Back to Journals » Journal of Blood Medicine » Volume 14
Military Blood Service in Poland
Authors Kryczka T , Jedynak A, Olszewski A, Sierpinska L, Kuzniarska P, Sulejczak D
Received 15 October 2022
Accepted for publication 25 February 2023
Published 17 April 2023 Volume 2023:14 Pages 309—316
DOI https://doi.org/10.2147/JBM.S390673
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Tomasz Kryczka,1,* Anna Jedynak,2,3,* Adam Olszewski,3,4 Lidia Sierpinska,5 Paula Kuzniarska,6 Dorota Sulejczak7
1Department of Development of Nursing and Social & Medical Sciences, Medical University of Warsaw, Warsaw, Poland; 2Department of Military Medical Service, Ministry of National Defence of Poland, Warsaw, Poland; 3Military Center of Blood Donation and Haemotherapy, Warsaw, Poland; 4Garrison Medical Outpatient Clinic, Modlin, Poland; 5Independent Public Health Care Unit, Military Teaching Hospital with Polyclinic, Lublin, Poland; 6Military Center of Blood Donation and Haemotherapy, Gdansk, Poland; 7Department of Experimental Pharmacology, Mossakowski Medical Research Institute, Polish Academy of Sciences, Warsaw, Poland
*These authors contributed equally to this work
Correspondence: Tomasz Kryczka, Medical University of Warsaw, Department of Development of Nursing and Social & Medical Sciences, ul. Ciołka 27, Warsaw, 01-445, Poland, Tel +48 604315103, Email [email protected]
Introduction: On 24 February 2022, the Russia–Ukraine military conflict unfolded just across the eastern border of the European Union. It made everyone realize how important it is to secure blood supplies to health-care units in the event of an armed conflict. This paper presents the principles of functioning of the Military Blood Donation Service and the Military Center for Blood Donation and Hemotherapy in Poland.
Methods: The study used data collected in the “Military Blood Bank” information processing system and data from annual reports (2010– 2021) sent to the Minister of Health of the Republic of Poland. The reports concerned, among others: demographic data on donors, reasons of permanent disqualifications, numbers of complete and incomplete donations, etc.
Results: Since 2005, the number of donors registered in military blood donation centers ranged between 15 and 35 thousand/year. The most dramatic declines in donors were observed in 2010 and 2020. Successful donations accounted for more than 98% of all donations/year (except 2015), and their number varied between 20 and 32 thousand/year. Among the blood donors, men always predominated and the dominant age group (except for 2010) was 25– 44 years. The reasons for permanent disqualification have varied over time: their proportions decreased for viral hepatitis and cardiovascular disease, and increased for respiratory and endocrine/metabolic diseases. Due to the COVID-19 pandemic in 2020/2021, these proportions have sometimes been reversed.
Discussion: The Military Blood Donation Service has been functioning in Poland for several decades. It is specialized in supplying blood and blood products to the Armed Forces. Unfortunately, it was not possible to refer to the functioning of similar institutions in other countries. Therefore, when evaluating the functioning of Polish military blood donation, we had to rely on numerical values (eg, number of donors/year, donor profile, etc.), which prove a very good organization of blood donation centers. However, it should be noted that, as in other countries, a more active promotion of blood donation in the media is advisable in order to encourage as many young people as possible to donate blood.
Keywords: blood donors, blood donation, military blood donation
Introduction
On 24 February 2022, the Russia–Ukraine military conflict unfolded just across the eastern border of the European Union, in the immediate vicinity of Poland, which borders both countries. According to media reports, this war has shaken the sense of security of most countries in the region and prompted them to review their defences and prepare for an escalation of the conflict, also in the medical context.
Considering the latter issue, a continuous supply of blood and blood products to medical institutions is one of the key elements of health care functioning in times of peace and war. In the European Union (EU) countries, the basic standards and guidelines for blood donation are included in relevant directives and regulations (eg, “Blood Guide” regularly updated by the European Committee for Blood Transfusion).1 In Poland, these regulations are based on the national law and recommendations of authorised institutions, which, however, cannot be incompatible with EU regulations.2–4 Poland and the majority of EU countries also belong to the North Atlantic Treaty Organisation (NATO), which obliges them to implement regulations ensuring the fulfilment of the alliance commitments, among others, in the aspect of blood donation and military blood supply for the time of “peace” (NATO Medical Doctrine).5 Key documents (regulations and guidelines) for the time of “war” are created in a confidential mode, eg, at meetings of the Committee of Chiefs of Military Medical Services in NATO (COMEDS).6 Additionally, meetings of experts from NATO member countries in the field of military transfusiology (Military Blood Advisory Team, MBAT) are held twice a year. The MBAT is an advisory body to the NATO Military Health Care Working Group (MHCWG) subordinated to the NATO Steering Committee and COMEDS. COMEDS and its agencies initiate and disseminate common foundations, principles, doctrines, concepts, procedures, programmes and techniques for medical security for NATO member countries. The MHCWG is responsible for the standardisation of procedures for medical supplies in the event of emergencies and peacetime in the aspect of military medicine with the highest possible quality of service and safety.6
In Poland, the Military Blood Donation (MBD), which functions similarly to civilian blood donation and haemotherapy units (based on WHO and EU guidelines and recommendations) on an everyday basis, has been operating for several decades. At the same time, MBD is specialized in supplying blood and blood products to the Armed Forces based on NATO regulations,5,6 like no other civilian institution in the country. Additionally, the Military Centre for Blood Donation and Haemotherapy (MCBDH), whose “flagship” unit is the Independent Public Health Care Institution based in Warsaw, has been operating in Poland since 2005. It consists of seven Field Stations (in larger cities) and the Medical Team in Warsaw.7 In addition to controlling and supervising blood treatment in medical entities of the Ministry of National Defence and giving opinions on legal acts in the field of blood donation and haemotherapy in Poland, MCBDH cooperates with national and international organizations, including partners from NATO member states, performing a number of functions specified in NATO regulations for the times of peace.8 However, the main task of MCBDH in times of peace or war is to ensure that military and civilian health-care institutions in Poland are provided with blood and blood products.
The aim of this study is to characterize candidates for blood donors reporting to the MCBDH and the reasons for their permanent disqualification since the inception of this unit in Poland.
Materials and Methods
The study used data collected in the “Military Blood Bank” information processing system and data from annual reports sent to the Minister of Health of the Republic of Poland (through the National Blood Centre in Warsaw) from 2010 to 2021. The annual reports concerned the activities of MCBDH, including field branches, mobile teams, personnel, hospitals, serological laboratories, and contained data on donors (number of potential donors available in the system, who can donate blood or its components, number of registered donors in mobile blood collection points, number of donors who donated blood/its components in a given year) by age and sex, number of permanent disqualifications.2,3 The reports also included information on the number of complete and incomplete donations (450 mL and 250 mL, respectively), blood components, the total number of donations, an updated list of hospital blood banks supplied, the total number of unused donations, the number of all components manufactured and distributed to health-care units, the occurrence and prevalence of infectious disease markers in blood donors, the number of products withdrawn, as well as the number of documented serious adverse events and reactions.
The collected data were analysed for the demographic profile of donors, number of donations classified as full and incomplete and reasons for disqualification of donors in the subsequent years of service of the military blood donation in Poland. The data accessed complied with relevant data protection and privacy regulations.
The Ethical Committee of Medical University of Warsaw approved this study (Statement No AKBE/171/2019).
Results
The first 5 years of MCBDH activity were characterized by a relatively high public interest in blood donation, with the number of donors between 27 and 35 thousand people per year (data not shown), while after a temporary sharp decline in donations in 2010–2011, the number of donors stabilized at around 21–23 thousand per year in the following years (Table 1). In 2020 and 2021, the number of donors significantly decreased below 20,000 per year, as did the number of donations (below 30,000 per year), with the most dramatic drop observed in 2020 (Table 1). Similarly, there was a dramatic fall in first-time donors to 6645 in 2020, whereas in previous years between 8000 and almost 12,000 new donors were registered (Table 1). In 2010, only 6665 repeated donors were registered, and their number increased each year to 14,731 in 2016; currently, the number of repeated donors is in the range of 10–12 thousand people per year (Table 1). Successful donations (so-called “full donations”) accounted for more than 98% of all donations over the analyzed time period (except in 2015, when the percentage of “failures” was about 3.5%; Table 1), and their number increased from 20,793 in 2010 to more than 31,000 in 2019, before dropping to 25,000–29,000/year in the next 2 years (Table 1).
 |
Table 1 Donations Registered at MCBDH in the Years 2010–2021 |
Men predominated among blood donors throughout the history of MCBDH – there were always 2–3 times more men than women, with almost 4 times more men donating blood than women in 2020 and 2021 (Table 2). Men aged 18–24 years constituted the majority of donors only in 2010. In subsequent years, men aged 25–44 years were the predominant group. The percentage of men donating blood aged 25–44 years increased over the years from 18.6% in 2010 to 54.4% in 2021, similarly to women – from 6% to 12.5%. At the same time, the number of young blood donors aged 18–24 years decreased significantly from 45.3% to 13.3% (men) and 19% to 5.25% (women); see Table 2. Young people and people aged ≥65 years accounted for less than 1% of donors over the observed time period.
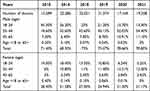 |
Table 2 Age Characteristics of Blood Donors in Selected Years |
Table 3 shows the main reasons for disqualification recorded at blood donation centers. Attention is drawn to the significant decrease in the number of disqualifications from 329–500 in 2005–2008 to 85–111 in 2019–2021. The data collected show an increase in disqualifications due to respiratory diseases from 1.52% in 2005 (10.91% in 2010) to a maximum of 29.68% in 2014, followed by a decrease to values of a few percent in subsequent years and 4.5% in 2021 (Table 3). Even more dramatic decreases were observed for viral hepatitis, from 15.20% in 2005 to values of a few percent between 2013 and 2021 (no disqualification due to viral hepatitis was registered in 2019, Table 3). Similarly, a reduction in the number of disqualifications, eg, due to cardiovascular diseases, was recorded from 8.21% in 2005 to 1.80% in 2019, although the last 2 years have seen a significant increase in disqualifications for this reason (5.88% and 9.91% of potential donors, respectively, Table 3).
 |
Table 3 Causes of Permanent Disqualification Among Blood Donors |
As for the increases in disqualifications, those related to endocrine function and metabolic diseases are noteworthy: from 3.04% in 2005 to 19.87%–37.16% between 2016 and 2018, followed by a moderate decrease in these disqualifications in subsequent years (Table 3). Even more significant are disqualifications for so-called “other reasons” (see legend Table 3), from 63.22% in 2005 to 20.95% in 2018, with an increase in the percentage of this category among potential donors in recent years – up to the value recorded 15 years ago (Table 3).
Due to the significant registration of disqualifications for “other reasons than systemic diseases” indicated in Table 3, data on disqualifications due to (i) cardiovascular-, (ii) pulmonary-, (iii) dermatology-, (iv) infectious liver- and (v) metabolic/endocrine diseases were reanalysed, comparing only these 5 reasons of disqualification. Among these 5 reasons for disqualification, cardiovascular diseases accounted for 22.32% in 2005 and less than 10% between 2014 and 2019 (Table 3). However, there was a significant increase in these disqualifications to 26.19% in 2021. In contrast, the most significant decrease in disqualifications was observed for viral hepatitis, from 41.33% to a few percent between 2016 and 2021. For pulmonary diseases, an increase in disqualifications was observed from 4.13% in 2005 to values 5–10 times higher between 2010 and 2020, and an equally high increase in disqualifications due to metabolic and endocrine diseases (Table 3). For skin diseases, the percentage of disqualifications for this reason was variable in both sets (with and without “other”) over the study period (Table 3).
Discussion
The Military Blood Donation has been functioning in Poland for several decades now. The MCBDH also belongs to the MBD as a relatively new organisational unit, which constitutes a significant supplement to the national blood donation and haemotherapy system.8 Maintaining a constant number of donations at the level of several dozen thousand/year for over 15 years is an indicator of the proper functioning of the military blood donation system (see Table 1). This is a significant observation as in some European countries, eg, Germany, the Netherlands or Switzerland, the number of blood donations is decreasing year by year.9–11 According to Chandler et al, this is related to the takeover of part of the donation market in these countries by private organizations or foundations.12 In the case of Poland, such a sharp decline in the number of donors was observed in 2020 and 2021, ie, when the threat of the COVID 19 pandemic was widely announced. The imposed restrictions strongly discouraged visits to medical facilities worldwide by healthy people who feared infection with the SARS-COV2 virus.13 In Poland, the number of first-time donors dropped at that time (Table 1), ie, those who did not have direct, practical knowledge about the donation procedure itself and were discouraged to visit the medical institution due to the risk of virus infection.
In our reports conducted since 2005, we observed a decrease in the number of donors aged 18–24 years in favour of an older group (25–44 years, Table 2). This may have resulted from insufficient knowledge of blood donation among young people, especially considering the fact that some authors indicate insufficient promotion of blood donation in the media, eg, social media.14–17 Fear of seeing own blood, fear of the procedure itself and negative experiences from previous, first-time blood donation or lack of appropriate “incentives”, eg, financial, may be an additional barrier for young people.17–25 Interestingly, women, who are more altruistic than men and more motivated to donate blood,19 accounted for only 1/4-1/3 of all donors in our analysis (Table 3). On the other hand, a similar proportion of female blood donors was also observed in other countries.12,26,27 According to Bilal et al, women are more likely to drop out of blood donation when they have limited access to a donation point (distance) or lack encouragement from supervisors at workplaces.28 An additional limitation is the medical regulation that a woman can only donate blood 4 times a year.2,3
With regard to the functioning of the MCBDH, it is noteworthy that the proportion of repeated donors over first-time donors has been increasing over time, and since 2014, repeated donors have outnumbered first-time donors (Table 1). On the one hand, this observation has positive connotations, implying that the medical organization and the atmosphere at the donation centre have made a positive impression on first-time donors, which, according to Alfieri et al, is important for attempting another donation.19 On the other hand, it may indicate a moderate or low interest in blood donation, especially among young people, which requires specific actions to promote this activity, as previously indicated, eg, in social media.14–17
In the course of MCBDH activity until 2021, 494,810 blood donations were collected from 420,086 donors, with a total number of disqualifications of 3862 people (data not shown). In the early years after establishing MCBDH, the annual number of disqualifications reached 329–500 donors, and the vast majority of these were defined for reasons “other” than diseases of the skin, respiratory-, circulatory-, metabolic/endocrine systems and viral hepatitis (see Table 3, columns “A-E”). By 2018, there was a decline in such “other” disqualifications to a record low of 20.95% in 2018, but in subsequent years it was 44–62% (Table 3). Disqualifications for “other reasons”, in a range that is very broad in terms of medical interpretation (see legend of Table 3), dropped by 2018 in favour of, for example, pulmonary diseases. It should be presumed that increasing environmental and especially air pollution has led to an increase in the incidence of lung diseases in recent years,29 which may have gone undiagnosed due to insufficient availability of prevention and treatment of these conditions in Poland.30 Therefore, it should be assumed that it was only during the qualification for blood donation that candidates for donors found out about their disease, hence the multiple increase in disqualifications for this reason comparing successive years of MCBDH activity (Table 3).
Surprisingly, there was a decrease in the number of disqualifications due to cardiovascular diseases, more noticeable compared to the main reasons for disqualification (Table 3, “A-E”), in the context of persistently high incidence and death rates due to these diseases.31,32 It is possible that awareness of one’s own cardiovascular health problems or treatment used33 significantly influence these patients’ decisions to donate blood, hence the decrease in such disqualifications (Table 3). What is equally positively surprising is the decrease in disqualifications of donors due to viral hepatitis (Table 3). At the beginning of the MCBDH activity, hepatitis B or C virus infections were the most common reasons for disqualification (apart from “other reasons”). Currently, in percentage terms, the values are in single digits (Table 3). The above may be a result of very intensive information and prophylactic campaigns conducted in Poland aimed at this group of diseases over many years, in which emphasis was placed on prevention of infections, in particular through vaccination and educational activities. As a result, there is a noticeable decrease in the incidence of viral hepatitis in Poland,34,35 and thus also the likelihood of a patient with undiagnosed hepatotropic virus infection reporting to a blood donation center.
The most significant increase in disqualifications in the observed period of time was reported for metabolic or endocrine diseases, ie, from single to double digit values (Table 3). Among the above diseases, diabetes mellitus came first, as a growing health problem in Poland, but also obesity, and thyroid dysfunction, etc.36 The above is mainly related to changes in nutrition and lifestyle of Poles, which has already been discussed on scientific forums many times. This is not only a problem of Poland, but of the vast majority of industrialized countries, where a sedentary lifestyle and reduced physical activity result in metabolic and endocrine problems of varying severity.37
A certain limitation of the analysis presented in this paper is the fact that most disqualifications recorded at donation points are only in a small part based on the results of laboratory tests – eg, tests for the presence of hepatotropic viruses, HIV, etc. The vast majority of such decisions are based on a questionnaire completed by a potential donor at the initial stage of qualification for donation. Interview with the MD, during which, on the basis of subjective or physical symptoms, the doctor makes an independent decision on permanent or temporary disqualification, is another “screening” stage. During the interview, the doctor is not required to make a diagnosis of the potential donor’s disease due to the limited availability of diagnostic tools, and therefore indicates in general terms the reasons for disqualification in the final report. Due to the prevalence of individual disqualification reasons, we have considered a few as the main ones (see “A-E”, Table 3), and have referred to the remaining disqualification reasons beyond those indicated above as “other reasons”.
The second limitation to this analysis, in which we attempted to reliably assess the functioning of the MCBDH since its inception, was the outbreak of the COVID19 pandemic. At that time, some potential donors declined to donate blood precisely because of the threat associated with the SARS-COV2 virus, which was noticeable in terms of the number of first-time donors. In addition, in the last 2 years, a more self-critical approach to their own health was observed among donors in terms of medical symptoms, such as persistent cough, which may indicate infection with this virus.38 This is likely to be the reason for the sharp decline in disqualifications due to pulmonary diseases in 2021 (Table 3).
The third limitation of this work was the inability to compare the activities of MCBDH in Poland with analogous institutions in other countries due to the lack of literature reports on the subject and the lack of access to data, which, due to the military nature of the units, were not available for us to review. Most of the available publications and reports refer to the functioning of military blood donation, eg, in places of warfare or in the immediate resource base (hospital units, frontline units), possibly in hospitals where military veterans reside. Therefore, our report should be treated as unique on the global scale, in which we indicate the state of functioning of military blood donation in Poland during the period of “peace”, without violating military secrecy concerning actions in the times of “war”.
Conclusions
Considering the current military threats appearing near the eastern border of Poland (conflict between Russia and Ukraine), it should be stated on the basis of the presented analysis, without the possibility of referring to similar institutions in other countries, that the organization and functioning of military blood donation and blood therapy in Poland is excellent, as evidenced by the relatively stable number of donors over the past years despite the changing profile of the donors themselves. However, it should be noted that, as in other countries, a more active promotion of blood donation in the media is advisable in order to encourage as many young people as possible to donate blood.
Abbreviations
MBAT, Military Blood Advisory Team; MHCWG, Military Health Care Working Group; COMEDS, Committee of Chiefs of Military Medical Services in NATO; MBD, Military Blood Donation; MCBDH, Military Centre for Blood Donation and Haemotherapy.
Disclosure
The authors have no relevant or potential conflicts of interest in this work.
References
1. European Directorate for the Quality of Medicines & HealthCare (EDQM). Council of Europe. Guide to the Preparation, Use and Quality Assurance of Blood Components. Recommendation No. R (95) 15; 2020. Available from: www.edqm.eu.
2. State Minister of Health of Republic of Poland. Announcement on the requirements of good practice for: collecting blood and its components, testing, preparation, storage, issuing and transport for organizational units of the public blood service. Official Journal of the Minister of Health 2021, No. 28. Available from: https://dziennikustaw.gov.pl/.
3. State Minister of Health of Republic of Poland. Regulation on the conditions for collecting blood from candidates for blood donors and blood donors. Journal of Laws 2017. No 1741. Available from: https://dziennikustaw.gov.pl/.
4. Parliament of Republic of Poland. Act on the public blood service; with later changes. Journal of Laws 2021. No 1749. Available from: https://dziennikustaw.gov.pl/.
5. North Atlantic Treaty Organization. NATO Standardizations Office (NSO): allied joint doctrine for medical support, C ed., version 1; 2019. Available from: https://shape.nato.int.
6. North Atlantic Treaty Organization. Recommendations of the committee of the chiefs of military medical services in NATO; 2021. Available from: https://www.nato.int/cps/en/natohq/topics-175736.html.
7. State Minister of National Defense od Republic of Poland. Regulation on the establishment of the military center for blood donation and haemotherapy. Journal of Laws 2004. No 243, Item 2433; 2004. Available from: https://dziennikustaw.gov.pl/.
8. Jedynak A, Klamrowski P, Olszewski A, Koper D, Sienkiewicz Z, Kryczka T. Krwiodawstwo i Krwiolecznictwo wojskowe w Polsce [Blood donation and military blood haemotherapy in Poland]. Surg Vasc Nurs. 2020;42:64–69. Polish.
9. Volken T, Buser A, Castelli D, et al. Red blood cell use in Switzerland: trends and demographic challenges. Blood Transfus. 2018;16(1):73–82. doi:10.2450/2016.0079-16
10. Müller-Steinhardt M, Weidmann C, Klüter H. Changes in the whole blood donor population in South-West Germany: 2010 versus 2016. Transfus Med Hemother. 2017;44(4):217–223. doi:10.1159/000479192
11. Borkent-Raven BA, Janssen MP, Van Der Poel CL. Demographic changes and predicting blood supply and demand in the Netherlands. Transfusion. 2010;50(11):2455–2460. doi:10.1111/j.1537-2995.2010.02716.x
12. Chandler T, Hiller J, Peine S, Stargardt T. Blood donation and donors: insights from a large German teaching hospital (2008–2017). Vox Sang. 2020;115(1):27–35. doi:10.1111/vox.12853
13. Khalilpourazari S, Hashemi Doulabi H. A flexible robust model for blood supply chain network design problem. Ann Oper Res. 2022;21:1–26.
14. Beyene GA. Voluntary blood donation knowledge, attitudes, and practices in central Ethiopia. Int J Gen Med. 2020;13:67–76. doi:10.2147/IJGM.S246138
15. Al-Hajri QR, Alfayez A, Alsalman D, et al. The impact of WhatsApp on the blood donation process in Saudi Arabia. J Blood Med. 2021;12:1003–1010. doi:10.2147/JBM.S339521
16. Ramondt S, Kerkhof P, Merz EM. Blood donation narratives on social media: a topic modeling study. Transfus Med Rev. 2022;36(1):58–65. doi:10.1016/j.tmrv.2021.10.001
17. Ramondt S, Zijlstra M, Kerkhof P, Merz EM. Barriers to blood donation on social media: an analysis of Facebook and twitter posts. Transfusion. 2020;60(10):2294–2306. doi:10.1111/trf.15998
18. Ugwu NI, Uneke CJ, Ugwu CN, Oti WJO, Agbo UN, Akamike IC. Effect of blood donor educational intervention on the knowledge and attitude towards voluntary blood donation among medical students at a Nigerian university. Niger Med J. 2020;61(3):163–168. doi:10.4103/nmj.NMJ_177_19
19. Alfieri S, Guiddi P, Marta E, Saturni V. Economic crisis and blood donation: how are donors motivations changing? Transfus Apher Sci. 2016;54(3):396–400. doi:10.1016/j.transci.2016.03.001
20. Otifi HM, Asiri MA, Ahmad MT, et al. Measuring public awareness about blood donation in Assir, South-Western Saudi Arabia. Transfus Clin Biol. 2020;27(3):122–127. doi:10.1016/j.tracli.2020.06.005
21. France CR, France JL, Himawan LK, et al. Fear is associated with attrition of first-time whole blood donors: a longitudinal examination of donor confidence and attitude as potential mediators. Transfusion. 2021;61(12):3372–3380. doi:10.1111/trf.16671
22. Rael CT, Pierre D, Frye V, et al. Evaluating blood donor experiences and barriers/facilitators to blood donation in the United States using YouTube video content. Transfusion. 2021;61(9):2650–2657. doi:10.1111/trf.16568
23. Ugwu NI, Oti WJ, Ugwu CN, Uneke CJ. Voluntary non-remunerated blood donation: awareness, perception, and attitude among potential blood donors in Abakaliki, Nigeria. Niger J Clin Pract. 2019;22(11):1509–1515. doi:10.4103/njcp.njcp_159_19
24. Veerus P, Kullaste R, Pungas K, Aavik T, Lang K. How to reverse first time donors to become regular donors? A questionnaire survey in Estonia. Transfus Clin Biol. 2017;24(4):404–409. doi:10.1016/j.tracli.2017.06.010
25. Alaskar SA, Alsadhan JA, Alanazi RM, et al. Voluntary blood donation among female health care university students in Saudi Arabia, knowledge and status. J Family Med Prim Care. 2021;10(6):2353–2357. doi:10.4103/jfmpc.jfmpc_2182_20
26. Bhuiyea MSH, Faiyaz SR, Jaman N, Uddin MJ. Factors influencing voluntary blood donation practice among university students of Bangladesh. Transfus Apher Sci. 2022;61(4):103379. doi:10.1016/j.transci.2022.103379
27. Saleh RA, Khalil H, Alsaleh M, et al. Voluntary and non-voluntary blood donations among doctors. Health Sci Rep. 2021;4(4):e377. doi:10.1002/hsr2.377
28. Bilal M, Haseeb A, Zahid I, et al. Knowledge, attitudes and perceptions among non blood donor female health care professionals. Glob J Health Sci. 2015;8(4):203–211. doi:10.5539/gjhs.v8n4p203
29. Nazar W, Niedoszytko M. Air pollution in Poland: a 2022 narrative review with focus on respiratory diseases. Int J Environ Res Public Health. 2022;19(2):895. doi:10.3390/ijerph19020895
30. Supreme Chamber of Control of Republic of Poland. Availability of prevention and treatment of respiratory diseases; 2016. Available from: https://www.nik.gov.pl/plik/id,11909,vp,14281.pdf.
31. Czerwinska K, Gac P, Poreba R, Mazur G, Pawlas K. Cardiac and vascular disorders as para-occupational diseases - a Polish perspective. Ann Agric Environ Med. 2021;28(2):231–236. doi:10.26444/aaem/122259
32. Main Statistical Office of Republic of Poland. Incidence and mortality from cardiovascular diseases and the demographic situation; 2022. Available from: https://stat.gov.pl/files/gfx/portalinformacyjny/pl/defaultaktualnosci/5468/22/1/1/statystyka_umieralnosci_w_wyniku_chuk.pdf.
33. Jankowski P, Banach M, Malyszko J, et al. May measurement month 2018: an analysis of blood pressure screening campaign results from Poland. Eur Heart J Suppl. 2020;22(SupplH):H108–H111. doi:10.1093/eurheartj/suaa041
34. Stawinska-Witoszynska B, Klos J, Moryson W, Wieckowska B. Trends in the incidence of acute hepatitis B in the Polish population and their determinants. Medicina. 2021;57(8):738. doi:10.3390/medicina57080738
35. Wojtczak A. Review of „the project KIK/35„ prevention of Hepatitis C Virus (HCV) infections” as an example of integrated public health interventions to reduce blood-borne infections in Poland. Przegl Epidemiol. 2017;71(3):283–285.
36. Placzkiewicz-Jankowska E, Czupryniak L, Gajos G, et al. Management of obesity in the times of climate change and COVID-19: an interdisciplinary expert consensus report. Pol Arch Intern Med. 2022;132(3):16216. doi:10.20452/pamw.16216
37. Lipinska-Ojrzanowska A, Walusiak-Skorupa J, Ojrzanowski M, Marcinkiewicz A, Plewka M, Wiszniewska M. Evaluation of selected risk factors for cardiovascular diseases and diabetes as a background for the prevention program in occupational healthcare. Int J Occup Med Environ Health. 2021;34(3):403–413. doi:10.13075/ijomeh.1896.01531
38. Semczuk-Kaczmarek K, Rys-Czaporowska A, Sierdzinski J, Kaczmarek LD, Szymanski FM, Platek AE. Association between air pollution and COVID-19 mortality and morbidity. Intern Emerg Med. 2022;17(2):467–473. doi:10.1007/s11739-021-02834-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
