Back to Journals » Cancer Management and Research » Volume 14
Mediterranean Dietary Pattern is Associated with Lower Odds of Gastric Cancer: A Case–Control Study
Authors Tayyem R , Al-Awwad N, Allehdan S, Ajeen R, Al-Jaberi T, Rayyan Y, Bawadi H , Hushki A
Received 29 January 2022
Accepted for publication 1 June 2022
Published 17 June 2022 Volume 2022:14 Pages 2017—2029
DOI https://doi.org/10.2147/CMAR.S360468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bilikere Dwarakanath
Reema Tayyem,1,2 Narmeen Al-Awwad,3 Sabika Allehdan,4 Rawan Ajeen,5 Tareq Al-Jaberi,6 Yaser Rayyan,7 Hiba Bawadi,1 Ahmad Hushki8
1Department of Human Nutrition, College of Health Sciences, QU Health, Qatar University, Doha, 2713, Qatar; 2Department of Nutrition and Food Technology, Faculty of Agriculture, University of Jordan, Amman, 11942, Jordan; 3Department of Clinical Nutrition and Dietetics, Faculty of Applied Health Sciences, Hashemite University, Zarqa, Jordan; 4Department of Biology, College of Science, University of Bahrain, Sakhir Campus, Zallaq, Kingdom of Bahrain; 5Department of Nutrition, Gillings School of Global Public Health, The University of North Carolina at ChapelHill, ChapelHill, NC, 27599, USA; 6Department of General & Pediatric Surgery, Faculty of Medicine, Jordan University of Science and Technology, Irbid, 22110, Jordan; 7Department of Gastroenterology & Hepatology, Faculty of Medicine, The University of Jordan, Amman, 11942, Jordan; 8Endoscopy Unit, King Hussein Cancer Center, Amman, Jordan
Correspondence: Ahmad Hushki, Endoscopy Unit, King Hussein Cancer Center, Amman, Jordan, Email [email protected] Reema Tayyem, Department of Human Nutrition, College of Health Sciences, Qatar University, Doha, 2713, Qatar, Email [email protected]
Background: Diet pattern is an important modifiable lifestyle factor. However, epidemiological studies show that the association between dietary patterns and gastric cancer (GC) is conflicting. This study aims to assess the impact of several dietary choices on the risk of GC among newly diagnosed Jordanian patients.
Methods: A case–control study was conducted at major oncology centers and hospitals in Jordan. Study participants included 172 patients with incident gastric cancer and 314 controls. Data was collected using interview-based questionnaires. Dietary intake was estimated using a validated Arabic and reproducible food-frequency questionnaire (FFQ). Dietary patterns were derived using Principal Component Analysis (PCA). Multinomial logistic regression was used to estimate the association between dietary patterns and GC.
Results: Four dietary patterns were itemized; “Mediterranean”, “Prudent”, “Unhealthy” and “High-fruit” dietary patterns. The “Mediterranean” dietary pattern, which includes a diet rich in fresh fruits, vegetables, milk, yogurt, lentils, and olive oil was associated with a significant decrease in the odds ratio (OR) of GC for the third and fourth quartiles (OR, 0.394 (confidence interval (CI): 0.211– 0.736); 0.212 (CI: 0.107– 0.419), respectively) after adjusting for age, gender, body mass index, smoking, marital status, total energy intake, education level, and physical activity. While the “Unhealthy” and “Prudent” dietary patterns enhance the risk of developing GC, this risk was insignificant at any quartile. Additionally, the “High-Fruit” dietary pattern shows an insignificant protective effect against the risk of GC.
Conclusion: The “Mediterranean” dietary pattern was associated with a reduced risk of GC among Jordanians. However, the other three identified dietary patterns were not significantly associated with the risk of GC.
Keywords: dietary patterns, gastric cancer, retrospective, case–control study
Introduction
Despite a reported decline in the incidence rate of gastric cancer (GC), the absolute number of new cases has increased to more than 1.3 million in 2015.1 As the fourth most common malignancy in the world, GC is known for its poor survival rates as it is the second most common cause of cancer-related deaths globally.2 Although the global incidence of GC is gradually decreasing, this malignancy is still expected to display an absolute increasing trend in the next several decades.3 Thus, primary prevention must be an area of focus for the improvement of the prognosis of gastric cancer.3
Growing evidence shows that GC is induced by the combined synergistic effects of Helicobacter pylori infection, genetic instability, and behavioural and environmental factors, including diet.4 Diet has been implicated as a leading contributor to cancer5 in agreement with other studies on nutrition and gastric cancer that suggested the relevancy of dietary factors.6 However, it is difficult to attribute individual foods and nutrients to disease risk in observational studies,7 due to the collinearity that exists between foods and nutrient-nutrient interactions.8 Therefore, a more appropriate method for assessing the combined effect of food and nutrient interaction is to explore the association between dietary patterns and disease.9
Previous diet-disease studies suggested that different food patterns have different effects on gastrointestinal tumors.6 The majority of these studies have identified that Western, Unhealthy, Healthy and Prudent dietary patterns play a role in disease outcome.7,10 However, the association of these dietary patterns and comparability across different populations remains unclear. Particularly, the association of a Western diet with GC. A case–control study from Iran reported that the Western dietary pattern which is typically high in processed meat, sweets, soft drinks, high-fat dairy, fast food, and sauces is directly associated with the risk of GC.11 Similarly, a case–control study conducted by researchers in Canada also found that the Western dietary pattern is associated with increased odds of GC.7 While another study reported no effect of the Western dietary pattern on the risk of GC.10 Additionally, a study conducted in Japan also found that a Western diet was not associated with the risk of GC.12
Due to the mixed results in the literature on the role of diet and dietary patterns on GC, our study aimed to explore the association between dietary patterns and the risk of GC in Jordan. Additionally, the study highlighted the role of dietary patterns in preventing or developing to GC in a country where both Mediterranean and Western diets are contemporary.
Methods
Study Design and Participants
This case–control study was conducted in Jordan between March 2015 and August 2018. Two hundred and fourteen GC patients with a confirmed medical diagnosis of gastric cancer were invited to participate in this study. However, only 172 patients accepted to participate in this study. Additionally, 350 controls were also invited to join the study. The control group included 314 individuals who were conveniently selected from the community without the diagnosis of any form of cancer. The response rate for the cases 80% was and for the controls was 90%. The population-based controls were matched to the cases based on age, occupation, and marital status. The ratio of cases to controls in this study was 1:2.
The inclusion criteria for both cases and controls included Jordanian nationality, 18 years or older at the time of enrollment, ability to communicate verbally, and free of any chronic diseases that require major dietary modifications such as kidney disease, liver disease, or celiac disease. For the cases, patients were conveniently enrolled if they were diagnosed with GC in the last six months. Exclusion criteria included individuals who were pregnant and lactating, following a vegetarian diet, critically ill, hospitalized, and unable to communicate verbally. Only participants with diabetes mellitus, cardiovascular diseases and hypertension were included. Around 28 participants were complaining of diseases that did not require major changes in diet (gallbladder, arthritis, migraine and knee joint replacement).
Cases were enrolled from four hospitals including an oncology center. These hospitals were King Hussein Cancer Center, King Abdullah University Hospital, Jordan University Hospital, and Al-Bashir Hospital. The selected cases represent almost the entire population of GC patients.
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board Ethics Committee of the King Hussein Cancer Center (IRB No. 15 KHCC 03, Amman, Jordan), King Abdullah University Hospital, Jordan University Hospital, and Al-Bashir Hospital. Informed consent was obtained from all participants before enrollment in the study and they were all informed about the purpose and the procedure of the study.
Data Collection
Trained dietitians completed personal, physical activity, and food frequency questionnaires via in-person interviews. The personal questionnaire included questions related to age, gender, marital status, educational level, employment status, family income/month, smoking status, previous and current health problems, and family history of cancer.
Dietary Assessment
Data on diet was collected using a validated Arabic food frequency questionnaire (FFQ) for dietary assessment.13 Standardized food models (NASCO, Saugerties, NY, USA) and standard measuring tools were used (NASCO, Saugerties, NY, USA) to estimate portion sizes. Food lists in the FFQ were categorized based on the type of food: 21 items of fresh and dried fruits and juices; 21 items of fresh and cooked vegetables; 8 items of the most common consumed cereals; 9 items of milk and dairy products; 4 items of legumes; 16 items of all types of meat; 4 items of soups and sauces; 5 items of drinks; 4 items of snacks and sweets; and 14 items of herbs and spices. Total energy intakes were analyzed using dietary analysis software (Food Processor SQL version 10.1.129; ESHA, USA) with additional data on foods consumed in Jordan14 to estimate daily intake of energy.
Anthropometric Measurements
Participants’ body weight and height were measured using standardized techniques and calibrated tools using a calibrated scale (Omron, Japan).15 Body mass index (BMI) was calculated by dividing weight (kilograms) by height squared (meters).15
Seven-Day Physical Activity Recall (PAR)
The validated Seven-Day Physical Activity Recall (Seven-Day PAR) questionnaire was used to measure physical activity levels. Seven-Day PAR is a questionnaire that focuses on a participant’s recall of the usual time spent doing a physical activity over a seven-day period.16 The scores of the physical activity were calculated according to Thompson et al.17
Statistical Analysis
SPSS version 22.0 (IBM SPSS Statistics for Windows, IBM Corporation) was used to perform all statistical analyses. For descriptive statistics, mean±standard deviation (SD) and percentages were used.
Dietary patterns were derived using principal component analysis (PCA) from factor analysis. Consumption frequency was used to identify the dietary patterns. The foods in the FFQ were separated into 51 food items based on their similarity of nutrient content and culinary usage or their reported relationship with GC (Table 1). These factors explained 30.34 of the total variance in the original data set. Only the magnitude of each loading was used to name the factors. A Kaiser–Meyer–Olkin (KMO) test and Bartlett’s test of sphericity were used to assess the suitability of using factor analysis for this exercise. Sampling adequacy and inter-correlation of factors were supported by KMO value >0.577 and Bartlett’s test of sphericity <0.001, respectively. Factors were retained based on an eigenvalue of >1.25 for the screen plot. Further, Varimax rotation was applied to review the correlations between variables and factors. Food items with absolute factor loadings > 0.25 were considered to have contributed significantly to the pattern. Potential confounders (adjusted for age, gender, BMI, smoking, marital status, total energy intake, education level, family history and physical activity) were chosen based on reported risk factors for GC.18 Odds ratios (OR) and their 95-confidence intervals (CI) were calculated using a multinomial logistic regression model. The significance level was set at p≤ 0.05.
 |  |  |  |
Table 1 Factor Loading Matrix for the Four Major Dietary Patterns Identified in a Representative Sample |
Results
Table 1 shows the different food groups loaded for our four-factor components. The first factor, “Mediterranean”, is mainly loaded with vegetables and fruits. The “Prudent” factor is loaded for food groups such as fruit and vegetables, milk, low- and free-fat white cheeses, soup, whole bread and cereal. In comparison, the “Unhealthy” group contained items like artificial fruit juice, cooked vegetables, cabbage salad, fried potato, pasta, burger and different kinds of processed meat. Lastly, “High- fruit” featured mainly fruits. As described by Al-Awwad et al, study on the same GC cases and controls, the pre-diagnosis weight and BMI of GC cases were significantly higher than controls (Table 2). Additionally, Table 2 reveals that the total physical activity metabolic equivalent- min/week (MET-min/week) was 1031.5 ±42.7 for GC cases and 1314.7±45.6 for controls. However, most of them were considered minimally active.19
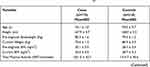 |  |  |
Table 2 Characteristics of the Study Participants (n=486)19 |
Table 3 shows the risk of GC across quartiles of the dietary patterns among study participants, the identified dietary patterns include “Mediterranean”, “High-Fruit”, “Unhealthy” and “Prudent”. The “Mediterranean” dietary pattern presents a diet rich in fresh fruits, vegetables, milk, yogurt, and lentils. This dietary pattern was associated with a significant decrease in the odds of GC at the third and fourth quartiles (OR, CI: 0.394 (0.211–0.736); 0.212 (0.107–0.419), respectively) after adjustment. While the “Unhealthy” and “Prudent” dietary patterns enhance the risk of developing GC, this risk was insignificant at any quartile. Additionally, the “High-Fruit” dietary pattern shows an insignificant protective effect against the risk of GC.
 |
Table 3 Risk of GC Across Quartiles of the Dietary Patterns Among Study Participants |
Discussion
Only a few studies have investigated the role of dietary patterns on GC development among populations living in Middle East countries. Therefore, this study was conducted to explore the possible association between dietary patterns and GC development among Jordanian adults. In the present study, we identified four major dietary patterns and labelled them as “Mediterranean”, “Prudent”, “Unhealthy”, and “High-fruit”. The “Mediterranean” diet is loaded with vegetable and fruit items while the “Prudent” pattern mainly included fruit; vegetables, milk, low and fat-free white cheeses, soup, whole bread and cereals, and the “High-fruit” diet featured fruits. In comparison, the “Unhealthy” diet is loaded with artificial fruit juices, cooked vegetables, cabbage salad, fried potato, pasta, burgers and different types of processed meats. However, due to differences in dietary patterns based on ethnicity, culture, religion, geography and other social determinants, the types of foods and dietary patterns identified may not always be comparable across all studies. Researchers may perceive and identify the same patterns, but these patterns may differ to a greater or lesser degree in the loading of each food variable and/or in the number of variables loaded.20,21 Therefore, dietary patterns should be compared thoroughly between studies, with particular emphasis on the substance of each pattern.21 In the literature, most of the studies that explore the association between data-driven dietary patterns and GC risk identify two types of dietary patterns: a Western/Unhealthy pattern and a Healthy/Prudent pattern.7,10
Our results show that a higher intake of a “Mediterranean” dietary pattern is associated with a lower risk of GC in a case–control study of Jordanian adults. The “Mediterranean” Jordanian diet features characteristics of the Mediterranean diet, such as high fruit and vegetable, olive oil and legume content. This may indicate an overall healthy and anti-carcinogenic eating pattern because of the high concentrations of antioxidant substances, vitamin C, and vitamin E compounds found in some of these foods.21 Antioxidants eliminate free radicals, decrease DNA oxidation, and interfere in several cancer-related biological processes, including carcinogen bio-activation, cell signaling, cell cycle regulation, angiogenesis, and inflammation.10 Furthermore, allium vegetables, particularly garlic, might lower the severity of H. pylori-associated gastritis, and bioactive components in fruit may protect against H. pylori-induced damage, notably inflammation, which has been linked to the development of GC. Additionally, omega-3 polyunsaturated fatty acids, found in fish and nuts, may have anti-cancer properties by affecting several targets involved in cancer progressions, such as cell proliferation, cell survival, angiogenesis, inflammation, and metastasis.10 Many previous case–control studies of GC have found inverse associations with vegetable and fruit consumption.12 Similar to our results, a previous study found that the largest factor loading on a “Mediterranean” pattern with consumption of fruits and vegetables (ie >0.3 KMO for each item) could prevent GC.10,14 Additionally, the frequent consumption of beans was also found to be significantly inversely associated with GC risk.22 A 10-year longitudinal study in Japan found an inverse relationship between a healthy pattern and the incidence of GC in women (rate ratio for highest quartile (RR) 0.56; 95% CI: 0.32–0.96; p for trend 0.03), but not in men. In contrast, the traditional Japanese dietary pattern, which is rich in salty foods such as miso soup and rice, was linked to an elevated risk of GC in both men and women (RR= 2.88, 95% CI: 1.76–4.72; RR= 2.40, 95% CI:1.32–4.3, respectively). A meta-analysis of the association between fruit and vegetable intake and GC risk has indicated relative risks of 0.81 (95% CI: 0.75–0.87) and 0.74 (95% CI: 0.69–0.81) for each 100-g increase in fruit intake and vegetable intake, respectively.7 In a recent systematic review and meta-analysis, the combined OR of gastric cancer for the highest Mediterranean diet score vs the referent was found to be 0.42 (95% CI: 0.2–0.86), and the combined HR was 0.89 (95% CI: 0.68–1.17). The combined OR for the dietary inflammatory index was 2.11 (95% CI: 1.41–3.15). Consequently, it was concluded that the consumption of Mediterranean dietary patterns might reduce gastric cancer risk, while inflammatory dietary patterns might enhance gastric cancer risk.23 Another recent systematic review and meta-analysis of 21 studies showed that a high-quality diet quantified by the Diet Inflammatory Index and Mediterranean Diet Score was significantly associated with a reduced risk of upper gastrointestinal cancer.24 Moreover, a meta-analysis of a case–control and cohort study was conducted to analyze the association between dietary fiber intake (abundant in fruit and vegetables) and GC risk. The authors found that the dose-response analysis associated a 10-g/day increase in fiber consumption with a significant (44%) reduction in GC risk.25 Our results reveal that a “High-fruit” dietary pattern shows no association with GC risk.
The Western/Unhealthy patterns are usually high in processed meat, sweets, soft drinks, high-fat dairy, fast food, and sauces and are directly associated with GC risk.11 On the other hand, other studies reported a null effect of the Western dietary pattern on GC risk.10 The “Unhealthy” pattern in the present study is comparable to the high-meat and western dietary patterns described previously, which is principally characterized by a high intake of all kinds of red meat, processed meat, fresh fish, fish paste, and salt-preserved fish.7,14 No association has been detected between the adherence to the “Unhealthy” dietary pattern and GC risk in the present case–control study. Similarly, the Western pattern was not associated with GC risk in Japan.12 In contrast to our results, it was noticed that higher adherence to the Western pattern in Spain was associated with higher odds of gastric adenocarcinoma even for moderate adherence, going from a 63% increased risk for participants in the second quartile of adherence (OR second vs first quartile (95% CI), 1.63 (1.05; 2.52)), to more than a twofold increased risk for participants in the third and fourth quartiles of adherence (OR third vs the first quartile (95% CI), 2.23 (1.45; 3.43), and OR fourth vs the first quartile (95% CI), 2.09 (1.31; 3.33)).10 A Canadian case–control study revealed that a Western dietary pattern, strongly correlated with soft drinks, French fries, white bread, hamburger, eggs, bacon, doughnuts, and hot dogs were associated with increased risk in women (OR ¼ 1.86, 95% CI: 1.20, 2.89) and men (OR ¼ 1.44, 95% CI: 1.03, 2.02).7 The findings of a population-based case–control study conducted in Connecticut, New Jersey, and Western Washington State suggest that meat/nitrite consumption is linked to an increased risk of esophageal and gastric cancer subtypes, while fruit/vegetable consumption lowers the risk of gastric cardia adenocarcinoma.26 It has been documented that a high amount of salt, nitrates or nitrites, and nitrosamine compounds in processed meat have been linked to an increased risk of GC.12,14 Salt does not directly act as a carcinogen, but it is considered to enhance the risk of GC by causing direct damage to the gastric mucosa, which causes gastritis, increased DNA synthesis, and cell proliferation.22 Although there is no evidence that meat increases the risk of GC, cooking techniques such as grilling or frying at high temperatures can produce carcinogenic heterocyclic amines or polycyclic aromatic hydrocarbons.10,14,22 The iron present in these types of meat might also induce free radicals, which cause DNA double-strand breaks and oncogene activation. Furthermore, saturated fats present in fast food, sauces, and sweets, all of which are part of the Western diet, might induce the production of inflammatory mediators linked to carcinogenesis.10 Additionally, a positive association between red meat consumption and the risk of gastric cancer, and a reverse relationship between white meat intake and the risk of this malignancy.11 Another study found that there was approximately a threefold increased risk of GC for frequent consumption (highest quartile) of both fresh meat (odds ratio (OR) = 3.1) and processed meat (OR = 3.2). Odds ratios were also significantly elevated for frequent consumption of dairy products (OR = 2.7) and fish (OR = 2.2).22 A similar study done in Italy suggested that an increased risk of GC was observed in an “animal product” dietary pattern (OR, 2.13; 95% CI, 1.34–3.40, for the highest versus the lowest quartile of factor score; P trend = 0.0003) and a “starch-rich” pattern (OR, 1.67; 95% CI, 1.01–2.77; P trend = 0.0463). In contrast, the “vitamins and fiber” pattern was inversely associated with GC, with an OR of 0.60 (95% CI, 0.37–0.99; P trend > 0.05) for subjects in the highest quartile as compared with those in the lowest one. The “vegetable unsaturated fatty acids” pattern was not significantly inversely related to gastric cancer.20
The results of our study demonstrated that the “Prudent” dietary pattern was not associated with GC risk. A study conducted in Spain, also found that the “Prudent” dietary pattern has no clear effect on gastric adenocarcinoma risk.10 However, the findings from a Canadian case–control study showed that a prudent dietary pattern rich in vegetables, fruits, and seafood was linked to a lower risk of GC in women (OR ¼ 0.58, 95% CI: 0.37–0.92). Individual scores for vegetables, fiber/whole-grain foods, low consumption of salted/preserved foods, and low intake of sweets/snacks were linked to a lower risk of gastric cancer in women. While, increased fiber/whole grain intake, low salted/preserved food intake, and reduced snack/sweets intake were all linked to a lower risk of GC in men.7 According to the findings of a systematic review and meta-analysis, the “Prudent/Healthy” diet rich in fruits and vegetables had a beneficial effect on the risk of GC, with an odds ratio (OR) of 0.75 (95% (CI): 0.63–0.90) for the highest vs lowest category.27 In contrast, the “Western/Unhealthy” diet, which is high in starchy foods, meat, and fats, was found to negatively impact GC, with an OR of 1.51 (95% CI: 1.21–1.89).27 In the case of dairy products, a collaborative cohort study in Japan found that a high-dairy diet is associated with a lower risk of GC mortality only in males, with multivariate HRs of 0.82 (95% CI: 0.61–1.10), 0.74 (95% CI: 0.54–1.01), and 0.72 (95% CI: 0.52–0.99) for the second, third, and fourth quartiles, respectively.21
Our results should be interpreted in the context of the study’s limitations. First, recall bias is always a concern in case–control studies, especially when evaluating the effect of self-reported dietary information. Moreover, the subjective decisions involved in the definition of dietary patterns, including the number of factors to retain, the type of rotation (if any), and the interpretation and naming of the factors. A further limitation in this study is the lack of available data on Helicobacter pylori infection among study participants. On the other hand, a major strength of our study was the use of a culturally appropriate food frequency questionnaire, which consists of many food items to capture the usual dietary intake of our study population. Finally, the inclusion of cases and controls recruited from major public hospitals ensures proper representation of the different diets coexisting in Jordan.
In conclusion, our study highlights the protective effect of the “Mediterranean” dietary pattern against gastric cancer risk. While, the “Unhealthy”, “Prudent” and “High-fruit” dietary patterns were insignificantly associated at any quartile with the risk of GC in Jordan. This suggests that a diet high in fruits and vegetables and low in processed meat and fat is beneficial to reducing the GC risk.
Data Sharing Statement
Data are available upon request from the corresponding author Reema Tayyem (email: [email protected]).
Ethics Approval and Consent to Participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of King Hussein Cancer Center (IRB No. 15 KHCC 03, Amman, Jordan), King Abdullah University Hospital, Jordan University Hospital, and Al-Bashir Hospital. A written consent form was obtained from each participant and they were all informed about the purpose of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors would like to thank Hashemite University for funding the research project (Grant number AM/16/13/10/1403938).
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Allen C, Allen C, Allen C, et al.; Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 Cancer Groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study published correction appears in JAMA Oncol. 2017 Mar 1; 3(3):418. JAMA Oncol. 2017;3(4):524–548. doi:10.1001/jamaoncol.2016.5688
2. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics published correction appears in CA Cancer J Clin. 2011 Mar-Apr;61(2):134. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107
3. Nagini S. Carcinoma of the stomach: a review of epidemiology, pathogenesis, molecular genetics and chemoprevention. World J Gastrointest Oncol. 2012;4(7):156–169. doi:10.4251/wjgo.v4.i7.156
4. Yamaguchi N, Kakizoe T. Synergistic interaction between Helicobacter pylori gastritis and diet in gastric cancer. Lancet Oncol. 2001;2(2):88–94. doi:10.1016/S1470-2045(00)00225-4
5. Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z. Risk factors for gastric cancer: a systematic review. Asian Pac J Cancer Prev. 2018;19(3):591–603. doi:10.22034/APJCP.2018.19.3.591
6. Lim H, Cho G, Kim S. Evaluation of nutrient intake and diet quality of gastric cancer patients in Korea. Nutr Res Pract. 2012;Jun(3):213–220. doi:10.4162/nrp.2012.6.3.213
7. Campbell PT, Sloan M, Kreiger N. Dietary patterns and risk of incident gastric adenocarcinoma. Am J Epidemiol. 2008;167(3):295–304. doi:10.1093/aje/kwm294
8. Willett W. Nutritional Epidemiology.
9. Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: the national health interview surveys, 1987 and 1992. J Nutr. 2004;134(7):1793–1799. doi:10.1093/jn/134.7.1793
10. Castello A, de Larrea NF, Martin V, et al. High adherence to the Western, Prudent, and Mediterranean dietary patterns and risk of gastric adenocarcinoma: MCC-Spain study. Gastric Cancer. 2018;21:372–382. doi:10.1007/s10120-017-0774-x
11. Zamani N, Hajifaraji M, Malekshah AF, et al. A case-control study of the relationship between gastric cancer and meat consumption in Iran. Arch Iran Med. 2013;16(5):324–329.
12. Kim MK, Sasaki S, Sasazuki S, Tsugane S. Prospective study of three major dietary patterns and risk of gastric cancer in Japan. Int j Cancer. 2004;110:435–442. doi:10.1002/ijc.20132
13. Tayyem RF, Abu-Mweis SS, Bawadi HA, Agraib L, Bani-Hani K. Validation of a food frequency questionnaire to assess macronutrient and micronutrient intake among Jordanians. J Acad Nutr Diet. 2014;114(7):1046–1052. doi:10.1016/j.jand.2013.08.019
14. Takruri H, Al-Ismail K, Tayyem R, Al-Dabbas M. Composition of Local Jordanian Food Dishes. Amman, Jordan: Dar Zuhdi; 2020.
15. Lee R, Nieman D. Nutritional Assessment. McGraw-Hill Education; 2012.
16. Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City project. Am J Epidemiol. 1985;121(1):91–106. doi:10.1093/oxfordjournals.aje.a113987
17. Thompson JK, Jarvie GJ, Lahey BB, Cureton KJ. Exercise and obesity: etiology, physiology, and intervention. Psychol Bull. 1982;91:55–79. doi:10.1037/0033-2909.91.1.55
18. Miao P, Guan L. Association of dietary cholesterol intake with risk of gastric cancer: a systematic review and meta-analysis of observational studies. Front Nutr. 2021;8:722450. doi:10.3389/fnut.2021.722450
19. Al-Awwad N, Allehdan S, Al-Jaberi T, et al. Dietary and lifestyle factors associated with gastric and pancreatic cancers: a case-control study. Prev Nutr Food Sci. 2021;26(1):30–39. doi:10.3746/pnf.2021.26.1.30
20. Bertuccio P, Edefonti V, Bravi F, et al. Nutrient dietary patterns and gastric cancer risk in Italy. Cancer Epidemiol Biomarkers Prev. 2009;18(11):2882–2886. doi:10.1158/1055-9965.EPI-09-0782
21. Pham TM, Fujino Y, Kikuchi S, Tamakoshi A, Matsuda S, Yoshimura T. Dietary patterns and risk of stomach cancer mortality: the Japan collaborative cohort study. Ann Epidemiol. 2010;20:356–363. doi:10.1016/j.annepidem.2010.02.002
22. Ward MH, Lopez-Carrillo L. Dietary factors and the risk of gastric cancer in Mexico City. Am J Epidemiol. 1999;149:925–932. doi:10.1093/oxfordjournals.aje.a009736
23. Du S, Li Y, Su Z, et al. Index-based dietary patterns in relation to gastric cancer risk: a systematic review and meta-analysis. Br J Nutr. 2020;123:964–974. doi:10.1017/S0007114519002976
24. Moazzen S, van der Sloot KWJ, Vonk RJ, de Bock GH, Alizadeh BZ. Diet quality and upper gastrointestinal cancers risk a meta-analysis and critical assessment of evidence quality. Nutrients. 2020;12:1863. doi:10.3390/nu12061863
25. Zhang Z, Xu G, Yang J, Liu X, Liu X. Dietary fiber intake reduces risk for gastric cancer: a meta-analysis. Gastroenterology. 2013;145:113–120. doi:10.1053/j.gastro.2013.04.001
26. Silvera SAN, Mayne ST, Risch HA, et al. Principal component analysis of dietary and lifestyle patterns in relation to risk of subtypes of esophageal and gastric cancer. Ann Epidemiol. 2011;21(7):543–550. doi:10.1016/j.annepidem.2010.11.019
27. Bertuccio P, Rosato V, Andreano A, et al. Dietary patterns and gastric cancer risk: a systematic review and meta-analysis. Ann Oncol. 2013;24:1450–1458. doi:10.1093/annonc/mdt108
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
