Back to Journals » Integrated Pharmacy Research and Practice » Volume 9
Medication-Related Needs and Humanistic Impact of Patient-Centered Pharmaceutical Care at University of Gondar Comprehensive Specialized Hospital, North-West Ethiopia
Authors Abdela OA , Abay E, Beka S, Mengistie B, Ayalew MB
Received 18 June 2020
Accepted for publication 24 September 2020
Published 6 November 2020 Volume 2020:9 Pages 229—242
DOI https://doi.org/10.2147/IPRP.S268248
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Ousman Abubeker Abdela,1 Enathun Abay,2 Senait Beka,3 Biset Mengistie,2 Mohammed Biset Ayalew1
1Department of Clinical Pharmacy, School of Pharmacy, College of Medicine and Health Science College, University of Gondar, Gondar, Ethiopia; 2School of Pharmacy, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia; 3Axum Pharmacy, Addis Ababa, Ethiopia
Correspondence: Ousman Abubeker Abdela Tel +251-912-02-3692
Fax + 251-058-114 1240
Email [email protected]
Purpose: To assess patients’ medication-related needs and the humanistic impact of patient-centered pharmaceutical care.
Patients and Methods: A hospital-based cross-sectional study was conducted using self-administered structured questionnaires from February 4 to 28, 2019, on patients attending ambulatory care for chronic non-communicable diseases at the University of Gondar specialized teaching hospital, North-west Ethiopia. Data were entered to SPSS version 22 for analysis. Descriptive statistics was used to describe the socio-demographic characteristics and medication-related needs of study participants. Independent sample t-test and one-way ANOVA analysis were performed to check for possible associations between dependent and independent variables.
Results: Information about what to do if patients missed doses and the potential side-effects or abnormal conditions caused by the prescribed medicines were not explained for most of the 425 patients studied. The majority of the study participants reported that they felt worried about adverse medicine effects, drug interactions, and long-term medicine use. Patients who were older than 50 or those receiving two or more medications were less satisfied with the effect of their medicine as compared to younger ones and those on monotherapy, respectively. People who were illiterate or had attended only primary schools thought that they received less disease and medicine information from health professionals than people who attended tertiary education.
Conclusion and Recommendation: Most of the participants were particularly unhappy with the amount of information received about side-effects and what to do if doses were missed. Special emphasis should be given to patients with a low level of education as they were not satisfied with medicine and disease information obtained from health professionals, experienced more psychological impacts of medicine use, and had poor overall quality-of-life.
Keywords: Ethiopia, pharmaceutical care, humanistic outcome, medication-related needs
Introduction
Pharmaceutical care is currently defined as “patient-centered practice in which the practitioner assumes responsibility for a patient’s medication-related needs and is held accountable for this commitment.”1 It is the practice that optimizes pharmaceutical treatments contributing to an improvement in HRQoL (humanistic outcome of therapeutic relevance) which can be reported directly by the patient as a patient-reported outcome (PRO) without requiring an interpretation of the response by others.2 It involves medication dispensing, providing medicines information, patient counseling, monitoring, parenteral nutrition preparation, adverse drug reaction monitoring, medication reconciliation, medicines’ protocol/guideline development, medical rounding with the healthcare team, and performing admission medication histories.3
 |
Figure 1 Participants overall quality-of-life for each domain of the PROMPT questionnaire. |
The Pharmacy profession continues to move towards being patient-centered because of an increase in health demand with a complex range of chronic medicines and poor adherence to medications.4 Pharmaceutical care philosophy requires all pharmacists to do their responsibilities to meet all of the patient’s drug-related needs through direct patient care and cooperation with other members of the healthcare system.5
Humanistic outcomes, also known as patients’ reported outcomes, involve the effect of treatment and pathology on the patient´s functional status, quality-of-life, and satisfaction with the particulars of their care.6 Quality-of-life is generally considered a multidimensional construct that includes physical, mental, and social functioning, as well as perceptions of general well-being. It has been a fundamental research topic in health, as its results are important to assess the effectiveness of care as well as to obtain social and health funding.7
Patient report outcomes (PROs) give us unique insights into how a therapy can affect a patient. Individuals with the exact same health status, diagnosis, or disease may have different perceptions about how they feel and function, as their ability to cope with limitations and disability and other factors can alter perceptions about satisfaction with life. PRO measures are important as they can lead to a medical science that is more focused on real benefits achievable for the patients.8
Ethiopia as a country is in a major economic transition, accompanied by changes with ways of life of its population. There is also an epidemiological transition in terms of diseases from infectious to non-communicable diseases (NCDs).9 People living with a chronic disease will experience chronic treatments and a profound life-changing experience which may impact all aspects of a patient’s life.10
There are inadequate studies on Ethiopian NCDs patients concerning medication-related needs and the humanistic impact of pharmaceutical care service. The current study aims at assessing patients’ medication-related needs and the humanistic impact of patient centred pharmaceutical care at the University of Gondar teaching and referral hospital, North-west Ethiopia.
Patients and Methods
Study Area and Period
This study was conducted at the University of Gondar teaching and referral hospital. It is a 680 bedded teaching hospital located 750 km North-west of Ethiopia. It has 21 ward rooms for inpatients. Based on the information from the hospitals’ managerial personnel, more than 18,000 people are being served per annum in the outpatient department section only. One out-patient department unit is responsible for delivering services to those patients with chronic non-communicable diseases including psychiatric disorders, diabetes mellitus, cardiovascular disorders, etc. At the department, each working day of a week has been scheduled for a follow-up service to those with particular diagnoses. The study was conducted from February 4–28, 2019.
Study Design
A hospital-based cross-sectional study was conducted.
Source Population
All adult patients who had chronic follow-up for management of their chronic non-communicable disease at the University of Gondar teaching and referral hospital.
Study Population
All adult patients who had chronic follow-up for management of their chronic non-communicable diseases and were available during the data collection period.
Inclusion and Exclusion Criteria
Inclusion Criteria
Ambulatory patients who had any type of non-communicable chronic disease.
Adults greater than 18 years old.
Patients who take one or more medication.
Exclusion Criteria
Those who were unwilling to participate.
Sample Size and Sampling Procedures
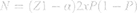
Sample size was determined using the formula for single population proportion by considering the prevalence of 50%; 95% level of confidence, and 5% margin of error. Therefore, sample size was determined as follows:
with a contingency of 10%. Total N=424, where
N is the number of patients to be sampled (sample size),
Z1-α is the Z-score at 95%=1.96, confidence interval is the proportion of patients, and δ is the margin of error.
Sampling Technique
The sampling technique employed in this study was a convenience sampling technique.
Data Collection Tools and Procedures
Data were collected from respondents using self-administered structured questionnaires. The questionnaire used is “Patient-reported outcomes measure of pharmaceutical therapy (PROMPT)”, a 16 item tool developed and validated by Sakthong et al11 with the intention of identifying patient’s medication-related needs and assessing the humanistic impact of patient-centered pharmaceutical care. It contains eight domains; a) Medicine and Disease Information (5 items); b) Medicine Effectiveness (2 items); c) Impacts of Medicines and Side-effects (1 item); d) Psychological Impacts of Medication Use (4 items); e) Convenience (1 item); f) Availability and Accessibility (1 item); g) Therapeutic Relationship with Healthcare Providers (1 item); and h) Overall QoL (1 item). All item responses used a 5-point Likert scale, and only these items were summed to calculate an overall PROMPT score for each domain. The questionnaire was translated to local Amharic language and pre-tested to identify potential problematic areas to any of the questions in 30 respondents having similar characteristics with the study subjects. Slight modification was made then. No language and/or understanding problem was encountered during actual data collection. Data were collected by three graduating class pharmacy students. The data collectors approached patients while they were at their waiting place and briefed them on the objective of the research. Then, they took informed consent from willing participants and administered the questionnaire.
Data Processing and Analysis
Data was entered to SPSS version 22 for analysis. Descriptive statistics were used to describe the sociodemographic characteristics and medication-related needs of study participants. ANOVA with Post-hoc test was used to check for possible associations between dependent and independent variables. In performing the statistical analysis, association was declared if P-value<0.05 with 95% CI.
Scoring for Domains
Item score ranges from 1–5, with higher scores indicating better QoL. The domain scores of PROMPT-QoL range from 0–100, where higher score indicates better QoL. They were calculated using the following formula: Domain score=100*(observed score-minimum domain score)/(maximum domain score-minimum domain score). For example, supposing a patient rated level 4 for all three items of Overall QoL domain. Thus, his/her score for this domain was 75, which was calculated from 100*(12–3)/(15–3). Each domain score was Interpreted as the following; 0–25=low, 25–50=fair-to-moderate, 50–75=moderate-to-good, 75–100=good-to-excellent.
Study Variables
Independent Variables
Socio-demographic variables including Age, Sex, marital status, education,
disease condition, and
number of medication.
Dependent Variables
Medication-related need. and
quality-of-life.
Ethical Consideration
All aspects of the study including the verbal informed consent were approved by the institutional review board (IRB) of the school of pharmacy, College of Medicine and Health Science, University of Gondar. The study is also in compliance with the Declaration of Helsinki.
Verbal informed consent was obtained from the respondents for the observation. Besides, confidentiality of the information was strictly maintained during data collection and the data analysis process. Each questionnaire was assigned a study identification number. Respondents were also informed that their information was used anonymously. In addition, the data collection instrument does not use personal identifiers so the privacy of each respondent is kept. Furthermore the data collected from each patient were kept confidential and used strictly for the purpose of the study only.
Results
A total of 424 patients participated in this study, 250 (59%) of whom were females. Two hundred and sixty-eight (63.2%) study participants were married. Illiteracy was recorded for 170 (40.1%) participants. Diabetes mellitus, psychiatric disorders, and hypertension were the top most frequent diagnoses documented in this study (see Table 1).
 |
Table 1 Socio-Demographic Characteristics and Clinical Data of Study Participants at UoGSRH |
Slightly more than 80% of participants responded that they received much or very much information about indications for treating their disease or relieving the symptoms they had and how to use their medicine (individual doses, frequency, before or after food and treatment course, including storage). However, 351 (82.8%) participants did not receive any information or received little information about what to do if doses are missed. Similarly, information about “side effects or abnormal conditions which would possibly be caused by their medicines, including how to resolve them” was not provided at all or the information given was little for 301 (71%) of participants.
Participants’ were also asked to grade their satisfaction with the effects of medicine use on alleviating symptoms. Accordingly, 370 (72.4%) participants rated their satisfaction as “very much” or “much”. An almost similar number of patients rated their satisfaction with regard to the effects their medicines had on managing their disease.
The impact of medicine usage or the side-effects derived from the medicine they use on working, study, household chores, hobbies, or socializing with friends or relatives was also assessed. Accordingly, 281 (66.2%) participants rated that their medicines and side-effects affected them “very much” and “much”.
With regard to the psychological impacts of medicine use, 322 (76%) study participants answered “bored very much” or “bored much” for the question “do you feel bored or uncomfortable for using your medicines regularly and strictly every day?”. Similarly, 75.2%, 40.1%, and 59.4% of participants answered “worried very much” when asked “Do you feel worried or afraid of medicines interacting with each other?”, “Do you feel worried or afraid of using your medicines for a long time or for life?”, and “Do you feel worried or afraid of adverse medicine effects, eg, allergies or damages to the liver, kidneys, or other organs?,” respectively.
Study participants were also asked to rate the convenience for use of the medicine they were using. Hence, 271 (64%) responders rated either “convenient much” or “convenient very much”. The problem about medicine expenses (eg, Medicine costs, travel fares, to treat their disease) was also assessed. More than one-third (160; 37.7%) of participants never faced availability and accessibility problem and 171 (40.3%) had little problem. Assessment of the therapeutic relationship participants had with their doctors, pharmacists, and nurses revealed that 326 (76.9%) participants rated “much” or “very much” for the question “Do you think the doctor, pharmacist, or nurse has friendly manners and give you an opportunity to ask questions about your medicines?” Finally, participants were asked how their medicine made live their life. Accordingly, 293 (69.1%) rated their response as “very much improved” and “much improved,” indicating that significantly more than two-thirds of participants believed the medicine they use has improved their overall quality-of-life (see Table 2).
 |
Table 2 Response of Participants to Patient-Reported Outcomes Measure of Pharmaceutical Therapy for Quality-of-Life (PROMPT-QoL) Questionnaire at UoGSRH |
Measurement of quality-of-ife of study participants for each of the eight domains of PROMPT-QoL questionnaire revealed that “moderate to good” quality-of-life was recorded for more than 50% of study subjects for three domains; satisfaction with the effect of medicines use, convenience of medicine use, and therapeutic relationship with doctors, pharmacists, or nurses. On the other hand, while 60.8% of participants had “moderate to good” overall quality-of-life for medicine use only, 6.8% of the participants had “good to excellent“ overall QoL for medicine use (see Figure 1).
As indicated in Table 3, males claim that they received more medicine and disease information from doctors, pharmacists, or nurses as compared to females. Those aged <50 or receiving single medication are better satisfied with the medicine effects as compared to their counterparts. Patients taking a single medication have better overall quality-of-life than those taking two or more medications. As compared to people older than 50 years, younger patients reported that their medicines have lesser convenience for use. Patients on two or more medications are less worried about the psychological impacts of medicine use than those taking single medication.
 |
Table 3 Independent Sample t-test, Comparison of Domains of PROMPT-QoL Scores in Terms of Sex, Age, and Number of Medications |
People who are illiterate or have attended only primary schools think that they received less disease and medicine information from health professionals than people who attended tertiary education. Patients with a diagnosis of diabetes mellitus and thyroid disorder received more disease and medicine information and are more satisfied with the effect of medicine use than people with other diagnoses. Psychological impacts of medicine use are more pronounced in people who have secondary education or less as compared to those attending tertiary education. In terms of overall quality-of-life, people with thyroid disorder reported that their medicines make them live better, while illiterate patients reported less improvement in their life as compared to their counterparts. Table 4 shows the detailed one-way ANOVA with Dunnett’s Post-Hoc analysis result.
 |  |  |
Table 4 One-Way ANOVA for Comparison of Domains of PROMPT-QoL Scores in Terms of Level of Education, Marital Status, and Diagnosis of Participants |
Discussion
Medication plays a great role in the treatment and prevention of human illnesses. Pharmaceutical care, which is a patient-focused medicine therapy service, can maximize the benefits of medication therapy and improve health outcomes, by ensuring the rational use of medicine.12 A study conducted by Singhal et al13 reported that pharmaceutical care in the ambulatory setting can positively influence patient’s health outcome. In spite of this, patient-oriented pharmacy service is only a recent experience in Ethiopia. To the authors best knowledge this is the first study to examine the humanistic impact of patient-centred pharmaceutical care in the country.
The results of the current study showed that more than 90% of patients with non-communicable chronic illnesses (NCCIs) who have follow-up at UoGSRH reported that they received sufficient information about how to use their medicine and were explained about the indications for treating their disease or symptoms. However, what to do if they missed doses and the potential side-effects or abnormal conditions caused by the prescribed medicines were not explained for most of the patients with NCCIs in the hospital. In line with the result of the current study, Puspitasari et al14,15 reported that medicine counseling is mainly focused on giving information about medication administration while information related to medication safety including side-effects was overlooked.,
Even though satisfaction with the effect of medicine use was reported to be moderate and above for more than 70% of participants, most of the patients expressed that they were affected by the medicine use or the side-effects on work, study, household chores, hobbies, or socializing with friends or relatives. This may be because patients with chronic illnesses should take their medicine for lifelong and the chance of experiencing medicines side-effects will be high due to the accumulation of the medicine or its metabolite in the body. Medicines’ interactions that may occur when other medications are taken for acute illnesses may also enhance the chance of side-effects from the long-term medications. In addition, taking medicines for lifelong on a daily basis regardless of the situations that the patient is facing is sometimes inconvenient and may significantly affect work and social life. The high proportion of patients whose work and social life is affected by medicine use or its side-effects may also be attributed to the poor counseling practice of health professionals to explain about the possible side-effects or abnormal conditions caused by the prescribed medicines. This is supported by the fact that more than 70% of participants in the current study were reported to have received nothing or only a little bit of information about the side-effects or abnormal conditions possibly caused by their medicines. A similar result was reported by Erica et al16 that patients were dissatisfied with the information on whether the medicine had any side-effects, the risks of getting side-effects, and what to do about unwanted side-effects.
Regarding the psychological impact of medicine use, the majority of the study participants reported that they felt worried about adverse medicine effects, medicines’ interactions, and long-term medicine use. They also felt bored with taking medicines regularly and strictly every day. Health professionals, especially pharmacists, should explain about the potential side-effects and interactions from medicines prescribed and should counsel patients on how to address it if happened. Patients with NCCIs should also be counseled on the consequences of not taking medicines, to make them cope with the taking of their medicine lifelong. In addition, healthcare providers should assess for any barrier that may prevent patients from taking medicine regularly and take appropriate corrective measures to ensure that they are adherent to their medicine.
Availability and accessibility of medicine was not reported as such a serious problem by most of the participants in the current study. Less than 15% of study participants reported that they were concerned much or very much with the problem of medicine expenses, while more than three quarters reported that they were never or only a little bit bothered about this problem. This could be justified by the availability of health insurance to cover medical expenses of most of the patients, and medicines for some selected chronic diseases (eg, psychiatric illnesses) are distributed for free. Most of the patients think that their doctors, pharmacists, or nurses have friendly manners with them and give them an opportunity to ask questions about their medicines. This might be because people with chronic illnesses have frequent contacts with these health professionals who in turn make them familiar and friendly with them.
Patients who were older than 50 or those receiving two or more medications were less satisfied with the effect of their medicine as compared to younger ones and those who were on monotherapy, respectively. This could possibly be because older people mostly have a greater number of co-morbidities and may still feel ill, despite being on medication for their primary diagnosis. Multiple medications are also mostly linked to multiple co-morbidities or advanced disease states or an increased risk of medicines’ interactions, as a result of people taking multiple medications being more likely to feel ill, unsatisfied with the effect of their medicine, and have poor quality-of-life. This also supports the result of the current study which showed that patients taking two or more medications have poor overall quality-of-life than those taking single medication.
People who are illiterate or have attended only primary school think that they received less disease and medicine information from health professionals than people who attended tertiary education. This may be as those patients who have a low level of education are less likely to have prior knowledge about their disease and medications and expect more from physicians, pharmacists, and nurses. As a result they are less likely to be satisfied with the information they get from health professionals. This in turn may make people with lesser education feel worried about their medication. This is marked by the result of the current study showing the psychological impacts of medicine use being more pronounced in people who have secondary education or less. Likewise, as compared to people with tertiary education, illiterate participants reported that their medicine brought lesser improvement in their life. The result of the current study showed that patients with a diagnosis of diabetes mellitus and thyroid disorder received more disease and medicine information and are more satisfied with the effect of medicine use than people with other diagnoses. In terms of overall quality-of-life, people with thyroid disorder reported that their medicines make them live better. This indicates that patients who feel that they receive sufficient medicine and disease-related information are more likely to be satisfied with the effect of the medicine and will have better overall quality-of-life.
Conclusion and Recommendation
Even though almost all of the study participants claim that their medicine brought some degree of improvement in their life, respondents expressed low degrees of satisfaction for some aspects of medication use. Most of the participants were particularly unhappy with the amount of information received about side-effects and what to do if doses were missed. Special emphasis should be given to patients with a low level of education as they were not satisfied with medicine and disease information obtained from health professionals, experienced more psychological impacts of medicine use, and had poor overall quality-of-life.
Limitations
The present study utilized a cross-sectional design. Therefore, it may not indicate the cause and effect relations among variables. In addition, data collectors were around and/or with participants until participants fill the questionnaire. This may influence participants to rush on questions or it may introduce social desirability biases.
Acknowledgment
We the authors would like to acknowledge University of Gondar for its permission and support to undertake the research. We would also like to acknowledge all patients willing to participate in this research. Finally, we are also grateful to the authors who developed and validated the short form of PROMPT-QoL for their permission to use it.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sakthong P, Sangthonganotai T. A randomized controlled trial of the impact of pharmacist-led patient-centered pharmaceutical care on patients’ medicine therapy-related quality of life. Res Social Administrative Pharm. 2018;14(4):332–339. doi:10.1016/j.sapharm.2017.05.001
2. Losada-Camacho M, Guerrero-Pabon MF, Garcia-Delgado P, Martínez-Martinez F. Impact of a pharmaceutical care programme on health-related quality of life among women with epilepsy: a randomised controlled trial (IPHIWWE study). Health Qual Life Outcomes. 2014;12(1):162.
3. Al-Quteimat OM, Amer AM. Evidence-based pharmaceutical care: the next chapter in pharmacy practice. Saudi Pharm J. 2016;24(4):447–451. doi:10.1016/j.jsps.2014.07.010
4. Ayalew MB, Solomon L, Abay S. Pharmaceutical care practice in community and institutional drug retail outlets of Gondar Town, North West Ethiopia. Global Adv Health Med. 2019;8:2164956119868777. doi:10.1177/2164956119868777
5. Tegegn HG, Abdel OA, Mekuria AB, Bhagavathula AS, Ayele AA. Challenges and opportunities of clinical pharmacy services in Ethiopia: a qualitative study from health care practitioners’ perspective. Pharmacy Practice. 16(1).
6. Correr CJ, Pontarolo R, Venson R, Melchiors AC, Wiens A. Effect of a pharmaceutical care program on quality of life and satisfaction with pharmacy services in patients with type 2 diabetes mellitus. Brazilian J Pharm Sci. 2009;45(4):809–817.
7. de Lyra DP, Júnior NK, Abriata JP, da Rocha CE, Dos Santos CB, Pelá IR. Impact of pharmaceutical care interventions in the identification and resolution of drug-related problems and on quality of life in a group of elderly outpatients in Ribeirão Preto (SP), Brazil. Ther Clin Risk Manag. 2007;3(6):989.
8. EUPATI. Patient-reported outcomes (PROs) assessment 2016, January 12. Available from: https://www.eupati.eu/clinical-development-and-trials/patient-reported-outcomes-pros-assessment/.
9. Abebe SM, Andargie G, Shimeka A, et al. The prevalence of non-communicable diseases in northwest Ethiopia: survey of dabat health and demographic surveillance system. BMJ Open. 2017;7(10). doi:10.1136/bmjopen-2016-015496
10. Forestier B, Anthoine E, Reguiai Z, Fohrer C, Blanchin M. A systematic review of dimensions evaluating patient experience in chronic illness. Health Qual Life Outcomes. 2019;17(1):1–3. doi:10.1186/s12955-019-1084-2
11. Sakthong P, Sonsa-ardjit N, Sukarnjanaset P, Munpan W, Sangthonganotai T. Development and psychometrics of a short-form pharmaceutical care-specific measure for quality of life. Int J Clin Pharm. 2018;40(3):642–649. doi:10.1007/s11096-018-0638-4
12. Wikipedia. Pharmaceutical care. Available from: https://en.wikipedia.org/wiki/Pharmaceutical_care.
13. Singhal PK, Raisch DW, Gupchup GV. The impact of pharmaceutical services in community and ambulatory care settings: evidence and recommendations for future research. Annals Pharmacother. 1999;33(12):1336–1355. doi:10.1345/aph.18440
14. Puspitasari HP, Aslani P, Krass I. A review of counseling practices on prescription medicines in community pharmacies. Res Social Administrative Pharm. 2009;5(3):197–210. doi:10.1016/j.sapharm.2008.08.006
15. Puspitasari HP, Aslani P, Krass I. Pharmacists’ and consumers’ viewpoints on counselling on prescription medicines in Australian community pharmacies. Int J Pharm Practice. 2010;18(4):202–208. doi:10.1111/j.2042-7174.2010.00041.x
16. van Geffen EC, Philbert D, van Boheemen C, van Dijk L, Bos MB, Bouvy ML. Patients’ satisfaction with information and experiences with counseling on cardiovascular medication received at the pharmacy. Patient Educ Couns. 2011;83(3):303–309. doi:10.1016/j.pec.2011.04.004
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.