Back to Journals » Clinical Interventions in Aging » Volume 18
Modified Frailty Index and Albumin-Fibrinogen Ratio Predicts Postoperative Seroma After Laparoscopic TAPP
Authors Zhou Y, Ge Y, Liu J, Shen W, Gu H, Cheng G
Received 22 April 2023
Accepted for publication 8 August 2023
Published 22 August 2023 Volume 2023:18 Pages 1397—1403
DOI https://doi.org/10.2147/CIA.S418338
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Yang Zhou, Yongxiang Ge, Jian Liu, Weijian Shen, Hailiang Gu, Guochang Cheng
Department of Hernia and Pediatric Surgery, Taizhou People’s Hospital, Taizhou Clinical Medical School of Nanjing Medical University, Taizhou City, Jiangsu Province, 225300, People’s Republic of China
Correspondence: Guochang Cheng, Email [email protected]
Background: Postoperative seroma is the most common minor complication after inguinal hernia repair surgery and can have negative consequences. The objective of this study was to identify potential risk factors for postoperative seroma.
Methods: This study consecutively included 354 elderly patients with inguinal hernia who underwent laparoscopic Transabdominal preperitoneal Patch Plasty (TAPP). Seroma diagnosis was conducted by the same experienced surgeon based on the physical examinations combined with ultrasound. Risk factors for seroma were identified through univariate analysis and subsequently included in the binary multivariate logistic regression model.
Results: A total of 40 patients experienced postoperative complications of seroma, with an incidence rate of 11.3% (40/354). The binary logistic regression analysis revealed that obesity (OR: 2.98, 95% CI: 1.20– 7.41, P = 0.018), disease duration ≥ 4.5 years (OR: 4.88, 95% CI: 2.14– 11.18, P < 0.001), albumin-fibrinogen ratio (AFR) level < 9.25 (OR: 6.13, 95% CI: 2.00– 18.76, P = 0.001), and modified frailty index (mFI) score ≥ 0.225 (OR: 6.38, 95% CI: 2.69– 15.10, P < 0.001) were four independent risk factors for postoperative seroma.
Conclusion: Obesity, prolonged disease duration, decreased AFR level, and increased mFI score independently predict postoperative seroma after laparoscopic TAPP.
Keywords: inguinal hernia, Transabdominal preperitoneal Patch Plasty, modified frailty index, albumin-fibrinogen ratio, risk factor
Introduction
Inguinal hernia is a very common surgical condition and over 20 million patients undergo inguinal hernia repair surgery worldwide every year.1 The prevalence of inguinal hernia increases with age, and it is 8–10 times higher in men than women.2,3 Because of the advantages of small wounds and allowing visual inspection of both inguinal regions, laparoscopic repair constitutes a large proportion of inguinal hernia surgeries.4 Transabdominal preperitoneal Patch Plasty (TAPP) is a very commonly used surgical method for inguinal hernia repair.5
Seroma, defined as the localized accumulation of serous fluid within tissue, represents the most frequent minor complication following inguinal hernia repair surgery.6 Due to the varying definitions and interpretations of seroma, the reported seroma incidence rates range widely from 0.5% to 78%, suggesting significant discrepancies among different studies.7,8 Although seroma typically resolves within a few weeks, it can lead to various complications. Among these, infected seromas are particularly challenging and may necessitate mesh removal or result in hernia recurrence.9,10 The occurrence of seroma can result in prolonged hospital stays, reduced patient comfort during treatment, hernia patch displacement and hernia recurrence.1 Therefore, it is imperative to conduct extensive research on the factors contributing to the development of postoperative seroma. According to a recent study conducted by Atsushi et al,4 it was found that two risk factors significantly contribute to the formation of postoperative seroma/hematoma: hernia size ≥ 3 cm and internal inguinal hernia. Despite extensive research on the subject, there is currently no consensus regarding the specific risk factors associated with the development of postoperative seroma. In addition, most studies focus on the surgery associated factors as main reasons and the points towards systematic (eg, frailty) are quite limited. The objective of this study was to identify the potential risk factors for postoperative seroma formation following TAPP surgery.
Materials and Methods
Patients
This study consecutively included 354 elderly patients with inguinal hernia who underwent laparoscopic TAPP at Taizhou People’s Hospital between 2020 and 2022. The inclusion criteria were: (1) elderly patients ≥ 65 years old; (2) with clinical manifestations, imaging, and intraoperative findings that met the diagnostic criteria for inguinal hernia; (3) undergoing laparoscopic TAPP without contraindications; (4) with no history of previous inguinal surgery, and (5) follow-up ≥ 3 months. The exclusion criteria were: (1) lack of clinical data or follow-up; (2) recurrent hernia; (3) with blood coagulation disorder, and (4) undergoing laparotomy or conversion to open repair. This study was approved by the ethics committee of our Hospital and enrolled patients were required to offer written consent.
Surgical Procedures
Preoperative prophylactic antibiotics were selectively administered based on specific conditions with high risk of infection (eg, combined with several underlying disease), rather than being routinely prescribed. All surgeries were performed by the same experience surgical team under general anesthesia. The intra-abdominal CO2 pressure was maintained at 8–10 mmHg throughout the procedure. Following dissection, a pre-shaped lightweight polypropylene mesh (3D Max, Bard) was utilized to precisely fit the defect. The mesh was inserted through the 10 mm umbilical port and unrolled to cover the entire myopectineal orifice on the hernia side(s) without fixation. The peritoneal flap was closed utilizing a continuous suture pattern with 3–0 Vicryl sutures.
Data Collection
The data presented herein were obtained from the medical records of the subjects enrolled in this study: (1) Demographic data, including age, gender, body mass index (BMI), obesity, and smoking habits; (2) Disease and treatment-related data, including duration of disease, antithrombotic drug, history of abdominal surgery, sides, operation time, hernia aperture diameter, types of hernias, classification of hernias, emergency surgery, and mFI; (3) Preoperative laboratory data (obtained on the morning of the day prior to surgery), including hemoglobin, white blood cell (WBC), C-reactive protein (CRP), albumin, fibrinogen, neutrophil, lymphocyte, and platelet.
Observational Endpoints and Definitions
The primary endpoint of the current study was the occurrence of seroma formation within 3 months following TAPP surgery. Patients were routinely follow-up at postoperative 7 days, 1, and 3 months. Seroma diagnosis was conducted by the same experienced surgeon based on the physical examinations combined with ultrasound. A seroma is characterized as the accumulation of fluid beneath the skin without the presence of any solid component.11
Modified frailty index (mFI) was calculated based on the previous criteria, incorporating eleven components (dividing the number of positive items by 11).12,13 The albumin-fibrinogen ratio (AFR) was determined by dividing the serum albumin level by the fibrinogen level. The neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) were calculated by dividing the levels of neutrophils and platelets, respectively, by the level of lymphocytes.
Statistical Analysis
The statistical analysis was conducted using SPSS 23.0 (SPSS Inc, IL, USA) and GraphPad Prism 9.0 (GraphPad Inc., CA, USA), respectively. The data are presented as means accompanied by their corresponding standard deviations (SD) and numbers expressed in percentages (n,%). Statistical analysis was conducted using Student t, Mann Whitney U, and Chi-square tests as appropriate. Additionally, a receiver operating characteristic (ROC) curve was constructed to evaluate the predictive and cut-off values of continuous variables. Binary logistic regression analyses were performed to identify risk factors for postoperative seroma. A test for multicollinearity, which involved the use of the tolerance and Variance Inflation Factor (VIF), was performed to assess the presence of multicollinearity among the factors. Significance was set at a two-tailed P-value of < 0.05.
Results
Based on the predefined inclusion and exclusion criteria, a total of 354 elderly patients with inguinal hernia were ultimately enrolled in this study. The cohort had an average age of 76.2 years, with male patients accounting for 85.9% (304/354) of the sample. Within the first three months after surgery, a total of 40 patients experienced postoperative complications of seroma, with an incidence rate of 11.3% (40/354). Table 1 displays the demographic, disease-related, and treatment-related characteristics of patients with or without postoperative seroma. Patients who developed seroma exhibited a significantly higher rates of obesity (P = 0.003), a longer duration of disease (P = 0.013), and a larger hernia aperture diameter (P = 0.003) compared to those without seroma. Patients in the seroma group exhibited a higher incidence of bilateral hernias (P = 0.041) and correspondingly longer operative duration (P = 0.023). Moreover, patients with irreducible/incarcerated hernias (P = 0.043) or those undergoing emergency surgery (P = 0.018) appear to have a higher susceptibility to seroma formation.
 |
Table 1 Variables Associated with Postoperative Seroma in Elderly Patients with Inguinal Hernia After TAPP |
The comparison of laboratory variables revealed no significant differences in hemoglobin, WBC, NLR, and PLR between patients with or without seroma (P > 0.05). Patients in the seroma group exhibited significantly lower levels of AFR (P < 0.001), higher levels of CRP (P = 0.040), and a greater mFI score (P < 0.001) compared to those in the non-seroma group.
Subsequently, we conducted ROC curve analyses to determine the optimal predictive values and cut-off points for continuous variables (with a significance level of P < 0.05 as shown in Table 1 and Table 2). As illustrated in Figure 1, the duration of disease (cut-off value: 4.5 years, sensitivity: 76.75%, specificity: 57.50%, AUC: 0.632, P = 0.007), operation time (cut-off value: 68.5 min, sensitivity: 69.43%, specificity: 55.00%, AUC: 0.609, P = 0.025), hernia aperture diameter (cut-off value: 4.5 cm, sensitivity: 75.16%, specificity: 47.50%, AUC: 0.651, P = 0.002), AFR (cut-off value: 9.25, sensitivity: 46.82%, specificity: 87.50%, AUC: 0.706, P < 0.001), and mFI score (cut-off value: 0.225, sensitivity: 72.93%, specificity: 67.50%, AUC: 0.744, P < 0.001) were five predictive factors for the occurrence of postoperative seroma.
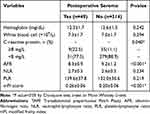 |
Table 2 Laboratory Variables Associated with Postoperative Seroma in Elderly Patients with Inguinal Hernia After TAPP |
Based on the optimal cut-off points, continuous variables were dichotomized into high (≥cut-off value) and low (< cut-off value) categories. As presented in Table 3, the multicollinearity analysis indicated no significant evidence of linearity between postoperative seroma and the potential risk factors. The binary logistic regression analysis revealed that obesity (OR: 2.98, 95% CI: 1.20–7.41, P = 0.018), disease duration ≥ 4.5 years (OR: 4.88, 95% CI: 2.14–11.18, P < 0.001), AFR level < 9.25 (OR: 6.13, 95% CI: 2.00–18.76, P = 0.001), and mFI score ≥ 0.225 (OR: 6.38, 95% CI: 2.69–15.10, P < 0.001) were four independent risk factors for postoperative seroma.
 |
Table 3 Binary Multivariate Logistic Regression Analysis of Postoperative Seroma in Elderly Patients with Inguinal Hernia After TAPP |
Discussion
The exact cause of postoperative seroma remains incompletely understood. Given its adverse effects, investigating potential risk factors and implementing preventative measures is crucial for improving prognosis. The overall incidence of seroma in this study was 11.3%, as determined by physical examinations combined with ultrasound, which is consistent with the reported rate of 12.6% by Ruze et al14 and lower than the rate of 19.2% reported by Morito et al.4
This study firstly highlighted obesity, disease duration ≥ 4.5 years, AFR level < 9.25, and mFI score ≥ 0.225 as four independent risk factors for postoperative seroma. Previous studies have reported a close relationship between the hernia aperture diameter and the formation of postoperative seroma.14 The local tissue adhesion and increased surgical difficulty caused by large hernia aperture diameter are probably the main reasons for the increased risk of postoperative seroma formation. However, our results did not support hernia aperture diameter as an independent risk factor for postoperative seroma. We consider that different patient characteristics, and different surgical strategies (eg, patch types, fixation methods, etc.) were the main potential reasons for the different conclusions.
A previous study conducted by Tomita et al15 has indicated that patients with an elevated BMI are at a higher risk of developing seroma compared to those with a normal BMI. Additionally, another study by Klink et al16 has also revealed a strong correlation between higher BMI and increased formation of seroma. These findings are in line with our results, indicating that patients with obesity exhibit a disproportionately enlarged wound cavity, which subsequently facilitates the development of seroma.16 Our research has also uncovered a strong correlation between the duration of the disease and the formation of seromas. We consider that long-term inguinal hernia, which contains a significant amount of abdominal contents within the hernia sac, is prone to inducing local inflammatory responses. This can lead to hyperplasia of postoperative scar tissue, obstruction of lymphatic reflux channels and an increased risk of postoperative seroma. This could potentially serve as an explanation for the independent association between the duration of disease and seroma risk.
AFR, which is calculated based on albumin and fibrinogen levels, serves as an optimal indicator for evaluating nutritional status, systemic inflammation, and coagulation function.17 Moreover, it has been widely utilized as a prognostic factor in various diseases.18,19 A decreased serum albumin is correlated with impaired tissue regeneration20 and elevated levels of proinflammatory mediators.21 In addition, fibrinogen exerts potent effects on both acute and reparative inflammatory pathways that modulate the spectrum of tissue injury, remodeling, and repair.22 A reduction in the albumin level or an increase in fibrinogen, or both, can lead to a decrease in the AFR. This may partially account for the strong correlation between the decreased AFR and postoperative seroma formation.
mFI, a widely used tool to assess the frailty status, has been widely used as prognostic factors in elderly patients.23,24 A recent study conducted on patients who underwent total joint arthroplasty revealed that frailty was associated with an increased risk of postoperative complications, including hematoma/seroma formation,25 which is consistent with our findings. Frailty is commonly associated with compromised immune function and reduced body resistance, rendering individuals more susceptible to infection and inflammation following surgery,26 thereby elevating the risk of postoperative seroma formation. Furthermore, the presence of muscle atrophy and impaired function in frail patients can negatively impact lymphatic drainage and fluid metabolism,27,28 potentially contributing to the development of postoperative seroma.
In conclusion, this study has underscored that obesity, prolonged disease duration, decreased AFR level, and increased mFI score are four independent risk factors for postoperative seroma in elderly patients with inguinal hernia after laparoscopic TAPP. This study has some limitations. The single centre single surgeon setting without an independent assessor of the clinical results parameters is a main weakness. Moreover, whether the improvements of some factors (eg, AFR) can reduce the incidence of seroma needs to be verified by further prospective studies.
Data Sharing Statement
Please contact the corresponding author for data requests.
Ethics Approval and Consent to Participate
This study was approved by the ethics committee of Taizhou People’s Hospital, Taizhou Clinical Medical School of Nanjing Medical University. All methods were carried out in accordance with relevant guidelines by Declaration of Helsinki. Written Informed consent was obtained from all participants/patients.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362(9395):1561–1571. doi:10.1016/S0140-6736(03)14746-0
2. Jensen KK, Henriksen NA, Jorgensen LN. Textbook of Hernia. Springer International Publishing; 2017.
3. HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1–165.
4. Morito A, Kosumi K, Kubota T, et al. Investigation of risk factors for postoperative seroma/hematoma after TAPP. Surg Endosc. 2022;36(7):4741–4747. doi:10.1007/s00464-021-08814-2
5. Hayakawa S, Hayakawa T, Watanabe K, et al. Evaluation of long-term chronic pain and outcomes for unilateral vs bilateral circular incision transabdominal preperitoneal inguinal hernia repair. Ann Gastroenterol Surg. 2022;6(4):577–586. doi:10.1002/ags3.12556
6. Cihan A, Ozdemir H, Uçan BH, et al. Fade or fate. Seroma in laparoscopic inguinal hernia repair. Surg Endosc. 2006;20(2):325–328. doi:10.1007/s00464-005-0052-6
7. Parker HH, Nottingham JM, Bynoe RP, Yost MJ. Laparoscopic repair of large incisional hernias. Am Surg. 2002;68(6):530–3; discussion 533–4. doi:10.1177/000313480206800605
8. Birch DW. Characterizing laparoscopic incisional hernia repair. Can J Surg. 2007;50(3):195–201.
9. Edwards C, Angstadt J, Whipple O, Grau R. Laparoscopic ventral hernia repair: postoperative antibiotics decrease incidence of seroma-related cellulitis. Am Surg. 2005;71(11):931–5; discussion 935–6. doi:10.1177/000313480507101106
10. Sodergren MH, Swift I. Seroma formation and method of mesh fixation in laparoscopic ventral hernia repair--highlights of a case series. Scand J Surg. 2010;99(1):24–27. doi:10.1177/145749691009900106
11. Willemin M, Schaffer C, Kefleyesus A, et al. Drain versus no drain in open mesh repair for incisional hernia, results of a prospective randomized controlled trial. World J Surg. 2023;47(2):461–468. doi:10.1007/s00268-022-06725-4
12. Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–30; discussion 1530–1. doi:10.1097/TA.0b013e3182542fab
13. Meng Y, Zhao P, Yong R. Modified frailty index independently predicts postoperative pulmonary infection in elderly patients undergoing radical gastrectomy for gastric cancer. Cancer Manag Res. 2021;13:9117–9126. doi:10.2147/CMAR.S336023
14. Ruze R, Yan Z, Wu Q, Zhan H, Zhang G. Correlation between laparoscopic transection of an indirect inguinal hernial sac and postoperative seroma formation: a prospective randomized controlled study. Surg Endosc. 2019;33(4):1147–1154. doi:10.1007/s00464-018-6374-y
15. Tomita K, Yano K, Masuoka T, Matsuda K, Takada A, Hosokawa K. Postoperative seroma formation in breast reconstruction with latissimus dorsi flaps: a retrospective study of 174 consecutive cases. Ann Plast Surg. 2007;59(2):149–151. doi:10.1097/SAP.0b013e31802c54ef
16. Klink CD, Binnebösel M, Lucas AH, et al. Serum analyses for protein, albumin and IL-1-RA serve as reliable predictors for seroma formation after incisional hernia repair. Hernia. 2011;15(1):69–73. doi:10.1007/s10029-010-0746-0
17. Ying J, Zhou D, Gu T, Huang J, Liu H. Pretreatment albumin/fibrinogen ratio as a promising predictor for the survival of advanced non small-cell lung cancer patients undergoing first-line platinum-based chemotherapy. BMC Cancer. 2019;19(1):288. doi:10.1186/s12885-019-5490-y
18. Chen S, Yan H, Du J, et al. Prognostic significance of pre-resection albumin/fibrinogen ratio in patients with non-small cell lung cancer: a propensity score matching analysis. Clin Chim Acta. 2018;482:203–208. doi:10.1016/j.cca.2018.04.012
19. Qin A, Wang S, Dong L, et al. Prognostic value of the albumin-to-fibrinogen ratio (AFR) in IgA nephropathy patients. Int Immunopharmacol. 2022;113(Pt A):109324. doi:10.1016/j.intimp.2022.109324
20. Horváthy DB, Simon M, Schwarz CM, et al. Serum albumin as a local therapeutic agent in cell therapy and tissue engineering. Biofactors. 2017;43(3):315–330. doi:10.1002/biof.1337
21. Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17(6):432–437. doi:10.1111/j.0894-0959.2004.17603.x
22. Luyendyk JP, Schoenecker JG, Flick MJ. The multifaceted role of fibrinogen in tissue injury and inflammation. Blood. 2019;133(6):511–520. doi:10.1182/blood-2018-07-818211
23. Lu J, Zheng HL, Li P, et al. High preoperative modified frailty index has a negative impact on short- and long-term outcomes of octogenarians with gastric cancer after laparoscopic gastrectomy. Surg Endosc. 2018;32(5):2193–2200. doi:10.1007/s00464-018-6085-4
24. Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J Am Coll Surg. 2018;226(2):173–181.e8. doi:10.1016/j.jamcollsurg.2017.11.005
25. Zalikha AK, Pham L, Keeley J, Hussein IH, El-Othmani MM. Frailty among total hip and knee arthroplasty recipients: epidemiology and propensity score-weighted analysis of effect on in-hospital postoperative outcomes. J Am Acad Orthop Surg. 2023;31(6):292–299. doi:10.5435/JAAOS-D-22-00642
26. Li H, Manwani B, Leng SX. Frailty, inflammation, and immunity. Aging Dis. 2011;2(6):466–473.
27. Shang T, Liang J, Kapron CM, Liu J. Pathophysiology of aged lymphatic vessels. Aging. 2019;11(16):6602–6613. doi:10.18632/aging.102213
28. Jeejeebhoy KN. Malnutrition, fatigue, frailty, vulnerability, sarcopenia and cachexia: overlap of clinical features. Curr Opin Clin Nutr Metab Care. 2012;15(3):213–219. doi:10.1097/MCO.0b013e328352694f
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

