Back to Journals » Infection and Drug Resistance » Volume 15
Mortality Risk Factors and Prognostic Analysis of Patients with Multi-Drug Resistant Enterobacterales Infection
Authors Wang X, Li Q, Kang J, Yin D, Li X, Wang S, Guo Q, Song Y, Wang J, Duan J
Received 23 March 2022
Accepted for publication 13 June 2022
Published 20 June 2022 Volume 2022:15 Pages 3225—3237
DOI https://doi.org/10.2147/IDR.S366808
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xinchun Wang,1,* Qi Li,2,* Jianbang Kang,1 Donghong Yin,1 Xiaoxia Li,1 Shuyun Wang,1 Qian Guo,1 Yan Song,1 Jing Wang,1 Jinju Duan1
1Department of Pharmacy, Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 2Department of Pharmacy, Shanxi Medical University, Taiyuan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jinju Duan, Department of Pharmacy, Second Hospital of Shanxi Medical University, No. 382, Wuyi Road, Xinghualing District, Taiyuan, People’s Republic of China, Tel +86 351 3365713, Email [email protected]
Background: The data from the China Network Antibacterial Surveillance Center (http://www.chinets.com) showed that the prevalence of Escherichia coli (E. coli), Klebsiella pneumoniae (KP), and Enterobacter cloacae (ecl), was 18.96%, 14.12%, and 2.74% in 2022, respectively. The resistance rates of E. coli and KP to 3rd or 4th generation cephalosporins were 51.7% and 22.1%, to carbapenems was 1.7% and 3.9%, to quinolones was 55.9% in Shanxi. The generation of extended-spectrum beta-lactamases (ESBLs) is a major mechanism resulting in drug resistance in Enterobacterales. To determine the mortality risk factors of multi-drug resistant Enterobacterales (MDRE) and multi-drug resistant Klebsiella pneumoniae (MDR-KP) infection.
Methods: 91 MDR strains from 91 patients were collected from 2015 to 2019 in the second hospital of Shanxi Medical University. The mortality risk factors for the MDRE infections and clinical outcomes were analyzed by univariable and multivariable analysis. The independent predictors of 30-day mortality were analyzed through the Cox regression analysis including the variables with a value < 0.2.
Results: The majority of patients were admitted to ICUs. Pulmonary infection was a major infection (43.96%, 40/91). Thirty-three (36.26%, 33/91) strains of MDR-KP were only detected in 2018. The proportion of multi-drug resistant Escherichia coli (MDR E. coli) and multi-drug resistant Enterobacter cloacae (MDR ecl) were 16.48% (15/91) and 17.58% (16/91), respectively. The presence of cerebrovascular diseases (OR, 4.046; 95%Cl, 1.434– 11.418; P=0.008) and central venous catheterization (OR, 4.543; 95%Cl, 1.338– 15.425; P=0.015) were associated with mortality in patients with MDRE infections. Endotracheal intubation (OR, 4.654; 95%Cl, 1.5– 14.438; P=0.008) was an independent mortality risk factor for patients infected with MDR-KP strains. Patients who received aminoglycoside antibiotics (P=0.057) had a higher 30-day survival rate. The β-lactam antibiotics were the major agent in the clinic.
Conclusion: This study implies that patients with cerebrovascular diseases, central venous catheterization, and endotracheal intubation are at risk of carrying MDR isolates.
Keywords: multi-drug resistance, Enterobacterales, carbapenem-resistant, risk factors
Introduction
Enterobacterales bacteria, which belong to Gram-negative bacilli, are common causes of serious infections (eg: bacteremia, community-acquired pneumoniae, complicated intra-abdominal infection).1–4 The most notorious bacteria is Klebsiella pneumoniae (KP), which is gradually evolving into strains resistant to common antibiotics in clinical practice and causing a severe or fatal infection.5,6 At the same time, Enterobacterales could carry different antimicrobial resistance (AMR) patterns, making them become multi-drug resistant strains.4 Thus, the emergence of multi-drug resistant Enterobacterales (MDRE) represents a significant global public health issue. It contains multi-drug resistant Escherichia coli (MDR E. coli), multi-drug resistant Klebsiella pneumoniae (MDR-KP), and multi-drug resistant Enterobacter cloacae (MDR ecl).7
Over the past decade, lots of research have shown an increase in the prevalence of multidrug-resistant organisms (MDROs) in the general population and the incidence of these bacteria in hospitals.8 One report showed that the prevalence of E. coli ranged from 10.1 to 53.6% (mean 32.1%); the prevalence of KP ranged from 0 to 33.9% (mean 8.2%).9 ESBL-producing Enterobacterales are more prevalent in the United States and Brazil, with isolation rates of approximately 12.05% and 11%, respectively.10,11 In Europe, studies conducted from 2011 to 2013 showed that the rate of ESBL-producing strains was 45.6% in KP. In Asian countries, a study conducted between 2008 and 2014 found that 94.3% of Enterobacterales strains were ESBL producers. On the African continent, between 2009 and 2014, the rate of ESBL-producing strains was 16.4% and 99% of the isolates identified by clinicians.12,13 The data from the China Network Antibacterial Surveillance Center (http://www.chinets.com) showed that the prevalence of E. coli, KP, and ecl was 18.96%, 14.12%, and 2.74% in 2022, respectively. Besides, rates of Enterobacterales strains’ resistance to imipenem and meropenem antibiotics were 9.4% and 9.6%. The China Antimicrobial Resistance Surveillance Report (http://www.carss.cn/), the largest survey of antimicrobial resistance in China, reported that the rate of carbapenem resistance in KP increased from 6.4% in 2014 to 10.9% in 2020, whereas in E. coli, the rate remained stable at under 2% over this period. In addition to, the mean rates of E. coli and KP resistance to 3rd or 4th generation cephalosporins were 51.6% and 22.1%, carbapenems were 1.6% and 10.9%, quinolones was 50.7% (only E. coli strains). Whereas the resistance rates of E. coli and KP to 3rd or 4th generation cephalosporins were 51.7% and 22.1%, to carbapenems was 1.7% and 3.9%, to quinolones was 55.9% in Shanxi. That being so, MDRE strains represent a significant threat to public health, which comes to our urgent attention.
The generation of extended-spectrum beta-lactamases (ESBLs) is a major mechanism resulting in drug resistance in Enterobacterales,4,11 which can hydrolyze different generations of cephalosporins and carbapenems.14 blaCTX-M can hydrolyze several cephalosporins. Another important mechanism is the production of carbapenemases. It has a broad hydrolytic activity and degrades all β-lactams, including carbapenems and β-lactam inhibitors. The genes encoding ESBL and carbapenemases are found on mobile genetic elements and are important in the propagation of drug resistance.15 blaKPCs, blaNDM, blaVIM, and blaOXA can specifically hydrolyze carbapenems. They are associated with nosocomial infections and may complicate infection control in hospitals.16–19 The most encountered ESBL genes among E. coli and KP are blaTEM, blaSHV, and blaCTXM.20 One study from the Netherlands showed that from 1990 to 2015, fecal colonization rates of ESBL-producing Enterobacterales were estimated to be 14% in healthy populations, increasing by about 5% per year.21 Moreover, MDRE strains could carry three or more resistance genes and have a broader spectrum of drug resistance than CRE. Therefore, MDRE should be paid more attention to.
MDRE infections are associated with higher morbidity and mortality.22 People with cardiovascular disease, a history of travel to high-prevalence countries, mechanical ventilation, a history of stay in ICU, and a history of usage of antibiotics could be more vulnerable to MDRE infection.23–25 Owing to the complicated and diverse resistance patterns, the therapeutic options for infections are extremely limited, which lead to the revival of colistin, as a last resort antibiotic to treat gram-negative bacterial infections.26 Thus, treatment of MDRE infection is increasingly more difficult and poses a serious challenge to clinical treatment.
Here, in this retrospective study, we attempted to analyze the clinical characteristics, and mortality risk factors for MDRE and MDR-KP infection to provide a theoretical basis for the clinical diagnosis and predictors for mortality in patients. Furthermore, our results could improve the prognostic for patients and strengthen the control of the spread of MDR-E infection.
Patients and Methods
Study Design and Setting
This retrospective study was performed from January 2015 to June 2019 in the second hospital of Shanxi Medical University. Patients with MDRE infections were resistant to at least three or more classes of antimicrobials in this study. To evaluate the risk factors for MDRE and MDR-KP infection, a retrospective study was performed. The inclusion criteria were as follows: The age of the patient was ≥18 years old. The hospitalized patient had complete clinical data. The exclusion criteria were as follows: The hospitalization was < 24 hours. This study was approved by the Ethics Committee of the second hospital of Shanxi medical university (Code 2019 YX-181).
Clinical Data Collection
Electronic medical records of patients who underwent MDRE infection were reviewed, including age, sex, length of hospitalization, hospital transfer, the length of ICU admission, underlying disease, complication, invasive procedure, and antibiotics usage within the 30 days. Bacterial cultures were processed in the clinical microbiology laboratory. Furthermore, dates of microorganism sampling and infection diagnosis were recorded. Blood, urine, sputum, cerebrospinal fluid, secretion and drainage fluid culture results, the causative agent for Enterobacterales, and site of infection of each patient were also recorded.
Definitions
The definitions of the infections included in this study followed by the Centers for Disease Control and Prevention Prevention (CDC) guidelines (https://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf), including pneumoniae, bloodstream infection, and infections from other sites.
Statistical Analysis
Categorical variables were using a χ2 test or Fisher’s exact test. Then, variables (p value < 0.1) were analyzed in the Logistic model analysis, to identify the independent risk factors of MDRE infection and MDR-KP infection. To determine the independent predictors of 30-day mortality, we analyzed the variables with a value < 0.2 in the Cox regression analysis.27–29 Aiming to analyze the effect of usage of aminoglycosides on the 30-day survival, patients were divided into two groups according to with or without the usage of aminoglycosides. P < 0.05 was considered statistically significant.
Clinical Treatment Analysis
The information on treatments was collected from the electronic medical system. We contained the common antibiotics in clinical practices. We divided the patients into three groups, according to the specific bacteria and the usage days.
Antibiotic Sensitive Testing
Antibiotic sensitive testing was performed using the Vitek 2 automated system (Biomerieux, France) and interpreted according to the latest standards of Clinical and Laboratory Standards Institute (CLSI) Guidelines.30
Results
Clinical Characteristic of Participants
A total of 91 patients were enrolled in this studied period. The majority of patients were admitted to intensive care units (n =26, 28.6%), followed by the neurosurgical wards (n = 18, 19.8%), hematological wards (n = 12, 13.2%), respiratory and critical wards (n = 9, 9.9%), respiratory wards (n = 7, 7.7%), general surgery wards (n = 6, 6.6%), neurology wards (n = 4, 4.4%), nephrology wards (n = 3, 3.3%), rheumatology wards (n = 2, 2.2%), and others (n = 1, 1.1%, each).
The major infection was pulmonary infection (44.0%, 40/91), followed by other infections (24.2%, 22/91), urinary tract infection (6.6%, 6/91), bloodstream infection (4.4%, 4/91), abdominal infection (2.2%, 2/91), and intracranial infection (1.1%, 1/91). The overall mortality was 33.0% (30/91).
The Distribution of Multi-Drug Resistant Enterobacterales
Three MDRE strains were identified in 2015, one strain was isolated in 2016, twenty-four strains were identified in 2017, forty-nine strains were isolated in 2018, and in 2019, fourteen strains were identified. Thirty-three strains of MDR-KP were only detected in 2018. CRKP accounted for 98.3% of the MDR-KP strains. The strains originated from different sites: sputum (n = 59, 64.8%), blood (n = 12, 13.2%), secretions (n = 10, 10.1%), urine (n = 8, 8.8%), cerebrospinal fluid (CSF) (n = 1, 1.1%), and drainage liquid (n = 1, 1.1%). Figure 1
Mortality Risk Factors of Multi-Drug Resistant Enterobacterales
Univariate analyses comparing the baseline characteristics of patients who survived or died are shown in Table 1. There was no significant difference in the demographic measures between the two groups. The median age of the dead patients was 62.5 years (range, 46.91–78.09), these patients were older than the survivors (55.2 vs 17.74, range, 37.46–72.94) (P=0.058). The following factors were most frequently detected in dead patients: MDRE strains were isolated in ICU (P = 0.017), cardiovascular disease (P = 0.039), cerebrovascular disease (P = 0.039), mechanical ventilation (P = 0.006), central venous cannula (P = 0.029), endotracheal intubation (P = 0.009), tracheotomy (P = 0.005), and urinary catheter (P = 0.005). Compared with patients in the survivor group, non-survivor group patients were more likely to have a higher proportion of factors in transfer (60.0% versus 47.5%), hospitalization history of ICU prior to isolation (40.0% versus 34.4%), lung diseases (66.7% versus 52.5%), renal disease (16.7% versus 9.8%), disease of digestive tract (20.0% versus 8.2%), arterial cannula (73.3% versus 57.4%), nasogastric tube (66.7% versus 52.5%), usage of parenteral nutrition (46.7% versus 29.5%), or usage of immunosuppressant (63.3% versus 42.6%). Furthermore, the majority of the patients in the non-survivor group had invasive procedures. Usage of antimicrobial in 30 days before bacteria isolation revealed no difference between the survivor and non-survivor groups. Compared to the survivor group, the proportion of utilization of carbapenems and tigecycline was higher in the non-survivor group but there was no statistically significant difference (P = 0.266, 0.075).
 |
Table 1 Univariable Analysis of Predictors Associated with Non-Survivors with MDRE Infection |
Variables with P < 0.1 were included into Logistic regression analysis. Multivariate analysis indicated that cerebrovascular diseases (OR, 4.046; 95% Cl, 1.434–11.418; P = 0.008) and central venous catheterization (OR, 4.543; 95% Cl, 1.338–15.425; P = 0.015) were independent mortality risk factors for infection with MDRE when compared with the survivor group. Table 2
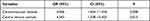 |
Table 2 Multivariate Logistic Analysis of Predictors of Non-Survivors with MDRE Infection |
Risk Factors for 30-Day Mortality and Prognostic Analysis of Multi-Drug Resistant Enterobacterales
Our study highlights the high mortality associated with MDRE infection (33.0%, 30/91), at the same time, the mortality in 30-day was 23.1% (21/91). The mean 30-day survival time of patients with MDRE infection was 24.6 days (7–30). Multivariate Cox survival regression analysis showed that the predictor independently associated with 30-day mortality was the usage of aminoglycoside (HR, 0.351; 95% CI, 0.118–1.044; P = 0.06). Patients were divided into two groups according to whether they received aminoglycoside antibiotics or not. The survival time of the group that did not receive aminoglycoside antibiotics was significantly lower than that of the group that received aminoglycoside antibiotics, but there was no statistical significance.
Mortality Risk Factors of Multi-Drug Resistant Klebsiella pneumoniae
Due to the isolation rate of MDR-KP being high (66.0%, 60/91), we do a further mortality risk factors analysis of MDR-KP strains. The mean duration of hospitalization of non-survivor group patients was 24 days (range 16–37.75), which had statistical significance, compared to the survivor group. The following factors were statistically different between the two groups: invasive procedures (P = 0.009), endotracheal intubation (P = 0.006), tracheotomy (P = 0.012), and urinary catheter (P = 0.03). Furthermore, we found that the history of immunosuppressant use was borderline statistical significance (P = 0.056). However, the usage of antibiotics was not statistically significantly different between the two groups. Table 3
 |
Table 3 Univariable Analysis of Predictors Associated with Non-Survivors with MDR-KP Infection |
Also, the variables with P < 0.1 were performed Logistic regression analysis. Multivariate analysis indicated that endotracheal intubation (OR, 4.654; 95% Cl, 1.5–14.438; P = 0.008) was an independent mortality risk factor for infection with MDR-KP strains. Table 4
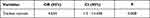 |
Table 4 Multivariate Logistic Analysis of Predictors of Non-Survivors with MDR-KP Infection |
In the Cox analyses, aminoglycoside antibiotics therapy was associated with a 30-day survival benefit with borderline statistical significance (P = 0.057). Thus, patients were divided into two groups, according to the usage of aminoglycoside. Overall, 22 patients receive aminoglycoside therapy, and 2 of them were dead (9.09%). But, it was not associated with 30-day survival between the two groups.
Clinical Treatments Characteristics
We collected the treatment of patients infected with MDRE during the hospitalization (Table 5). The patients were divided into three groups, according to the bacteria species. In MDR E. coli, the most frequent antibiotic was β-lactam inhibitors, which account for 66.7%. The second most frequently used were quinolones (46.7%). Carbapenems were not commonly used in MDR E. coli infections. In MDR-KP group, β-lactam inhibitors were the major agents. Carbapenems were the second most frequently treatment in the clinic. While the proportion of aztreonam was 1.7%. During MDR ecl bacteria, β-lactam inhibitors were also the main treatment. Carbapenems (62.5%) and quinolone (56.3%) also had a higher proportion. Usage of cefoperazone/sulbactam and piperacillin/tazobactam ≧7 days accounted for 20.0% and 13.3%, 18.3% and 8.3%, and 31.3% and 25.0% in MDR E. coli, MDR-KP, and MDR ecl, respectively. Tigecycline had a lower usage frequency.
 |
Table 5 Thetreatment of Patients with MDRE Infecton |
Investigation of Patients with Multiple Detections of Multi-Drug Resistant Enterobacterales
In our study, 18 patients have been detected with different MDRE strains more than once. Among them, three patients dead eventually, two of them diagnosed with a lung infection. Most patients (14/18, 77.8%) were isolated MDR-KP during the hospitalization. The detailed information about these patients was shown in Figure 2. During the hospitalization, 12 patients had received combination therapies. Here, we highlighted the description of the non-survivors’ information.
Patient 2 a 69-year-old man with no recent travel history, was admitted on 13 November 2015 for the neurosurgery with hemorrhage from the right cerebellar hemisphere into the ventricle. He had a history of nervous system disease, smoking, and cerebrovascular disease. Patient 2 received long-term rehabilitation persistently (80 days). During his hospitalization, he received invasive procedures, drainage tube, central venous cannula, endotracheal intubation, tracheotomy, and urinary catheter. On 11 November and 14 November, the MDR-KP strains were isolated from sputum specimens. He was treated with CSL and CIP. Meanwhile, CSL was administered for more than 7 days and the combined treatment of CSL and CIP lasted from December 22 to January 1. Unfortunately, he was dead eventually due to the unrelieved condition.
Patient 12 was 76 years old and was admitted with pulmonary infection from 17 July 2018 to 1 September 2018. He was transferred from another hospital. He had underlying diseases such as lung diseases and neurological diseases. During his 46-day hospitalization, he received mechanical ventilation, drainage tube, central venous cannula, tracheotomy, and urinary catheter. We had isolated MDR-KP strains seven times from sputum samples. The CSL, TGC, VA, MEM, and LZD were used as effective therapeutic agents to confer the infections. Furthermore, he also used enteral nutrition preparations and immunosuppressants. On 1 September, he was dead of an intracranial infection and pulmonary infection.
Patient 18 was a 76-year-old male and admitted on 2 June 2019 with pulmonary infection and cerebral hernia. He had lung diseases and neurological diseases and received invasive procedures, drainage tube, and central venous cannula, including endotracheal intubation, tracheotomy, and urinary catheter. During his hospitalization, MDR-KP strains were isolated twice from sputum samples. CSL antibiotic treatment was started and combined with TGC. Unfortunately, he was dead within 18 days.
Antimicrobial Susceptibility Results
91 MDRE isolates were tested antimicrobial susceptibility testing. All isolates were resistant to cefazolin, cefuroxime, and cefoxitin, followed by ceftriaxone, 98.9%. The antimicrobial resistance rates were as follows: imipenem, 97.8%; meropenem, 96.7%; cefepime 96.7%; ceftazidime, 96.7%; cefoperazone/sulbactam 96.7%, piperacillin/tazobactam 96.7%; levofloxacin, 92.3%; aztreonam, 90.1%; ciprofloxacin, 89.0%; amikacin, 19.8%.
Discussion
Multi-drug resistant Enterobacterales strains are one of the greatest public health threats, often causing severe infections, such as bloodstream infections, pneumoniae, and abdominal infections.14,20 However, data from Shanxi in patients infected with MDR-E is scarce, and the available literature has revealed the risk factors of Gram-negative bacteria infection. Therefore, we reported the mortality risk factors of the patients infected with MDRE pathogens isolated from a tertiary hospital located in Shanxi, China. In our study, the presence of cerebrovascular diseases and central venous catheterization was associated with the death of patients with MDRE infections. Endotracheal intubation was an independent mortality risk factor for patients infected with MDR-KP strains.
Many studies revealed that the infections caused by MDRE commonly occurred in ICU.22,31 While our study showed that MDR-KP strains were the main bacteria species and the same result in department distribution. Moreover, pulmonary infection was the major infection in our study. In contrast, the report from Lebanon indicated that Gram-negative organisms were responsible for 78.8% of bloodstream infections.1
Knowledge of potential clinical risk factors for infection with MDRE might help to better understand MDRE infection, improve the control precautions, and optimize antibiotic therapy. In the present study, we found that MDRE infection was more vulnerable to lead to unimaginable outcomes in patients with the elderly, transfer hospitals, bacteria isolated from ICU, more underlying diseases, and invasive producers. These findings were similar to previous studies.22,32 Unlike the previous study, our study failed to find a difference between the survival and non-survivor groups for immune and diabetes.3,33 This might be due to the limited number of cases in our study.
Furthermore, some studies had investigated the risk factors in patients infected with CRE and ICU, and the history of antibiotics was regarded as independent risk factor.15,18,23 In our study, cerebrovascular diseases and central venous catheterization were considered as independent predictors associated with MDRE infection. This finding was the same as the previous study.2 Interestingly, we found patients, infected with MDRE strains, who had received the aminoglycoside agents may have a lower risk of death. Though there was no statistical significance between the two groups. This result was different from the previous study and the need for more in-depth research.34
Due to the high isolation rate of MDR-KP strains, we analyzed the mortality factors of MDR-KP. Mechanical ventilation, endotracheal intubation, and urinary catheter had statistical significance between the two groups. Surprisingly, the usage of immunosuppressors had borderline statistical significance. Previous research demonstrated that patients with a history of ICU, invasive procedures, and prior to carbapenem exposure were risk factors in CRKP infection.34–36 Unfortunately, the history of antimicrobial drug use was not a risk factor in this study. The endotracheal intubation was an independent predictor of MDR-KP infection. In this study, the usage of aminoglycoside antibiotics was a mortality risk factor with borderline statistical significance.
Clinical treatment of infection with MDRE in this study was also investigated. In our study, the β-lactam antibiotics were the major agent in the clinic. The proportion of carbapenems was 45.05%. This might lead to ESBL-resistance, increasing the drug resistance and difficulty in treatment.37 A study conducted on patients, who were infected with community-acquired pneumonia caused by Enterobacterales, considered prior ESBL infection as the risk factor.2 However, we did not gain the same result. This was likely to suffer from under-reporting due to the reliance on clinician documentation. Previous studies have shown that appropriately targeted therapy based on drug sensitivity results can help reduce morbidity and mortality.38,39
Three patients were selected to do a further analysis of their entire hospitalization based on multiple isolations of MDRE and poor prognosis. During the 3 non-survivors’ hospitalization, they all received more than 3 species of antibiotics. One study suggested that the risk of infection with MDR-resistant isolates may increase to 60% when antibiotic pretreatment is ≥7 days.31 In our study, three patients had received CSL or TGC for more than seven days. And they all had received combination treatment. Others also suggested that combination therapies should be used to treat severe CRE infection.15 Although no symptoms of fever were found, the information from 18 patients also suggested that clinicians be more vigilant against the possibility of drug-resistant bacterial infections when confronted with clinical symptoms such as fever, calcitonin (PCT) index, or even shock in patients. Due to the small size population, the funding was limited.
Carbapenem antibiotics were regarded as the last resort treatment, while in our antimicrobial susceptibility test in vitro, the antimicrobial susceptibility rates of imipenem and meropenem were 2.2% and 3.3%, respectively. This result was in line with the published report, which thought that 82 of CRE strains were resistant to both imipenem and meropenem.20 Carbapenem resistance in Enterobacterales is a complicated issue. A study showed that the incidence of CRE infection was increasing to 16% in Enterobacterales.3 It can occur in various Enterobacterales and may be mediated by several mechanisms, including the production of carbapenemases.15,40–42 In our published study, we found that blaNDM-5 carbapenemase was the main resistance mechanism of CRKP strains. Furthermore, it also showed that the ST11 was the predominant sequence type.35 Another study suggested that the patients in the meropenem MIC ≥ 8 mg/L had a significantly higher 30-day mortality than those in the meropenem MIC = 2 or 4 mg/L groups and ≤ 1 mg/L group.33 Furthermore, E. coli strains had a high resistance rate of 3,4 generation cephalosporin. A study indicates that from 2001 to 2008, the 3rd generation cephalosporin-resistant E. coli has a ten-fold increase, and the highly resistant E. coli have a 30% increase in infection rate and higher mortality compared to susceptible isolates.43 Meanwhile, the frequency of antibiotic use and exposure to any antibiotics may be responsible for the development of drug resistance.1 Multiple studies recommend avoiding single antibiotics for anti-infective treatment in the case of drug-resistant bacterial infections.31 The combination treatment was most effective and can reduce the resistance rate of carbapenem and colistin.
Our study has some limitations. Firstly, we used the retrospective observational study. Thus, there might be some bias, such as the loss of some clinical and laboratory data. Secondly, our population was small. This might lead to limited results, and the reference value for comparison is small. However, our study, which collected cases from 2015 to 2019, is also a long-term study. So, our study has certain significance for the treatment of MDRE strains in the local region. While these results could not represent the condition of China and a larger sample is necessary for further study.
Conclusion
Collectively, cerebrovascular diseases and central venous catheterization factors were associated with the death of patients with MDRE infections. Endotracheal intubation was an independent mortality risk factor for patients infected with MDR-KP strains. The MDRE strains have a high resistance rate to common antibiotics. Keeping this in mind, combined treatment of more than two antibiotics is recommended in MDRE patients. Our results imply that the more tailored treatment plans still need to be further developed according to the local epidemiological characteristics. More infection control measures should be performed and formulated to stem Enterobacterales infections.
Data Sharing Statement
The original data supporting the conclusions of this manuscript will be made available by the Jinju Duan ([email protected]), without undue reservation, to any qualified researcher.
Ethics Statement
This study was approved by the Ethics Committee of the second hospital of Shanxi medical university (Code 2019 YX-181). The data of patients’ clinical variables were collected from their medical records and did not contain names, addresses, or other personal information. The study was a retrospective observational study, so all the information was collected from the medical record. Thus, the patients’ written informed consent was exempt. This study was also in line with the guidelines outlined in the Declaration of Helsinki.
Acknowledgments
We thank the Department of Pharmacy, Second Hospital of Shanxi Medical University, for supporting this research.
Funding
This work was supported by the Shanxi Province Natural Science Foundation (grant number 201803D31124). The sponsor had no involvement in any of the stages from the study design to the submission of the paper for publication.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Moghnieh R, Estaitieh N, Mugharbil A, et al. Third generation cephalosporin resistant Enterobacteriaceae and multidrug resistant gram-negative bacteria causing bacteremia in febrile neutropenia adult cancer patients in Lebanon, broad spectrum antibiotics use as a major risk factor, and correlation with poor prognosis. Front Cell Infect Microbiol. 2015;5:11. doi:10.3389/fcimb.2015.00011
2. Villafuerte D, Aliberti S, Soni NJ, et al. Prevalence and risk factors for Enterobacteriaceae in patients hospitalized with community-acquired pneumonia. Respirology. 2020;25(5):543–551. doi:10.1111/resp.13663
3. Liu J, Zhang L, Pan J, et al. Risk factors and molecular epidemiology of complicated intra-abdominal infections with carbapenem-resistant Enterobacteriaceae: a multicenter study in China. J Infect Dis. 2020;221(Suppl 2):S156–S163. doi:10.1093/infdis/jiz574
4. Manandhar S, Zellweger RM, Maharjan N, et al. A high prevalence of multi-drug resistant Gram-negative bacilli in a Nepali tertiary care hospital and associated widespread distribution of Extended-Spectrum Beta-Lactamase (ESBL) and carbapenemase-encoding genes. Ann Clin Microbiol Antimicrob. 2020;19(1):48. doi:10.1186/s12941-020-00390-y
5. Blin C, Passet V, Touchon M, Rocha E, Brisse S. Metabolic diversity of the emerging pathogenic lineages of Klebsiella pneumoniae. Environ Microbiol. 2017;19(5):1881–1898. doi:10.1111/1462-2920.13689
6. Liu Z, Gu Y, Li X, et al. Identification and characterization of NDM-1-producing Hypervirulent (Hypermucoviscous) Klebsiella pneumoniae in China. Ann Lab Med. 2019;39(2):167. doi:10.3343/alm.2019.39.2.167
7. Doi Y, Bonomo RA, Hooper DC, et al. Gram-negative bacterial infections: research priorities, accomplishments, and future directions of the antibacterial resistance leadership group. Clin Infect Dis. 2017;64(suppl_1):S30–S35. doi:10.1093/cid/ciw829
8. Saliba R, Ghelfenstein-Ferreira T, Lomont A, et al. Risk factors for the environmental spread of different multidrug-resistant organisms: a prospective cohort study. J Hosp Infect. 2021;111:155–161. doi:10.1016/j.jhin.2021.01.029
9. Trecarichi EM, Tumbarello M. Antimicrobial-resistant Gram-negative bacteria in febrile neutropenic patients with cancer: current epidemiology and clinical impact. Curr Opin Infect Dis. 2014;27(2):200–210. doi:10.1097/QCO.0000000000000038
10. Reynoso A, Munson E. Surveillance of Wisconsin organisms for trends in antimicrobial resistance and epidemiology (SWOTARE): 2018–2019 report on Enterobacter cloacae and Klebsiella pneumoniae clinical isolates. Clin Med Res. 2021;19(3):123–131. doi:10.3121/cmr.2021.1588
11. de Oliveira Santos JV, da Costa Junior SD, de Fátima Ramos Dos Santos Medeiros SM, et al. Panorama of bacterial infections caused by epidemic resistant strains. Curr Microbiol. 2022;79(6):175. doi:10.1007/s00284-022-02875-9
12. Iabadene H, Messai Y, Ammari H, et al. Prevalence of plasmid-mediated AmpC beta-lactamases among Enterobacteriaceae in Algiers hospitals. Int J Antimicrob Agents. 2009;34(4):340–342. doi:10.1016/j.ijantimicag.2009.05.011
13. Naas T, Bentchouala C, Cuzon G, et al. Outbreak of Salmonella enterica serotype infantis producing ArmA 16S RNA methylase and CTX-M-15 extended-spectrum beta-lactamase in a neonatology ward in Constantine, Algeria. Int J Antimicrob Agents. 2011;38(2):135–139. doi:10.1016/j.ijantimicag.2011.04.012
14. Mohsin M, Hassan B, Khan AU, Ali A, Swedberg G, Hasan B. Genomic characterization of high-risk Escherichia coli and Enterobacter hormaechei clones recovered from a single tertiary-care hospital in Pakistan. J Appl Microbiol. 2022;132(5):3907–3914. doi:10.1111/jam.15482
15. Biset S, Moges F, Endalamaw D, Eshetie S. Multi-drug resistant and extended-spectrum beta-lactamases producing bacterial uropathogens among pregnant women in Northwest Ethiopia. Ann Clin Microbiol Antimicrob. 2020;19(1):25. doi:10.1186/s12941-020-00365-z
16. Mathers AJ, Peirano G, Pitout JDD. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev. 2015;28(3):565–591. doi:10.1128/CMR.00116-14
17. Cejas D, Elena A, Guevara Nunez D, et al. Changing epidemiology of KPC-producing Klebsiella pneumoniae in Argentina: emergence of hypermucoviscous ST25 and high-risk clone ST307. J Glob Antimicrob Resist. 2019;18:238–242. doi:10.1016/j.jgar.2019.06.005
18. Taggar G, Attiq Rheman M, Boerlin P, Diarra MS. Molecular epidemiology of carbapenemases in enterobacteriales from humans, animals, food and the environment. Antibiotics. 2020;9(10). doi:10.3390/antibiotics9100693
19. Evans BA, Amyes SG. OXA beta-lactamases. Clin Microbiol Rev. 2014;27(2):241–263. doi:10.1128/CMR.00117-13
20. Ngoi ST, Chong CW, Ponnampalavanar SSS, et al. Genetic mechanisms and correlated risk factors of antimicrobial-resistant ESKAPEE pathogens isolated in a tertiary hospital in Malaysia. Antimicrob Resist Infect Control. 2021;10(1):70. doi:10.1186/s13756-021-00936-5
21. Voor AF, Mourik K, Beishuizen B, et al. Acquisition of multidrug-resistant Enterobacterales during international travel: a systematic review of clinical and microbiological characteristics and meta-analyses of risk factors. Antimicrob Resist Infect Control. 2020;9(1):71. doi:10.1186/s13756-020-00733-6
22. Kajova M, Khawaja T, Kangas J, Makinen H, Kantele A. Import of multidrug-resistant bacteria from abroad through interhospital transfers, Finland, 2010–2019. Euro Surveill. 2021;26(39). doi:10.2807/1560-7917.ES.2021.26.39.2001360
23. Woerther PL, Andremont A, Kantele A. Travel-acquired ESBL-producing Enterobacteriaceae: impact of colonization at individual and community level. J Travel Med. 2017;24(suppl_1):S29–S34. doi:10.1093/jtm/taw101
24. Josseaume J, Verner L, Brady WJ, Duchateau FX. Multidrug-resistant bacteria among patients treated in foreign hospitals: management considerations during medical repatriation. J Travel Med. 2013;20(1):22–28. doi:10.1111/j.1708-8305.2012.00668.x
25. Angue M, Allou N, Belmonte O, et al. Risk factors for colonization with multidrug-resistant bacteria among patients admitted to the intensive care unit after returning from abroad. J Travel Med. 2015;22(5):300–305. doi:10.1111/jtm.12220
26. Baron SA, Cassir N, Hamel M, et al. Risk factors for acquisition of colistin-resistant Klebsiella pneumoniae and expansion of a colistin-resistant ST307 epidemic clone in hospitals in Marseille, France, 2014 to 2017. Euro Surveill. 2021;26(21). doi:10.2807/1560-7917.ES.2021.26.21.2000022
27. Wu C, Zheng L, Yao J. Analysis of risk factors and mortality of patients with carbapenem-resistant Klebsiella pneumoniae infection. Infect Drug Resist. 2022;15:2383–2391. doi:10.2147/IDR.S362723
28. Zheng G, Shi Y, Cao Y, et al. Clinical feature, therapy, antimicrobial resistance gene distribution, and outcome of nosocomial meningitis induced by multidrug-resistant Enterobacteriaceae-a longitudinal cohort study from two neurosurgical centers in Northern China. Front Cell Infect Microbiol. 2022;12:839257. doi:10.3389/fcimb.2022.839257
29. Chen D, Zhang Y, Wu J, et al. Analysis of hypervirulent Klebsiella pneumoniae and classic Klebsiella pneumoniae infections in a Chinese hospital. J Appl Microbiol. 2022;132(5):3883–3890. doi:10.1111/jam.15476
30. CaLS I. Performance Standards for Antimicrobial Susceptibility Testing. Wayne, PA: Clinical and Laboratory Standards Institute; 2021.
31. Renk H, Stoll L, Neunhoeffer F, et al. Suspicion of respiratory tract infection with multidrug-resistant Enterobacteriaceae: epidemiology and risk factors from a paediatric intensive care unit. BMC Infect Dis. 2017;17(1):163. doi:10.1186/s12879-017-2251-x
32. Pouch SM, Patel G; Practice ASTIDCo. Multidrug-resistant gram-negative bacterial infections in solid organ transplant recipients-guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13594. doi:10.1111/ctr.13594
33. Wang Q, Zhang Y, Yao X, et al. Risk factors and clinical outcomes for carbapenem-resistant Enterobacteriaceae nosocomial infections. Eur J Clin Microbiol Infect Dis. 2016;35(10):1679–1689. doi:10.1007/s10096-016-2710-0
34. Williams PCM, Bartlett AW, Palasanthiran P, Armstrong B, McMullan BJ. Successful treatment of invasive carbapenemase-producing Enterobacteriaceae infections in children using carbapenem-aminoglycoside combination therapy: a case series. Infect Dis Health. 2020;25(4):314–318. doi:10.1016/j.idh.2020.06.002
35. Li Q, Zhu J, Kang J. Emergence of NDM-5-producing carbapenem-resistant Klebsiella pneumoniae and SIM-producing hypervirulent Klebsiella pneumoniae isolated from aseptic body fluid in a large tertiary hospital, 2017–2018: genetic traits of blaNDM-like and blaSIM-like genes as determined by NGS. Infect Drug Resist. 2020.
36. Paczosa MK, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiol Mol Biol Rev. 2016;80(3):629–661. doi:10.1128/MMBR.00078-15
37. Ruppe E, Andremont A, Armand-Lefevre L. Digestive tract colonization by multidrug-resistant Enterobacteriaceae in travellers: an update. Travel Med Infect Dis. 2018;21:28–35. doi:10.1016/j.tmaid.2017.11.007
38. Daikos GL, Markogiannakis A. Carbapenemase-producing Klebsiella pneumoniae: (when) might we still consider treating with carbapenems? Clin Microbiol Infect. 2011;17(8).
39. Patel TS, Nagel JL, Doern GV. Clinical outcomes of Enterobacteriaceae infections stratified by carbapenem MICs. J Clin Microbiol. 2015;53(1):201–205. doi:10.1128/JCM.03057-14
40. Navon-Venezia S, Kondratyeva K, Carattoli A. Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol Rev. 2017;41(3):252–275. doi:10.1093/femsre/fux013
41. Tooke C, Hinchliffe P, Bragginton E, et al. β-Lactamases and β-Lactamase inhibitors in the 21st century. J Mol Biol. 2019;431(18):3472–3500. doi:10.1016/j.jmb.2019.04.002
42. Rapp R, Urban C. Klebsiella pneumoniae carbapenemases in Enterobacteriaceae: history, evolution, and microbiology concerns. Pharmacotherapy. 2012;32(5):399–407. doi:10.1002/j.1875-9114.2012.01035.x
43. Wendt C, Baum H, Kaase M. Hygienemaßnahmen bei Infektionen oder Besiedlung mit multiresistenten gramnegativen bakteriellen Erregern[Hygienic treatment of bacteria carrying multidrug-resistant bacteria]. Slides. 2017;55:18–20.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


