Back to Journals » Cancer Management and Research » Volume 10
Model of lymph node metastasis posterior to the right recurrent laryngeal nerve in papillary thyroid carcinoma
Authors Luo Y , Xu XC, Shen J , Shi JJ, Lu S , He W, Lei JY, Luo DC
Received 13 March 2018
Accepted for publication 3 May 2018
Published 6 August 2018 Volume 2018:10 Pages 2449—2455
DOI https://doi.org/10.2147/CMAR.S167997
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Leylah Drusbosky
Yi Luo,1 Xiao-Cheng Xu,2 Jie Shen,3 Jing-Jing Shi,4 Si Lu,5 Wei He,6 Jian-Yong Lei,7 Ding-Cun Luo4
1West China School of Medicine, Sichuan University, Chengdu, China; 2Department of Surgery of Thyroid and Breast, Wujiang District of Suzhou First People’s Hospital, Suzhou, China; 3Clinical Medical College, Nanjing Medical University, Nanjing, China; 4Department of Surgical Oncology, Hangzhou First People’s Hospital, Nanjing Medical University, Hangzhou, China; 5Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, China; 6Department of Oncology, Taixing People’s Hospital, Taixing, China; 7Department of Thyroid Surgery, West China hospital of Sichuan University, Chengdu, China
Background: Cervical lymph node metastasis (LNM) is a prognostic factor of papillary thyroid carcinoma (PTC). The way to deal with lymph node posterior to the right recurrent laryngeal nerve (LN-prRLN) is controversial. Nevertheless, if metastatic lymph nodes are not removed during the first operation, the subsequent salvage surgery of recurrent tumor in this area would entail high risk and complication. The purpose of this study was to develop a preoperative prediction model for LN-prRLN metastasis in PTC patients using clinicopathological characteristics.
Patients and methods: We performed a prospective study of 595 patients with PTC who underwent LN-prRLN dissection from March 2014 to June 2017. The clinicopathological data were randomly divided into derivation (n=476) and validation sets (n=119). A predictive model was initially established based upon the data of the derivation set via multivariate analyses, and the accuracy of the model was then examined with data of the validation set. The discriminative power of this model was assessed in both sets.
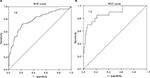
Results: Metastases of the LN-prRLN were identified in 102 (17.14%) of 595 patients. Age (odds ratio [OR] 0.971, 95% CI, 0.949–0.994, p=0.013), tumor size (OR 2.163, 95% CI, 1.431–3.270, p<0.001), capsular invasion (OR 1.934, 95% CI, 1.062–3.522, p=0.031), and right LNM (OR 3.786, 95% CI, 2.012–7.123, p<0.001) were significantly associated with LN-prRLN metastasis. The areas under the curves were 0.790 for the derivation set (sensitivity 71.95%, specificity 78.68%) and 0.878 for the validation set (sensitivity 85.00%, specificity 78.79%).
Conclusion: We developed and validated the first model to predict LN-prRLN metastases in patients with PTC based on clinicopathological parameters.
Keywords: papillary thyroid carcinoma, lymph node posterior to right recurrent laryngeal nerve, neck dissection, risk factors, metastasis, model
Introduction
Papillary thyroid carcinoma (PTC) is prone to cervical lymph node metastasis (LNM).1 At the time of diagnosis, approximately 30%–80% of PTC patients exhibit cervical lymph node metastases.2,3 The presence of cervical lymph node metastases adversely affected disease-free survival rate,4 especially for those measuring larger than or equal to 2 mm.5 Another study with long-term follow-up data showed an association with worse overall survival of the patients.6 Therefore, cervical lymph node dissection is usually performed during the surgical treatment of PTC, although this involves a number of issues that are not yet settled. One of the controversies concerns the lymph node posterior to the right recurrent laryngeal nerve (LN-prRLN) dissection in patients with PTC. Some researchers advised against routine LN-prRLN dissection because of the low rate of metastases to this region, the greater technical difficulty involved, and the resulting higher complication rate.7–13 On the other hand, if there are untreated metastases, the salvage operation would be substantially more difficult and risky. Therefore, there is a need for a model to estimate this risk, so that the diseases are optimally removed, while the rate of unnecessary procedure is minimized. To that end, we performed this prospective study to identify the risk factors for LN-prRLN metastasis in patients with PTC. Our earlier work involving patients suffering right thyroid lobe or bilateral PTC identified a range of factors showing positive association with the rate of LN-prRLN metastasis. They include patients’ age, tumor size of the right thyroid lobe, capsular invasion, number and size of the metastatic lymph nodes anterior to right recurrent laryngeal nerve (RLN), and the number of metastatic lymph nodes in the right lateral compartment.14 In this study, more patients were recruited and preoperative characteristics were recorded in details, including sex, age, tumor size and number, capsular invasion, and right lateral LNM. A prediction model was then developed as a tool to estimate the risk of LN-prRLN metastasis and facilitate therapeutic decision in the resection of PTC.
Patients and methods
In our study, 595 consecutive PTC patients (right PTC/ bilateral PTC) underwent LN-prRLN dissection conducted by a surgical team over a period of 40 months (from March 2014 to June 2017). Patients who had history of other malignant tumors or previous operation in this area were excluded. The size and number of thyroid tumors and the presence or absence of capsular invasion were recorded by high frequency B ultrasonography. Each thyroid cancer patient was independently examined by two ultrasonographers. If the two ultrasonographers had different opinions, the third ultrasonographer would participate in the examination to verify the data. The suspicious right lateral cervical lymph node metastases would be subjected to confirmation by fine needle aspiration cytology. All patients were followed up from 6 months to 46 months without local recurrence or distant metastasis (Table 1).
  | Table 1 Baseline characteristics of all patients Note: ‘’–’’ Not applicable. Abbreviation: LN-prRLN, lymph node posterior to the right recurrent laryngeal nerve. |
LN-prRLN dissection
In our study, all patients underwent conventional open thyroidectomy (hemithyroidectomy or total thyroidectomy) and neck dissection in the same operation. We subdivided the right cervical central compartment VI into right cervical central VI-1 subzone and VI-2 subzone. Right central VI-1 subzone lies anterior to the RLN bounded by the hyoid bone superiorly, the suprasternal notch inferiorly, the inner edge of the common carotid artery laterally, and the midline of the trachea medially. Right central VI-2 subzone lies posterior to the right RLN. The superior, inferior, lateral, and medial borders are the laryngeal entry points of RLN, the intersection of the RLN with the innominate artery (near the right apical pleura), the inner edge of the common carotid artery, and esophagus, respectively. The floor of right central VI-2 is the prevertebral fascia. All patients in this study underwent a lymph node dissection of both right cervical central VI-1 and VI-2 (LN-prRLN). Additional lateral compartment neck dissections would be performed if metastases were identified in this compartment.14 Two expert pathologists independently examined the surgical specimens.
Ethics statement
The research was approved by the institutional review board of Hangzhou First People’s Hospital, and each patient signed written informed consent form to participate in the study. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statistical analysis
Medians with interquartile ranges were calculated for continuous variables and numbers with percentages were reported for categorical variables. Mann-Whitney U test was used for continuous abnormally distributed variables, and χ2 test was used for categorical variables. Normality was tested with Q–Q plots and Kolmogorov-Smirnov tests. The data were subjected to univariate analysis to identify the possibly predictors. Following that, stratified random sampling was used to derive and validate a logistic regression model. The sample was stratified into two strata according to the presence (n=102) or absence (n=493) of LN-prRLN metastasis. Within a stratum, each sample was numbered with a label by a random number generator. A list of samples was then established with the number labels placed in an ascending order. The preceding 80% of the samples were used to derive a predictive model and the remaining 20% were used for its validation. The comparability between two sets of data was analyzed by 2-tailed χ2 test for categorical variables or Mann-Whitney U test for continuous variables. The variables that showed statistical association (p<0.05) with LN-prRLN metastases in univariate analysis were selected in backward stepwise logistic regression analysis to identify independent predictors (p<0.05) associated with LN-prRLN metastasis. The discriminative power of the predictive model was assessed by area under the receiver operating characteristic curves in both derivation and validation sets. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive likelihood ratio (LR+) were calculated for each cutoff point of the total score. All the analyses were performed using SPSS package (Version 20.0, IBM SPSS Statistics; IBM Corporation, Armonk, NY, USA), and a 2-tailed p-value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
In this group of patients with either right thyroid lobe PTC or bilateral PTC, the metastatic rate of the LN-prRLN was 17.14% (102/595). Among those who had LN-prRLN metastasis, 24.8% were males and the median age was 39.5 years old (interquartile range of 25.25). The median primary tumor size of LN-prRLN positive patients was 1.2 cm, which was twice that of LN-prRLN negative patients. Those with four or more foci of PTC in the thyroid had a 54.55% chance of harboring LN-prRLN metastases, which was much higher than patients with less than four thyroid cancer foci. The LN-prRLN metastasis rate of patients with capsular invasion of the primary tumor was higher than those without (33.09% vs 12.28%). LN-prRLN metastasis rate of patients with right lateral LNM was higher than those without (52.63% vs 10.40%). A univariate analysis of data from the 595 PTC patients indicated a significant association (p<0.05) between LN-prRLN metastasis and sex, age, size and number of right thyroid lobe tumor focus/foci, the presence of capsular invasion, and metastatic lymph node in the right cervical lateral compartment.
Prediction model
On comparing the derivation and validations sets, no significant difference between age, sex, tumor size, capsular invasion, the number of the primary lesions, and right lateral LNM was found between the two groups (p>0.05) (Table 2). On univariate analyses of the derivation set, patients’ sex, age, tumor size, capsular invasion, and right lateral LNM were found to be associated with LN-prRLN metastasis, whereas multifocality was not. On further logistic regression analysis, age (odds ratio [OR] 0.971, 95% CI, 0.949–0.994, p=0.013), tumor size (OR 2.163, 95% CI, 1.431–3.270, p<0.001), capsular invasion (OR 1.934, 95% CI, 1.062–3.522, p=0.031), and right lateral LNM (OR 3.786, 95% CI, 2.012–7.123, p<0.001) remained statistically significant but not patients’ sex (p=0.094) (Table 3). Using the coefficients obtained from the multivariate analysis, we derived the following prediction equation for LN-prRLN metastasis where the categorical variables were coded as “1” if present and “0” if absent:
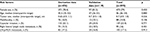  | Table 2 Risk factors of LN-prRLN metastasis in the derivation and validation data sets Abbreviation: LN-prRLN, lymph node posterior to the right recurrent laryngeal nerve. |
Y=−0.029×age+0.771×tumor size+0.660×capsular invasion+1.331×right lateral lymph node metastasis−1.687, where Y means the chance of a positive LN-prRLN metastasis.
In the derivation set, the logistic regression model yielded a receiver operating characteristic (ROC) curve with an area under the curve (AUC) of 0.790 (95% CI, 0.731–0.849) (Figure 1A). We selected 0.16 as the optimal cutoff point, which meant that the patients with a predictive rate higher than 0.16 were prone to have LN-prRLN metastases. The sensitivity, specificity, PPV, NPV, and LR+ were 71.95%, 78.68%, 41.26%, 93.09%, and 3.37 respectively. The Hosmer-Lemeshow test was significant (p=0.680), indicating a good fit of the model. In the validation set, the model showed good predictability of LN-prRLN metastasis (AUC 0.878, 95% CI, 0.789–0.967) (Figure 1B). At the cutoff point of 0.16, the sensitivity, specificity, PPV, NPV, and LR+ were 85.00%, 78.79%, 44.74%, 96.30%, and 4.00, respectively.
Discussion
At present, LN-prRLN dissection is controversial. Some surgeons advocate against routine LN-prRLN dissection because of the supposedly insignificant LN-prRLN metastasis rate, more technically demanding dissection, and thus a higher complication rate. However, in our study, we found that the metastatic rate of the LN-prRLN was 17.14% (102/595), which is not insignificant. While the dissection of LN-prRLN subzone is not straightforward, the complication rate is not higher for experienced thyroid surgeons. On the contrary, if LN-prRLN dissection is not done, 17.14% of the cases would have untreated residual disease according to our data. Future relapse from these foci would be a big problem as revision surgery in the scarred area would be very difficult and bring huge risk to the RLN, parathyroid gland and its blood supply. Therefore, an accurate assessment of the LN-prRLN metastases, providing evidence for precise and adequate treatment before the primary surgery, is very necessary. Unfortunately, it is not easy to preoperatively assess the cervical lymph node status in this area. Generally, ultrasonography is a very effective evaluation method for cervical LNM; however, its application is very limited in some central special anatomical regions. For instance, the sensitivity of central LNM using B ultrasonography is 27.5%,15 and even more difficult in the diagnosis of LN-prRLN. Thin-cut computed tomography scan can help to supplement the assessment of lymph node status, but it is not routinely recommended for patients with PTC examination.15,16 Therefore, it is clinically important to assess whether there is LN-prRLN metastasis according to the clinicopathological features of PTC patients.
This study demonstrated a significant association between LN-prRLN metastasis and the clinicopathological characteristics of PTC, such as sex, age, tumor size and number, capsular invasion, and right lateral LNM. Though the proportion of men with PTC was much less than women with a male to female ratio of 1:4 (Table 1), the probability of male patients with LN-prRLN metastasis (24.80%) was significantly higher than female patients (15.11%) (p<0.05) according to the univariate analysis (Table 1). The coefficient for age in the LN-prRLN metastasis predictive model was −0.029, indicating extra change in log (OR) for LN-prRLN metastasis as −0.029 per unit increment in age to baseline. In other words, younger patients were prone to have LN-prRLN metastasis. Similar findings of male sex and younger age as risk factors for LN-prRLN metastasis were also reported in the literature.17,18 Another study suggested that adolescents are more likely to develop neck LNM.19
In our early work, we found that the larger a tumor was, the higher the metastatic rate would be. In patients with a tumor diameter ≤0.5 cm, lymph node dissection is not necessary because the LNM rate of this group should be very low. Based on the ROC curve analysis, a tumor size >0.85 cm has a reasonable sensitivity of 78.43% and specificity of 72.40% in predicting LN-prRLN metastasis.14 In the current study, the tumor diameter, analyzed as continuous variable in order to be more consistent with clinical practice, was positively correlated with the LN-prRLN metastasis (OR 2.163, 95% CI, 1.431–3.270, p<0.001). Similarly, it was documented that tumor size larger than 1 cm is significantly correlated with LN-prRLN metastasis.10,13
At the same time, the present results indicated that multifocality was a risk factor in LN-prRLN metastasis in univariate analysis but not in multivariate analysis. Similarly, Chang et al reported that multifocality was more common in the LN-prRLN positive group than in the LN-prRLN negative group (52.7% vs 38.3%) , though it was not an independent factor.20 Nevertheless, on subgroup analysis of our data, patients with four or more tumor foci in the thyroid had a 54% chance of LN-prRLN metastasis (Table 1). This finding suggests that the multifocality is also a useful indicator for LN-prRLN metastasis in patients with four or more tumors or diffuse lesions.
Univariate analyses and multivariate analyses showed a strong correlation between capsular invasion and LN-prRLN metastasis. We thus suggest that attention should be paid to the PTC patients with capsular invasion, which can be adequately assessed by preoperative B ultrasound examination.
In this study, 52.63% patients with metastatic lymph nodes in the right cervical lateral compartment harbored LN-prRLN metastasis, compared to 10.40% of those patients without. The difference was highly significant (p<0.001). Therefore, we recommend that the metastatic lymph node in the right cervical lateral compartment be an indicator for LN-prRLN dissection. Our finding is consistent with another study that showed similar findings.20
To our knowledge, this is the first prediction model for LN-prRLN metastasis in patients with PTC, in which multiple variables were systematically considered to estimate an individual risk of LN-prRLN metastasis. In our analysis, the OR of right lateral LNM was 3.786, suggesting that it played a major role in the model. This is consistent with the pattern of PTC LNM. Generally, central lymph node is the first station for lymphatic metastasis and followed by lateral lymph node. Therefore, preoperatively confirmed right lateral LNM indicates the necessity of a careful and thorough cervical central dissection including the area posterior to the right RLN, which is also supported by clinical practice. The second and third important risk factors were capsular invasion and tumor size with the OR of 2.163 and 1.934, respectively. The weight of the age in the equation is the lowest, indicating that among 4 significant factors, it has the least predictive value. The AUC of derivation and validation sets were 0.790 and 0.878, respectively, indicating a good discriminative power of the model.
Conclusion
Age, tumor size, capsular invasion, and right lateral LNM have been identified as independent risk factors of LN-prRLN metastasis. Based on the data, we propose a mathematical model to quantitatively predict LN-prRLN metastasis, with the aim to better guide the surgical treatment of PTC. These high-risk factors or features can be preoperatively assessed by ultrasonography, imaging exams, and fine needle aspiration cytology. Given the strong association between right lateral LNM and LN-prRLN metastasis in the model, a thorough inspection of the lateral compartment is recommended in PTC patients with risk factors. We recommend multicenter studies with long-term follow-ups to ascertain the optimal surgical approach for patients with PTC.
Acknowledgments
The authors are grateful to all members of the Department of Surgical Oncology at Hangzhou First People’s Hospital for assistance with surgical treatment of PTC and clinical data collection. This study was supported by the Major Scientific and Technological Innovation Program of Hangzhou (20131813A08).
Disclosure
The authors report no conflicts of interest in this work.
References
Shindo M, Wu JC, Park EE, Tanzella F. The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg. 2006;132(6):650–654. | ||
Roh JL, Kim JM, Park CI. Central lymph node metastasis of unilateral papillary thyroid carcinoma: patterns and factors predictive of nodal metastasis, morbidity, and recurrence. Ann Surg Oncol. 2011;18(8):2245–2250. | ||
Yun JS, Lee YS, Jung JJ, Nam KH, Chung WY, Park CS. Central neck recurrence patterns and morbidity following reoperation for recurrent papillary thyroid carcinoma. J Korean Surg Soc. 2008;74(1):42–47. | ||
Baek SK, Jung KY, Kang SM, et al. Clinical risk factors associated with cervical lymph node recurrence in papillary thyroid carcinoma. Thyroid. 2010;20(2):147–152. | ||
Kim SY, Kim BW, Ju YP, Hong SW, Chang HS, Park CS. Macrometastasis in papillary thyroid cancer patients is associated with higher recurrence in lateral neck nodes. World J Surgery. 2017;42(1):123–129. | ||
Podnos YD, Smith D, Wagman LD, Ellenhorn JD. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg. 2005;71(9):731–734. | ||
Peng Y, Ding J, Zhang W, Pan G, Ding Z, Luo D. [Research progress of the lymph node dissection posterior to fight recurrent laryngeal nerve of papillary thyroid carcinoma]. Zhonghua Wai Ke Za Zhi. 2015;53(3):233–236. Chinese [with English abstract]. | ||
Lee BJ, Lee JC, Wang SG, Kim YK, Kim IJ, Son SM. Metastasis of right upper para-esophageal lymph nodes in central compartment lymph node dissection of papillary thyroid cancer. World J Surg. 2009;33(10):2094–2098. | ||
Ito Y, Fukushima M, Higashiyama T, et al. Incidence and predictors of right paraesophageal lymph node metastasis of N0 papillary thyroid carcinoma located in the right lobe. Endocr J. 2013;60(3):389–392. | ||
Pinyi Z, Bin Z, Jianlong B, Yao L, Weifeng Z. Risk factors and clinical indication of metastasis to lymph nodes posterior to right recurrent laryngeal nerve in papillary thyroid carcinoma: a single-center study in China. Head Neck. 2014;36(9):1335–1342. | ||
Zhang DG, Gao L, Miao YW, He GF, Xie L. Risk factors for posterior to right recurrent laryngeal nerve lymph node metastasis in papillary thyroid carcinoma. Saudi Med J. 2014;35(8):832–837. | ||
Kim YS, Park WC. Clinical predictors of right upper paraesophageal lymph node metastasis from papillary thyroid carcinoma. World J Surg Oncol. 2012;10:164. | ||
Bae SY, Yang JH, Choi MY, Choe JH, Kim JH, Kim JS. Right paraesophageal lymph node dissection in papillary thyroid carcinoma. Ann Surg Oncol. 2012;19(3):996–1000. | ||
Luo DC, Xu XC, Ding JW, et al. Clinical value and indication for the dissection of lymph nodes posterior to the right recurrent laryngeal nerve in papillary thyroid carcinoma. Oncotarget. 2017;8(45):79897–79905. | ||
Kim SK, Woo JW, Park I, et al. Computed tomography-detected central lymph node metastasis in ultrasonography node-negative papillary thyroid carcinoma: is it really significant? Ann Surg Oncol. 2017;24(2):442–449. | ||
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. | ||
Tao Y, Wang C, Li L, et al. Clinicopathological features for predicting central and lateral lymph node metastasis in papillary thyroid microcarcinoma: analysis of 66 cases that underwent central and lateral lymph node dissection. Mol Clin Oncol. 2017;6(1):49–55. | ||
Zhao C, Jiang W, Gao Y, Niu W, Zhang X, Xin L. Risk factors for lymph node metastasis (LNM) in patients with papillary thyroid microcarcinoma (PTMC): role of preoperative ultrasound. J Int Med Res. 2017;45(3):1221–1230. | ||
Lu ZZ, Zhang Y, Wei SF, et al. Outcome of papillary thyroid microcarcinoma: study of 1,990 cases. Mol Clin Oncol. 2015;3(3):672–676. | ||
Chang H, Yoo RN, Kim SM, et al. The clinical significance of the right para-oesophageal lymph nodes in papillary thyroid cancer. Yonsei Med J. 2015;56(6):1632–1637. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.