Back to Journals » Vascular Health and Risk Management » Volume 18
Mortality and Deep Vein Thrombosis in the Gamma Variant of Covid 19 and Lung Injury
Authors Hungaro Cunha C, Yuri Sato D, Pereira de Godoy JM , da Silva Russeff GJ, Franccini Del Frari Silva D, Pereira de Godoy HJ, Menezes da Silva MO, Amorim Santos H, Guerreiro Godoy MDF
Received 8 April 2022
Accepted for publication 15 September 2022
Published 3 November 2022 Volume 2022:18 Pages 833—838
DOI https://doi.org/10.2147/VHRM.S367930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Carolina Hungaro Cunha,1 Debora Yuri Sato,1 Jose Maria Pereira de Godoy,2 Gleison Juliano da Silva Russeff,1 Desirée Franccini Del Frari Silva,1 Henrique Jose Pereira de Godoy,3 Mariana Orate Menezes da Silva,4 Henrique Amorim Santos,4 Maria de Fatima Guerreiro Godoy5
1Ecography Service in Hospital de Base-FUNFARME/FAMERP, Sao Jose do Rio Preto, Brazil; 2Cardiology and Cardiovascular Surgery Department Sao Jose do Rio Preto School Medicine-FAMERP, Sao Jose do Rio Preto, Brazil; 3General Surgery Department São Jose do Rio Preto School Medicine-FAMERP, Sao Jose do Rio Preto, Brazil; 4Vascular Surgery Service São Jose do Rio Preto School Medicine-FAMERP, Sao Jose do Rio Preto, Brazil; 5Post-Graduate Program São José do Rio Preto-FAMERP, Sao Jose do Rio Preto School Medicine-FAMERP, Sao Jose do Rio Preto, Brazil
Correspondence: Jose Maria Pereira de Godoy, Cardiology and Cardiovascular Surgery Department São Jose do Rio Preto School Medicine-FAMERP, Rua Floriano Peixoto, São Jose do Rio Preto, SP, 2950, Brazil, Tel/Fax +551732326362, Email [email protected]
Purpose: The SARS-CoV-2 disease predisposes infected individuals to thrombosis, the underlying mechanisms of which are not fully understood. The balance between pro-coagulant factors and natural coagulation inhibitors in critically ill patients with Covid-19 is fundamental to the prevention and treatment of complications. The aim of the present study was to investigate the pulmonary injury patterns in Covid-19 having higher mortality in the presence of deep vein thrombosis in comparison to patients without venous thrombosis and determine the Gamma variant.
Methods: A retrospective study was conducted involving the evaluation of 200 medical records of patients with Covid-19 and a clinical suspicion of deep vein thrombosis (DVT) at the intensive care unit of a public hospital. The sample was divided into two groups of patients were formed – those positive and those negative for DVT. Statistical analysis involved the use of Fisher’s exact test, the paired t-test and chi-square test.
Results: Patients with DVT had more severe lung injuries (greater than 70%) compared to those without DVT (p = 0.003). Lesions affecting 50% to 70% of the lung area occurred in little more half of the group with DVT and just under half in the group without DVT (p = 0.5). Pulmonary lesions affecting less than 50% of the lung occurred more in patients without DVT (p = 0.0001). The Gamma variant increased prevalence of the both DVT and mortality (p=0.0001).
Conclusion: Deep vein thrombosis is an aggravating factor of mortality in patients with SARS-CoV-2, and the Gamma variant is an aggravating factor of both thrombotic events and mortality.
Keywords: Covid-19, deep vein thrombosis, pulmonary thrombosis, mortality
Introduction
The SARS-CoV-2 disease predisposes infected individuals to thrombosis, the underlying mechanisms of which are not fully understood. The balance between pro-coagulant factors and natural coagulation inhibitors in critically ill patients with Covid-19 is fundamental to the prevention and treatment of complications.1 A study confirms that critically ill patients with coronavirus may develop arterial and deep vein thrombosis, which increased the risk of mortality. Thus, adequate early conduct can improve the overall survival rate, especially among patients 60 years of age or younger.2
D dimer concentrations are high in nearly all patients with Covid-19. Moreover, concentrations ≥3000 ng/mL (more than 13-fold higher than the normal range) seem to be reliable with regard to screening for deep vein thrombosis (DVT) in the lower limbs.3
Anticoagulant therapy is associated with a reduction in mortality. However, the best dose and option timing remain the object of study. One study found a 2.5% rate of major hemorrhagic events in a group given an intermediate dose, with a 1.07% rate of fatal events, compared to only four major hemorrhagic events (1.4%) and no mortality in the group given a standard prophylactic dose.4
The sequencing of the genome of the virus sampled in the city of Manaus (Brazil) between November 2020 and January 2021 revealed the emergence and circulation of a worrisome novel variant of SARS-CoV-2. The Gamma variant line acquired 17 mutations, including three in the spike protein (K417T, E484K and N501Y), and an increase in bonding to the human angiotensin converting enzyme 2 (ACE2) receptor.5
Recent observations suggest that venous thrombosis is a clinical aggravating factor in patients with SARS-CoV-2. The aim of the present study was to investigate the mortality rate in patients with pulmonary injury patterns in Covid-19 in the presence of deep vein thrombosis in comparison to patients with the same pulmonary injury patterns without venous thrombosis and determine the effect of the Gamma variant.
Methods
Patients and Setting
Patients with SARS-CoV-2 and a clinical suspicion of DVT at intensive care units (ICUs) of the public hospital affiliated with the São Jose do Rio Preto School of Medicine were evaluated until forming two groups of 100 patients each (positive and negative for DVT) between March 2020 and April 2021.
Design
A retrospective study of medical records was conducted using 200 consecutive medical records of patients with SARS-CoV-2. The patients formed two groups (100 positive for DVT and 100 negative for DVT). Fisher’s exact test was used to determine whether mortality due to pulmonary lesions in Covid-19 and the Gamma variant was associated with DVT.
Inclusion Criteria
Medical records of patients with SARS-CoV-2 evaluated at the Doppler service of the hospital having testing positive and negative for DVT and having undergone chest tomography.
Exclusion Criterion
Medical records of patients with inconclusive exam results.
Ethical Approval and Informed Consent Statements
This study received approval from the institutional review board Sao Jose do Rio Preto School of Medicine-FAMERP-Brazil (certificate number #4.720.521). The consent form required for patients participating in a study or for data verification, their medical records, which were the case for this research, was waived by the local ethics committee because of not having contact with the patients or died, all of whom were discharged from the hospital, but with a document attached by the researchers to the ethics committee with a term of commitment to use data for research in compliance with the Declaration of Helsinki. The researchers signed a term of commitment to use data with absolute secrecy, approved by the institution in conformity local ethical committee.
Statistical Analysis
Descriptive statistics of the data were performed. Comparisons between groups were performed using Fisher’s exact test, the paired t-test and chi-square test considering a 5% alpha error.
Selection of Patients
Consecutive patients with SARS-CoV-2 and a suspicion of DVT by the ICU team sent for bilateral venous Doppler exam of the lower limbs and submitted to chest tomography until completing two groups of patients – 100 positive for DVT and 100 negative for DVT.
Development
In a population of more than 5700 patients hospitalized in the infirmaries and ICUs of the public hospital between March 2020 and April 2021 for SARS-CoV-2, 200 admitted to the ICUs that had a clinical suspicion of DVT based on high D dimer levels were selected and divided into two groups – 100 patients positive for DVT and 100 negative for DVT. The data were correlated with the tomographic results, and the patients were subdivided based on the extent of pulmonary injury (≥25% to ≤50% of the lungs affected; ≥50% to ≤70%; and ≥70% the lungs affected). Associations between DVT and mortality were investigated. Correlations between mortality and data on the frequency of Brazilian variants were also investigated by sequencing the genome of the virus. The data were entered into an Excel table, and associations were tested using Fisher’s exact test, the paired t-test and chi-square test.
Results
Forty-two patients in the group without DVT were women and 58 were men. Thirty-four of the patients in the group with DVT were women and 66 were men. No statistically significant difference in sex was found between groups (p = 0.2, Fisher’s exact test). Mean age was 55.58 years with a standard deviation of 12.91 years in the group with DVT and 58.61 years with a standard deviation of 14.21 in the group without DVT; with no significant difference between groups (p = 0.12, paired t-test).
Patients with DVT had more severe pulmonary lesions (greater than 70%) compared to those without DVT (p = 0.003, Fisher’s exact test). Lesions affecting 50% to 70% of the lung area occurred in little more than half of the group with DVT and little less than half in the group without DVT (p = 0.5). Pulmonary lesions affecting less than 50% of the lung occurred more in patients without DVT (p = 0.0001), as shown in Table 1.
 |
Table 1 Extent of Lung Injury According to Presence or Absence of Deep Vein Thrombosis (DVT) |
The mortality rate due to lung injury was higher among the patients with DVT. For injuries affecting ≥25% to ≤50% of the lungs, the mortality rate was 36.36% (4/11) in the group with DVT and 16.12% (5/31) in the group without DVT (p = 0.2, Fisher’s exact test). For injuries affecting ≥50% to ≤70% of the lungs, the mortality rate was 71.15% (37/52) in the group with DVT and 26.19% (11/42) in the group without DVT (p = 0.0001, Fisher’s exact test). For injuries affecting ≥70% of the lungs, the mortality rate was 74.26% (26/35) in the group with DVT and 40.9% (9/22) in the group without DVT (p = 0.01, Fisher’s exact test), as shown in Table 2.
 |
Table 2 Mortality and Survival Rates Associated with Extent of Lung Injury According to Presence or Absence of Deep Vein Thrombosis |
Cases of DVT before predominance of Gamma variant (November 2020 to February 2021) and after predominance of Gamma variant (March to May 2021) are shown in Table 3. Figure 1 shows a significant increase in the occurrence of DVT chi-square test = P < 0.0001; odds ratio = 0,197,889; approximate 95% confidence interval = 0,126,446 to 0,309,698, and mortality chi-square test =P < 0.0001 with odds ratio = 0,576,321 [95% CI] = 0,490,695 to 0,67,689 after the emergence of the Gamma variant.
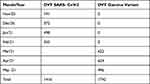 |
Table 3 DVT Before Predominance of Gamma Variant (November 2020 to February 2021) and After Predominance of Gamma Variant (March to May 2021) |
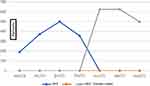 |
Figure 1 Variations in occurrence of deep venous thrombosis before and after Gamma variant. |
Discussion
The present study shows that the presence of deep vein thrombosis (DVT) increases the risk of mortality in SARS-CoV-2 patients with lung injury compared to patients without DVT, as found in all categories of lung injury investigated. Therefore, DVT is an indicator of an increase in mortality in patients with SARS-CoV-2. Gamma variant increased both the prevalence of DVT and the mortality rate in these patients.
A study by the authors in the publication phase found that the Gamma variant increased both the prevalence of DVT and the mortality rate in these patients. Another study by the authors involving two groups of 100 consecutive patients found that pulmonary thrombosis associated with DVT doubled the mortality rate in these patients.
The main cause of mortality in SARS-CoV-2 is vascular and associated with pulmonary thrombosis, with the occurrence of pulmonary embolism in some cases. The increase in the extent of thrombotic processes in the venous microcirculation, may be the cause of this increase in mortality. Thus, one of the goals for reducing the mortality rate in these patients is an improvement in the prevention of thrombotic events, the early diagnosis of thrombosis and adequate treatment.
Thrombotic events have occurred in hospitalized patients. However, there are several cases in which patients have had thrombotic episode days after being discharged. Another finding is that thrombotic events occur at several venous sites bilaterally and mainly below the knee. An aggravating factor is the rapid predominance of the Gamma variant, which was identified in more than 45% of patients in February 2021 and increasing to 83%, 97% and 98% in the subsequent months. This is the second wave that we are experiencing and is associated with a greater frequency of DVT compared to previous viral types.
The present study stresses two negative aspects – the higher mortality rate of SARS-CoV-2 in patients with DVT and the aggravation of the condition by the novel variant of the virus. The challenges are to improve the prevention of thrombosis, perform an early diagnosis and establish adequate treatment.
The identification of the physiopathological processes involved in thrombotic events is fundamental to the establishment of the best prophylactic and therapeutic measures. Anticoagulant therapy with heparin is the most widely used form throughout the world, but an important failure is seen at the moment, with a significant increase in the occurrence of thrombotic events associated with the Gamma variant. The use of aspirin is another option, but only in select cases as monotherapy or combined with anticoagulant therapy. Therefore, the aim is to interfere with the cascade of coagulation or platelet aggregation.
SARS-CoV-2 has challenged these routine prevention methods because it encompasses multiple physiopathological mechanisms involving inflammation, the coagulation cascade and the immune response of the patient. Therefore, immunothrombosis constitutes our challenge, as routine measures have an unacceptable failure rate at the moment.
One of the options is the indication of an intermediate dose of heparin for selected patients in ICUs. The constant tracking of thrombotic events in these patients and that adjustment of the anticoagulant dose are conducts that many services employ. However, new measures must be taken with the emergence of the Gamma variant.
In patients with the Gamma variant in hospital ward, the combination of 100 mg of aspirin and a prophylactic dose of anticoagulant is a suggestion. This option used for the prevention of recurrent miscarriage due to antiphospholipid antibody syndrome, which constitutes a cause of immunothrombosis.6–8 Therefore, this is the best suggestion at the moment for patients admitted to ICUs and failed cases of intermediate anticoagulant therapy.
In summary, the Gamma variant is an aggravating factor for thrombotic events and greater mortality in these patients. Thus, there is a need for prophylaxis as well as a reevaluation of prophylactic conduct.
Conclusion
Deep vein thrombosis is an aggravating factor of mortality in patients with SARS-CoV-2, and the Gamma variant is an aggravating factor of both thrombotic events and mortality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these aspects. All authors took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declared no financial support received for this study.
Disclosure
The authors declared no conflict of interest for this study.
References
1. Voicu S, Delrue M, Chousterman BG, et al. Imbalance between procoagulant factors and natural coagulation inhibitors contributes to hypercoagulability in the critically ill COVID-19 patient: clinical implications. Eur Rev Med Pharmacol Sci. 2020:9161–9168. doi:10.26355/eurrev_202009_22866
2. Bozzani A, Arici V, Tavazzi G, et al. Acute arterial and deep venous thromboembolism in COVID-19 patients: risk factors and personalized therapy. Surgery. 2020. doi:10.1016/j.surg.2020.09.009
3. Gibson CJ, Alqunaibit D, Smith KE, et al. Probative value of the D-Dimer assay for diagnosis of deep venous thrombosis in the coronavirus disease 2019 syndrome. Crit Care Med. 2020;48(12):e1322–e1326. doi:10.1097/CCM.0000000000004614
4. Clark CC, Jukema BN, Barendrecht AD, et al. Thrombotic events in COVID-19 are associated with a lower use of prophylactic anticoagulation before hospitalization and followed by decreases in platelet reactivity. Front Med. 2021. doi:10.3389/fmed.2021.650129
5. Faria NR, Mellan TA, Whittaker C, et al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021. doi:10.1126/science.abh2644
6. Spegiorin LC, Galão EA, Bagarelli LB, Oliani AH, de Godoy JM. Prevalence of anticardiolipin antibodies in pregnancies with history of repeated miscarriages. Open Rheumatol J. 2010;4:28. doi:10.2174/1874312901004010028
7. de Godoy JM, de Godoy MF, Braile DM. Recurrent thrombosis in patients with deep vein thrombosis and/or venous thromboembolism associated with anticardiolipin antibodies. Angiology. 2006;57(1):79–83. doi:10.1177/000331970605700111
8. Doms J, Horisberger A, Ribi C. Prise en charge du syndrome des anticorps antiphospholipides chez l’adulte [Management of the antiphospholipid syndrome in adults]. Rev Med Suisse. 2020;16(689):670–674.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
