Back to Journals » Clinical Ophthalmology » Volume 8
Meta-analysis comparing same-day versus delayed vitrectomy clinical outcomes for intravitreal retained lens fragments after age-related cataract surgery
Received 21 July 2014
Accepted for publication 19 August 2014
Published 18 November 2014 Volume 2014:8 Pages 2261—2276
DOI https://doi.org/10.2147/OPTH.S71494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Elizabeth A Vanner,1 Michael W Stewart2
1Department of Preventive Medicine, Pathology and Bioinformatics, Stony Brook University, Stony Brook, NY, USA; 2Department of Ophthalmology, Mayo Clinic College of Medicine, Jacksonville, FL, USA
Purpose/design: We aimed to perform a systematic review and meta-analysis comparing the risk difference of clinical outcomes for same-day (SD) vs delayed (DEL) pars plana vitrectomy (PPV).
Methods: We searched MEDLINE (English; January 1, 1985 to July 16, 2013) and article reference lists, for patients with crystalline retained lens fragments and discussion of SD-PPV vs DEL-PPV. For the meta-analysis, articles needed the number of patients receiving SD-PPV and DEL-PPV, and the number, in each group, who experienced one or more of the outcomes: not good visual acuity (VA) (<20/40), bad VA (≤20/200), retinal detachment, increased intraocular pressure/glaucoma, intraocular infection/inflammation, cystoid macular edema, and corneal edema.
Results: Of 304 articles identified, 23 provided data for the meta-analysis. Results were mixed, indicating 1) neither vitrectomy time produced better outcomes in all studies (not good VA risk difference =10.3% [positive numbers favored SD-PPV; negative numbers favored DEL-PPV], 95% confidence interval [CI] = [-0.4% to 21.0%], P=0.059; and bad VA risk difference =-0.3%, 95% CI = [-10.7% to 10.1%], P=0.953); 2) better outcomes with immediate SD-PPV compared with all DEL-PPV (not good VA risk difference =16.2%, 95% CI = [0.8% to 31.5%], P=0.039; and bad VA risk difference =8.5%; 95% CI = [0.8% to 16.2%], P=0.030); and 3) immediate SD-PPV and prompt DEL-PPV (3 to 14 days after cataract surgery) had no significant differences and so may produce similar outcomes (not good VA risk differences range = [-19.9% to 6.5%], 95% CI = [-59.9% to 36.4%]; and bad VA risk differences range = [-6.9% to 7.4%], 95% CI = [-33.1% to 31.8%]).
Conclusion: Perhaps SD-PPV should be limited to facilities at which a vitreoretinal surgeon is immediately available. Otherwise, these results support referring a patient with retained lens fragments promptly to a vitreoretinal surgeon but do not support interfacility transport for SD-PPV.
Keywords: retained lens fragments, vitrectomy, time factors, visual acuity, meta-analysis, systematic review
Introduction
Phacoemulsification lensectomy1 occasionally results in retained lens fragments or the entire crystalline lens dislocating into the vitreous, which increases the risk of postoperative complications and vision loss.2,3 With an estimated 10 million cataract surgeries performed per year worldwide,4 the estimated annual incidence of retained lens fragments is between 10,000–160,000 (mean =85,000). The timing of pars plana vitrectomy (PPV) to remove retained lens fragments is controversial, especially concerning whether, and under what circumstances, a “same day” (SD) (as the cataract surgery) vitrectomy (SD-PPV) might be performed. Optimal management of retained lens fragments has not been determined, but cataract surgeons have been urged to avoid attempting to retrieve retained lens fragments by manipulating the vitreous,5,6 to prevent complications such as retinal detachment,7 and to refer patients to a vitreoretinal surgeon promptly.8–13
Some vitreoretinal surgeons suggest performing an SD-PPV, as they believe this to be the optimal time to remove retained lens fragments.14,15 However, the logistics of arranging an SD-PPV can be daunting.16,17 Others feel that SD-PPV is unnecessary, complicates the informed consent process, and may increase the risk of complications.18,19 A survey of cataract surgeons indicated they believed that 58% of patients had retained lens fragments removed immediately,20 far higher than reported by vitreoretinal surgeons, who indicated only 13% (536 of 4,150) of eyes received an SD-PPV.21
Policies for performing SD-PPV differ among facilities. Lack of the necessary equipment and/or the immediate availability of an experienced vitreoretinal surgeon may preclude an SD-PPV.22 Preliminary examination of the SD-PPV results in the literature23 found that some facilities had good visual acuity (VA) results,22,24,25 while other facilities’ results were not as good26–28 (data not shown). Reasons for this dichotomy were not clear, but lower rates of increased intraocular pressure (IOP) and cystoid macular edema (CME) with SD-PPV may be related to reduced intraocular inflammation/infection.24 Several authors reported better VA and lower rates of complications (including retinal detachment, increased IOP, corneal edema, CME, and intraocular inflammation/infection) among patients who had SD-PPV compared with delayed vitrectomy (DEL-PPV), but these differences were not always statistically significant.25,29–31 Other authors reported little or no differences in these and other outcomes when comparing SD-PPV and DEL-PPV.32–34
This is our second meta-analysis about vitrectomy timing for retained lens fragments. The first, which included no SD-PPV patients, indicated that prompt DEL-PPV (3 to 7 or possibly 3 to 14 days after cataract surgery) was associated with better VA and fewer cases of previtrectomy and postvitrectomy retinal detachment, increased IOP, and intraocular inflammation/infection compared with later (nonprompt) DEL-PPV.13 As in our previous study, the primary outcomes for this meta-analysis were not good VA (<20/40) and bad VA (≤20/200). Secondary outcomes included retinal detachment, increased IOP, intraocular inflammation/infection, CME, and corneal edema. All outcome data were postvitrectomy, preferably at final examination. The aim of this research was to explore 1) differences in clinical outcomes between SD-PPV and DEL-PPV, 2) the observed heterogeneity in SD-PPV results, and 3) the effect of policy differences on SD-PPV results. Complete citations and greater detail may be found in the first author’s doctoral dissertation,21 which is available upon request. All references to our previous research are to this dissertation and the authors’ previous meta-analysis.13
Materials and methods
Search strategy
Details of the article search for the systematic review and meta-analyses of the literature on retained lens fragments timing were described previously13,21 and are summarized in Figure S1. The publication date range for the MEDLINE search was January 1, 1985 to July 16, 2013. All study designs were considered, and no previous meta-analysis comparing SD-PPV and DEL-PPV outcomes was found. Internal review board approval and informed consent are not required for a meta-analysis.
Inclusion criteria
A study was included in the meta-analysis if it contained at least ten patients who received a vitrectomy for intravitreal retained lens fragments after surgery for an age-related cataract; had mean follow-up of at least 3 months; and had results for both SD-PPV and DEL-PPV patients, including the number receiving each treatment (SD-PPV and DEL-PPV), and the number in each treatment group who experienced at least one of the outcomes.
Data extraction
For each study/outcome combination, the number of patients was recorded, separately for those who did and did not experience that outcome, for SD-PPV and DEL-PPV. Our previous research indicated that when an SD-PPV was not performed, a vitreoretinal surgeon should wait at least 3 days after cataract surgery before attempting a vitrectomy unless severe complications preclude a delay. Therefore, whenever possible, DEL-PPVs were limited to those performed at least 3 days after cataract surgery. Additional details of the data extraction were described previously.13,21
Study classification
The Mayo Clinic Florida (MCF) SD-PPV policy permits an SD-PPV under a “no move, no wait” policy only if a vitreoretinal surgeon begins the vitrectomy within 15 minutes of cataract surgery and the patient is not moved from the original operating room. In addition, the policy precludes cataract surgeons from attempting to remove intravitreal retained lens fragments.35 Based on the information available, articles were classified as MCF+ if their SD-PPVs met criteria similar to those at the MCF and as MCF− if their SD-PPVs did not meet these criteria.
The three criteria were SD-PPVs performed 1) at the same facility as the cataract surgery, 2) with only a short time between cataract surgery and vitrectomy, and 3) without any cataract surgeons attempting to remove the intravitreal retained lens fragments. SD-PPV was coded as “same facility” if the authors indicated immediate vitrectomy, vitrectomy at the time of cataract surgery, or that SD-PPV was possible only if cataract surgery was done in a facility where a vitreoretinal surgeon was available. SD-PPV was coded as “a short time between cataract surgery and vitrectomy” if the authors indicated this explicitly or implied this, for example: immediate, converted to vitrectomy, or same operating room. SD-PPV was coded as “different facility” and/or “not a short time between cataract surgery and vitrectomy” if the above conditions were not met and/or if the authors indicated that some or all of the SD-PPV patients were “referred to our facility”. All facilities were coded based on whether the authors indicated that any cataract surgeons attempted to remove intravitreal retained lens fragments for SD-PPV patients during cataract surgery.
Estimating the effect for each study
The summary effect for the meta-analysis was the risk difference of patients experiencing each outcome between the SD-PPV and DEL-PPV treatment groups. To estimate the risk difference in the population, using sample data from each study, the observed risk was determined by dividing the number of events (occurrence of the adverse outcome, such as retinal detachment) in each treatment group (SD-PPV and DEL-PPV) by the number of patients in that group. The risk difference for each study was the proportion of DEL-PPV patients minus the proportion of SD-PPV patients, so positive numbers “favored” (indicated superior outcomes with) SD-PPV, while negative numbers favored DEL-PPV.
When possible, the variance for each risk difference was estimated using the standard formula for estimating the variance of a risk difference.36 However, when there were no events (or no nonevents) in a study treatment group (SD-PPV and/or DEL-PPV), the variance was estimated using the observed proportion of events in the total sample (SD-PPV plus DEL-PPV groups) for that study or the overall proportion of events (in that treatment group) in all studies.21 The effect of including studies whose variance was not estimated using the standard formula for estimating the variance of a risk difference was assessed with a sensitivity analysis.
Statistical analyses
Meta-analyses were performed using Comprehensive Meta-Analysis, version 2.2 (Biostat Inc., Englewood, NJ, USA). As in our previous research, random-effects models were used in the main meta-analyses. All additional meta-analyses, which compared subgroups of studies, used mixed-effect models, combining studies within subgroups using random-effects models but combined subgroups using fixed-effects models. These mixed-effect models did not assume a common variance across subgroups (no pooling of variance), but rather, the variance in each subgroup was estimated separately. These additional analyses assessed how results differed between MCF+ and MCF− studies and, for MCF+ studies only, by the timing of the DEL-PPV. We also assessed effects of reporting and publication biases, including studies whose variance was not estimated using the standard formula (discussed above), and assessed whether the results were robust with sensitivity analyses.37,38 Results were statistically significant with P-value ≤0.05 and marginally significant with 0.05<P≤0.15.35,39
Results
Search results
A total of 304 articles were identified (230 through PubMed and 74 from other sources, including articles’ reference lists), with 128 excluded based on reading the title and abstract. Full text of the remaining 176 articles was retrieved and reviewed. A total of 76 articles were included in the systematic review of the retained lens fragments literature. However, only 23 articles with 21 unique study cohorts had the data necessary for the SD-PPV vs DEL-PPV meta-analysis.
In one article,40 there were data for only the study (not the control) group, so only these patients were included. All the patients in Kim et al22 and Moore et al7 were also in Modi et al32 but no patients were double-counted. Modi et al32 was used for VA, CME, and corneal edema; Moore et al7 was used for retinal detachment; and Kim et al22 was used for increased IOP and intraocular inflammation/infection. This was done to preferentially use data for final outcomes rather than for outcomes any time after the vitrectomy. Nine (39%) articles were MCF− and 14 (61%) were MCF+ (see the “Study classification” section). A summary of the initial search results of the “retained lens fragments timing” literature appeared previously.13 Figure 1 contains a summary, in the standard format,41 of the updated search results.
Table 1 contains details for the 23 articles (21 studies). The studies’ locations were: six of 21 from the USA/Canada (29%), nine from Europe (43%), five from Asia (24%), and one from Australia (5%). Patients were treated from 1988 to 2011, so overall, there were 24 years of service for all the studies collectively, with an average of 6.6 years of service per study (range 1 to 22 years of service). The studies tended to be small, with 17 (81%) including fewer than 100 patients. Collectively, studies included in the meta-analysis had data for 1,606 eyes, with a mean of 76.5 eyes per study (median =25; range 12 to 569 eyes). Of these, 1,596 (99.4%) eyes received a vitrectomy (article range 83% to 100%), and ten eyes (0.6%) received medical management. Of the eyes that received a vitrectomy, 337 (21%) received an SD-PPV and 1,259 (78%) received a DEL-PPV. Approximately 52% of the patients were female, with an average age of 74.2 years (study means range from 54 to 78 years). Including the SD-PPV patients, the average time between cataract surgery and vitrectomy was 13.8 days (study mean range 1.7 to 41 days), and mean follow-up time was approximately 13.6 months (study mean range 3 to 63 months).
Quality analysis
Overall quality issues were similar to those in our previous meta-analysis.13 In 18 (78%) of 23 articles, patients were a consecutive series (a representative sample of the population), but only one (4%) article was a prospective study. In 21 (91%) articles, the years of service were stated, all patients were accounted for, and patients’ characteristics at presentation were reported. Reasons were given for all lost/excluded patients in 20 (87%) articles, but in only 17 (74%) articles was information reported on all patients excluded for missing data or loss to follow-up. In 14 (61%) articles, the authors specified standardized assessments of outcomes, and in 13 (57%) articles, the authors indicated their criteria for treatment choice (vitrectomy timing). Only eleven (48%) articles reported preexisting ocular comorbidities and actual P-values.
Also, using the Minckler42 evidence-based rating system, for clinical importance, 19 (83%) articles were rated A, one (4%) article was rated B, and three articles were rated C (13%). For Minckler’s other criterion, strength of evidence, all articles were rated III (weak), mainly because the research was retrospective. Two (9%) articles reported data for all seven outcomes, two (9%) articles for six outcomes, five (22%) articles for five outcomes, three (13%) articles for four outcomes, three (13%) articles for three outcomes, four articles (17%) for two outcomes, and four (17%) articles for one outcome. Five (22%) articles had average follow-up time between 3 and 6 months, nine (39%) articles between 6 and 12 months, six (26%) articles between 12 and 24 months, and three (13%) articles for more than 24 months.
Statistical significance analysis
Our previous research discussed low statistical power in the retained lens fragments timing literature. The analysis estimating each study’s power for comparing outcomes was updated, and the results (mean =24%, median =14%) again indicated that many studies had low power. Figure 2A shows whether SD-PPV or DEL-PPV seemed better for each outcome, for all articles with these data.2,3,6,7,11,12,14,15,17–19,22,24–27,29–31,34,35,40,43–45 These SD-PPV vs DEL-PPV results appear mixed and do not obviously favor either vitrectomy time.
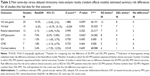
Main SD-PPV vs DEL-PPV meta-analysis
These results (Table 2) favored SD-PPV for all outcomes except bad VA, remembering that a positive risk difference “favored” (indicated superior outcomes with) SD-PPV, while a negative risk difference favored DEL-PPV. However, only one of the results among the outcomes that favored SD-PPV (not good VA, retinal detachment, increased IOP, intraocular inflammation/infection, CME, and corneal edema) was statistically significant. The IOP results indicated a significant risk difference of 7.0% between SD-PPV and DEL-PPV (P=0.042 [z-test], 95% confidence interval = [0.2% to 13.8%]). Also, the corneal edema results were heavily influenced by a single case, which was the only SD-PPV patient in one study.6 These results do not provide enough evidence to indicate a consistent association between clinical outcomes and vitrectomy timing (SD-PPV or DEL-PPV) and agree with the statistical significance analysis in Figure 2A.
Separate MCF+ and MCF− meta-analyses
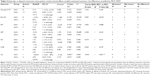
Another statistical significance analysis, with studies separated into MCF+ (Figure 2B) and MCF− (Figure 2C), indicted that SD-PPV might have produced better outcomes in MCF+ studies2,7,11,17–19,22,24,25,27,30,32,35,40,44,45 but not in MCF− studies.3,6,12,14,15,26,29,31,34,43 Table 3 compares the percent of SD-PPV and DEL-PPV patients with each outcome, by MCF policy status. Figures 2B and 2C, along with the data in Table 3, support a hypothesis that the risk differences between immediate SD-PPV and DEL-PPV (in MCF+ studies) more consistently favor SD-PPV than the risk differences between nonimmediate SD-PPV and DEL-PPV (in MCF− studies).
  | Table 3 Same-day vitrectomy and delayed vitrectomy risk and risk difference for each clinical outcome, separated for MCF− and MCF+ articles |
Therefore, meta-analyses were done separately for the MCF+ and MCF− studies, and these results differed from those done with all the studies combined (compare Tables 2 and 4). For the MCF+ studies, all results favored SD-PPV (except intraocular inflammation/infection, which was essentially neutral). For five of seven outcomes (not good VA, bad VA, retinal detachment, increased IOP, and corneal edema), the effect favoring SD-PPV was statistically significant. In the MCF+ studies, the number needed to treat, with immediate SD-PPV rather than DEL-PPV, to avoid all five statistically significant outcomes, was four.36 This provided some evidence that immediate SD-PPVs (performed according to policies similar to the MCF SD-PPV policies) produced better outcomes than DEL-PPVs.
For the MCF− studies, three outcomes favored SD-PPV (not good VA, increased IOP, and intraocular inflammation/infection) and four favored DEL-PPV (bad VA, retinal detachment, CME, and corneal edema). The only significant (corneal edema) or marginally significant (bad VA) effects favored DEL-PPV. Based on these mixed, mostly nonsignificant results, there was little evidence to favor either vitrectomy timing (SD-PPV or DEL-PPV) for the MCF− studies, so further analyses were limited to the MCF+ studies only.
An examination of the forest plot from the not good VA meta-analysis (Figure 3) visually supported a conclusion that the estimated summary risk difference did not indicate better outcomes with either SD-PPV or DEL-PPV for the MCF− studies (top) but did indicate better outcomes with immediate SD-PPV for the MCF+ studies (bottom). The forest plots for the remaining outcomes (not shown) were similar.
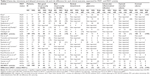
Subgroup analysis: DEL-PPV time after cataract surgery (MCF+ only)
The results of our previous meta-analysis indicated, for vitrectomies performed 3 or more days after cataract surgery, that prompt (earlier) vitrectomies (3 to 7 or 3 to 14 days after cataract surgery) provided better outcomes (for not good VA, bad VA, retinal detachment, increased IOP, and intraocular inflammation/infection).13 Based on these results, we investigated whether superior outcomes for immediate SD-PPV (in MCF+ studies) were sensitive to the time until the DEL-PPV. These analyses did not include CME and intraocular inflammation/infection because for these outcomes, there were no significant or marginally significant differences between SD-PPV and DEL-PPV in the MCF+ studies (Table 4).
Delayed vitrectomy time periods and data issues
Five DEL-PPV time periods (after cataract surgery) were analyzed. Three time periods were considered “prompt” DEL-PPV (3 to 7, 3 to 14, and 7 to 14 days after cataract surgery), and two time periods were considered “nonprompt” DEL-PPV (7 or more days and 15 or more days after cataract surgery. For studies that provided individual patient data (including the exact day postcataract surgery of the vitrectomy), the time periods were exact. However, for studies that provided data grouped into time intervals, the time periods were based on average (often estimated) times. For these studies, some vitrectomies done on days 1 and 2 after cataract surgery (previously determined to be time needed for the eye to “recover” from cataract surgery)13 may have been included in the 3 to 7 and 3 to 14 days, data, and some vitrectomies done in weeks 3 and 4 after cataract surgery may have been included in the 3 to 14 and 7 to 14 days, data. This occurred as long as the average delay was within these time periods because it was impossible to separate the grouped results.
In addition, not every study provided data for each time period. For example, in some studies, no vitrectomies were performed 3 to 7 days after cataract surgery. For each outcome (not good VA, bad VA, retinal detachment, increased IOP, and corneal edema), an initial analysis was performed to estimate a summary effect (risk difference) comparing SD-PPV to various DEL-PPV time periods, including all MCF+ studies with data for any of the DEL-PPV time periods. Summaries of these results are found in the shaded areas of Table 5. Three subsequent analyses were performed, using only studies that had data for all the time periods being compared. One analysis compared SD-PPV to DEL-PPV performed 3 to 7, 7 to 14, and 15+ days after cataract surgery. The second analysis compared SD-PPV to DEL-PPV performed 3 to 7 and 7+ days after cataract surgery. The third analysis compared SD-PPV to DEL-PPV performed 3 to 14 and 15+ days after cataract surgery. Summaries of these results are found in the unshaded areas of Table 5. These subsequent comparisons were done because there was a reasonable amount of heterogeneity (ie, between-study variability in effects [see the I-squared statistics in Table 4]) in some of the initial MCF+ analyses.
Because the above analyses compared the results for immediate SD-PPVs to only a subset of the DEL-PPVs for each study, the sample size and number of events was often quite small, and there were many studies with no events (or nonevents) in one or both treatment groups. In particular, some corneal edema results were based on only one or two MCF+ studies. Therefore, these results are preliminary and not conclusive.
Detailed results (discussed below) for these analyses are not shown but are available on request. Figure 4A shows the median and range of the estimated risk differences for immediate SD-PPV (MCF+) vs prompt DEL-PPV, and Figure 4B provides the same information for immediate SD-PPV vs nonprompt DEL-PPV.
Same-day vs prompt delayed vitrectomies
Overall, these results (Figure 4A) show no consistent pattern of risk differences favoring either immediate SD-PPV or prompt DEL-PPV (3 to 7, 3 to 14, or 7 to 14 days after cataract surgery). Of the 35 total comparisons of immediate SD-PPV and prompt DEL-PPV, only one (3%) (favoring immediate SD-PPV) was statistically significant, nine (26%) had P-values between 0.05 and 0.50 (eight [23%] favoring immediate SD-PPV and one favoring prompt DEL-PPV), and 25 (71%) had P-values greater than 0.50, providing little evidence of an association between clinical outcomes and immediate SD-PPV or prompt DEL-PPV. Based on this lack of a consistent pattern in comparisons of immediate SD-PPV and prompt DEL-PPV, there is a preliminary indication that prompt DEL-PPV produces outcomes that are similar to those produced by immediate SD-PPV (Figures 4A and 5).
Same-day vs nonprompt delayed vitrectomies
However, all 25 results comparing immediate SD-PPV to nonprompt DEL-PPV (7+ and 15+ days after cataract surgery) favored immediate SD-PPV with eight (32%) statistically significant, 14 (56%) with P-values between 0.05 and 0.50, and three (12%) with P-values greater than 0.50. None favored nonprompt DEL-PPV. This provides a preliminary indication that nonprompt DEL-PPV produces outcomes that may be inferior to those from immediate SD-PPV (Figures 4B and 5).
Results summary
The SD-PPV vs DEL-PPV results are summarized in Figure 6, for all studies (Figure 6A) and separately for MCF+ (Figure 6B) and MCF− studies (Figure 6C). For all studies together and for the MCF− studies, the results did not indicate an association between clinical outcomes and whether the patient had an SD-PPV or DEL-PPV. However, there was evidence that immediate SD-PPV (MCF+ studies) may produce better outcomes than DEL-PPV. These results were robust in analyses for publication/reporting biases and all sensitivity analyses (results not shown).21
Comparisons of immediate SD-PPV with prompt or nonprompt DEL-PPV cannot be considered conclusive, due to small samples, but were congruent with results from our previous meta-analyses.13 Comparisons of immediate SD-PPV and prompt DEL-PPV did not consistently favor either vitrectomy time. This supports a preliminary hypothesis that patients who receive a prompt DEL-PPV might enjoy outcomes that are comparable with those who receive an immediate SD-PPV. However, all comparisons of immediate SD-PPV and nonprompt DEL-PPV favored SD-PPV.
Discussion
Patient displeasure is common following complicated cataract surgery46,47 and tends not to improve if reduced VA persists.48 One article reported that, “most patients [with retained lens fragments], who had expected a rapid visual recovery after cataract surgery, were very dissatisfied with poor vision postoperatively.”27 SD-PPV could help to mitigate this patient dissatisfaction.49
Some authors have suggested that cataract surgery on eyes with increased risk for retained lens fragments be performed at a facility where a vitreoretinal surgeon is available.28 One author extended this recommendation to any cataract surgeon learning phacoemulsification.50 Our results do not support these suggestions for all cataract surgery patients (although future research may support these for patients with specific risk factors). As long as the cataract surgeon refers the patient to a vitreoretinal surgeon in time for a prompt DEL-PPV (3 to 7 or perhaps 14 days after cataract surgery), our results provide support for current cataract surgery practice patterns and locations.
Previously reported results for SD-PPV were mixed.23 Some facilities had good VA results,22,24,25 while other facilities’ results were not as good.26–28 In one study, six SD-PPV patients had cataract surgery done at a facility with a vitreoretinal unit: one had a massive choroidal hemorrhage, and another had corneal decomposition, possibly “related to prolonged use of intraocular fluids”.26 Elsewhere, excessive use of infusion fluid was contraindicated to prevent traction and retinal complications.6 One study reported no retinal detachments among 38 patients who received an SD (or next-day) vitrectomy,31 while, in another study, four of six SD-PPV patients had a retinal detachment.18
The reasons for inconsistent SD-PPV results are not clear, but based on our results, part of the explanation may be that policies and strategies for SD-PPV differ. It is possible that immediate SD-PPV, when cataract surgeons do not attempt retained lens fragment retrieval, produces superior results,35 but other SD-PPV strategies may not be as good. Perhaps immediate SD-PPV removes the lens fragments before the onset of time-dependent inflammation and the accompanying choroidal congestion that occurs with same-day patient transfer between surgical facilities. Immediate SD-PPV for retained lens fragments closely resembles a planned pars plana lensectomy, something frequently performed, without complications, by vitreoretinal surgeons. Compared with waiting several hours between surgeries, immediate SD-PPV may take advantage of a clear cornea and minimally inflamed eye to enable better removal of retained lens fragments, with fewer complications. Reasons for inconsistent SD-PPV results might also include characteristics of the eyes and/or surgeons, which could not be explored in a meta-analysis using study-level data.
These results support our previous research on vitrectomy timing. Our previous analysis of MCF SD-PPV vs DEL-PPV data35 indicated that immediate SD-PPV was associated with superior clinical outcomes. Our previous meta-analysis, which assessed the effect of increasing vitrectomy delays (3 or more days after cataract surgery), indicated that prompt DEL-PPV outcomes were superior to later (nonprompt) DEL-PPV outcomes.13 The current meta-analysis indicated that immediate SD-PPV was associated with superior clinical outcomes compared with all and nonprompt DEL-PPV but that prompt DEL-PPV was associated with outcomes comparable with immediate SD-PPV.
Future research
This leads to a hypothesis that immediate SD-PPV and prompt DEL-PPV may produce equivalent outcomes. A multicenter, randomized controlled trial would be needed to test a noninferiority hypothesis comparing immediate SD-PPV and prompt DEL-PPV outcomes. Although the MCF policy is one alternative, different facilities may have other successful SD-PPV policies. Further research should analyze how SD-PPV results differ based on various SD-PPV strategies, to determine the optimal circumstances for an SD-PPV.
Study limitations
Major limitations include low power due to few patients with adverse events, especially in the SD-PPV group, which was generally much smaller than the DEL-PPV group, and especially in the MCF+ studies (Table 3). Another limitation was the classification of studies as MCF+ or MCF− based solely on information provided in each article (study-based). It is possible that some SD-PPV patients in the MCF− studies received an immediate SD-PPV, which would undermine the internal validity of MCF+/MCF− comparisons and understate any actual differences between these groups.51 Another possible threat to internal validity was selection bias51 because it was not possible to determine whether there were significant between-group (SD-PPV vs DEL-PPV) differences in baseline variables. Comparisons of immediate SD-PPV and prompt DEL-PPV (3 to 7, 3 to 14, or 7 to 14 days after cataract surgery) were affected by data grouped into time intervals, so data from DEL-PPV performed outside these time periods were included in some analyses.
Several additional limitations to meta-analysis of these data were discussed previously.13 As with our previous meta-analysis, this one had little evidence of publication bias, but the studies did exhibit reporting bias, and it is possible that authors were more likely to report significant, rather than nonsignificant, results. However, sensitivity analyses indicated that the overall conclusions were not affected by reporting bias, the inclusion of small studies and those with no events (or nonevents) in a treatment group, or the removal of any one study from the analyses.21
Clinical recommendations
The question of whether SD-PPV for retained lens fragments is appropriate has long been debated by vitreoretinal surgeons, with many firmly on one side (in favor of SD-PPV) and others just as firmly on the other. This research raises the possibility that this lack of consensus may have occurred because all SD-PPVs cannot be considered as the same clinical option. There appears to be at least two distinct variations of SD-PPV: immediate SD-PPV performed under strategies such as the MCF “no move, no wait” policy35 and SD-PPV performed under different strategies that permit longer waits and/or interfacility patient transport.
Some ophthalmologists who support SD-PPV may have had good clinical experience with immediate SD-PPV compared with DEL-PPV that occurred weeks, months, or even years after cataract surgery. On the other hand, it is possible that some ophthalmologists who do not support SD-PPV have had experiences with SD-PPV after long delays and/or interfacility patient transport that were not as positive. This meta-analysis may help inform the SD-PPV debate with the contribution that while SD-PPV may be appropriate under some policies (for example, immediately with no waiting or interfacility patient transport), SD-PPV may often be inappropriate under other policies.
Conclusion
This research provides some preliminary evidence that SD-PPV may be unnecessary as long as prompt DEL-PPV would be performed. Some cataract surgery practice patterns can accommodate either immediate SD-PPV or prompt DEL-PPV because the cataract surgeons operate at the same facility as a vitreoretinal surgeon, but most operate where a vitreoretinal surgeon is not readily available. These results, coupled with the results of our previous meta-analysis, provide a preliminary indication that if an immediate SD-PPV cannot be performed, the cataract surgeon need not attempt to transfer the patient to another facility for an SD-PPV, but should refer the patient to a vitreoretinal surgeon so that a prompt DEL-PPV can be performed.
Disclosure
The authors report no conflicts of interest in this work.
References
Slusher MM. The new cataract surgery: phacoemulsification. South Med J. 1976;69(4):385–386. | ||
Kaynak S, Celik L, Kocak N, Oner FH, Kaynak T, Cingil G. Staining of vitreous with triamcinolone acetonide in retained lens surgery with phacofragmentation. J Cataract Refract Surg. 2006;32(1):56–59. | ||
Chiang A, Garg SJ, Alshareef RA, et al. Removal of posterior segment retained lens material using the OZil phacoemulsification handpiece versus Fragmatome during pars plana vitrectomy. Retina. 2012;32(10):2119–2126. | ||
Foster A. Vision 2020: The cataract challenge. Community Eye Health. 2000;13(34):17–19. | ||
Rofagha S, Bhisitkul RB. Management of retained lens fragments in complicated cataract surgery. Curr Opin Ophthalmol. 2011;22(2):137–140. | ||
Ross WH. Management of dislocated lens fragments following phacoemulsification surgery. Can J Ophthalmol. 1993;28(4):163–166. | ||
Moore JK, Scott IU, Flynn HW, et al. Retinal detachment in eyes undergoing pars plana vitrectomy for removal of retained lens fragments. Ophthalmology. 2003;110(4):709–713; discussion 713–714. | ||
Stewart MW. Managing retained lens fragments: raising the bar. Am J Ophthalmol. 2009;147(4):569–570. | ||
Merani R, Hunyor AP. Medical versus surgical management of retained lens fragments. J Cataract Refract Surg. 2009;35(12):2181; author reply 2181. | ||
Blodi BA, Flynn HW, Blodi CF, Folk JC, Daily MJ. Retained nuclei after cataract surgery. Ophthalmology. 1992;99(1):41–44. | ||
Hansson LJ, Larsson J. Vitrectomy for retained lens fragments in the vitreous after phacoemulsification. J Cataract Refract Surg. 2002;28(6):1007–1011. | ||
Yang CS, Lee FL, Hsu WM, Liu JH. Management of retained intravitreal lens fragments after phacoemulsification surgery. Ophthalmologica. 2002;216(3):192–197. | ||
Vanner EA, Stewart MW. Vitrectomy timing for retained lens fragments after surgery for age-related cataracts: a systematic review and meta-analysis. Am J Ophthalmol. 2011;152(3):345–357.e3. | ||
Stefaniotou M, Aspiotis M, Pappa C, Eftaxias V, Psilas K. Timing of dislocated nuclear fragment management after cataract surgery. J Cataract Refract Surg. 2003;29(10):1985–1988. | ||
Tajunisah I, Reddy SC. Dropped nucleus following phacoemulsification cataract surgery. Med J Malaysia. 2007;62(5):364–367. | ||
Al-Amri AM. Visual outcome of pars plana vitrectomy for retained lens fragments after phacoemulsification. Middle East Afr J Ophthalmol. 2008;15(3):107–111. | ||
Ruiz-Moreno JM, Barile S, Montero JA. Phacoemulsification in the vitreous cavity for retained nuclear lens fragments. Eur J Ophthalmol. 2006;16(1):40–45. | ||
Borne MJ, Tasman W, Regillo C, Malecha M, Sarin L. Outcomes of vitrectomy for retained lens fragments. Ophthalmology. 1996;103(6):971–976. | ||
Stenkula S, Byhr E, Crafoord S, et al. Tackling the “dropped nucleus”. Acta Ophthalmol Scand. 1998;76(2):220–223. | ||
Pande M, Dabbs TR. Incidence of lens matter dislocation during phacoemulsification. J Cataract Refract Surg. 1996;22(6):737–742. | ||
Vanner EA. Analysis of Timing Effects of Pars Plana Vitrectomy for Removal of Intravitreal Crystalline Retained Lens Fragments after Surgery For Age-Related Cataracts [dissertation]. Stony Brook, NY: Stony Brook University; 2013. | ||
Kim JE, Flynn HW Jr, Smiddy WE, et al. Retained lens fragments after phacoemulsification. Ophthalmology. 1994;101(11):1827–1832. | ||
Stewart MW. Management of retained lens fragments: can we improve? Am J Ophthalmol. 2007;144(3):445–446. | ||
Chen CL, Wang TY, Cheng JH, Tai MC, Lu DW, Chen JT. Immediate pars plana vitrectomy improves outcome in retained intravitreal lens fragments after phacoemulsification. Ophthalmologica. 2008;222(4):277–283. | ||
Romero-Aroca P, Fernández-Ballart J, Méndez-Marín I, Salvat-Serra M, Baget-Bernaldiz M, Buil-Calvo JA. Management of nucleus loss into the vitreous: long term follow up in 63 patients. Clin Ophthalmol. 2007;1(4):505–512. | ||
Stilma JS, van der Sluijs FA, van Meurs JC, Mertens DA. Occurrence of retained lens fragments after phacoemulsification in The Netherlands. J Cataract Refract Surg. 1997;23(8):1177–1182. | ||
Tommila P, Immonen I. Dislocated nuclear fragments after cataract surgery. Eye (Lond). 1995;9(Pt 4):437–441. | ||
Lai TY, Kwok AK, Yeung YS, et al. Immediate pars plana vitrectomy for dislocated intravitreal lens fragments during cataract surgery. Eye (Lond). 2005;19(11):1157–1162. | ||
Watts P, Hunter J, Bunce C. Vitrectomy and lensectomy in the management of posterior dislocation of lens fragments. J Cataract Refract Surg. 2000;26(6):832–837. | ||
Konstantopoulos A, Yadegarfar G, Madhusudhana K, et al. Prognostic factors that determine visual outcome following cataract surgery complicated by vitreous loss. Eur J Ophthalmol. 2009;19(2):247–253. | ||
Merani R, Hunyor AP, Playfair TJ, et al. Pars plana vitrectomy for the management of retained lens material after cataract surgery. Am J Ophthalmol. 2007;144(3):364–370. | ||
Modi YS, Epstein A, Smiddy WE, Murray TG, Feuer W, Flynn HW. Retained lens fragments after cataract surgery: outcomes of same-day versus later pars plana vitrectomy. Am J Ophthalmol. 2013;156(3):454–459. | ||
Scott IU, Flynn HW, Smiddy WE, et al. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments. Ophthalmology. 2003;110(8):1567–1572. | ||
Colyer MH, Berinstein DM, Khan NJ, et al. Same-day versus delayed vitrectomy with lensectomy for the management of retained lens fragments. Retina. 2011;31(8):1534–1540. | ||
Vanner EA, Stewart MW, Liesegang TJ, Bendel RE, Bolling JP, Hasan SA. A retrospective cohort study of clinical outcomes for intravitreal crystalline retained lens fragments after age-related cataract surgery: a comparison of same-day versus delayed vitrectomy. Clin Ophthalmol. 2012;6:1135–1148. | ||
Bland M. An Introduction to Medical Statistics. 3rd ed. Oxford: Oxford University Press; 2000. | ||
Deeks JJ, Higgins JPT, Altman DG, editors. Chapter 9: Analyzing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons Ltd; 2008:243–296. | ||
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. Chichester: John Wiley & Sons, Ltd; 2009. | ||
Pagano M, Gauvreau K. Principles of Biostatistics. 2nd ed. Pacific Grove, CA: Duxbury; 2000. | ||
Verma L, Gogoi M, Tewari HK, Kumar A, Talwar D. Comparative study of vitrectomy for dropped nucleus with and without the use of perfluorocarbon liquid. Clinical, electrophysiological and visual field outcomes. Acta Ophthalmol Scand. 2001;79(4):354–358. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W264. | ||
Minckler D. Evidence-based ophthalmology series and content-based continuing medical education for the journal. Ophthalmology. 2000;107(1):9–10. | ||
Terasaki H, Miyake Y, Miyake K. Visual outcome after management of a posteriorly dislocated lens nucleus during phacoemulsification. J Cataract Refract Surg. 1997;23(9):1399–1403. | ||
Greve MD, Peyman GA, Mehta NJ, Millsap CM. Use of perfluoroperhydrophenanthrene in the management of posteriorly dislocated crystalline and intraocular lenses. Ophthalmic Surg. 1993;24(9):593–597. | ||
Ang GS, Whyte IF. Effect and outcomes of posterior capsule rupture in a district general hospital setting. J Cataract Refract Surg. 2006;32(4):623–627. | ||
Lambrou FH Jr, Stewart MW. Management of dislocated lens fragments during phacoemulsification. Ophthalmology. 1992;99(8):1260–1262. | ||
Boscher C, Lebuisson DA, Lean JS, Nguyen-Khoa JL. Vitrectomy with endoscopy for management of retained lens fragments and/or posteriorly dislocated intraocular lens. Graefes Arch Clin Exp Ophthalmol. 1998;236(2):115–121. | ||
Lu H, Jiang YR, Grabow HB. Managing a dropped nucleus during the phacoemulsification learning curve. J Cataract Refract Surg. 1999;25(3):447–450. | ||
Dickinson PJ, Greven CM. Avoiding and managing the dislocated crystalline lens. Compr Ophthalmol Update. 2006;7(3):113–127. | ||
Gonvers M. New approach to managing vitreous loss and dislocated lens fragments during phacoemulsification. Cataract Refract Surg. 1994;20(3):346–349. | ||
Shi L. Health Services Research Methods. 2nd ed. Clifton Park, NY: Delmar Learning; 2008. |
Supplementary materials
  | Figure S1 Original search methods for identification of studies (MEDLINE/PubMed). |
Reference
Lefebvre C, Manheimer E, Glanville J. Searching for studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons Ltd; 2008:95–150. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.