Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Medication Administration Error Perceptions Among Critical Care Nurses: A Cross-Sectional, Descriptive Study
Authors Alzoubi MM, Al-Mahasneh A, Al-Mugheed K , Al Barmawi M, Alsenany SA, Farghaly Abdelaliem SM
Received 2 April 2023
Accepted for publication 17 May 2023
Published 30 May 2023 Volume 2023:16 Pages 1503—1512
DOI https://doi.org/10.2147/JMDH.S411840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Majdi M Alzoubi,1 Asmaa Al-Mahasneh,1 Khalid Al-Mugheed,2 Marwa Al Barmawi,1 Samira Ahmed Alsenany,3 Sally Mohammed Farghaly Abdelaliem4
1Faculty of Nursing, Al-Zaytoonah University of Jordan, Amman, Jordan; 2College of Nursing, Riyadh Elm University, Riyadh, Saudi Arabia; 3Department of Community Health Nursing, College of Nursing, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 4Department of Nursing Management and Education, College of Nursing, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Correspondence: Majdi M Alzoubi, Faculty of Nursing, Al-Zaytoonah University of Jordan, Amman, Jordan, Email [email protected] Khalid Al-Mugheed, College of Nursing, Riyadh Elm University, Riyadh, Saudi Arabia, Email [email protected]
Purpose: This study aimed to investigate the medication administration error perceptions among Jordanian critical care nurses.
Methods: A cross-sectional, descriptive design was used among Jordanian critical care nurses. The total number of completed questionnaires submitted for analysis was 340. Data were collected between July and August 2022 in two health sectors (governmental hospitals and educational hospital) in the middle and north region in Jordan through a self-administered questionnaire on medication administration errors which includes 65 items with three parts.
Results: Nurses showed negative perceptions toward medication administration errors. The majority of participants agreed that “The packaging of many medications is similar” (76.7%), followed by “different medications look alike” (76.2%), as the main reasons for medication error occurrence. Two thirds of participants agreed that “when med errors occur, nursing administration focuses on the individual rather than looking at the systems as a potential cause of the error” (74.1%). Similarly, 73.5% of them believed nurses were blamed if something happens to the patient as a result of the medication error was the main reason for underreporting of MAEs. The highest reported levels of medication errors were in a range between 41% and 70%, for both types intravenous (IV) medication errors and non-intravenous (non-IV) medication errors.
Conclusion: Implement interventions centered on MAEs in particular among critical care nurses, owing to the proven significance of it in foretelling their crucial role in delivering safe care to patients, which will lead to quantifiable returns on both patient outcomes and nurse health, as well as the overall efficiency and image of the organization.
Keywords: medication administration errors, critical care nurses, perceptions, underreporting
Introduction
The National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) define medication administration errors (MAEs) as any preventable incident that may induce or inevitably lead to unsuitable medication use or patient injury while the medication is under the control of the healthcare professional and patient.1 MAEs can increase the burden of care, cost of care, and length of stay of patients.2 In 2017, the World Health Organization launched the Third Global Patient Safety Challenge (Medication without harm) which aims to decrease medication-related injury over the next five years.3
MAEs are a global challenge with 5% being fatal, and about 50% preventable in a routine clinical environment.4 It has been discovered that 19% of MAEs in the intensive care unit (ICU) are life-threatening, and 42% are significant enough or clinically significant to justify extra life-sustaining treatment.5 Furthermore, critically ill patients vary from the majority of hospital patients in that they have limited capacity to participate in their medical care and lack the physiological reserves to withstand further harm.6 According to data, MAEs are the most common type of error, accounting for 78% of severe medical errors in the ICU.7 Furthermore, the annual cost of managing patients with medication-related errors surpasses $40 billion.8 MAEs, in agreement, lengthen hospitalizations by two days and raise expenditures by $2000–$2500 for each patient.1
Medication errors can occur in any parts of the medication process: during prescribing, preparing, or administering and dispensing.9 The administration phase of the medication process revealed the most frequent occurrence of medication errors that were administered by nurses.1,10 Several frequent types of MAEs include omission of doses, wrong route, wrong dose, lack of documentation, wrong time, wrong patient, wrong drug, and technical errors.5
Nurses, as members of multidisciplinary teams, play an important role in providing care in ICUs, where the treatment they deliver is often more complicated than that delivered in a different place in the hospital.11,12 Working in a field that requires so much multitasking, as well as a heavy workload and the need to provide specialized care to seriously ill and dependent patients, can be intimidating for nurses.11,13,14
Despite increased global attention on this topic, the number of medication errors has not dropped considerably.15 Personal variables,16 institutional factors,17 drug-related variables and unclear pharmacological information,8,18 heavy workload, preparing the medication without double verifying,19 and shortage of nurses and a deficiency of pharmacological knowledge20–23 have all been identified as potential causes of MAEs. Addressing correct reporting practices of MAEs, and recognizing factors that contribute to the underreporting of MAEs, may assist to decrease the occurrence of MAEs and raise the reported error percentage. Therefore, this study aimed to investigate the MAEs among Jordanian critical care nurses.
Method
Research Design
A cross-sectional, descriptive design was used in the investigation.
Study Population and Sampling
The convenience sampling method was used to select the hospitals in the two health sectors (governmental hospitals and educational hospital) in the middle and north region in Jordan. The sample size was calculated using the G*Power 3.1.10 program.24 Using a regression test, the minimal required sample size was 178 (power = 0.95, α = 0.05, and medium effect size = 0.11 with 11 predictors). The inclusion criteria included the critical care unit (CCU) and at least one year of experience. The nurses who worked in the general department and trainees were excluded. The total nurses of the CCU were 400. A total of 366 out of 400 questionnaires were received with a response rate of 91.5%. The missing data and questionnaires not completely filled were excluded from analysis. The total questionnaires submitted for analysis was 340.
Instruments
Demographic data included participant’s age, educational level, experience in CCU in years, and shift work and shift-work hours. To examine the critical care nurses’ perception of MAEs, the researcher used the MAE self-reported questionnaire developed by Wakefield et al.25 It includes 65 items with three parts; the first part comprises 29 items related to reasons for MAE occurrence, and the second part comprises 16 items related to underreporting of medication administration errors. A five-point Likert-type scale with fixed values ranging from 5 = strongly agree to 1 = strongly disagree was used to examine the perception of respondents of MAEs. The third part comprised 20 items related to the percentage of each type of medication error; non-intravenous (non-IV) medication errors 9 items, and intravenous (IV) medication errors 11 items. The estimated percentage of errors reported was represented by the frequencies for each percent increment. The pilot study was chosen from among the enrolled nurses working in critical care units (N = 40) to test the functionality of the forms. All questions were clear, simple, and understandable, according to the results. The pilot study was excluded from the main data.
In this study, the reliability of the subscales, reasons for MAE occurrence, underreporting of MAEs, percentage of non-IV MAEs, and percentage of IV MAEs scales were 0.957, 0.927, 0.925, and 0.955 respectively.
Data Collection
Data were collected through a self-administered questionnaire between July and August 2022. During data collection, each participant received a copy of the informed consent and questionnaire. Researchers avoided the periods when nurses were providing treatment and care to patients, to avoid stressing participants that could affect the proficiency of the data collection process. In addition, the optimal time to complete a questionnaire was 10–15 minutes. The principal researcher met the nursing director and participants to explain to them the purpose of the study and guaranteed them that the study was secret and availability to withdraw without any direct or indirect harm. The researcher took the responsibility to collect these data for privacy issues through reading literally the statements in the surveys without any additional explanations or delineation. All data were saved in the personal computer of the primary researcher.
Ethics Committee
Prior to data collection, ethical approval was gained from the faculty of nursing in Al-Zaytoonah University of Jordan and the ethical board to the target institutions with number 2022–2021\380103. Informed consent was obtained from the study participants. In this study, guidelines outlined in the declaration of Helsinki were followed.
Data Analysis
First, data cleaning and investigation were carried out to look for missing values and incorrect data entry. The descriptive and inferential statistics were used in the current study’s statistical analysis. The descriptive analysis displays the mean, standard deviation, frequency distribution, and percentages. Logistic regression analysis was performed to identify significant factors associated with the reason for MAE, underreport of MAE, percentage of non-IV MAE, and percentage of IV MAE. P-values of less than 0.5 were considered significant.
Results
Table 1 shows the descriptive characteristics of the participants. Amongst the study participants, 42.9% (n = 146) were male and 57.1% (n = 194) were female and the mean age of the participants was 32.8 (SD = 6.92). The majority of the participants (73.8%, n = 251) were married. The mean years of experience in the ICU was 7.0 respectively. Furthermore, the majority of the participants (63.5%, n = 216) worked an 8-hour shift.
 |
Table 1 Participants’ Sociodemographic Characteristics |
The results in Table 2 show that nurses responded negatively to the medication administration error perceptions. The mean of reason for ME (4.10) was slightly lower than the mean of underreport ME (4.12). The mean of estimated percentage for non-IV ME (42.75) was slightly higher than the mean of estimated percentage for IV ME (41.35). Furthermore, the Cronbach’s alpha of the subscales ranged from 0.925 to 0.957.
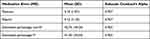 |
Table 2 Level of Perceptions of Medication Administration Error Among Jordanian Critical Care Nurses |
The highest frequencies were sum agree and total agree. The majority of participants agreed that “The packaging of many medications is similar” (76.7%), followed by “different medications look alike” (76.2%), as the main reasons for medication error. Then followed “Physicians change orders frequently” (75.8%), “Unit staff do not receive enough in-services on new medications” (75%), “Unit staffing levels are inadequate” (74.4%), “More than half of participants believed that errors are made in the Medication Kardex” (60.5%), “Nurse is unaware of a known allergy” (59.0%), and “Pharmacy does not label the med correctly” (57.4%) (Table 3).
 |
Table 3 Reasons for Medication Error Occurrence |
The highest frequencies were sum agree and total agree. Two thirds of participants agreed that “when med errors occur, nursing administration focuses on the individual rather than looking at the systems as a potential cause of the error” (74.1%). Similarly, 73.5% of them “believed nurses blamed if something happens to the patient as a result of the medication error” was the main reason for underreporting of MAEs. Followed by “Believed that other nurses will think they are incompetent if they make medication errors” (72.3%). Among the respondents, “nurses do not agree with hospital’s definition of a medication error” (60.2%) and “The expectation that medications be given exactly as ordered is unrealistic” (61.1%) (Table 4).
 |
Table 4 Underreporting of Medication Administration Errors |
Table 5 shows the percentage reported in medication errors for both types. The highest percentage reported level of medication errors were in a range between 41% and 70% for both types. For non-IV medication errors, “Medication is omitted” was the highest frequency reported (N = 181). Followed by “Given to patient with a known allergy” (N = 175), “wrong time of administration” (N = 174). For IV errors, the highest frequency was reported in the item “wrong rate of administration” (N = 194), followed by “wrong method of administration” (N = 179) and “wrong time of administration” (N = 178). The lowest percentage reported levels of medication errors were 71% or above for both types. For non-IV medication errors, “wrong patient” (N = 38) and “wrong drug” (N = 37). For IV errors, “wrong rate of administration” (N = 25).
 |
Table 5 Percentage Reported of IV Errors and Non-IV Medication Errors |
Table 6 for the logistic regression analysis shows predictors of medication administration errors. For 1 year increased experience in the CCU the estimated percentage of non-IV ME will increase by 5% (AOR = 1.05, P = 0.026). For working shift hours: those with the 8-hour shift were 68% more likely to have high estimated percentage of non-IV ME than others (AOR = 1.68, P = 0.087); and those with the 12-hour shift were 11.3 times more likely to have high estimated percentage of non-IV ME than others (AOR = 11.25, P < 0.001).
 |
Table 6 Assessment of Factors Affecting Nurses’ MAE Reporting Score |
Discussion
In the current study, participants demonstrated negative perception toward medication error reporting; these findings disagreed with a national study conducted among Jordanian nurses to evaluate their behaviour toward medication errors in which the nurses showed positive perception.26 Also, in Saudi Arabia nurses reported positive perception in medication error,27 and in the United States nurses reported positive perception in medication error.28,29 Participants’ negative perceptions confirm that nursing schools are the suitable place to increase awareness and behavior in terms of medication error attitudes before graduation and the shifting in clinical practice necessary to improve nurses’ decision-making skills.30 In addition, they confirm that the hospital should offer special courses to nurses to enhance their perception of medication error and how to deal with the error and reduce the number of needle stick injuries.31
According to nurses, inadequate unit staffing, medications looking alike, and lack of in-services were the main reasons for underreporting of MAEs. Our finding was in agreement with other studies.26,30 This result might be due to inefficient institutional regulations. Reporting adverse events is necessary for boosting patient safety through discovering mistakes and becoming the key element of patient safety.32 Providing in-service education is important for medication errors decreasing and infection control that allows the nurses to adapt with recent guidelines of medication, and new administration techniques.33,34
The current findings demonstrated that estimated percentage medication errors were in a range between 41% and 70% for both types IV ME and non-IV ME. These findings are lower than those reported (73.43% and 80%) for the Iranian critical care nurses reporting the occurrence of medication errors.8,19 However, the current results are parallel with those reported by Ehsani et al, who found that 46.8% of emergency department nurses reported the occurrence of medication errors during the past year, which is nearly similar to the current study’s results.20 Additionally, another study by Agalu et al found that Ethiopian critical care nurses report 51.8% levels of medication errors.35 Further, our findings support the previous findings reported by Al-Shara, who found that the highest level of medication errors was 48.4% among Jordanian nurses which is relatively near to our findings.36 Medication administration is nursing practice and has been promoted by experience. When experienced nurses can earn more knowledge and enhance their skills on medication administration practice it may contribute to the quality of nursing care improvement and reduce MAEs.37–39
The logistic regression analysis shows that only working shift hours was considered an important predictor of medication administration errors. Similar to our study findings40. Besides, Di Muzio et al identified that stress, fatigue, increased workload, night shifts, nurse staffing ratio, and workflow interruptions are significant predictors of MAEs, which are deemed particularly parallel to our findings in agreeing the working shift hours as a significant predictor.41 Additionally, our findings are on the contrary to Shahrokhi et al, who concluded that the nurse’s inadequate attention, the errors occurring in the transfer of medication orders from the patient’s file to Kardex, and the ward’s heavy workload were significant predictors of MAEs.42
Limitations
Some limitations were faced in this study. For example, because this was a cross-sectional study, the variables were only studied for a brief time; hence, the responses were mostly based on the participants’ judgments of MEs only at the time of data collection, which may have contributed to selection bias. This study’s generalizability is restricted because the sample was not chosen randomly and was chosen from a particular department. Moreover, because the study was cross-sectional, it was not possible to make conclusions regarding cause-and-effect correlations. Furthermore, researchers appeared to have some sample selection constraints since the sample only included critical care nurses; as a result, researchers may have overlooked a large number of other nurses, contributing to sampling bias.
Conclusion
Nurses showed negative perceptions toward medication administration errors. The main reasons for medication error occurrence were that packaging of many medications is similar and different medications look alike. The underreporting of MAEs were blamed and fear of adverse consequences. Implement interventions centered on MEs in particular among CCU nurses, owing to the proven significance of it in foretelling their crucial role in delivering safe care to patients, which will lead to quantifiable returns on both patient outcomes and nurse health, as well as the overall efficiency and image of the organization. Establishing a responsible department for reacting to nursing issues and errors, and establishing a punishment-free environment will boost the nurse’s willingness to report errors.
Funding
The research was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number PNURSP2023R279, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Disclosure
The authors have no conflicts of interest to disclose.
References
1. Alrabadi N, Haddad R, Haddad R, et al. Medication errors among registered nurses in Jordan. J Pharm Health Serv Res. 2020;11(3):237–243. doi:10.1111/jphs.12348
2. Alrabadi N, Shawagfeh S, Haddad R, et al. Medication errors: a focus on nursing practice. J Pharm Health Serv Res. 2021;12(1):78–86. doi:10.1093/jphsr/rmaa025
3. Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: who’s third global patient safety challenge. Lancet. 2017;389:1680–1681. doi:10.1016/S0140-6736(17)31047-4
4. Ali LAI, Saifan AR, Alrimawi I, Atout M, Salameh B. Perceptions of nurses about reporting medication administration errors in Jordanian hospitals: a qualitative study. Appl Nurs Res. 2021;59:151432. doi:10.1016/j.apnr.2021.151432
5. Koyama AK, Maddox C, Li L, Bucknall T, Westbrook JI. Effectiveness of double checking to reduce medication administration errors: a systematic review. BMJ Qual Saf. 2020;29(7):595–603. doi:10.1136/bmjqs-2019-009552
6. Farzi S, Irajpour A, Saghaei M, Ravaghi H. Causes of medication errors in intensive care units from the perspective of healthcare professionals. J Res Pharm Pract. 2017;6(3):158. doi:10.4103/jrpp.JRPP_17_47
7. Chalasani SH, Ramesh M. Towards patient safety: assessment of medication errors in the intensive care unit in a developing country’s tertiary care teaching hospital. Eur J Hosp Pharm. 2017;24(6):361–365. doi:10.1136/ejhpharm-2016-001083
8. Cheraghi MA, Nikbakhat AR, Mohammad NE, Salari A, Ehsani SR. Medication errors among nurses in intensive care units (ICU). J Maz Univ Med Sci. 2012;21(1):115–119.
9. Dorothy A, Yadesa TM, Atukunda E. Prevalence of medication errors and the associated factors: a prospective observational study among cancer patients at Mbarara regional referral hospital. Cancer Manag Res. 2021;13:3739. doi:10.2147/CMAR.S307001
10. Mrayyan MT. Reported incidence, causes, and reporting of medication errors in teaching hospitals in Jordan: a comparative study. Contemp Nurse. 2012;41:216–232. doi:10.5172/conu.2012.41.2.216
11. Al‐Mugheed K, Bayraktar N. Patient safety attitudes among critical care nurses: a case study in North Cyprus. Int J Health Plann Manage. 2020;35(4):910–921. doi:10.1002/hpm.2976
12. AL-Mugheed K, Bayraktar N, Al-Bsheish M, et al. Patient safety attitudes among doctors and nurses: associations with workload, adverse events, experience. Healthcare. 2022;10:631. doi:10.3390/healthcare10040631
13. Alharbi H, Alshehry A. Perceived stress and coping strategies among ICU nurses in government tertiary hospitals in Saudi Arabia: a cross-sectional study. Ann Saudi Med. 2019;39(1):48–55. doi:10.5144/0256-4947.2019.48
14. AL-Mugheed K, Bayraktar N, Al-Bsheish M, et al. Patient safety attitudes among doctors and nurses: associations with workload, adverse events, experience. Healthcare. 2022;631(10):1.
15. Shahin M, Alwaqfi B, Alabed H. Perception of medication errors among critical care nurses in Jordanian Hospitals: causes and reporting. Int J Curr Res. 2018;10(11):75657–75663.
16. Henneman EA, Roche JP, Fisher DL, et al. Error identification and recovery by student nurses using human patient simulation: opportunity to improve patient safety. Appl Nurs Res. 2010;23(1):11–21. doi:10.1016/j.apnr.2008.02.004
17. Keers RN, Williams SD, Cooke J, Ashcroft DM. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf. 2013;36(11):1045–1067. doi:10.1007/s40264-013-0090-2
18. Agyemang RE, While A. Medication errors: types, causes and impact on nursing practice. Br J Nurs. 2010;19(6):380–385. doi:10.12968/bjon.2010.19.6.47237
19. Farzi S, Farzi S, Alimohammadi N, Moladoost A. Medication errors by the intensive care units’ nurses and the preventive strategies. Anesth Pain Med. 2016;6(4):33–45.
20. Ehsani SR, Cheraghi MA, Nejati A, Salari A, Esmaeilpoor AH, Nejad EM. Medication errors of nurses in the emergency department. J Med Ethics Hist Med. 2013;6:6.
21. Innab A. The Influence of Individual and System Factors on Medication Administration Errors in Acute Care Settings in Saudi Arabia [Doctoral dissertation]. Saint Louis University; 2019.
22. Kerari A, Innab A. The influence of nurses’ characteristics on medication administration errors: an integrative review. SAGE Open Nurs. 2021;7:23779608211025802. doi:10.1177/23779608211025802
23. Fathallah MM, Ibrahem AA, Sayed S. Medication administration errors and barriers to reporting: critical care nurses’ point of view. Int Egypt J Nurs Sci Res. 2023;3(2):103–121.
24. Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi:10.3758/BF03193146
25. Wakefield BJ, Uden-Holman T, Wakefield DS. Development and validation of the medication administration error reporting survey. In: Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005.
26. Yousef A, Abu Farha R, Da’meh K. Medication administration errors: causes and reporting behaviours from nurse’s perspectives. Int J Clin Pract. 2021;75:e14541. doi:10.1111/ijcp.14541
27. Almutary HH, Lewis PA. Nurses’ willingness to report medication administration errors in Saudi Arabia. Qual Manag Healthcare. 2012;21:119–126. doi:10.1097/QMH.0b013e31825e86c8
28. Throckmorton T, Etchegaray J. Factors affecting incident reporting by registered nurses: the relationship of perceptions of the environment for reporting errors, knowledge of the nursing practice act, and demographics on intent to report errors. J PeriAnesthesia Nurs. 2007;22:400–412. doi:10.1016/j.jopan.2007.09.006
29. Ulanimo VM, O’Leary-Kelley C, Connolly PM. Nurses’ perceptions of causes of medication errors and barriers to reporting. J Nurs Care Qual. 2007;22:28–33. doi:10.1097/00001786-200701000-00007
30. Rababa M, Bani-Hamad D, Hayajneh AA, Al Mugheed K. Nurses’ knowledge, attitudes, practice, and decision-making skills related to sepsis assessment and management. Electron J Gen Med. 2022;19(6):em420. doi:10.29333/ejgm/12556
31. Al-Mugheed K, Farghaly SM, Baghdadi NA, Oweidat I, Alzoubi MM. Incidence, knowledge, attitude and practice toward needle stick injury among nursing students in Saudi Arabia. Front Public Health. 2023;11:1160680. doi:10.3389/fpubh.2023.1160680
32. Kim KS, Kwon S-H, Kim J-A, Cho S. Nurses’ perceptions of medication errors and their contributing factors in South Korea. J Nurs Manag. 2011;19:346–353. doi:10.1111/j.1365-2834.2011.01249.x
33. AL-Mugheed K, Bayraktar N, Al-Bsheish M, et al. Effectiveness of game-based virtual reality phone application and online education on knowledge, attitude and compliance of standard precautions among nursing students. PLoS One. 2022;17(11):e0275130. doi:10.1371/journal.pone.0275130
34. Wondmieneh A, Alemu W, Tadele N, Demis A. Medication administration errors and contributing factors among nurses: a cross sectional study in tertiary hospitals, Addis Ababa, Ethiopia. BMC Nurs. 2020;19:4. doi:10.1186/s12912-020-0397-0
35. Agalu A, Ayele Y, Bedada W, Woldie M. Medication administration errors in an intensive care unit in Ethiopia. Int Arch Med. 2012;5(1):1–6. doi:10.1186/1755-7682-5-15
36. Al-Shara M. Factors contributing to medication errors in Jordan: a nursing perspective. Iran J Nurs Midwifery Res. 2011;16(2):158.
37. Blignaut AJ, Coetzee SK, Klopper HC, Ellis SM. Nurses’ perceptions of medication administration safety in public hospitals in the Gauteng Province: a mixed method study. Int J Africa Nurs Sci. 2022;17:100504.
38. Alzoubi M, Hayati KS, Rosliza AM, Ahmad AA, Al-Hamdan Z. Total quality management in the health-care context: integrating the literature and directing future research. Risk Manag Healthc Policy. 2022;12:167–177. doi:10.2147/RMHP.S197038
39. Alrahbeni T, Alenezi ME. Root cause analysis of medication administration error by nursing staff at a number of medical institutes in Riyadh. J Pharm Res Int. 2021;33(35B):152–161. doi:10.9734/jpri/2021/v33i35B31914
40. Montgomery AP, Azuero A, Baernholdt M, et al. Nurse burnout predicts self-reported medication administration errors in acute care hospitals. J Healthc Qual. 2021;43(1):13–23. doi:10.1097/JHQ.0000000000000274
41. Di Muzio M, Dionisi S, Di Simone E, et al. Can nurses’ shift work jeopardize the patient safety? A systematic review. Eur Rev Med Pharmacol Sci. 2019;23(10):4507–4519. doi:10.26355/eurrev_201905_17963
42. Shahrokhi A, Ebrahimpour F, Ghodousi A. Factors effective on medication errors: a nursing view. J Res Pharm Pract. 2013;2(1):18. doi:10.4103/2279-042X.114084
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
