Back to Journals » Hepatic Medicine: Evidence and Research » Volume 15
Medicinal Plants Used for the Management of Hepatitis Over the Past 15 Years in Ethiopia: A Systematic Review
Authors Aschale Y , Tegegne BA , Yihunie W
Received 12 January 2023
Accepted for publication 1 March 2023
Published 9 March 2023 Volume 2023:15 Pages 11—19
DOI https://doi.org/10.2147/HMER.S402975
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gerry Lake-Bakaar
Yibeltal Aschale,1 Bantayehu Addis Tegegne,2 Wubetu Yihunie2
1Department of Medical Laboratory Sciences, Debre Markos University, Debre Markos, Ethiopia; 2Department of Pharmacy, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Yibeltal Aschale, Tel +251910962733, Email [email protected]
Background: Treatment of human and animal ailments using botanical sources has obtained significant attention in Ethiopia. The compounds available in plants comprise a plentiful source of bioactive ingredients able to treat many complications. The review aimed to present an updated list of plants used for managing hepatitis over the past 15 years in Ethiopia.
Methods: Systematic, comprehensive search was undertaken from electronic databases (PubMed, Google Scholar, Science Direct, and Scopus) between September 01 and October 15, 2022, using standard search terms. Original researches carried out in Ethiopia, written and published in English between January 01/2007 and December 31/2021, and reported hepatitis as a disease treated by medicinal plants were included in the review. Plants beyond the list of Ethiopian and Eritrean floral were excluded. Data were extracted from texts and tables of original papers on a Microsoft Excel. Quality was assessed by applying the Joanna Briggs Institute Critical Appraisal Checklist.
Results: A total of 317 papers were obtained from the database search. After removing duplicates and screening, 15 articles fit the inclusion criteria and selected for final review. Of the 24 plants identified, 35.7% were herbs. Leaf and root (35.7% each) were the predominant plant parts used for remedy preparation. Combined use of leaf and root comprised 10.7%. The families Apocynaceae, Asteraceae, Euphorbiaceae, Cucurbitaceae, and Fabaceae comprise the highest number of plant species. About 89.3% of remedies were administered orally.
Conclusion: The majority of plants belong to herbs and the frequently used plant parts are leaf and roots. Evidence generated from the present review indicated that lots of plants have been used to manage hepatitis. Moreover, the findings could serve as preliminary information to formulate new drugs acting against hepatitis. Therefore, it is desirable for scholars to recognize, document, and keep plants and the associated knowledge appropriately.
Keywords: hepatitis, medicinal plant, Ethiopia
Introduction
Herbal medicine has obtained great attention in Ethiopia and continues to be the source to relieve many human and animal ailments.1 It is believed that the oral and/or written knowledge has been conveyed from a skilled grandparent, parent, or elder in general to the next generation. About 6500–7000 plant species are available in Ethiopia, of which 12–19% are endemic, making the country among the most diverse floristic countries in the world.2,3 It is estimated that about 80% of the Ethiopian population and 60% of the world population depend on traditional medicine to treat a variety of health problems. About 25% of the current medicines have compounds from medicinal plants.4
The high demand for using traditional medicine is mainly attributed to its minimal cost and ease of accessibility, in addition to serving as a source of knowledge for plant-based synthetic drugs. In Ethiopia, high achievement in the utilization of traditional medicine is believed to be due to a high diversity of plants, rich cultures, beliefs, and language.5 Sometimes it becomes the only available and affordable option, especially in remote or underserved areas. Ayalew et al 2022 reported the ethnomedicinal uses, biological activities, and chemical constituents of Ethiopian endemic medicinal plants.6 The global scientific community ranked plants to be investigated and used for human and animal disease treatment. Of which, neem tree (Azadirachta indica) was included in the top ten lists and referred to as the tree of the 21st century or miracle tree because of its multipurpose uses and excellent therapeutic potential for all diseases. This tree contains ingredients that have anti-hepatitis activity.7,8
Emerging infectious diseases remain to impose a threat on humans. Of which, viral disease is one of the most life threatening challenging the survival of human beings on earth, followed by bacterial and parasitic diseases.9,10 Hepatitis is an inflammation of the liver tissue. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. Some people or animals with hepatitis have no symptoms. Others may develop yellow discoloration of the skin, whites of the eyes, vomiting, and abdominal pain. The common causes of hepatitis are the viruses hepatovirus A, B, C, D, and E. Other common noninfectious causes include heavy alcohol use, certain medications, toxins, and autoimmune diseases. More than one million deaths are recorded due to hepatitis annually.11,12
Screening of plants for the existing bioactive constituents is crucial to discovering and formulating promising drugs that cure hepatitis. Therefore, new drugs of plant origin are urgently needed and drug screening efforts should be encouraged. Despite the excessive role of medicinal plants in primary health care, little work has been conducted in Ethiopia to properly recognize and preserve plants and the associated facts. Therefore, the present review aimed to present an updated list of plants used for managing hepatitis over the past 15 years in Ethiopia.
Methods and Materials
Search Design and Strategy
International electronic databases (PubMed, Google Scholar, Scopus, and Science direct) were systematically searched for published articles about medicinal plants utilized for the treatment of hepatitis over the last 15 years in Ethiopia. All searches were limited to articles published in English between January 01/2007 and December 31/2021. The last search was done on December 31/2021. The search was conducted between September 01 and October 15, 2022. This review has used the Preferred Reporting of Systematic Reviews and Meta-Analysis (PRISMA) guidelines13 to assure scientific rigor. Common search terms were “medicinal plants”, “human ailment”, and “Ethiopia”. These search terms were used separately and in combination using Boolean operators like “OR” or “AND”. The reference lists of included studies were screened for additional eligible studies. Grey literature and unpublished data were not included. Search results from different databases were exported to EndNote and then combined after the removal of duplicates.
Procedure for Study Selection
Two researchers (YA, WY) were involved in study selection. After removing duplicate articles, they performed initial screening by reading titles and abstracts of each article for eligibility. Then, the full text of the eligible articles was assessed for inclusion in the review. Articles that did not report the outcome of interest in the full text were removed. Any discrepancy between researchers in inclusion decisions was resolved via discussion. If still not resolved and additional clarification is required, the primary author of eligible studies was contacted via email at least two times.
Study Selection Criteria
Inclusion Criteria
Original articles conducted in Ethiopia, published in English between January 01/2007 and December 31/ 2021, contain full ethnobotanical information (family name, scientific name, local name, growth form, plant parts used, and route of administration), and reported hepatitis as a disease treated by traditional healers were included in the review.
Exclusion Criteria
Studies without a full text were excluded after contacting the primary author at least two times and no response at all through email. Studies that include only plants of livestock usage were excluded. Plants which are beyond the list of Ethiopian and Eritrean flora were excluded.14
Data Extraction
Two researchers (YA, BA) extracted all the required data (scientific, family, and local names, growth forms of plants, plant parts used, methods of preparation, and route of administration) independently using a standardized data extraction form adapted from the JBI data extraction format in a Microsoft Excel spreadsheet. Data were extracted from text and tables. If there was a discrepancy between investigators on the data to be extracted, it was resolved via discussion or a third researcher. If still not resolved and additional clarification is required, the primary author of the included studies was contacted via email at least two times. The collected data were analyzed using descriptive statistics to calculate frequency and percentage.
Assessment of Methodological Quality
Two researchers (WY, BA) independently assessed the quality of each original study using a standard quality assessment tool adapted from the JBI Critical Appraisal Checklist. The methodological quality of all 15 papers (Table 1) was therefore checked by applying the Joanna Briggs Institute Critical Appraisal Checklist15 prior to inclusion. This tool has nine quality items that focus on sample size, methods used for identification of the outcome, and statistical analysis. If disagreement between two assessors occurs, it is resolved by discussion and by contacting the primary author of the included studies via email. Articles assessed with a score of ≥6 out of 9 quality items were considered high quality.
 |
Table 1 Characteristics of the Studies Included in This Systematic Review |
Data Processing and Analysis
The data extracted from Excel spreadsheets were imported to SPSS version-24 software and analyzed using descriptive statistics to calculate mean, range and percentage. The data synthesized were provided from the included studies regarding the frequency of the identified plant family and species, growth form of the plant, plant part used and route of administration.
Results
The search for international databases provided a total of 317 published studies. After the removal of duplicates, 128 remained. Of these, 70 studies were discarded after reading their titles and abstracts since they did not meet the inclusion criteria. Of the 58 studies assessed for eligibility, 43 studies were discarded due to provision of incomplete information. Finally, 15 studies met the inclusion criteria and were selected for final review (Figure 1). In the current review, 24 plants (distributed over 17 families) were identified to be used by the traditional healers to manage hepatitis. The detailed information of each plant recorded from the included original papers is available in Table 2.16–30
 |
Table 2 List of Plants Used for the Management of Hepatitis Over the Past 15 Years |
 |
Figure 1 Flowchart of study selection for medicinal plants used for the treatment of hepatitis in Ethiopia. |
Commonly Used Families and Plant Species
The family Apocynaceae, Asteraceae, Euphorbiaceae, Cucurbitaceae, Solanaceae, and Fabaceae had the relatively highest number of plant species. Acokanthera schimperi, Cucumis species, Vernonia species, and Acacia tortilis were some of the commonly used plant species (Table 2).
Growth Forms of Medicinal Plants and Plant Parts Used
Of the medicinal plants identified, the majority of them were herbs (35.7%), followed by shrubs (32.1%), trees (25%), and climbers (7.2%) (Figure 2). The commonly used plant parts were leaf and root (35.7% each) followed by a combination of roots and leaves (10.7%) (Figure 3).
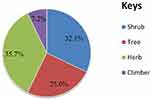 |
Figure 2 Growth forms of medicinal plants used for the treatment of hepatitis. |
 |
Figure 3 Plant parts used for the treatment of hepatitis in Ethiopia. |
Method of Preparation and Route of Administration
Traditional medicinal practitioners use simple compounding procedures like drying, crushing, concoction, and decoction, and remedies are given using honey and water as an additive and/or solvent (Table 2). They prefer the oral route as the best administration route (89.3%). Other routes, even if minimal, were also used to administer remedies (dermal=7.1%, nasal=3.6%) (Figure 4).
 |
Figure 4 Route of administration of medicinal plants used for the treatment of hepatitis. |
Discussion
Ethnobotany is a useful scheme for pharmaceutical research and novel drug discovery. Claimed medicinal plants play a great role in this purpose. Their outstanding therapeutic effect along with ease of formulation results in their widespread usage in the management of infectious and non-infectious diseases. The reasons for choosing drugs from herbal/botanical sources over traditional/conventional drugs are their minimal side effects, efficacy and multi-target activities. The current review identified 24 plant species having been applied by traditional healers to manage hepatitis. This shows the level of knowledge existing in the diverse communities of Ethiopia. High species diversity of plants was observed, which might be due to differences in climate in Ethiopia. The family Apocynaceae, Asteraceae, Euphorbiaceae, Cucurbitaceae, Solanaceae, and Fabaceae had the relatively highest number of plant species. A study done in Spain and Korea revealed the dominance of Family Asteraceae.31,32 Another study conducted in the Hawassa Zuria district33 showed the dominance of the family Fabaceae, which might be attributed to their extensive distribution and abundance and plenty of bioactive ingredients.
According to this review, most plants belong to herbs, followed by shrubs and trees. Other studies conducted elsewhere in Ethiopia also showed the dominance of herbs.33–38 Herbs are periodical that require storing and/or farming in a restricted area. However, shrubs are not periodical (easily available throughout the year) and do not need storage. Use of shrubs and trees in the preparation of remedies is therefore beneficial over herbs. Leaf and root (alone and in combination) were the predominant plant parts used for remedy preparation. This was in agreement with other research work.33,39,40 The frequent use of leaves in most preparations might be due to the presence of bioactive compounds in variety and abundance, ease of accessibility and formulation into different dosage forms. Collecting leaves is preferable for mother plant survival than other plant parts (root and stem) which might pose a serious threat. Removal of up to 50% of plant leaves does not significantly affect their growth. However, root and stem harvesting if not performed carefully, may cause harmful effect on the mother plant.
Simple methods (crushing, powdering, pounding, and wetting) were commonly employed to prepare remedies. This might be due to poor training and lack of processing equipment which are important for drug formulation processes. Similar studies conducted earlier reported crushing, grinding, or pounding as the most common remedy preparation.41–43 Lulekal et al44 reported boiling as the most frequently used method of remedy preparation. Honey and water, which are vital for improving odor, solubility, and taste, were commonly used during remedy preparation. Water has a high ability to extract different phytochemicals from plant origins. This finding is consistent with other studies conducted elsewhere.16,40,45,46
As shown in Figure 4, practitioners prefer the oral route as a principal mode of administration. Nasal and dermal routes were minimal. This might be due to the relative easiness of the oral route, inability to administer preparations via parenteral ways, and fear of associated adverse effects. This finding agrees with a study conducted in Dega Damot District,45 Tigray Region,23 Hawassa Zuria district,33 Addis Ababa,47 Gemad District,48 and Kenya.49 However, other studies conducted in Southern Ethiopia revealed that most medicinal plant preparations were administered cutaneously.50 Eshete et al20 reported that both oral and dermal routes allow the rapid physiological reaction of remedies to agents of diseases to increase potency. Depending on the type of ailment treated, patients are instructed to be careful during and after intake of remedies. They might be restricted from drinking tella, tej, and milk and/or eating meat and eggs as such practices are believed to interfere with, potency of the remedies. The action of these medicinal plants is generally supposed to have a direct effect on the virus particle and is able to inhibit cell-to-cell spread.
Limitations of the Study
This systematic review has considered only studies conducted in English, which may have restricted some reports/articles from being included. This systematic review also did not summarize the dosage schedule of the remedies given as it was not reported by the original studies. Moreover, the restriction in the study period might exclude studies conducted earlier.
Conclusions and Recommendations
In this ethnomedicinal review, a total of 24 plants, belonging to 17 families, have been identified to be used for managing hepatitis. Though the majority of the remedies are prepared from leaves, it does not cause the reduction of plant biodiversity. Oral route is the principal mode of remedy administration. Evidence generated from the present review could serve as preliminary information to formulate new drugs that can treat hepatitis. Efforts should be made to protect these important plants using any available means. Therefore, it is desirable for scholars to recognize, document, and keep plants and the associated knowledge appropriately and test for safety and efficacy.
Data Sharing Statement
The datasets used and/or analyzed during the current study are included in this article.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Maki H. Medicinal crops in Ethiopia: current status and future potentials. Japan Assoc Int Collab Agric Forest. 2008;5(2):258–273.
2. Bekele E. Study on Actual Situation of Medicinal Plants in Ethiopia. Addis Ababa, Ethiopia: Japan Association for International Collaboration of Agriculture and Forestry; 2007.
3. Tesfahuneygn G, Gebreegziabher G. Medicinal plants used in traditional medicine by Ethiopians: a review article. J Respir Med Lung Dis. 2019;4(1):1–3.
4. Fentahun Y, Eshetu G, Worku A, Abdella T. A survey on medicinal plants used by traditional healers in Harari regional State, East Ethiopia. J Med Plants. 2017;5(1):85–90.
5. Balick MJ, Cox PA. Plants, People, and Culture: The Science of Ethnobotany. Garland Science; 2020.
6. Ayalew H, Tewelde E, Abebe B, Alebachew Y, Tadesse S. Endemic medicinal plants of Ethiopia: ethnomedicinal uses, biological activities and chemical constituents. J Ethnopharmacol. 2022;293:115307. doi:10.1016/j.jep.2022.115307
7. Fernandes JB. Secondary metabolism as a measurement of efficacy of botanical extracts: the use of Azadirachta indica (Neem) as a model. Insecticides. Adv Integr Pest Manage. 2012;2012:367.
8. Paul R, Prasad M, Sah NK. Anticancer biology of Azadirachta indica L (neem): a mini review. Cancer Biol Ther. 2011;12(6):467–476. doi:10.4161/cbt.12.6.16850
9. World Health Organization. Viral vaccines and antiviral drugs. Rep Sci Group WHO. 1983;693:5–38.
10. Howard CR, Fletcher NF. Emerging virus diseases: can we ever expect the unexpected? Emerg Microbes Infect. 2012;1:1–11. doi:10.1038/emi.2012.47
11. Maddrey WC, Boitnott JK, Bedine MS, Weber FL, Mezey E, White RI. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–199. doi:10.1016/0016-5085(78)90401-8
12. McFarlane IG. Definition and classification of autoimmune hepatitis. Semin Liver Dis. 2002;22(4):317–324. doi:10.1055/s-2002-35702
13. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi:10.1016/j.jclinepi.2009.06.006
14. Hedberg I, Edwards S. Flora of Ethiopia and Eritrea. Vol. 8. Addis Ababa, Ethiopia and Uppsala, Sweden: Uppsala University; 2009.
15. Joanna Briggs Institute. Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data. Adelaide: Joanna Briggs Institute; 2017.
16. Giday M, Teklehaymanot T, Animut A, Mekonnen Y. Medicinal plants of the Shinasha, Agew-awi and Amhara peoples in northwest Ethiopia. J Ethnopharmacol. 2007;110(3):516–525. doi:10.1016/j.jep.2006.10.011
17. Tedila H, Dida G. Ethnobotanical study of traditional medicinal plants used for treatment of human and livestock ailments by traditional healers in Goba woreda, Bale zone, Oromia, South East Ethiopia. J Natural Sci Res. 2019;9:10.
18. Chekole G, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants in the environs of Tara-gedam and Amba remnant forests of Libo-Kemkem District, Northwest Ethiopia. J Ethnobiol Ethnomed. 2015;11(1):4. doi:10.1186/1746-4269-11-4
19. Andarge E, Shonga A, Agize M, Tora A. Utilization and conservation of medicinal plants and their associated indigenous knowledge (IK) in Dawuro Zone: an ethnobotanical approach. Int J Med Plants Res. 2013;4(3):330–337.
20. Eshete MA, Kelbessa E, Dalle G. Ethnobotanical study of medicinal plants in Guji agro-pastoralists, Blue Hora District of Borana Zone, Oromia region, Ethiopia. J Med Plants Stud. 2016;4(2):170–184.
21. Abera B. Medicinal plants used in traditional medicine by Oromo people, Ghimbi District, Southwest Ethiopia. J Ethnobiol Ethnomed. 2014;10(1):40. doi:10.1186/1746-4269-10-40
22. Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5(1):28. doi:10.1186/1746-4269-5-28
23. Teklay A, Abera B, Giday M. An ethnobotanical study of medicinal plants used in Kilte Awulaelo District, Tigray Region of Ethiopia. J Ethnobiol Ethnomed. 2013;9(1):65. doi:10.1186/1746-4269-9-65
24. Belayneh A, Asfaw Z, Demissew S, Bussa NF. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Wereda, Eastern Ethiopia. J Ethnobiol Ethnomed. 2012;8(1):42. doi:10.1186/1746-4269-8-42
25. Osman A, Sbhatu DB, Giday M. Medicinal plants used to manage human and livestock ailments in Raya Kobo District of Amhara Regional State, Ethiopia. Evid Based Complement Altern Med. 2020;2020:1–19. doi:10.1155/2020/1329170
26. Shimels A, Atinafu K, Akalu M, Getachew M. Ethnobotanical study of medicinal plants used by agro pastoralist Somali people for the management of human ailments in Jeldesa Cluster, Dire Dawa Administration, Eastern Ethiopia. J Med Plants Res. 2017;11(9):171–187. doi:10.5897/JMPR2016.6292
27. Amare F, Getachew G. An ethnobotanical study of medicinal plants in Chiro district, West Hararghe, Ethiopia. Afri J Plant Sci. 2019;13(11):309–323. doi:10.5897/AJPS2019.1911
28. Tuasha N, Petros B, Asfaw Z. Medicinal plants used by traditional healers to treat malignancies and other human ailments in Dalle District, Sidama Zone, Ethiopia. J Ethnobiol Ethnomed. 2018;14(1):1–21. doi:10.1186/s13002-018-0213-z
29. Tsegay B, Mazengia E, Beyene T. Diversity of medicinal plants used to treat human ailments in rural Bahir Dar, Ethiopia. Asian J Forest. 2019;3(2):63.
30. Assefa B, Megersa M, Jima TT. Ethnobotanical study of medicinal plants used to treat human diseases in Gura Damole District, Bale Zone, Southeast Ethiopia. Asian J Ethnobiol. 2021;4(1). doi:10.13057/asianjethnobiol/y040105
31. Gorka M. Medicinal plants traditionally used in the northwest Spain. J Ethnopharmacol. 2013;4(9):01–22.
32. Song MJ, Kim H, Heldenbrand B, Jeon J, Lee S. Ethnopharmacological survey of medicinal plants in Jeju Island, Korea. J Ethnobiol Ethnomed. 2013;9:1–8. doi:10.1186/1746-4269-9-48
33. Tefera BN, Kim Y-D. Ethnobotanical study of medicinal plants in the Hawassa Zuria District, Sidama zone, Southern Ethiopia. J Ethnobiol Ethnomed. 2019;15(1):25. doi:10.1186/s13002-019-0302-7
34. Mekuanent T, Zebene A, Solomon Z. Ethnobotanical study of medicinal plants in Chilga District, Northwestern Ethiopia. J Natural Remedies. 2015;15(2):88–112. doi:10.18311/jnr/2015/476
35. Seifu T, Asres K, Gebre-Mariam T. Ethnobotanical and ethnopharmaceutical studies on medicinal plants of Chifra district, Afar region, North Eastern Ethiopia. Ethiop Pharma J. 2004;24(1):41–58.
36. Amsalu N. An Ethnobotanical Study of Medicinal Plants in Farta Wereda. South Gonder Zone of Amhara Region Ethiopia: Plant Biology and Biodiversity Management. Addis Ababa: Addis Ababa University; 2010.
37. Behailu E. Ethnobotanical Study of Traditional Medicinal Plants of Goma Woreda, Jima Zone of Oromia Region, Ethiopia [Master’s Thesis], Addis Ababa University; 2010.
38. Agisho H, Osie M, Lambore T. Traditional medicinal plants utilization, management and threats in Hadiya Zone, Ethiopia. J Med Plants. 2014;2(2):94–108.
39. Abubakar M, Musab A, Ahmeda M, Hussaini IM. The perception and practice of traditional medicine in the treatment of cancers and inflammations by the Hausa and Fulani tribes of Northern Nigeria. J Ethno Pharmacol. 2007;111:625–629. doi:10.1016/j.jep.2007.01.011
40. Tora A, Heliso T. Assessment of the indigenous knowledge and use of traditional medicinal plants in Wolaita Zone, southern Ethiopia. Int J Med Plants Natural Prod. 2017;3(1):16–22.
41. Amenu E. Use and Management of Medicinal Plants by Indigenous People of Ejaji Area (Chelya Wereda) West Shewa, Ethiopia: An Ethnobotanical Approach [M.Sc. Thesis]. Addis Ababa, Ethiopia: Addis Ababa University; 2007.
42. Hunde D, Asfaw Z, Kelbessa E. Use of traditional medicinal plants by people of ‘Boosat’sub district, Central Eastern Ethiopia. Ethiop J Health Sci. 2006;16(2):141–155.
43. Girmay T, Teshome Z. Assessment of traditional medicinal plants used to treat human and livestock ailments and their threatening factors in Gulomekeda District, Northern Ethiopia. Int J Emerging Trends Sci Technol. 2017;4(4):5061–5070. doi:10.18535/ijetst/v4i4.03
44. Lulekal E, Kelbessa E, Bekele T, Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu District, southeastern Ethiopia. J Ethnobiol Ethnomed. 2008;4:10. doi:10.1186/1746-4269-4-10
45. Wubetu M, Abula T, Dejenu G. Ethnopharmacologic survey of medicinal plants used to treat human diseases by traditional medical practitioners in Dega Damot district, Amhara, Northwestern Ethiopia. BMC Res Notes. 2017;10(1):157. doi:10.1186/s13104-017-2482-3
46. Regassa R. Assessment of indigenous knowledge of medicinal plant practice and mode of service delivery in Hawassa city, southern Ethiopia. J Med Plants Res. 2013;7(9):517–535.
47. Birhan W, Giday M, Teklehaymanot T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomed. 2011;7:1–7. doi:10.1186/1746-4269-7-39
48. Mesfin K, Tekle G, Tesfay T. Ethnobotanical study of traditional medicinal plants used by indigenous people of Gemad District, Northern Ethiopia. J Med Plants Stud. 2013;1(4):32–37.
49. Mbwayo AW, Ndetei DM, Mutiso VN, Khasakhala LI. Traditional healers and provision of mental health services in cosmopolitan informal settlements in Nairobi, Kenya. Afri J Psychiatr. 2013;16(2):134–140. doi:10.4314/ajpsy.v16i2.17
50. Giday M, Asfaw Z, Woldu Z. Ethnomedicinal study of plants used by Sheko ethnic group of Ethiopia. J Ethnopharmacol. 2010;132(1):75–85. doi:10.1016/j.jep.2010.07.046
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
