Back to Journals » Clinical Ophthalmology » Volume 17
Modified Anterior Lamellar Recession for All Grades of Upper Eyelid Trachomatous Cicatricial Entropion
Authors Ibrahim ENA , Tharwat E , Khalil MMAA , Mohammed AR, Mohammed MF , Alkady AMM , Ezzeldin ER , Hassan Ahmed RE , Al-Faky YH, Hassanein M, Elsayed AN , Abd El-Salam ME
Received 12 May 2023
Accepted for publication 18 July 2023
Published 10 August 2023 Volume 2023:17 Pages 2323—2332
DOI https://doi.org/10.2147/OPTH.S420992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ezzat Nabil Abbas Ibrahim,1,* Ehab Tharwat,2,* Mahmoud Mohammed Ahmed Ali Khalil,1 Ahmed Rabie Mohammed,1 Mostafa F Mohammed,1 Ahmed Mohammed Madinah Alkady,1 Ezzeldin Ramadan Ezzeldin,2 Riad Elzaher Hassan Ahmed,2 Yasser H Al-Faky,3 Mohamed Hassanein,1 Ahmed N Elsayed,1 Mohammed Eid Abd El-Salam1,*
1Department of Ophthalmology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt; 2Department of Ophthalmology, Faculty of Medicine, Al-Azhar University, Damietta, Egypt; 3Department of Ophthalmology, King Faisal Specialist Hospital and Research Center, Riyadh, Saudia Arabia
*These authors contributed equally to this work
Correspondence: Ehab Tharwat, Department of Ophthalmology, Faculty of Medicine, Al-Azhar University, Alkawthar Building at Alshenawy St, from Algeish St, Mansoura, Dakahlia, Egypt, Tel +20 10 06952497, Fax +20 50 2507370, Email [email protected]
Purpose: This study aims to assess the combination of anterior lamellar recession (ALR) with blepharoplasty, suprasternal fixation, and internal eyelash bulb extirpation of aberrant lashes posteriorly located in patients with any grade of upper eyelid trachomatous cicatricial entropion.
Patients and Methods: We reviewed the clinical data of eighty-six patients (143 eyelids) including age, gender, systemic medical illnesses, and comprehensive ophthalmological assessment. Eyelid evaluation was recorded, including laterality, previous surgical technique used, possible trichiasis etiology, abnormality of the lid margin, tarsal plate consistency (shrinkage or loosening), skin fold overhanging, laxity of the pretarsal skin, margin reflex distance 1 (MRD1), lagophthalmos, and lid retraction. The success rate was assessed at 3, 6, 9, and 12 months postoperative.
Results: The success rate was 97.2% in the third month, which decreased significantly to 92.3% in the 6th month and 90.2% in the 9th month (P = 0.01, and 0.001 respectively). In the 9th month, we had fourteen failed cases. All of them were submitted for a second intervention. Three underwent electrolysis, four cases underwent re-internal bulb extirpation, four cases underwent the same procedure, and three cases underwent epilation. The success of the failed cases after the second intervention was significantly associated with the type of reintervention (P = 0.03), in which all of them succeed except two cases that underwent epilation. Kaplan-Meier analysis showed that the mean recurrence time in our study was 6.8 months (95% CI = 5.8– 7.7 months).
Conclusion: This study showed the combination of ALR with blepharoplasty, suprasternal fixation, and cauterization or internal bulb extirpation of posteriorly located lashes procedure resulted in a high success rate in patients with any form of UCE with no increase in incidence or degree of lagophthalmos associated with UCE.
Keywords: anterior lamellar recession, ALR, blepharoplasty, cicatricial entropion, suprasternal fixation
Introduction
Trachomatous trichiasis (TT) is a major risk factor for corneal opacity (CO), which is the fourth leading cause of blindness in the world (5.1%).1 Communities with inadequate environmental cleanliness and low socioeconomic status in rural areas are most commonly affected by trachoma.2–4 Population-based surveys in Egypt have reported that trachoma is still a public health problem.5
There is widespread consensus that primary TT should be surgically treated. The World Health Organization recommends surgery for one or more lashes that rub together, even if the lashes are in the center, on the edges, or in different grades. This is because patients with mild trichiasis may not be checked on for a long time, which raises the risk that the condition will get worse and cause vision loss.6
There are various surgical techniques available depending on the severity of upper eyelid cicatricial entropion (UCE). Each UCE severity requires a different procedure, so the type of procedure used should be customized.7 It was reported that previous surgical procedures may violate the transconjunctiva which may promote the inflammatory process which in turn inducing the trachomatous scarring process and increasing the conjunctival contracture.8 So, we need a new surgical technique to avoid such disadvantages.
ALR is one of the procedures used to treat cicatricial entropion and trichiasis.9 Few studies present the effect of modifications to this procedure in trachomatous entropion and trichiasis.10 Because trachoma is common in our country, there is a probability that the number of surgeries for TT will rise.5
In the present study, we aimed to assess the combination of anterior lamellar recession with blepharoplasty, suprasternal fixation, and internal eyelash bulb extirpation of aberrant lashes posteriorly located in patients with any grade of upper eyelid trachomatous cicatricial entropion.
Materials and Methods
Study Populations
This was a retrospective study that reviewed the data of eighty-six patients (143 eyelids) who underwent surgical correction for upper eyelid cicatricial entropion from May 2018 to March 2021 in a tertiary university hospital. Our study followed the Helsinki Declaration principles. Ethical Approval was obtained from the Committee of Al-Azhar University Faculty of Medicine, and this approval included waiver to use the medical records as our institution took the consent from the patients to use their medical data in the future at the time of their admission. This study was registered on the Clinical trial.gov (NCT05854420). The inclusion criteria were: All patients presented with upper lid trachomatous cicatricial entropion associated with rubbing lashes. Patients having a history of argon laser ablation, electrolysis, epilation, or past unsuccessful surgery were also included. The exclusion criteria were: 1) Patients with a follow-up period of fewer than 12 months. 2) Patients with very severe UCE and required posterior lamellar grafts. 3) Patients with etiology other than trachoma. 3) Patients with dysplastic lashes without entropion were excluded.
Data Collection
We reviewed clinical data of the patients including age, gender, systemic medical illnesses, and comprehensive ophthalmological assessment which included best corrected visual acuity “BCVA”, examination of the anterior segment by the slit lamp bio microscopy especially, the status of the cornea and assessment of the degree of corneal opacity if present as well as posterior segment evaluation. Eyelid evaluation was recorded, including laterality, previous surgical technique used, possible trichiasis etiology, abnormality of the lid margin, tarsal plate consistency (shrinkage or loosening), skin fold overhanging, laxity of the pretarsal skin, margin reflex distance 1 (MRD1), lagophthalmos, and lid retraction. The severity of the eyelid involvement was categorized as mild (on up gaze, the meibomian gland orifices migrate posteriorly and the lash touches the globe), moderate (as mild with either contact between the lash and globe in the primary position or tarsal plate thickening), and severe (as moderate with the presence of keratin plaques and lid retraction causing incomplete lid closure). The tarsal plate consistency was recorded, either shrinkage (shortening with or without thickening) or loosening (loss of tarsal consistency). Anterior lamellar laxity was defined as an overhanging skin fold beyond the lid margin and/or pretarsal skin laxity.8
Surgical Procedure
The surgeries were performed by two Surgeons (ENA) and (MEA) (Figures 1 and 2). The surgery was done under local anesthesia (5 mL of lidocaine (2%) with epinephrine 1:100 000). At the intended eyelid crease across the entire lid, the inferior incision was marked. Depending on how much redundant skin needed to be removed, a second (upper) incision was made at various distances from the first line, guided by a pinching test to avoid lagophthalmos. Then, the skin was incised with the excision of excess skin leaving the orbicularis muscle. The orbicularis muscle (anterior lamella) opened and was dissected to identify the upper tarsal margin. The sub orbicularis dissection continued using Westcott scissors to expose the anterior tarsal surface to reach the upper lid margin. Then, a lid spatula was inserted to evert the lid making the lid margin face up; then, a grey line incision was made to dissect the anterior lamella from the posterior lamella for about 2 mm above the lid margin peeling the whole anterior lid margin with aberrant lashes and keratinization away from the tarsus then meet the crease incision. A bipedicle flap was formed, completely separating the anterior lamella from the tarsus. Cauterization and internal eyelash bulb extirpation of aberrant or metaplastic lashes originating from posterior lamella.
The anterior lamella was retracted until it was 3–4 mm above the edge of the eyelid. Then, it was sutured 4–5 interrupted sutures by vicryl (6–0) (Ethicon, Cincinnati, OH, USA). The additional anterior lamella was then removed if needed.
Finally, 3–5 supra tarsal fixation sutures of the anterior lamella were put anchoring the upper border of the orbicularis muscle of the recessed anterior lamella to the supratarsal part 2 mm above the upper border of the tarsus to the levator aponeurosis. After applying a topical antibiotic ointment, the eyelid was dressed. After surgery, eye patching, systemic antibiotic, analgesic and topical antibiotics were given for every patient.
Follow-Up
The patients were seen one day postoperative (opening the dressing), one week (suture removal), three months, six months, nine months, and after one year (success assessment). The primary outcome measure was assessed as success or failure. Success was defined as none of the lashes touching the cornea. In contrast, failure was defined as having any eyelashes touching or reoperation during the follow-up. The secondary outcomes were visual acuity, corneal status, papillary reaction, conjunctivalization of the lid margin, feeling of pain, lacrimation, and dryness.”
Statistical Analysis
Statistical analysis was performed with SPSS statistical software, version 26 (IBM, Chicago, Illinois, USA). The normality of the data was tested by the Kolmogorov–Smirnov test. Continuous data were expressed as mean ± SD. Categorical data were expressed as numbers and percent (N (%)) and were compared by using the Chi-square test. Kaplan-Meier analysis was done to determine the period which precedes the failure. P-value <0.05 was considered significant.
Results
Available records included 86 (143 eyelids) patients diagnosed with upper lid cicatricial entropion associated with rubbing lashes. Among the included patients, 35 (40.7%) were males, and 51 (59.3%) were females, with a mean age of 58.6 ± 5.8 years. Fifty-seven 57 (66.2%) patients had bilateral cicatricial entropion, and 29 (33.7%) patients had unilateral cicatricial entropion (Table 1). All patients had signs of trachoma, such as pannus siccus, subconjunctival fibrosis, and/or Post Trachomatous Degenerations (PTDs).
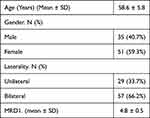 |
Table 1 Demographics and Baseline Characteristics of the Studied Patients |
The baseline clinical characteristics of the studied patients are described in Table 2. Most of the studied eyelids had a moderate degree of entropion 87 (60.8%). However, severe entropion with misdirected and metaplastic lashes and lid retraction was present in 19 eyelids (13.3%), with a mean preoperative MRD1 of 4.8 ± 0.5 mm. Regarding the extent of affection, 88.8% of the studied eyelids had generalized affection.
 |
Table 2 Baseline Clinical Data of the Studied Eyelids (n = 143) |
In terms of previous intervention, previous electrolysis for rubbing lashes was done in thirty-one eyelids (21.7%), partially epilated lashes were done in sixty-three eyelids (44.1%), posterior lamellar tarsal rotation (PLTR) was done in seventeen eyelids (11.9%), and ALR was done in eleven eyelids (7.7%). Forty-six eyes (38.3%) had preoperative corneal punctate epithelial erosions.
According to the corneal state of the studied eyelids, corneal opacity of variable densities and the location was present in sixty-five eyes (45%), and Punctal epithelial erosion was found in fifty-six eyelids (39%).
Skin laxity was present in 109 eyelids (76.2%), atrophic tarsus (shrinkage) was present in thirty eyelids (21%), loosening of the tarsal plate was found in thirty eyelids (21%), and lagophthalmos in fifteen eyelids (10.5%) (Table 2).
All patients had post-operative lid edema and/or ecchymosis, yet all had good lid closure. By the fourth week, all the lids had a slight thickening, which got better over time and went away by the third month. No postoperative ptosis or lagophthalmos or new onset upper eyelid retraction with post-operative MRD1 6.30 ± 1.3 mm.
The success rate was 97.2% in the third month, which decreased significantly to 92.3% in the 6th month and 90.2% in the 9th month (P = 0.01, and 0.001 respectively). In the 9th month, we had fourteen failed cases (Table 3). All of them were submitted for a second intervention. Three underwent electrolysis, four cases underwent re-internal bulb extirpation, four cases underwent A, and three cases underwent epilation. The success of the failed cases after the second intervention was significantly associated with the type of reintervention (P = 0.03), in which all of them succeed except two cases that underwent epilation (Table 4).
 |
Table 3 Success Rate at the Follow-Up Periods |
 |
Table 4 Association Between the Type of Reintervention and Success Rate in Failed Cases at the 9th Month Postoperative. (N = 14) |
Factors that can affect the success rate are described in Table 5, and we found that postoperative notching or lash ptosis is the only significant factor that can affect the success rate (P = 0.001, 0.05, respectively).
 |
Table 5 Factors Affecting the Success Rate at 9th Months Postoperative |
Kaplan-Meier analysis showed that the mean recurrence time in our study was 6.8 months (95% CI = 5.8–7.7 months) (Figure 3).
 |
Figure 3 Kaplan-Meier analysis for the recurrence time. |
Discussion
The shortening of the posterior lamella and subsequent in-turning of the lid edge, which may be secondary to some etiologies, cause cicatricial upper eyelid entropion. These causes include advanced Meibomian Gland Dysfunction and trachoma, Burns, Stevens-Johnson syndrome, vernal keratoconjunctivitis, herpes zoster ophthalmicus, and ocular cicatricial pemphigoid. The success of surgical procedures for repair depends on choosing the right approach for the disease.11
Most surgical series indicated a considerable recurrence rate (21–71%) despite the variety of treatment modalities available for treating UCE.12 ALR is a well-known treatment with a reported high success rate of 72–89% for treating cicatricial entropion.9,13
In our case series, we added the blepharoplasty, suprasternal fixation sutures, and internal bulb extirpation to the anterior lamellar recession procedure to address postoperative anterior lamellar sliding and posteriorly located metaplastic lashes. We performed this procedure in patients with any grade of cicatricial lid margin abnormality secondary to trachoma.
The complete success rate was 90.2% in the 9th month and 98.6% in the 12th month. The success rate was not related to tarsal-plate consistency. The failed cases Included 6 cases with normal tarsus, five with atrophic tarsus, and three with tarsal loosening. We noticed an eyelid margin thickening in most of the study cases, especially in the first month after the operation, decreasing with time. This was due to the healing of the bare eyelid margin.
We could argue that avoiding an incision along the eyelid’s margin by instead performing an anterior lamellar recession from the crease would preserve the natural thickness of the eyelid’s margin. Because the pathology lies at the eyelid margin, anterior lamellar recession at the site of the incision will not alleviate the underlying cicatricial force. A full separation and depression of the anterior lamella on the posterior lamella are required for the eversion effect to take place. Thus, it is possible that the pathology can be addressed, and anterior lamella dissection can be facilitated by combining the crease incision with the assumed grey line incision.
The procedure for ALR in this study was similar to the procedure described by Bi et al,14 and Ross et al12 with a few modifications where we postponed the grey line incision after the crease incision and used a lid spatula in the pretarsal plane after dissection of pretarsal orbicularis to evert the lid making the rotated lid margin facing up facilitating the meticulous dissection of the two lamellae at the assumed grey line.
Skin redundancy of the upper eye lid is common after ALR technique, however in our study the addition of blepharoplasty prevented such complication which agree with Ahmed et al,12 and Bi et al.14
Sliding of the anterior lamellae to its preoperative site is a common cause of ALR failure.15
Therefore, different surgical approaches have been proposed to counteract this anterior lamellar sliding, such as taking a mattress suture between the upper tarsus and the lash line.16 Another technique was proposed by Tie et al,17 which removes the excess skin and orbicularis of the upper lid followed by transplantation of the amniotic membrane. Bi et al14 and Sadiq et al18 combined blepharoplasty with their techniques with an outcome similar to our results.
Aghai et al,16 in a study that included blepharoplasty, anterior lamellar recession, and suprasternal fixation, showed a success rate of 75%. This difference between the two studies may be due to the fact that Aghai et al had smaller sample size, they did not do cauterization or internal bulb extirpation, and they excluded the UCE with lagophthalmos.
We believe that supra tarsal fixation increased the success rate and prevented long-term recurrence of entropion but did not affect the lagophthalmos status according to our results which showed no increase in the degree of preoperative lagophthalmos or appearance of new cases of lagophthalmos as a complication of the procedure. Hence, we recommend our procedure in all forms of UCE, even if there is preoperative lagophthalmos.
To move the posterior lamella inferiorly and make up for the degree of lid retraction, several authors advocated dissecting the upper lid retractors from the tarsus during UCE surgery.12,16 Barr et al19 reasoned that the failure to execute concurrent levator recession was the cause of the high recurrence rate (21%), which was reported in their study after ALR. However, we believe that supra tarsal fixation combined with blepharoplasty addressed this issue and prevented the high recurrence rate according to our results, where the success rate in our study was observed in 129 (90.2%) at the 9th month postoperative.
The mean recurrence time in our study was 6.8 months (95% CI = 5.8–7.7 months), which could be due to either the anterior lamellar sliding during the healing. In this study, we had no early cases of recurrence; usually, due to cauterization or internal bulb extirpation that was added to the ALR. Missing distichiasis and trichiasis, which might occur during the operation are considered a risk factor for failure, as documented by Aghai et al.16
Weak points in our study may include an evaluation of the cosmetic satisfaction of the patients and the surgeries done by two experienced surgeons in lid surgery which makes it difficult to generalize the procedure as a treatment for all cases of trachomatous cicatricial upper eyelid entropion.
Conclusion
Combination of ALR, blepharoplasty, suprasternal fixation, and cauterization or internal bulb extirpation of posteriorly located lashes is effective with a high success rate in patients with any form of UCE with no increase in incidence or degree of lagophthalmos associated with UCE.
Availability of the Data
The data set used or analyzed in this study available from the corresponding author (Ehab Tharwat) on reasonable request after taking approval from our institution to share the patient’s data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Al Arab GE. The burden of trachoma in the rural Nile Delta of Egypt: a survey of Menofiya governorate. Br J Ophthalmol. 2001;85:1406–1410. doi:10.1136/bjo.85.12.1406
2. World Health Organization. Report of the 4th Global Scientific meeting on trachoma, 27–29 November 2018. Geneva: World Health Organization; 2019.
3. Baneke A. Review: targeting trachoma: strategies to reduce the leading infectious cause of blindness. Travel Med Infect Dis. 2012;10:92–96. doi:10.1016/j.tmaid.2012.01.005
4. Callahan K, Ogale YP, Palmer SL, et al. Trachoma control as a vehicle toward international development and achievement of the millennium development goals. PLoS Negl Trop Dis. 2014;8:e3137. doi:10.1371/journal.pntd.0003137
5. Mousa A, Paul C, Kazanjian A, Bassett K. A community-based eye care intervention in Southern Egypt: impact on trachomatous trichiasis surgical coverage. Middle East Afr J Ophthalmol. 2015;22:478. doi:10.4103/0974-9233.167808
6. Mousa A, El Arab GE, Rashad E. Reaching women in Egypt: a success story. Comm Eye Heal. 2009;22:22–23.
7. Rajak SN, Collin JRO, Burton MJ. Trachomatous trichiasis and its management in endemic countries. Surv Ophthalmol. 2012;57:105–135. doi:10.1016/j.survophthal.2011.08.002
8. Diab MM, Allen RC. Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach. Eye. 2021;35:2781–2786. doi:10.1038/s41433-020-01306-y
9. Kemp EG, Collin JR. Surgical management of upper lid entropion. Br J Ophthalmol. 1986;70:575–579. doi:10.1136/bjo.70.8.575
10. Gawdat TI, Kamal MA, Saif AS, Diab MM. Anterior lamellar recession for management of upper eyelid cicatricial entropion and associated eyelid abnormalities. Int J Ophthalmol. 2017. doi:10.18240/ijo.2017.12.07
11. Gower EW, Merbs SL, Munoz BE, et al. Rates and risk factors for unfavorable outcomes 6 weeks after trichiasis surgery. Investig Opthalmology Vis Sci. 2011;52:2704. doi:10.1167/iovs.10-5161
12. Ross AH, Cannon PS, Selva D, Malhotra R. Management of upper eyelid cicatricial entropion. Clin Experiment Ophthalmol. 2011;39:526–536. doi:10.1111/j.1442-9071.2011.02503.x
13. Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol. 2015;2015:1–7. doi:10.1155/2015/568363
14. Bi YL, Zhou Q, Xu W, Rong A. Anterior lamellar repositioning with complete lid split: a modified method for treating upper eyelids trichiasis in Asian patients. J Plast Reconstr Aesthetic Surg. 2009;62:1395–1402. doi:10.1016/j.bjps.2008.06.035
15. Sodhi PK, Yadava U, Pandey RM, Mehta DK. Modified grey line split with anterior lamellar repositioning for treatment of cicatricial lid entropion. Ophthalmic Surg Lasers. 2002;33:169–174. doi:10.3928/1542-8877-20020301-19
16. Aghai GH, Gordiz A, Falavarjani KG, Kashkouli MB. Anterior lamellar recession, blepharoplasty, and supratarsal fixation for cicatricial upper eyelid entropion without lagophthalmos. Eye. 2016;30:627–631. doi:10.1038/eye.2016.12
17. Ti S-E, Tow SL, Chee S-P. Amniotic membrane transplantation in entropion surgery. Ophthalmology. 2001;108:1209–1217. doi:10.1016/S0161-6420(01)00599-1
18. Sadiq MN, Pai A. Management of trachomatous cicatricial entropion of the upper eye lid: our modified technique. J Ayub Med Coll Abbottabad. 2005;17:1–4.
19. Barr K, Essex RW, Liu S, Henderson T. Comparison of trichiasis recurrence after primary bilamellar tarsal rotation or anterior lamellar repositioning surgery performed for trachoma. Clin Experiment Ophthalmol. 2014;42:311–316. doi:10.1111/ceo.12197
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


