Back to Journals » Clinical Interventions in Aging » Volume 17
Medication Appropriateness, Polypharmacy, and Drug-Drug Interactions in Ambulatory Elderly Patients with Cardiovascular Diseases at Tikur Anbessa Specialized Hospital, Ethiopia
Authors Adem L, Tegegne GT
Received 25 January 2022
Accepted for publication 11 April 2022
Published 16 April 2022 Volume 2022:17 Pages 509—517
DOI https://doi.org/10.2147/CIA.S358633
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Maddalena Illario
Limi Adem, Gobezie T Tegegne
Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Gobezie T Tegegne, Email [email protected]
Background: Appropriate prescribing is often challenging in geriatric patients due to age-related pharmacokinetic and pharmacodynamic alterations. Elderly patients with cardiovascular diseases are frequently prescribed multiple medications. Hence, it is imperative to investigate medication appropriateness, polypharmacy, and drug-drug interactions in these groups of patients.
Objective: To assess medication appropriateness using the 2019 American Geriatric Society Beers and Medication Appropriateness Index criteria, polypharmacy and drug-drug interactions among elderly ambulatory patients with cardiovascular diseases at Tikur Anbessa Specialized Hospital.
Methods: A hospital-based retrospective cross-sectional study was conducted among 384 elderly (60 years and older) ambulatory patients with cardiovascular diseases between May 01-August 30, 2021. Data was collected from the patient’s medical record using a data abstraction tool. The data were entered and analyzed using the SPSS program. Descriptive and logistic regression models were used to present the findings.
Results: The most frequent diagnosis was hypertension (78.4%) followed by ischemic heart disease (31.3%). Averagely, 4.4 ± 2 medications were prescribed per patient. More than half of (53.1%) the patients received polypharmacy. According to Beer’s and medication appropriateness index criteria, over one-third (28.1%) and the majority (95.1%) of the patients were prescribed potentially inappropriate medications, respectively. In addition, 53.1% and 90.1% of patients had polypharmacy, and were exposed to potential drug-drug interactions ranging from mild to major interactions, respectively. Further, polypharmacy was significantly associated with inappropriate medication prescribing.
Conclusion: The study found that more than half of the patients got one or more potentially inappropriate medications in both criteria. The medication appropriateness index tool identified more potentially inappropriate medication than the Beers criteria. In addition, more than half of the patients got polypharmacy and had potential drug-drug interactions. Further, polypharmacy was significantly associated with inappropriate medication prescriptions. These findings highlight the need for interventions to improve appropriate prescribing practice among elderly patients.
Keywords: inappropriate medication, polypharmacy, drug interaction, cardiovascular disease and elderly
Introduction
The world’s aging population is speedily increasing from 9% to 16% between 2019 to 2050.1 Increasing age is associated with higher rates of co-morbidity, disability (cognitive, mental, and functional impairments),2 and multiple medication use.3–5 Aging influences heart activities by decreasing cardiac muscle elasticity and the ability to respond to changes in pressure.6 Hence, it is an independent risk factor for cardiovascular disease (CVD) which poses a great burden to elderly patients.7 Globally, 32% of the deaths were due to CVD. Of which, three fourth of them were from low and middle-income countries.8
Due to multiple chronic diseases, and age-related physiological changes that affect drugs’ pharmacodynamics and pharmacokinetic properties, pharmacotherapy is complex and challenging in the elderly.9 Polypharmacy, non-adherence, inappropriate medication prescription,10,11 drug-drug interaction,12,13 and medication-related problems14 are frequent in elderly patients with CVD. Due to this, elderly patients are at a higher risk of adverse drug events (ADEs).15
Explicit and implicit criteria are used to assess medication safety in the elderly. The explicit criteria (the 2019 American Geriatrics Society (AGS) Beers Criteria)16 involves six medication appropriateness issues, while the implicit criteria (Medication Appropriate Index (MAI))17,18 uses ten criteria. The explicit criteria are primarily concerned with medications and assess how well they meet a set of predetermined criteria, criterion-based with rigid standards. On the other hand, the implicit criteria consider healthcare professionals’ judgment to assess medication appropriateness.
In Ethiopia, the pooled prevalence of CVD was 5% (1–20%) in the general population,19 but its prevalence is expected to be higher in the elderly population. Despite CVD is the leading cause of death and disability among the elderly,20 data are scarce regarding the appropriate use of medication in Tikur Anbessa Specialized Hospital (TASH). Hence, this study aimed to investigate medication appropriateness using both the 2019 AGS and MAI criteria and associated factors in ambulatory elderly cardiac patients at TASH.
Methods
Study Setting
The study was conducted at TASH, As Ababa, Ethiopia. It is the largest referral hospital in Ethiopia, established in 1964. It has more than 800 beds and serves over 250,000 outpatient and 48,000 inpatients annually. Several clinics serve ambulatory patients. The cardiac outpatient clinic serves more than thousands of patients with CVDs.
Study Design and Period
A retrospective cross-sectional study was performed in a cardiac clinic of TASH, Addis Ababa, Ethiopia. The study was conducted from May 01– August 30, 2021.
Study Population and Sample Size
All elderly patients (aged ≥ 60 years) with CVD were the source population. The sample population consisted of elderly CVD patients who are on follow-up during 2018–2021. As per the cardiac clinic officer, there were a total of 1993 elderly CVD patients during the mentioned follow-up period in TASH. The sample size was then calculated by using a simple proportion formula by considering a confidence interval of 95%, marginal error of 5%, and, the prevalence of 50%. The calculated sample size was 384. Systematic random sampling method was used to choose 384 patients’ medical records. Patients with incomplete medical records were excluded.
Study Variables
The dependent variables were medication appropriateness, polypharmacy and drug-drug interactions (DDIs). On the other hand, the independent variables include socio-demographic characteristics, clinical characteristics (comorbidity, Charlson comorbidity index (CCI)), and prescribed number of medications.
Data Collection Tool and Procedure
The data collection form was prepared based on published study findings and standard tools, which consisted of four sections. The first section included questions on the demographic characteristics of patients. The second section contained clinical and medication-related information. The third section was the AGS Beers Criteria and, the fourth section was MAI tool (Supplementary Table 1).
Data were collected retrospectively from patient medical records. The most recent visit was considered for assessment. Medication appropriateness (Supplementary File) was evaluated according to one explicit (AGS Beers’ criteria) and one implicit (MAI) criteria. Both prescription and Over The Counter (OTC) medications were considered. On the contrary, herbal supplements were excluded as they were not well documented. The collected data were thoroughly reviewed and analyzed by experienced clinical pharmacists. DDI was checked using Drugs.com online drug interaction checker. Polypharmacy is considered when the patient is prescribed five or more medications.
Data Quality Control
Before the actual research, a pre-test was done in 5% of patients to check for data collection instrument clarity, consistency, and acceptability. All required changes were made based on the results of the pre-test.
Ethical Consideration
The ethical clearance was obtained from the ethical review committee of the Department of Pharmacology and Clinical Pharmacy (ERB/SOP/315/13/2021), College of Health Sciences, Addis Ababa University. Then, patients, during follow up time, were briefed about the objectives of the study and the confidentiality of their information. In addition, they were informed of the right to abstain from participation in the study or to withdraw consent to participate at any time without reprisal. After ensuring that the patient has understood the information, the data collectors obtained written informed consent.
Statistical Analysis and Interpretation
Data were entered, cleaned analyzed using the Statistical Package for Social Sciences (IBM SPSS Statistics for Windows, version 23). Descriptive statistics were performed to summarize the sociodemographic and clinical characteristics. The results were presented in frequencies, percentages, tables, and figures. Logistic regression was used to determine factors associated with inappropriate medication use which is assessed by the AGS Beers Criteria. The results of the multivariable logistic analysis were reported using adjusted odds ratio (AOR) and 95% CI. Statistical significance was declared at p < 0.05.
Results
Demographic and Clinical Characteristics of the Study Participants
A total of 384 ambulatory elderly cardiac patients were included in the study. The mean age of patients was 68.1 ± 6.5 years, ranging from 60–92 years. Majority (82.6%) of patients were young-old (60 to 74 year age). In addition, 52.6% of them were females, and the majority of (93.7%) the elderly patients had at least one comorbidity (mean 2.68 ±1.2). The average duration of the disease was 8.14 ±7.4 years. Further, 57.6% of patients had ≥ 5 CCI (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of the Study Participants (N=384) |
Disease and Medication Use Pattern
The most frequent CVD encountered were hypertension (78.4%), ischemic heart disease (31.3%), hypertensive heart disease (26.3%), degenerative valvular disease (16.7%), and atrial fibrillation (11.2%).
A total of 1698 medications were prescribed, averagely 4.4 ± 1.9 per patient (range; 1–12 medications). The most frequently prescribed medications were atorvastatin (65%), enalapril (58.6%), aspirin (46.9%), furosemide (44.3%), and amlodipine (37.2%) (Table 2).
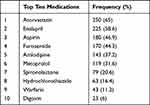 |
Table 2 The Most Frequent CVD Medications Prescribed Among Study Participants |
Medication Appropriateness Among Ambulatory Elderly Patients
Explicit Beer’s Criteria (AGS Beers Criteria)
Over one-third of (28.1%) of elderly CVD patients were prescribed at least one potentially inappropriate medication (PIM), averagely 1.51 ±1.3 per patient. Of these patients, 19.8%, 26.6%, 17.4%, and 6% were prescribed one, two, three, and four or more PIM, respectively. A total of 617 medication-related issues were identified. 54.9% (277), 28.1% (108), 13.4% (38), 4.6% (18) and 1% (4) of patients prescribed medications that should be used with caution, PIM as per the Beers criteria, medications that should be avoided or reduce dose in renal failure, potentially inappropriate medications to avoid in older adults with certain conditions, and medications with clinically important DDIs to be avoided, respectively.
The frequently prescribed inappropriate medications were diuretics (46.29%) and antiplatelet agents (31.5%). (Figure 1) In addition, the frequently prescribed medications that should be avoided in the elderly were amitriptyline (29.6%), proton pump inhibitors (21.3%), digoxin (20.3%), glibenclamide (16.3%), and non-steroidal anti-inflammatory medications (NSAIDs) (12.3%).
 |
Figure 1 Inappropriate drug classes based on the AGS Beers criteria. |
Implicit Criteria (MAI Criteria)
The majority (365, 95.1%) of elderly patients were prescribed one or more PIM. The average MAI score per patient was 18.2 ±12.3 (median 17; range 0–90). The criteria with the highest MAI score were effectiveness, correct dosage, unnecessary duplication, and indication-related issues. On the other hand, the lowest score was the duration of therapy. Considering the cumulative MAI, 320 medications (84.4%) met inappropriate ratings of 0–30 weighted average MAI, 57 (14.8%) met inappropriate ratings of 31–60 weighted average MAI and 3 (0.8%) met inappropriate rating of ≥ 61 weighted average MAI (Table 3).
 |
Table 3 Distribution of Inappropriate Prescriptions Using MAI Criteria |
Polypharmacy and Drug-Drug Interactions in the Elderly
More than half the study participants had polypharmacy (53.1%, 212) and, the majority had (90.1%, 346) potential DDIs which can range from mild to major interactions. Of all DDIs, 15.1%, 75%, and 83.3% were major, moderate, and minor interactions, respectively. (Table 4) The most frequently prescribed major DDIs were enalapril and spironolactone (73%, 46) (causes hyperkalemia), amlodipine and carbamazepine (11.1%, 7) (reduces the blood levels of amlodipine), and enalapril and allopurinol (3.2%, 2) (increases hypersensitivity to allopurinol) (Table 5).
 |
Table 4 Polypharmacy and Drug-Drug Interaction in the Study Participants |
 |
Table 5 List of Severe DDI, Their Prevalence, and Expected Negative Effects |
Factors Associated with Inappropriate Medication Prescription
Patients with polypharmacy were 5.1 times riskier to have inappropriate prescriptions (AOR=5.1, 95% CI [0.110,0.386] p<0.001) than patients having less than five medications (Table 6).
 |
Table 6 Factors Associated with Inappropriate Medication Use |
Discussion
This study analyzed medication appropriateness, polypharmacy and DDI in the ambulatory elderly (aged 60 years and above) patients with CVD at TASH, Addis Ababa with a focus on prevalence and associated factors of PIM.
Our findings showed that 28.1% of the patients received at least one PIM according to the AGS Beers Criteria. Ethiopian studies conducted in geriatric patients at Tirunesh Beijing Hospital, University of Gondar Teaching Hospital chronic care clinic, and Jimma Medical Center reported that 46.9%,21 47.2%,22 and 83.1%23 of older adults were prescribed at least one PIM, respectively. In these studies, medication appropriateness was assessed using Beers criteria in two studies,22,23 while the remaining study21 used both WHO core prescribing indicators and Beers criteria. In addition, our finding was lower than a study done in the United States, with 87.4% of the patients receiving at least one PIM.24 As it is seen in different studies, PIM is common in the elderly. However, the different prevalence may be due to variation in case-mix, availability of medications, type and number of comorbidities.
Our study also revealed that more PIM was detected using MAI than Beers criteria (MAI:95.1%, Beers criteria: 28.1%), which is comparable to a study conducted in Spain (94.1% PIM by MAI, 68.8% by Beers criteria).25 In addition, Awad et al26 detected more cases of PIMs using MAI (74%) than Beers criteria (53.1%). The reason for this could be the Beers criteria have rigid criteria that focus on the drug/drug class, and it does not address patient preference, while MAI focuses on the patients who address the entire medication regimen with the clinical conditions.
Diuretics (46.3%), antiplatelets (31.5%), and tricyclic antidepressants (5.7%) were the frequently prescribed PIMs in our study. However, angiotensin-converting enzyme inhibitors (ACEIs) (15.6%), a combination of aspirin and Vitamin K Antagonist (14%), and statins (3.16%) were the common PIMs reported by Abegaz et al.27 In addition, Tesfaye et al23 found diuretics (46.3%), antiplatelets (31.5%) and tricyclic antidepressants were the common PIMs. Further, a study conducted in Serbia showed that proton pump inhibitors (15.7%) were the frequent PIM according to Beers criteria.28 Such variation may be due to the different clinical conditions, comorbidities, and disease severity of the studied population.
More than half the patients (53.1%) were prescribed polypharmacy, which is higher than the studies conducted in various parts of Ethiopia (10.8–42.5%).21–23 As aging is associated with multiple comorbidities,29,30 polypharmacy is common in the elderly. Similarly, DDI is common in elderly patients.30 Our study revealed that 90.1% of patients had potential mild to major DDIs, which lies in the recent systematic review finding (DDIs: 80.5–90.5%).31 However, it is higher than Bhagavathula et al (2.8%)22 and Assefa et al (84.3%) studies. Of all the DDIs, enalapril and spironolactone interactions (73%) were the most frequent DDI like de Oliveira et al study result.31 On the other hand, van Heerden et al found that central nervous system medications (30.6%) were the frequent causes of DDIs.32 The variation could be due to differences in geriatric circumstances as well as methodological discrepancies, particularly in the methods/software utilized to detect DDIs. In addition, our study revealed that 15.1% of patients had major DDIs, which is relatively lower than the studies conducted in studies conducted at Ethiopian Yekatit 12 medical college hospital (17.3%),12 and in the South African elderly ambulatory patients (25.8%).32 The difference could be due to the variation in the case-mix of targeted patients, and professional expertise.
Regarding risk factors, polypharmacy is significantly associated with PIM (AOR=5.1 95 CI [0.110,0.386], p=0.000). Polypharmacy, which was more common with older people, is recognized as the primary contributor of PIM in the Serbian study.33 In addition, a study done in France reported that the presence of comorbidities, taking multiple medications, and the higher CCI were associated with the likelihood of PIM.34 As the number of medications is increased, the possibility of potential DDIs and drug-disease interactions are increased. This predisposes the patient to have PIM. The variation of PIM risk factors could be due to the type and number of comorbidities, and the case mix of the study population.
The strengths of our study include; firstly, patient-specific factors were considered to evaluate PIM. Secondly, two methods of medication appropriateness were used. On the other hand, there were certain limitations which include (i) doctors were not interviewed to identify their reasons for prescribing the identified PIMs; (ii) the exclusion of herbal supplements may have resulted in an underestimation of PIMs; (iii) the study was done in a single study, and (iv) some medication appropriateness lists were difficult to analyze due to the retrospective nature of the study.
Conclusion
The study found a considerable number of patients prescribed PIM. MAI identified more PIM than the Beers criteria. More than half of the patients prescribed polypharmacy. In addition, the majority of the patients experienced potential mild to major DDIs. Of which, around 15% had major potential DDIs. Moreover, PIM is significantly associated with polypharmacy. These findings highlight the need for interventions that improve appropriate prescription in elderly patients, reduce the number of medications and reduce DDIs.
Abbreviations
ACEi, angiotensin-converting enzyme inhibitors; ADE, adverse drug event; ADR, adverse drug reaction; AGS, American Geriatrics Society; AHA, American Heart Association; AOR, adjusted odds ratio; CCI, Charlson comorbidity index; CHS, College of Health Science; CI, confidence interval; CNS, central nervous system; COR, crude odds ratio; CVD, cardiovascular disease; DDI, drug-drug interaction; HR, hazard ratio; IPET, improving prescribing in the elderly tool; MAI, medication appropriateness index; NSAID, non-steroidal anti-inflammatory drug; OR, odds ratio; OTC, over the counter; PIDP, potentially inappropriate drug prescribing; PIMs, potentially inappropriate medications; PIP, potentially inappropriate prescribing; PP, polypharmacy; PPI, proton pump inhibitors; PPO, potential prescription omissions; SD, standard deviation; SPSS, Statistical Package for Social Sciences; START, Screening Tool of Older People’s Prescription; STOPP, Screening Tool to Alert Doctors to Right Treatment; TASH, Tikur Anbessa Specialized Hospital; TCA, tricyclic antidepressants; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Ethical Review Committee of the School of Pharmacy (ERB/SOP/315/13/2021), College of Health Sciences, Addis Ababa University. Then, patients, during follow up time, were briefed about the objectives of the study and the confidentiality of their information. In addition, they were informed of the right to abstain from participation in the study or to withdraw consent to participate at any time without reprisal. After ensuring that the patient has understood the information, the data collectors obtained written informed consent.
Acknowledgments
We want to acknowledge Addis Ababa University for giving us such an opportunity. In addition, we want to thank study participants and TASH management.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. United Nations. Department of Economic and Social Affairs, Population Division. World population ageing 2019: highlights (ST/ESA/SER.A/430); 2019.
2. Carneiro JA, Cardoso RR, Durães MS, et al. Frailty in the elderly: prevalence and associated factors. Rev Bras Enferm. 2017;70(4):747–752. PubMed PMID: 28793104. doi:10.1590/0034-7167-2016-0633
3. Su BB, Ma JX, Song W, Yuan J, Dong XY, Wan J. [Analysis of comorbidity and polypharmacy in middle-aged and elderly patients]. Zhonghua Yi Xue Za Zhi. 2020;100(25):1983–1987. PubMed PMID: 32629601. Chinese. doi:10.3760/cma.j.cn112137-20200403-01066
4. Preparing for an aging World. The case for Cross-National Research. Washington (DC): National Academies Press (US); 2001. 6, The Health of Aging Populations. Available from: https://www.ncbi.nlm.nih.gov/books/NBK98373/.
5. Berrut G, de Decker L. [Comprehensive assessment of comorbidity in the elderly]. Geriatr Psychol Neuropsychiatr Vieil. 2015;13(Suppl 1):7–12. PubMed PMID: 26345582. French. doi:10.1684/pnv.2015.0543
6. Strait JB, Lakatta EG. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail Clin. 2012;8(1):143–164. PubMed PMID: 22108734. doi:10.1016/j.hfc.2011.08.011
7. Kane AE, Howlett SE. Differences in cardiovascular aging in men and women. Adv Exp Med Biol. 2018;1065:389–411. PubMed PMID: 30051398. doi:10.1007/978-3-319-77932-4_25
8. World Health Organization. Cardiovascular diseases. Available from: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1.
9. Roman YM, Dixon DL, Salgado TM, et al. Challenges in pharmacotherapy for older adults: a framework for pharmacogenomics implementation. Pharmacogenomics. 2020;21(9):627–635. PubMed PMID: 32425117. doi:10.2217/pgs-2019-0198
10. Martínez-Arroyo JL, Gómez-García A, Sauceda-Martínez D. [Polypharmacy prevalence and potentially inappropriate drug prescription in the elderly hospitalized for cardiovascular disease]. Gac Med Mex. 2014;150(Suppl 1):29–38. Norwegian.
11. Stuhec M, Flegar I, Zelko E, Kovačič A, Zabavnik V. Clinical pharmacist interventions in cardiovascular disease pharmacotherapy in elderly patients on excessive polypharmacy: a retrospective pre-post observational multicentric study. Wien Klin Wochenschr. 2021;133(15–16):770–779. PubMed PMID: 33471149. doi:10.1007/s00508-020-01801-y
12. Assefa YA, Kedir A, Kahaliw W. Survey on polypharmacy and drug-drug interactions among elderly people with cardiovascular diseases at yekatit 12 hospital, Addis Ababa, Ethiopia. Integr Pharm Res Pract. 2020;9:1–9. PubMed PMID: 32021833. doi:10.2147/IPRP.S231286
13. Björkman IK, Fastbom J, Schmidt IK, Bernsten CB. Drug—Drug Interactions in the Elderly. Ann Pharmacother. 2002;36(11):1675–1681. doi:10.1345/aph.1A484
14. Ahmad A, Mast MR, Nijpels G, Elders PJ, Dekker JM, Hugtenburg JG. Identification of drug-related problems of elderly patients discharged from hospital. Patient Prefer Adherence. 2014;8:155–165. PubMed PMID: 24523581. doi:10.2147/PPA.S48357
15. Davies EA, O’Mahony MS. Adverse drug reactions in special populations – the elderly. Br J Clin Pharmacol. 2015;80(4):796–807. doi:10.1111/bcp.12596
16. American Geriatrics Society. 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. PubMed PMID: 30693946. doi:10.1111/jgs.15767
17. Hanlon JT, Schmader KE, Samsa GP, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45(10):1045–1051. PubMed PMID: 1474400. doi:10.1016/0895-4356(92)90144-c
18. Spinewine A, Dumont C, Mallet L, Swine C. MEDICATION APPROPRIATENESS INDEX: RELIABILITY AND RECOMMENDATIONS FOR FUTURE USE. J Am Geriatr Soc. 2006;54(4):720–722. doi:10.1111/j.1532-5415.2006.00668_8.x
19. Angaw DA, Ali R, Tadele A, Shumet S. The prevalence of cardiovascular disease in Ethiopia: a systematic review and meta-analysis of institutional and community-based studies. BMC Cardiovasc Disord. 2021;21(1):37. doi:10.1186/s12872-020-01828-z
20. Ali S, Misganaw A, Worku A, et al. The burden of cardiovascular diseases in Ethiopia from 1990 to 2017: evidence from the Global Burden of Disease Study. Int Health. 2020;13(4):318–326. doi:10.1093/inthealth/ihaa069
21. Lemma W, Islam M, Loha E. Potentially inappropriate medication prescribing patterns in geriatric patients in a health facility in Addis Ababa, Ethiopia. Trop J Pharm Res. 2020;19(11):2441–2446.
22. Bhagavathula AS, Seid MA, Adane A, Gebreyohannes EA, Brkic J, Fialová D. Prevalence and determinants of multimorbidity, polypharmacy, and potentially inappropriate medication use in the older outpatients: findings from EuroAgeism H2020 ESR7 Project in Ethiopia. Pharmaceuticals. 2021;14(9):844. doi:10.3390/ph14090844
23. Tesfaye BT, Tessema MT, Yizengaw MA, Bosho DD. Potentially inappropriate medication use among older adult patients on follow-up at the chronic care clinic of a specialized teaching hospital in Ethiopia. A cross-sectional study. BMC Geriatr. 2021;21(1):530. doi:10.1186/s12877-021-02463-9
24. Sheikh-Taha M, Dimassi H. Potentially inappropriate home medications among older patients with cardiovascular disease admitted to a cardiology service in USA. BMC Cardiovasc Disord. 2017;17(1):189. doi:10.1186/s12872-017-0623-1
25. Lopez-Rodriguez JA, Rogero-Blanco E, Aza-Pascual-Salcedo M, et al. Potentially inappropriate prescriptions according to explicit and implicit criteria in patients with multimorbidity and polypharmacy. MULTIPAP: a cross-sectional study. PLoS One. 2020;15(8):e0237186. doi:10.1371/journal.pone.0237186
26. Awad A, Hanna O, Van Dijk L. Potentially inappropriate medication use among geriatric patients in primary care setting: a cross-sectional study using the Beers, STOPP, FORTA and MAI criteria. PLoS One. 2019;14(6):e0218174. PubMed PMID: 31194800; PubMed Central PMCID: PMCPMC6563997. doi:10.1371/journal.pone.0218174
27. Abegaz TM, Birru EM, Mekonnen GB, Marengoni A. Potentially inappropriate prescribing in Ethiopian geriatric patients hospitalized with cardiovascular disorders using START/STOPP criteria. PLoS One. 2018;13(5):e0195949. doi:10.1371/journal.pone.0195949
28. Di Martino E, Provenzani A, Polidori P, De Luca V. Evidence-based application of explicit criteria to assess the appropriateness of geriatric prescriptions at admission and hospital stay. PLoS One. 2020;15(8):e0238064. doi:10.1371/journal.pone.0238064
29. Slabaugh SL, Maio V, Templin M, Abouzaid S. Prevalence and risk of polypharmacy among the elderly in an outpatient setting: a retrospective cohort study in the Emilia-Romagna region, Italy. Drugs Aging. 2010;27(12):1019–1028. PubMed PMID: 21087071. doi:10.2165/11584990-000000000-00000
30. Sheikh-Taha M, Asmar M. Polypharmacy and severe potential drug-drug interactions among older adults with cardiovascular disease in the United States. BMC Geriatr. 2021;21(1):233. doi:10.1186/s12877-021-02183-0
31. de Oliveira LM, Diel J, Nunes A, Dal Pizzol TDS. Prevalence of drug interactions in hospitalised elderly patients: a systematic review. Eur J Hosp Pharm. 2021;28(1):4–9. PubMed PMID: 33355278; PubMed Central PMCID. doi:10.1136/ejhpharm-2019-002111
32. van Heerden JA, Burger JR, Gerber JJ, Vlahović-Palčevski V. Prevalence of potentially serious drug-drug interactions among South African elderly private health sector patients using the Mimica Matanović/Vlahović-Palčevski protocol. Int J Pharm Pract. 2018;26(2):156–164. PubMed PMID: 28665037. doi:10.1111/ijpp.12383
33. Cvetković Z, Perić A, Dobrić S. Potentially Inappropriate prescribing and potential clinically significant drug-drug interactions in older outpatients: is there any association? Medicina. 2019;55(7):332. PubMed PMID: 31277258; PubMed Central PMCID: PMCPMC6680842. doi:10.3390/medicina55070332
34. Cool C, Cestac P, Laborde C, et al. Potentially inappropriate drug prescribing and associated factors in nursing homes. J Am Med Dir Assoc. 2014;15(11):
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
