrepancy, avoid argumentation, overcome resistance, and support self-efficacy.33 That is, this approach encourages providers to be collaborative, preventing resistance, eliciting the patient’s own motivation for change, and focusing their attention on resources and planning to make and achieve these changes.12 Therefore, it requires the professional to act as an equal partner with the client and refrain from offering unrequested advice, instructions, confrontations, or warnings. It is not a way to “get people to make changes” or a set of techniques to force a conversation.34
Although originally developed to address abuse disorders, over 120 research studies have provided evidence confirming that this is an increasingly implemented, useful, and effective approach in a wide range of therapeutic interventions, including brief encounters.34,35 Currently, however, no studies have analyzed the use of this tool in Long COVID patients.
Hence, the objective of this study was to examine the effectiveness of MI on adherence to telerehabilitation for individuals diagnosed with Long COVID using a mobile application (APP). As a secondary objective, factors related to increased motivation before and after the MI were analyzed.
Methodology
Design
This is a longitudinal study analyzing sociodemographic and clinical data. The findings have been reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (Guidelines for reporting observational studies, Supplementary Material).36
This research is also a sub-study, given that it relies on a sample of patients who make up the intervention group of a Randomized Clinical Trial (RCT). The main objective of the RCT was to analyze the effectiveness and profitability of a telerehabilitation treatment program using an APP offering therapeutic recommendations and exercises (own development), to improve the symptoms and quality of life of patients with Long COVID, in addition to other secondary variables.37,38
Participant Recruitment
Most of the recruitment was performed by healthcare professionals from Primary Health Care (PHC) consultations, but members from the Long COVID Association of Aragón (Spain) also participated. Patients meeting the inclusion criteria were approached, provided their consent, and were included in the study. Recruitment was carried out between January and March 2022, until reaching the sample size.
Participants and Sample Size
All of the study participants were patients diagnosed with Long COVID,39 of legal age (18 years or older), and treated by Primary Health Care (PHC) in the Autonomous Community of Aragón (Spain). This study implemented the exclusion criteria established in the clinical trial: not having a positive COVID-19 diagnosis in at least the past 3 months; participation in a clinical trial over the past six months; engaging in rehabilitative or psychotherapeutic treatment structured by health professionals; having a diagnosis of severe uncontrolled disease; significant risk of suicide; being pregnant or in a period of lactation; and the presence of any medical, psychological, or social problem that may significantly interfere with the patient’s participation in the study.
The study sample consisted of 52 participating subjects. This was a sub-sample of the clinical trial, in which a minimum sample size of 78 subjects was estimated, and 100 participating subjects were finally recruited. The 52 participants in this study were those forming the clinical trial’s intervention group.
Intervention
The intervention group of the original study attended 3 sessions based on the MI methodology, in order to reinforce the individual´s motivation and commitment to the telerehabilitation process in which he/she was going to participate. To do so, the research team, along with professionals from the field of motivation, created potential model guides for these patients, their problems, and their needs.
The motivational methodology proposed by Miller and Rollnick (3rd ed.) was followed, considering four basic processes involved in the flow of MI: linking the patient to the therapeutic process, focusing the process on a specific purpose, evoking the patient’s own motivations to engage in the process-change and planning what and how to do this. Furthermore, the fundamental aspects found in all interventions were collaboration, acceptance, compassion, and evocation.40
The first two sessions were held individually and the third was held in a group. All sessions were guided by one of the project researchers, who had prior training and experience in MI. The individual sessions lasted approximately 20–25 minutes for each patient. Group sessions lasted approximately 50 minutes and were conducted with a minimum of eight and a maximum of twelve participants. Therefore, each participant participated in two individual sessions and one group session for 3 consecutive weeks, with one session per week.
In the first session, the phases of linking, focusing, and evoking were developed, through patient presentation, APP installation, and initial use of the same. In the second session, after having used the APP for one week, the planning phase was carried out, referring to the personalized rehabilitation treatment to be undergone over the upcoming 3 months. The purpose of the third and final intervention, which was developed in groups, was to mutually reinforce the maintenance discourse and the theme revolving around patient emotional well-being and the exchange of “tricks” to improve their physical and mental health by using distinct community resources that were available to them (aspects considered in the process rehabilitated through the APP).
Outcomes and Measures
Primary Outcomes
The main study variables were adherence to the telerehabilitation APP and motivation before and after the MI.
“Adherence” refers to the degree to which a patient’s behavior regarding medication or lifestyle changes is consistent with therapeutic recommendations.41 In this study, adherence was measured in terms of the time of use of the mobile APP. To do this, the seconds of use of the APP were recorded over the three months in which the telerehabilitation intervention took place using this device.
“Motivation” is defined as the process by which goal-directed activities or behaviors are initiated and sustained. It is a determining factor in the success of interventions, specifically behavioral ones.42 In this study, a personal registration form was prepared, to be completed in each of the sessions. In this file, among other variables, the degree of motivation at the beginning and end of the motivational intervention was collected, using a 0–10 Visual Analogue Scale (VAS).
Secondary Outcomes
Age, gender, marital status, educational level, occupational status, and economic income were collected.
The date of contracting COVID-19 and the number and severity of persistent symptoms measured by the Visual Analog Scale43 were collected. These symptoms include general, gastrointestinal, urinary, neurological, and other symptoms that the participants considered persistent.44–46
The affective state was assessed using the Hospital Anxiety and Depression Scale (HADS) questionnaire, a self-report-based scale designed to screen for depression and anxiety disorders in primary care settings. It includes 14 items, assessing symptoms of anxiety (HADS-A) and depression (HADS-D), with each item corresponding to a 4-point (zero to three) scale. The total score ranges from 0 to 21 for symptoms of both anxiety and depression, and higher scores indicate more severe symptoms.47
The Health Literacy Europe Questionnaire (HLS-EUQ16) measured the participant’s health literacy. Health literacy is defined as the population’s motivation, knowledge, and individual understanding and the ability to make decisions regarding the promotion and maintenance of their health.48 This questionnaire is made up of 16 items, scored between 1 (very easy) and 4 (very difficult). The total score is obtained by calculating the sum of the 16-item scores. It can be transformed into a dichotomous response: very difficult and difficult =0; or easy and very easy =1. Higher scores indicate worse health literacy.49
Self-efficacy was measured with the Self-Efficacy Scale-12 (GSES12).50 This scale evaluates three factors: willingness to initiate the behavior (“Initiative”), willingness to strive to complete the behavior (“Effort”), and persistence in the face of adversity (“Persistence”). The original scale consisted of 17 items, scored on a 5-point Likert-type scale. Five items, however, were excluded due to low item-rest correlations and ambiguous wording, resulting in a 12-item version of the scale (GSES12).51
Patients’ activation on their own health was measured using the Patient Activation Measure (PAM). This instrument evaluates the skills, knowledge, and confidence that patients perceive when engaging in health-related self-management activities. It consists of 13 items measured using a Likert Scale from one (totally disagree) to four (totally agree). The total score ranges from 13 to 52, with higher scores indicating higher activation levels.52
Table 1 summarizes the description of the outcomes, as well as the measurement times.
 |
Table 1 Outcomes Description and Measurement Times |
Statistical Analysis
Statistical analyses were conducted using the IBMR SPSSR Statistics version 22.0.0.0 software and Microsoft Excel. First, the sample distribution was analyzed using non-parametric statistics, obtaining Shapiro–Wilk statistic values below 0.05. Subsequently, a descriptive analysis was performed (frequencies and percentages for categorical variables; median and interquartile range for continuous variables). Next, a bivariate analysis was performed. The degree of participant motivation was analyzed as a quantitative variable. Correlations were evaluated with Spearman’s Rho statistic between the initial, final motivation, and the change in motivation, and the rest of the variables. A linear regression model was developed to analyze factors related to adherence to the APP intervention (seconds of use). Gender, age, self-efficacy (GSES12), health literacy (HLS-EUQ16), patient activation (PAM), number of symptoms, and final motivation were introduced into this model. Linear regression was used since the residuals of the model had a finite mean, constant variance, and normal distribution. However, a bootstrapping analysis with 2000 samples was also conducted. All significance levels were set at 0.05.
Ethical Considerations
Ethical approval was granted by the Clinical Research Ethics Committee of Aragón (Spain) (PI21/454). The procedures carried out for the production of this work were adjusted to the ethical standards of the aforementioned committee and were in accordance with the 1975 Declaration of Helsinki.53 All subjects signed a written informed consent form; their data were anonymized and used only for research purposes. Clinical Trial Registration: ISRCTN registry ISRCTN91104012.
Results
Of the 52 participants, 44 were women (84.6%) and 8 were men (15.4%). The median age was 47 years (IQR 14.5 years, range: 39.5–54). Table 2 below presents a description of the total sample. The sample profile was female, married, aged approximately 47 years, with secondary or university studies, in active employment (income 1–2 the MIS), or temporary work incapacity. The median number of persistent symptoms was 18 (IQR 6.7).
 |
Table 2 Description of Sociodemographic and Clinical Variables of the Total Sample |
As for patient motivation levels, the initial motivation median was 8 (IQR 2), the final one (at the end of the MI) was 8.5 (IQR 2.75), and the changes in motivation levels after conducting the motivational intervention was 0.5 (IQR 1).
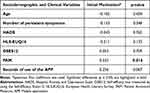
Table 3 shows the bivariate analysis related to the initial motivation score and the other variables collected. A relationship exists between the initial motivation level (at the onset of the motivational intervention) and the patient activation scores with regard to their health care (PAM). The analysis also added the variable seconds of use of the APP to analyze the relationship between initial motivation and adherence to the intervention. In this case, no significant relationship is found.
Table 4 shows the bivariate analysis related to the final motivation score, that is, after the motivational intervention, and the rest of the variables collected. The variable seconds of use of the APP is also added to analyze the relationship between final motivation and intervention adherence. The results suggest a relationship between the final motivation and the time of use of the APP, that is, adherence to the intervention. The greater the motivation after the interview, the greater the time devoted to the intervention. The final motivation is also related to age.
Table 5 shows the bivariate analysis related to the range of change between the initial and final motivation after having completed the motivational intervention and the rest of the variables collected. The results show that the change in motivation is related to the time of use of the APP, that is, with adherence to the intervention. Again, a relationship with age is found to exist.
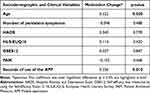
In order to respond to the general study objective, adherence (seconds of use of the APP) was included in the multivariate analysis as a dependent variable, and was analyzed together with the other study variables. The multivariate analysis is shown in Table 6. The affective state (b = 3071.20; p < 0.05) and the level of final motivation, after the motivational intervention (b = 6259.87; p < 0.05), are predictors of greater adherence to the APP intervention (greater number of seconds of time of use of the APP). This model explains 30% of the overall variance [R2 adjusted=0.308, F(8,43) = 3.842, p= 0.002].
Discussion
To the best of our knowledge, this is the first study examining the use of MI as a tool in a telerehabilitation intervention for Long COVID patients. Specifically, it has been carried out on individuals from an intervention group within a clinical trial in which the effectiveness of the mobile APP is analyzed as a telerehabilitation tool for this population.37
The results of this study show that MI is an effective tool for increasing adherence to the intervention in patients diagnosed with Long COVID, since a higher score on the final motivation scale (ie, after the development of the three motivational intervention sessions) was associated with more seconds of APP use. In addition, in the bivariate analysis, it was also observed that the change in motivation levels after the interviews was related to said adherence. Existing scientific evidence has stated that one of the main functions of MI is to increase personal motivation and commitment,11 and some studies have confirmed that the use of this technique achieves not only change but also the maintenance of positive health behaviors, such as smoking cessation, weight loss, or increased physical activity.54,55
Although the Long COVID management guidelines continue to evolve as new scientific evidence emerges, symptom-oriented approaches continue to be adopted in routine clinical practice.5,56 Some studies have already confirmed the positive impact of the use of MI on health-promoting behaviors related to symptom management for distinct pathologies.57–62 In our study, the APP in which MI was applied used this same approach, offering recommendations and exercises related to physical activity, respiratory rehabilitation, cognitive stimulation, the Mediterranean diet, sleep hygiene, and community resources.
Long COVID is still considered a new and unknown disease,63 and treatment options remain limited,4–6 leading patients suffering from this disease to feel frustrated when seeking treatment, willing to try anything to control and manage their symptoms and recover their highly deteriorated quality of life.64,65 This could explain the high levels of motivation at the beginning of our study.
This motivation to be proactive in disease management is also related to patient activation.66 This positive relationship between the level of patient activation and the degree of motivation at the onset of the motivational intervention is reflected in our study. However, patient activation is no longer significantly related to motivation at the end of the intervention, nor to the change in motivation levels throughout the sessions. These findings could be due to the fact that MI may be less useful in patients with a greater disposition, as Hettema et al previously described.67
In the case of the other two personal constructs measured in our study, health literacy, and self-efficacy perception, no significant relationships or associations were observed in the correlation and regression models. Therefore, the effects of MI use on these constructs cannot be determined and further studies on this population type are necessary. Scientific evidence does however reveal a positive and significant relationship between health literacy and adherence to treatment.68–71 Understanding is a motivating factor for patients since the more they know and understand their situation, the greater the need to change it.72 Regarding the perception of self-efficacy, studies have related it to health-associated behaviors, specifically to promotional activities, such as communication with health professionals or adaptation and adherence to disease treatment.73–75
In our correlation analyses, age was also a significant factor. According to our results, older people presented higher levels of final motivation, as well as a greater change in motivation levels throughout the motivational intervention. These results are in line with the findings of Lundahl et al in their meta-analysis on the use of MI, determining that a significant association exists between studies with older participants and better results of MI.76
In addition to the previously mentioned personal constructs, the affective state of the participants was also measured. A growing number of studies have confirmed a negative emotional impact of Long COVID.9 Scientific evidence reveals that the presence of depression and anxiety can cause deficits in motivation and impair adherence to treatment for different diseases.15,77–81 In this study, however, the opposite was observed. A significant relationship was found between higher levels of depression and anxiety and increased adherence. A priori, this may appear to be a contradictory result, but it should be noted that our sample did not have a high score on the HADS Scale (mean and median of 17 points out of a total of 42). These scores do not suggest levels of depression and anxiety that are high enough to do nothing due to their mood, but they are sufficiently high to seek solutions. Therefore, the level of anxiety could be a cause of patient activation. Strack et al previously stated that, although in most cases anxiety is considered a debilitating factor, it may also be a source of energy, activating fighting stress and causing an excitement that facilitates performance and effort in the face of challenges.82
Limitations and Future Research Directions
To date, no past studies have investigated the use of MI as a tool in telerehabilitation interventions for Long COVID patients. It is therefore a novel study that sheds light on a complex and heterogeneous pathology. However, this study has certain limitations. On the one hand, baseline motivation scores were found to be high, with a significantly low change in scores from the baseline until the end of the motivational intervention. For this reason, it was decided to evaluate the effectiveness of the motivational interview by including the final motivation within the regression model, and not the change in motivation. On the other hand, the type of persistent symptomatology has not been considered in depth, only the number of symptoms. The type of prevalent symptoms (physical, cognitive, respiratory, etc.) could be an influential factor in motivation levels. This issue may be explored in future studies.
Conclusion
In conclusion, a high level of motivation after conducting a MI appears to be related to higher levels of adherence to interventions by Long COVID patients, and MI seems to be an effective tool for interventions with this type of population. Although it is true that this is a highly motivated population seeking solutions for this new disease that is significantly reducing their quality of life.
Abbreviations
HL, Health Literacy; MI, Motivational Interviewing; APP, Application; PHC, Primary health care; VAS, Visual Analogue Scale; HADS, Hospital Anxiety and Depression Scale; HADS-A, Hospital Anxiety and Depression Scale – anxiety subscale; HADS-D, Hospital Anxiety and Depression Scale – depression subscale; HLS-EUQ16, European Health Literacy Survey Questionnaire; GSES12, Self-Efficacy Scale-12; PAM, Patient Activation Measure; MIS, Minimum Interprofessional Salary; IQR, Interquartile range; N, Sample; M, Mean; Me, Median; SD, Standard Deviation.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval and Consent to Participate
Ethical approval was granted by the Ethics Committee for Clinical Research of Aragón (Spain) (PI21/454). All of the procedures carried out in this work complied with the Ethical standards of this Committee and with the Declaration of Helsinki of 1975.53 All participants signed an informed consent form, and their data were anonymized and were only used for the purposes of the study.
Acknowledgments
We wish to thank the Aragon Primary Care Research Group (GAIAP, B21_23R), part of the Department of Innovation, Research and University in the Government of Aragon (Spain), and the Aragon Institute for Health Research (IIS Aragon); the Research Network on Chronicity, Primary Care, and Health Promotion (RICAPPS, RD21/0016/0005), which is part of the Results-Oriented Cooperative Research Networks in Health (RICORS) (Carlos III Health Institute); and Feder Funds “Another way to make Europe”.
Author Contributions
All authors made a significant contribution to the work, either in its conception, study design, execution, data acquisition, analysis, and interpretation, or in all of these areas; participated in drafting, revising, or critically reviewing the article; provided final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This work has been supported by the Carlos III Health Institute, grant number PI21/01356, FEDER Funds “Another way to make Europe”. The funders have no role in study design, data collection, analysis, decision to publish, or manuscript preparation. The funding organization will conduct an annual audit.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. 2021;53(10):737–754. doi:10.1080/23744235.2021.1924397
2. Ceban F, Leber A, Jawad MY, et al. Registered clinical trials investigating treatment of long COVID: a scoping review and recommendations for research. Infect Dis. 2022;54(7):467–477. doi:10.1080/23744235.2022.2043560
3. Rodriguez-Sanchez I, Rodriguez-Mañas L, Laosa O. Long COVID-19: the need for an interdisciplinary approach. Clin Geriatr Med. 2022;38(3):533–544. doi:10.1016/J.CGER.2022.03.005
4. Aiyegbusi OL, Hughes SE, Turner G, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114(9):428–442. doi:10.1177/01410768211032850
5. Koc HC, Xiao J, Liu W, Li Y, Chen G. Long COVID and its management. Int J Biol Sci. 2022;18(12):4768–4780. doi:10.7150/IJBS.75056
6. Yelin D, Moschopoulos CD, Margalit I, et al. ESCMID rapid guidelines for assessment and management of long COVID. Clin Microbiol Infect. 2022;28(7):955–972. doi:10.1016/J.CMI.2022.02.018/ATTACHMENT/52310673-5E83-429A-A10B-E1F27B4A70BA/MMC1.DOCX
7. Nurek M, Rayner C, Freyer A, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. Br J Gen Pract. 2021;71(712):E815–E825. doi:10.3399/BJGP.2021.0265
8. Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–875. doi:10.1016/J.DSX.2021.04.007
9. Samper-Pardo M, Oliván-Blázquez B, Magallón-Botaya R, Méndez-López F, Bartolomé-Moreno C, León-Herrera S. The emotional well-being of Long COVID patients in relation to their symptoms, social support and stigmatization in social and health services: a qualitative study. BMC Psychiatry. 2023;23(1):68. doi:10.1186/S12888-022-04497-8/FIGURES/1
10. Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93(2):157–168. doi:10.1016/J.PEC.2013.07.012
11. Bischof G, Bischof A, Rumpf H-J. Motivational interviewing: an evidence-based approach for use in medical practice. Dtsch Arztebl Int. 2021;118(7):109–115. doi:10.3238/ARZTEBL.M2021.0014
12. Stonerock GL, Blumenthal JA. Role of counseling to promote adherence in healthy lifestyle medicine: strategies to improve exercise adherence and enhance physical activity. Prog Cardiovasc Dis. 2017;59(5):455–462. doi:10.1016/J.PCAD.2016.09.003
13. Salvo MC, Cannon-Breland ML. Motivational interviewing for medication adherence. J Am Pharm Assoc. 2015;55(4):e354–e363. doi:10.1331/JAPHA.2015.15532
14. Beauvais C. Motivational interviewing to improve treatment adherence. Joint Bone Spine. 2019;86(5):535–537. doi:10.1016/J.JBSPIN.2019.02.005
15. Volpato E, Toniolo S, Pagnini F, Banfi P. The relationship between anxiety, depression and treatment adherence in chronic obstructive pulmonary disease: a systematic review. Int J Chron Obstruct Pulmon Dis. 2021;16:2001–2021. doi:10.2147/COPD.S313841
16. Magallón-Botaya R, Méndez-López F, Oliván-Blázquez B, Carlos Silva-Aycaguer L, Lerma-Irureta D, Bartolomé-Moreno C. Effectiveness of health literacy interventions on anxious and depressive symptomatology in primary health care: a systematic review and meta-analysis. Front Public Health. 2023;11. doi:10.3389/FPUBH.2023.1007238
17. Méndez-López F, Oliván-Blázquez B, Domínguez-García M, Bartolomé-Moreno C, Rabanaque I, Magallón-Botaya R. Protocol for an observational cohort study on psychological, addictive, lifestyle behavior and highly prevalent affective disorders in primary health care adults. Front Psychiatry. 2023;14. doi:10.3389/FPSYT.2023.1121389
18. Selçuk-Tosun A, Zincir H. The effect of a transtheoretical model-based motivational interview on self-efficacy, metabolic control, and health behaviour in adults with type 2 diabetes mellitus: a randomized controlled trial. Int J Nurs Pract. 2019;25(4). doi:10.1111/IJN.12742
19. Schönfeld MS, Pfisterer-Heise S, Bergelt C. Self-reported health literacy and medication adherence in older adults: a systematic review. BMJ Open. 2021;11(12):e056307. doi:10.1136/bmjopen-2021-056307
20. Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: a randomized controlled trial. Patient Educ Couns. 2020;103(2):336–342. doi:10.1016/j.pec.2019.08.028
21. Yeung DL, Alvarez KS, Quinones ME, et al. Low–health literacy flashcards & mobile video reinforcement to improve medication adherence in patients on oral diabetes, heart failure, and hypertension medications. J Am Pharm Assoc. 2017;57(1):30–37. doi:10.1016/j.japh.2016.08.012
22. Hyvert S, Yailian AL, Haesebaert J, et al. Association between health literacy and medication adherence in chronic diseases: a recent systematic review. Int J Clin Pharm. 2023;45(1):38–51. doi:10.1007/s11096-022-01470-z
23. Skolasky RL, Mackenzie EJ, Wegener ST, Riley LH. Patient activation and adherence to physical therapy in persons undergoing spine surgery. Spine. 2008;33(21):E784–E791. doi:10.1097/BRS.0b013e31818027f1
24. Graffigna G, Barello S, Bonanomi A. The role of Patient Health Engagement Model (PHE-model) in affecting patient activation and medication adherence: a structural equation model. PLoS One. 2017;12(6):e0179865. doi:10.1371/journal.pone.0179865
25. Paukkonen L, Oikarinen A, Kähkönen O, Kaakinen P. Patient activation for self‐management among adult patients with multimorbidity in primary healthcare settings. Health Sci Rep. 2022;5(4). doi:10.1002/hsr2.735
26. Xie Z, Liu K, Or C, Chen J, Yan M, Wang H. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health. 2020;20(1):1227. doi:10.1186/s12889-020-09274-4
27. Daniali S, Darani F, Eslami A, Mazaheri M. Relationship between self-efficacy and physical activity, medication adherence in chronic disease patients. Adv Biomed Res. 2017;6(1):63. doi:10.4103/2277-9175.190997
28. Levensky ER, Forcehimes A, O’Donohue WT, Beitz K. Motivational interviewing: an evidence-based approach to counseling helps patients follow treatment recommendations. Am J Nurs. 2007;107(10):50–58. doi:10.1097/01.NAJ.0000292202.06571.24
29. Fortune J, Breckon J, Norris M, Eva G, Frater T. Motivational interviewing training for physiotherapy and occupational therapy students: effect on confidence, knowledge and skills. Patient Educ Couns. 2019;102(4):694–700. doi:10.1016/J.PEC.2018.11.014
30. Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12(9):709–723. doi:10.1111/J.1467-789X.2011.00892.X
31. Miller WR. Motivational Interviewing with Problem Drinkers. Behavioural Psychotherapy. 1983;11(2):147–172. doi:10.1017/S0141347300006583
32. Frost H, Campbell P, Maxwell M, et al. Effectiveness of Motivational Interviewing on adult behaviour change in health and social care settings: a systematic review of reviews. PLoS One. 2018;13(10). doi:10.1371/JOURNAL.PONE.0204890
33. Miller WR, Rollnick S. Motivational interviewing: preparing people for change; 1991. Available from: https://psycnet.apa.org/record/2002-02948-000.
34. Prescott DS. Motivational interviewing: as easy as it looks? Curr Psychiatry Rep. 2020;22(7). doi:10.1007/S11920-020-01158-Z
35. Lundahl B, Droubay BA, Burke B, et al. Motivational interviewing adherence tools: a scoping review investigating content validity. Patient Educ Couns. 2019;102(12):2145–2155. doi:10.1016/J.PEC.2019.07.003
36. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi:10.1016/S0140-6736(07)61602-X
37. Samper-Pardo M, León-Herrera S, Oliván-Blázquez B, et al. Development and validation of a mobile application as an adjuvant treatment for people diagnosed with long COVID-19: protocol for a co-creation study of a health asset and an analysis of its effectiveness and cost-effectiveness. Int J Environ Res Public Health. 2022;20(1):462. doi:10.3390/IJERPH20010462
38. Samper-Pardo M, León-Herrera S, Oliván-Blázquez B, Méndez-López F, Domínguez-García M, Sánchez-Recio R. Effectiveness of a telerehabilitation intervention using ReCOVery APP of long COVID patients: a randomized, 3-month follow-up clinical trial. Sci Rep. 2023;13:7943. doi:10.1038/s41598-023-35058-y
39. World Health Organization. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021. World Health Organization; 2021.
40. Miller WR, Rollnick S. La Entrevista Motivacional. Ayudar a Las Personas a Cambiar [Motivational Interviewing: Helping People Change and Grow].
41. World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
42. Medalia A, Saperstein A. The role of motivation for treatment success. Schizophr Bull. 2011;37(suppl 2):S122–S128. doi:10.1093/schbul/sbr063
43. Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8(12):1153–1157. doi:10.1111/J.1553-2712.2001.TB01132.X
44. Vaes AW, Machado FVC, Meys R, et al. Care dependency in non-hospitalized patients with COVID-19. J Clin Med. 2020;9(9):2946. doi:10.3390/jcm9092946
45. Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi:10.1136/bmj.m3026
46. National Health Service (NHS). Long-term effects of coronavirus (long COVID). London, UK: National Health Service; 2022. Available from: https://www.nhs.uk/conditions/coronavirus-covid-19/long-term-effects-of-coronavirus-long-covid/.
47. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
48. Nolasco A, Barona C, Tamayo-Fonseca N, et al. Alfabetización en salud: propiedades psicométricas del cuestionario HLS-EU-Q16 [Health literacy: psychometric behaviour of the HLS-EU-Q16 questionnaire]. Gac Sanit. 2018;34(4):399–402. Spanish. doi:10.1016/J.GACETA.2018.08.006
49. Sørensen K, Pelikan JM, Röthlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. 2015;25(6):1053–1058. doi:10.1093/eurpub/ckv043
50. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self-Efficacy Scale: construction and Validation. Psychol Rep. 1982;51(2):663–671. doi:10.2466/pr0.1982.51.2.663
51. Woodruff SL, Cashman JF. Task, domain, and general efficacy: a reexamination of the Self-Efficacy Scale. Psychol Rep. 1993;72(2):423–432. doi:10.2466/PR0.1993.72.2.423
52. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4p1):1005–1026. doi:10.1111/j.1475-6773.2004.00269.x
53. World Medical Association. World Medical Association Declaration of Helsinki. JAMA. 2013;310(20):2191. doi:10.1001/jama.2013.281053
54. N J, van L I, N M, V H, van W T, van D S. Do trained practice nurses apply motivational interviewing techniques in primary care consultations? J Clin Med Res. 2012;4(6). doi:10.4021/JOCMR1120W
55. Movahedi M, Khamseh F, Ebadi A, Hajiamini Z, Navidian A. Comparison of group motivational interviewing and multimedia education on elderly lifestyle. J Educ Health Promot. 2018;7(1):133. doi:10.4103/JEHP.JEHP_59_18
56. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid—mechanisms, risk factors, and management. BMJ. 2021;374. doi:10.1136/BMJ.N1648
57. Davoli AM, Broccoli S, Bonvicini L, et al. Pediatrician-led motivational interviewing to treat overweight children: an RCT. Pediatrics. 2013;132(5):e1236–e1246. doi:10.1542/PEDS.2013-1738
58. Harman K, MacRae M, Vallis M, Bassett R. Working with people to make changes: a behavioural change approach used in chronic low back pain rehabilitation. Physiother Can. 2014;66(1):82. doi:10.3138/PTC.2012-56BC
59. Mckenzie K, Chang YP. The effect of nurse-led motivational interviewing on medication adherence in patients with bipolar disorder. Perspect Psychiatr Care. 2015;51(1):36–44. doi:10.1111/PPC.12060
60. Jung MJ, Jeong Y. Motivation and self-management behavior of the individuals with chronic low back pain. Orthop Nurs. 2016;35(5):330–337. doi:10.1097/NOR.0000000000000233
61. Iles RA, Taylor NF, Davidson M, O’Halloran P. An effective coaching intervention for people with low recovery expectations and low back pain: a content analysis. J Back Musculoskelet Rehabil. 2014;27(1):93–101. doi:10.3233/BMR-130424
62. Dashti A, Yousefi H, Maghsoudi J, Etemadifar M. The effects of motivational interviewing on health promoting behaviors of patients with multiple sclerosis. Iran J Nurs Midwifery Res. 2016;21(6):640. doi:10.4103/1735-9066.197682
63. Wah K, Id F, Baye F, Baik SH, Zheng Z, Mcdonald CJ. Prevalence and characteristics of long COVID in elderly patients: an observational cohort study of over 2 million adults in the US. PLoS Med. 2023;20(4):e1004194. doi:10.1371/JOURNAL.PMED.1004194
64. Brown K, Yahyouche A, Haroon S, Camaradou J, Turner G. Long COVID and self-management. Lancet. 2022;399(10322):355. doi:10.1016/S0140-6736(21)02798-7
65. Samper-Pardo M, León-Herrera S, Oliván-Blázquez B, Gascón-Santos S, Sánchez-Recio R. Clinical characterization and factors associated with quality of life in Long COVID patients: secondary data analysis from a randomized clinical trial. PLoS One. 2023;18(5):e0278728. doi:10.1371/JOURNAL.PONE.0278728
66. Al Juffali L, Almalag HM, Alswyan N, et al. The patient activation measure in patients with rheumatoid arthritis: a systematic review and cross-sectional interview-based survey. Patient Prefer Adherence. 2022;16:2845–2865. doi:10.2147/PPA.S379197
67. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi:10.1146/ANNUREV.CLINPSY.1.102803.143833
68. Lor M, Koleck TA, Bakken S, Yoon S, Dunn Navarra AM. Association between health literacy and medication adherence among Hispanics with hypertension. J Racial Ethn Health Disparities. 2019;6(3):517–524. doi:10.1007/S40615-018-00550-Z/METRICS
69. Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns. 2016;99(7):1079–1086. doi:10.1016/J.PEC.2016.01.020
70. Kim H, Goldsmith JV, Sengupta S, et al. Mobile health application and e-health literacy: opportunities and concerns for cancer patients and caregivers. J Cancer Educ. 2019;34(1):3–8. doi:10.1007/S13187-017-1293-5/METRICS
71. Geboers B, Brainard JS, Loke YK, et al. The association of health literacy with adherence in older adults, and its role in interventions: a systematic meta-review. BMC Public Health. 2015;15(1):1–10. doi:10.1186/S12889-015-2251-Y/TABLES/3
72. Lussier MT, Richard C. The motivational interview. Can Family Physician. 2007;53(11):1895. doi:10.23938/assn.0423
73. Kara S. General self-efficacy and hypertension treatment adherence in Algerian private clinical settings. J Public Health Afr. 2022;13(3):2121. doi:10.4081/jphia.2022.2121
74. Huang J, Ding S, Xiong S, Liu Z. Medication adherence and associated factors in patients with type 2 diabetes: a structural equation model. Front Public Health. 2021;9:730845. doi:10.3389/FPUBH.2021.730845/BIBTEX
75. Buchmann WF. Adherence: a matter of self-efficacy and power. J Adv Nurs. 1997;26(1):132–137. doi:10.1046/J.1365-2648.1997.1997026132.X
76. Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract. 2010;20(2):137–160. doi:10.1177/1049731509347850
77. Turan O, Yemez B, Itil O. The effects of anxiety and depression symptoms on treatment adherence in COPD patients. Prim Health Care Res Dev. 2014;15(3):244–251. doi:10.1017/S1463423613000169
78. Gacina DL, Jandrokovic S, Marcinko D, et al. Anxiety and treatment adherence among glaucoma patients during COVID-19 pandemic and earthquakes in Croatia. Psychiatry Danub. 2022;34(2):348–355. doi:10.24869/PSYD.2022.348
79. Sadeghi O, Keshteli AH, Afshar H, Esmaillzadeh A, Adibi P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr Neurosci. 2021;24(4):248–259. doi:10.1080/1028415X.2019.1620425
80. Bauer LK, Caro MA, Beach SR, et al. Effects of depression and anxiety improvement on adherence to medication and health behaviors in recently hospitalized cardiac patients. Am J Cardiol. 2012;109(9):1266–1271. doi:10.1016/j.amjcard.2011.12.017
81. Schulz D. Depression development: from lifestyle changes to motivational deficits. Behav Brain Res 2020;395:112845. doi:10.1016/j.bbr.2020.112845
82. Strack J, Lopes PN, Esteves F. Will you thrive under pressure or burn out? Linking anxiety motivation and emotional exhaustion. Cogn Emot. 2015;29(4):578–591. doi:10.1080/02699931.2014.922934
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.