Back to Journals » Patient Preference and Adherence » Volume 16
Medication Adherence Among Hypertensive Patients Attending Different Primary Health Centers in Abha, Saudi Arabia: A Cross-Sectional Study
Authors Thirunavukkarasu A, Naser Abdullah Alshahrani A, Mazen Abdel-Salam D , Homoud Al-Hazmi A, Farhan ALruwaili B, Awad Alsaidan A , Narapureddy BR , Muteb AL-Ruwaili A, Ghuwayli aljabri F, Khalaf Albalawi R, Alanazi KAF
Received 6 September 2022
Accepted for publication 12 October 2022
Published 19 October 2022 Volume 2022:16 Pages 2835—2844
DOI https://doi.org/10.2147/PPA.S388365
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ashokkumar Thirunavukkarasu,1 Abdullah Naser Abdullah Alshahrani,1,2 Doaa Mazen Abdel-Salam,3 Ahmad Homoud Al-Hazmi,1 Bashayer Farhan ALruwaili,1 Aseel Awad Alsaidan,1 Bayapa Reddy Narapureddy,3 Aliyah Muteb AL-Ruwaili,4 Fahad Ghuwayli aljabri,5 Rahaf Khalaf Albalawi,5 Khaled Abdulrahman F Alanazi5
1Department of Community and Family Medicine, College of Medicine, Jouf University, Sakaka, Saudi Arabia; 2Department of Public Health, Asir Health Affairs, Asir Region, Saudi Arabia; 3Department of Public Health and Community Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt; 4Department of Public Health, Ministry of Health, Jouf Health Affairs, Sakaka, Aljouf, Saudi Arabia; 5College of Medicine, Jouf University, Sakaka, Saudi Arabia
Correspondence: Ashokkumar Thirunavukkarasu, Email [email protected]
Background and Objectives: Optimal blood pressure control is achieved by medication adherence. This will reduce the risk of associated morbidities and mortalities. The present study aimed to determine medication adherence and its associated factors among hypertensive patients attending different primary health centers (PHC) in Abha, Saudi Arabia (KSA).
Methods: A cross-sectional study was conducted among ten different PHCs in Abha, KSA. Simple random sampling procedure was utilized to choose 400 participants. A structured anonymous questionnaire was used in the present study. Analysis of the data was done using the SPSS program, version 23. A logistic regression statistical test was applied to identify the independent associated factors of medication adherence. Furthermore, we have applied Spearman’s test to find the correlation between overall B-IPQ score and medication adherence score.
Results: A total of 400 hypertensive patients responded in the present survey. More than one-third of the participants (36.3%) were in the high adherence category group, while the remaining participants (63.7%) were either low or medium adherence category. The binary logistic regression analysis revealed that low and medium adherence category is significantly associated with age (adjusted odds ratio [AOR] = 0.96, 95% CI =0.93– 0.99, p = 0.021), married participants (AOR = 0.42, 95% CI =0.33– 0.58, p = 0.001), residing at village (AOR = 1.49, 95% CI =1.14– 1.73, p = 0.038), and participants with monthly family income of 5000 to 7000 SAR (AOR = 3.06, 95% CI =1.62– 5.79, p = 0.001). A negligible positive correlation was revealed between illness perception and medication adherence.
Conclusion: The present study revealed that hypertensive patients poorly adhere to their antihypertensive medications. This low adherence is significantly associated with the age, monthly income, people living in rural areas, and married participants. The present study results recommend sustained efforts to implement health education programs and awareness-raising interventions targeted at hypertensive patients.
Keywords: medication adherence, hypertension, illness perception, primary health centers, Saudi Arabia
Erratum for this paper has been published.
Introduction
Healthcare adherence is defined by the World Health Organization (WHO) as “The extent to which an individual behavior (in terms of medications intake, adopting healthy diets, or performing lifestyle modifications) concurs with medical or health advice”.1 Healthcare adherence includes the timely and proper use of medicines, the timely presence in the predetermined treatment programs, follow-up of the disease for any later required referral, and adherence with health behaviors change. In healthcare non-adherence, patients do not comply with therapeutic recommendations intentionally and consciously.2,3 Non-adherence may result in disappointment of healthcare providers, undesirable health outcomes, increased use of health services, increased rate of morbidity and mortality, and wastage of resources in healthcare systems.4–6
Hypertension is one of the serious public health problems globally as it is considered one of the leading preventable causes of morbidities and mortalities. Globally, this is a major cause of premature mortality affecting one in four males and one in five females.7–9 In the kingdom of Saudi Arabia (KSA), hypertension is one of the leading causes of death and morbidity among adults. It has been estimated that about one in four adults have been diagnosed with hypertension.10–12 Furthermore, poor blood pressure control among Saudi patients is well demonstrated in the literature.13,14
A study conducted in Malaysia to assess medication adherence among hypertensive patients of primary health centers (PHC) showed good adherence in 53.4% of the total population studied. They reported that female patients were more likely to adhere to the medication than male patients. Also, the Chinese patients adhered to hypertensive medications two times more than the Indian patients.15 A study was carried out to determine the barriers to medication adherence among hypertensive patients in deprived rural areas. It showed that medication adherence was significantly decreased and had a significant positive correlation with gender and economic status, while it was negatively correlated with age. Medication Adherence had a positive correlation with the duration of hypertension, while it negatively correlated with the number of medications used and concurrently with other diseases.16 In the KSA, Khayyat et al surveyed Saudi hypertensive patients attending primary care clinics and assessed the predictors of medication adherence and blood pressure control. In their survey, 54% of hypertensive patients did not adhere to the medicines prescribed by their physicians. Binary logistic regression tests reported that highly adherent participants were around five times more likely to have a well-controlled blood pressure than low-adherent hypertensive patients. Female gender, Age > 65 years, and being diabetic were found to be independent predictors of medication adherence.17
Illness perception is an individual feelings and experiences about a particular disease. This concept is particularly important in hypertension management as it is directly associated with in changing behavior, utilization of healthcare services, and adherence to medications prescribed by the physicians.18–20 Some researchers reported that illness perception is one of the important correlates of medication adherence.19 However, very few studies have attempted to correlate the brief illness perception with medication adherence, especially in the KSA.
The main concerns of the healthcare system nowadays are problems associated with patients’ non-adherence to medical problems. The desired blood pressure control will not be achieved if the patients do not comply with the therapeutic recommendations of physicians, despite the tremendous efforts of physicians.21 The government of Saudi arranges the health system at four levels ranging from primary care centers to apex hospitals. The healthcare services, including hypertension management at PHCs are given free of cost for their country citizens and government expatriate workers. Also, concerned Saudi authorities made health insurance mandatory for all other category populations residing and visiting the KSA. The PHCs play a critical role in creating awareness, screening, diagnosis, and management of hypertension. Hence, it is essential to investigate medication adherence and factors affecting adherence among hypertensive patients receiving care at PHCs. So that necessary measures can be taken within the PHCs to promote patients’ adherence to their medications, prevent long-term side effects of non-adherence and decrease the burden on tertiary health care.22,23 The present study was conducted to determine medication adherence and its associated factors among hypertensive patients attending different PHCs in Abha, KSA. Also, the authors aimed to identify the correlation between hypertensive patients’ medication adherence and brief perception of illness.
Materials and Methods
Study Design and Setting
The present study is a descriptive, cross-sectional carried out to determine medication adherence among hypertensive patients attending different primary health centers in Abha, Saudi Arabia from December 2021 to June 2022.
Sampling Technique
There were 40 PHCs in Abha, KSA, 10 centers were selected by simple random sampling technique. The number of participants included in each PHC were proportional to the number of patients served by this center. The questionnaires were distributed by the researchers to all patients attending the selected centers except those who refused to participate in the study.
Sample Size
We have estimated the required number of participants using the Epi-Info version 7 StatCalc, which is available from the Centers for Disease Control (CDC) and the WHO. The authors determined the following criteria after reviewing the available literature to calculate the least sample size: infinite population size, expected frequency of 50%, confidence level of 95%, power of study as 80%, design effect of 1 and a margin of error of 5%. The calculated sample size was 384 and rounded to 400.
Inclusion and Exclusion Criteria
Patients over 18 years of age, both male and female, with a confirmed diagnosis of hypertension for at least one year and taking at least one medication to treat hypertension were included in the study. The present study included the patients visiting the primary health centers and excluded the patients receiving care at private clinics. Patients with mental health issues, cancers, or any other terminal illness and unwilling to participate in the study were excluded from the study.
Data Collection Method
The present study’s protocol was ethically cleared by the local committee of bioethics (LCBE) of the Jouf University, Saudi Arabia through approval number 20-08-42. We have obtained informed consent from the study participants prior to study commencement. A structured anonymous questionnaire was used in the present study. The authors made the questionnaire based on existing literatures24–27 (Please see Appendix 1 for more information). “In the beginning, independent experts from internal medicine, family medicine, and public health departments discussed, and the contents were finalized. The structured data collection instrument was translated to Arabic by the bilingual medical team. Next, it was back translated to English, and we found the details are correct. Next, we pretested the questionnaire on 30 hypertensive patients to check respondents’ views for face validity testing. The pilot study of hypertensive patients ensured the data collection tool was precise, and the analysis did not find any missing variables among the completed questionnaires. The Cronbach’s coefficient alpha value of the data collection instrument was 0.76 for the medication adherence section and 0.85 for the Brief Illness Perception Questionnaire (B-IPQ). The data collection tool was divided into three parts. The first part inquired about socio-demographic characteristics such as age, sex, residence, educational status, working status, marital status, monthly income. The second part was composed of questions related to medication adherence. It consists of 8 questions. The hypertensive patients responded either “yes” or “no” for questions 1 to 7 and Item 8 had a 5-point Likert answer scale. We have marked answer “no” as 1 and each “yes” answer is marked as 0 apart from item 5, in which each “yes” answer is marked as 1 and each “no” answer is marked as 0. For Item 8, the code (0–4) has to be standardized by dividing the result by 4 to calculate a summated score. Total scores on this part of the questionnaire range from 0 to 8, with scores of 8 reflecting high adherence, 7 or 6 reflecting medium adherence, and <6 reflecting low adherence. This category by the present study authors is similar to other studies categories that assessed medication adherence among hypertensive and diabetes patients.28,29 The research team executed necessary validation and reliability tests for this structured questionnaire.
The third part was about assessment of illness perception. Assessment of illness perception was done using the B-IPQ, a pretested and validated tool that estimates eight different characteristics of illness perception: consequences, timeline, personal control, treatment control, identity, concerns, understanding, and emotional representation.27 The B-IPQ tool assesses all the stated aspects of illness perception using an 11-point Likert scale. A higher score indicates a more threatening view of the illness, while a lower score indicates a benign view.27
Data Analysis
Data was analyzed using SPSS program, version 23. Mean and standard deviation were calculated for quantitative data. Qualitative data was presented as number and percent. A multivariate binary logistic regression model was applied to identify the independent predictors of medication adherence (High adherence vs low/medium adherence). The basis for the adherence categories is “High medication adherence is associated with the higher odds of better cardiovascular disease outcome”. Furthermore, the basis of the current categories was supported by previous studies by Kim et al, Ho et al, and a medication scale used by Laghous et al28,30,31 In the logistic regression model (enter method), the above-mentioned binary outcome variables were compared with the potential predictor as included in the data collection form. After including all covariates in the analysis, we made the category in each variable as the reference category. We have obtained the odds ratio (OR) and confidence interval (CI) of OR of each variable as the final results from logistic regression after adjusting with other independent variables. An adjusted OR of more than one that did not include a null value (0) in the confidence interval was considered a significant predictor. Furthermore, we have applied Spearman’s test to find the correlation between overall B-IPQ score and medication adherence values. A P value ≤ 0.05 was set as a statistically significant value.
Ethical Considerations
The current survey was done according to the guidelines of the Declaration of Helsinki. The research team ensured the ethical aspects of this survey by, firstly, briefing the objectives of the current study to the selected hypertensive patients before administering the data collection form to them. Secondly, we have taken informed consent from participants willing to participate in the survey. Furthermore, the present survey utilized an anonymous tool to ensure the privacy and confidentiality of participants.
Results
Of the 400 studied population, most of them were males (62.8%), working in government sectors (41.3%), married (78.5%), residing in an urban area (57.8%), and without other chronic diseases (57.5%). The mean age (±SD) of the studied participants was 49.92 ± 10.9 (Table 1).
 |
Table 1 Background Details of Hypertensive Patients Attending Different Primary Health Centers (PHC) in Abha, KSA |
The medication adherence categories of the participated hypertensive patients are presented in Figure 1. Of the sampled participants, more than one-third of the participants (36.3%) were in the high adherence category group, while the remaining participants (63.7%) were either low or medium adherence category.
 |
Figure 1 Medication adherence status of hypertensive patients attending different PHCs in Abha, KSA. |
The research team performed a univariate analysis followed by multivariate analysis. The binary logistic regression analysis revealed that low and medium adherence category is significantly associated with age (adjusted odds ratio [AOR] = 0.96, 95% CI =0.93–0.99, p = 0.021), married participants (ref: unmarried: AOR = 0.42, 95% CI =0.33–0.58, p = 0.001), residing at village (ref: urban: AOR = 1.49, 95% CI =1.14–1.73, p = 0.038), and participants with monthly family income of 5000 to 7000 SAR (ref: > 7000: AOR = 3.06, 95% CI =1.62–5.79, p = 0.001 (Table 2).
 |
Table 2 Correlates of the Low /Medium Medication Adherence Among Hypertensive Patients Attending Different PHCs in Abha, KSA |
Table 3 presents the respondents’ B-IPQ descriptive data (median and IQR). Of the 400 participants, the lowest median (IQR) value was noted in the statement “How much does the illness (hypertension) affects your life?” with a median (IQR) score of 2 (4).
 |
Table 3 Descriptive Data (Median and IQR) of the Brief Illness Perception Questionnaire |
The Spearman correlation test revealed a negligible positive correlation between the overall B-IPQ score and the medication adherence score (r = 0.158, p= 0.002) (Table 4).
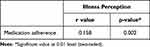 |
Table 4 Correlation Analysis Between Illness Perception and Medication Adherence Scores Among Hypertensive Patients Attending Different PHCs in Abha, KSA |
Discussion
The world hypertension day is celebrated every year on 17th of May with the aim to control, prevent and treat the hypertension. Adhering to the prescribed medication is one of the key elements to achieve it.32 Patients’ adherence to their antihypertensive drugs is of crucial importance in preventing hypertension related complications. The present study assessed the medication adherence among hypertensive patients and its associated factors.
The present study revealed that only 36.3% of hypertensive patients had high adherence practice towards antihypertensive medications. Poor adherence to antihypertensive drugs is not only correlated with poor blood pressure control but also associated with development of morbidities and mortalities.33 A survey conducted by Algabbani et al in the Riyadh region of the KSA found a slightly higher proportion (42%) of the participants aged 18 years and above had high adherence with the prescribed antihypertensive medications.34 However, the finding of the present study was lower than that of other studies conducted among Swedish adults (87.3%),35 and Africa Americans (64.0%).36 The possible reasons for the differences in the percentage of adherence rate could be variation in the methodsapplied to determine medication adherence among various populations. Other reasons could be due to variation in the educational level of the participants, complexity of drug regimens, participants’ knowledge, and health conditions. In the present survey, a significant association was revealed between residence and medication adherence. The participants who lived in rural regions were nearly 2 times as possible to have low and medium medication adherence as compared to those who lived in urban areas. This is consistent with a study conducted in northwest Ethiopia.37 This may be because rural residents are farmers busy with their agricultural land and they may forget taking their hypertensive medications on time. In addition, differences in educational levels and access to different health services may be other probable factors contributed for the variations, as urban residents have more access to different health services and more likely to be more educated than rural residents. Antihypertensive drugs are long term medications that requires continued replenishing. The cost of antihypertensive medications is one of the barriers that hinders the continuity of treatment for patients with low monthly income.38 Hypertensive patients with low monthly income are fighting to adhere to antihypertensive medications because of their cost.38 The present study revealed that monthly income is a significant predictor for adherence to antihypertensive medications. Participants with low income in this study were more liable to low or medium medication adherence. This is consistent with other study findings.39,40 The results of the present study showed that marital status was negatively associated with medication adherence as married participants were more liable to low or medium medication adherence. This finding is contrary to the results of the earlier surveys which showed that married respondents had adherence levels more than divorced, widowed, or not married.40,41 The above difference in the attitude may be attributed to the fact that married participants in the present study are busy in their life and do not care on taking the medicine on time. This is in addition to the medicine may be costly for them. The present explored that age is one of the significant predictors of medication adherence (AOR = 0.96, 95% CI =0.93–0.99, p = 0.021). The present study’s findings related to age were consistent with the previous studies by Hyre et al in New Orleans and Lee et al in China.42,43 This may be due to possible comorbidities associated with aged patients. Hence, they perceive themselves as sicker and follow a better medication adherence practice to the antihypertensive regime prescribed by the physicians. The current study revealed a significant correlation between medication adherence and illness perception which is similar with the findings of previous surveys indicating high perception of illness will lead to high level of medication adherence.44–46 However, a study conducted by Saarti et al revealed that medication adherence by hypertensive patients were associated with treatment satisfaction rather than illness perception.20 The dissimilarities in the findings may be because of using different questionnaire to estimate illness perception and medication adherence.
Limitations
The research team executed this study with a standard methodology. However, certain constraints need to be considered while reading the results of this survey. Firstly, the present cross-sectional study assessed only association, not the causation. This study used a self-reported survey questionnaire. Hence, bias related to self-reported surveys like recall, exaggerated response, and selection bias can occur.
Conclusion
The present study revealed that low medication adherence practice among hypertensive patients. This low adherence is significantly associated with the age, monthly income, people in village area, and married participants. Hence, it is recommended to raise awareness among the hypertensive patients on the importance of adhering to the medications prescribed by the treating physicians. Moreover, the concerned authorities need to develop structured intervention and health education programs to target low and medium-adherence groups. A multidisciplinary team approach with greater participation of patients in managing the hypertensive status should be encouraged to promote better medication adherence. Finally, future studies are warranted in other healthcare facilities, including private clinics in other KSA regions.
Acknowledgments
The authors wish to thank all the participants for their willingness to participate in the study. Also, we wish to extend our sincere thanks to ministry of health, Asir region, Saudi Arabia for their help for this survey.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Healthcare adherence: section I setting the scene. World Health Organization; January 25, 2022. Available from: https://www.who.int/chp/knowledge/publications/adherence_Section1.pdf.
2. Rodriguez-Saldana J. Patient Adherence: Challenges, Myths, and Realities. Springer International Publishing; 2019:381–400.
3. Kvarnström K, Airaksinen M, Liira H. Barriers and facilitators to medication adherence: a qualitative study with general practitioners. BMJ Open. 2018;8(1):e015332. doi:10.1136/bmjopen-2016-015332
4. Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
5. Kleinsinger F. The unmet challenge of medication nonadherence. Perm J. 2018;22(3):18–033. doi:10.7812/tpp/18-033
6. Aznar-Lou I, Fernández A, Gil-Girbau M, et al. Impact of initial medication non-adherence on use of healthcare services and sick leave: a longitudinal study in a large primary care cohort in Spain. Br J Gen Pract. 2017;67(662):e614–e622. doi:10.3399/bjgp17x692129
7. World Health Organization. Hypertension. World Health Organization; January 22, 2022. Available from: https://www.who.int/health-topics/hypertension#tab=tab_1.
8. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–237. doi:10.1038/s41581-019-0244-2
9. NCD-RisC. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–980. doi:10.1016/s0140-6736(21)01330-1.
10. Aldiab A, Shubair MM, Al-Zahrani JM, et al. Prevalence of hypertension and prehypertension and its associated cardioembolic risk factors; a population based cross-sectional study in Alkharj, Saudi Arabia. BMC Public Health. 2018;18(1):1327. doi:10.1186/s12889-018-6216-9
11. Aljuraiban GS, Al Slail FY, Aldhwailea SK, et al. May measurement month 2019: an analysis of blood pressure screening results from Saudi Arabia. Eur Heart J Suppl. 2021;23(Supplement_B):B128–B130. doi:10.1093/eurheartj/suab029
12. Yagoub U, Saiyed NS, Al Qahtani B, Al Zahrani AM, Birema Y, Al Hariri I. Investigating the incidence and risk factors of hypertension: a multicentre retrospective cohort study in Tabuk, Saudi Arabia. PLoS One. 2022;17(1):e0262259. doi:10.1371/journal.pone.0262259
13. Almalki ZS, AlOmari BA, Alshammari T, et al. Uncontrolled blood pressure among hypertensive adults with rheumatoid arthritis in Saudi Arabia: a cross-sectional study. Medicine. 2022;101(4):e28763. doi:10.1097/MD.0000000000028763
14. Al-Qahtani AM. Prevalence and determinants of blood pressure control among hypertensive patients in primary care centers, Najran, Saudi Arabia. Biomed Pharmacol J. 2018;11(2):821–825. doi:10.13005/bpj/1437
15. Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–622. doi:10.2147/ppa.S34704
16. Mamaghani EA, Hasanpoor E, Maghsoodi E, Soleimani F. Barriers to medication adherence among hypertensive patients in deprived rural areas. Ethiop J Health Sci. 2020;30(1):85–94. doi:10.4314/ejhs.v30i1.11
17. Khayyat SM, Khayyat SM, Hyat Alhazmi RS, Mohamed MM, Abdul Hadi M. Predictors of medication adherence and blood pressure control among Saudi hypertensive patients attending primary care clinics: a cross-sectional study. PLoS One. 2017;12(1):e0171255. doi:10.1371/journal.pone.0171255
18. Basu S, Poole J. The brief illness perception questionnaire. Occup Med. 2016;66(5):419–420. doi:10.1093/occmed/kqv203
19. Salome Oyiela O, Deborah Kemunto K. Illness Perceptions and adherence to medication regimen among hypertensive patients attending a county referral hospital in Kenya. J Hypertens Manag. 2021;7(1):1–6. doi:10.23937/2474-3690/1510059
20. Saarti S, Hajj A, Karam L, et al. Association between adherence, treatment satisfaction and illness perception in hypertensive patients. J Hum Hypertens. 2016;30(5):341–345. doi:10.1038/jhh.2015.86
21. Vrijens B, Antoniou S, Burnier M, de la Sierra A, Volpe M. Current situation of medication adherence in hypertension. Front Pharmacol. 2017;8:100. doi:10.3389/fphar.2017.00100
22. Teh XR, Lim MT, Tong SF, Husin M, Khamis N, Sivasampu S. Quality of hypertension management in public primary care clinics in Malaysia: an update. PLoS One. 2020;15(8):e0237083. doi:10.1371/journal.pone.0237083
23. Waked K, Nagge J, Grindrod K. Managing hypertension in primary care. Can Fam Physician. 2019;65(10):725–729.
24. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
25. Uchmanowicz B, Jankowska EA, Uchmanowicz I, Morisky DE. Self-reported medication adherence measured with morisky medication adherence scales and its determinants in hypertensive patients aged ≥60 years: a systematic review and meta-analysis. Front Pharmacol. 2019;10:168. doi:10.3389/fphar.2019.00168
26. Chan AHY, Horne R, Hankins M, Chisari C. The Medication Adherence Report Scale: a measurement tool for eliciting patients’ reports of nonadherence. Br J Clin Pharmacol. 2020;86(7):1281–1288. doi:10.1111/bcp.14193
27. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi:10.1016/j.jpsychores.2005.10.020
28. Laghousi D, Rezaie F, Alizadeh M, Asghari Jafarabadi M. The eight-item Morisky Medication Adherence Scale: validation of its Persian version in diabetic adults. Caspian J Intern Med. 2021;12(1):77–83. doi:10.22088/cjim.12.1.77
29. Alotayfi MJY, Alsohaimi SA, Al-Qadi BK, et al. Poor compliance to anti-hypertensive drugs in Saudi Arabia. Egypt J Hosp Med. 2018;73(5):6696–6701. doi:10.21608/ejhm.2018.16015
30. Kim J, Combs K, Downs J, Tillman F. Medication adherence: the elephant in the room. US Pharm. 2018;43(1):30–34.
31. Ho PM, Bryson CL, Rumsfeld JS. Medication Adherence. Circulation. 2009;119(23):3028–3035. doi:10.1161/CIRCULATIONAHA.108.768986
32. PAHO/WHO. World hypertension day. World Health Organization; March 15, 2022. Available from: https://www.paho.org/en/world-hypertension-day.
33. Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19(11):1190–1196. doi:10.1016/j.amjhyper.2006.04.006
34. Algabbani FM, Algabbani AM. Treatment adherence among patients with hypertension: findings from a cross-sectional study. Clin Hypertens. 2020;26(1):18. doi:10.1186/s40885-020-00151-1
35. Hedna K, Hakkarainen KM, Gyllensten H, et al. Adherence to antihypertensive therapy and elevated blood pressure: should we consider the use of multiple medications? PLoS One. 2015;10(9):e0137451. doi:10.1371/journal.pone.0137451
36. Tsadik DG, Berhane Y, Worku A. Adherence to antihypertensive treatment and associated factors in central Ethiopia. Int J Hypertens. 2020;2020:9540810. doi:10.1155/2020/9540810
37. Teshome DF, Bekele KB, Habitu YA, Gelagay AA. Medication adherence and its associated factors among hypertensive patients attending the Debre Tabor General Hospital, northwest Ethiopia. Integr Blood Press Control. 2017;10:1–7. doi:10.2147/ibpc.S128914
38. Herttua K, Tabák AG, Martikainen P, Vahtera J, Kivimäki M. Adherence to antihypertensive therapy prior to the first presentation of stroke in hypertensive adults: population-based study. Eur Heart J. 2013;34(38):2933–2939. doi:10.1093/eurheartj/eht219
39. Khanam MA, Lindeboom W, Koehlmoos TL, Alam DS, Niessen L, Milton AH. Hypertension: adherence to treatment in rural Bangladesh–findings from a population-based study. Glob Health Action. 2014;7(1):25028. doi:10.3402/gha.v7.25028
40. Hamza SA, El Akkad RM, Abdelrahman EE, Abd Elghany SA. Non adherence to Antihypertensive medications among hypertensive elderly patients in outpatient geriatric clinic. Arch Gerontol Geriatr. 2019;6(1):1–7. doi:10.21608/ejgg.2019.30888
41. Alhaddad IA, Hamoui O, Hammoudeh A, Mallat S. Treatment adherence and quality of life in patients on antihypertensive medications in a Middle Eastern population: adherence. Vasc Health Risk Manag. 2016;12:407–413. doi:10.2147/vhrm.S105921
42. Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens. 2007;9(3):179–186. doi:10.1111/j.1524-6175.2007.06372.x
43. Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8(4):e62775. doi:10.1371/journal.pone.0062775
44. Shakya R, Shrestha S, Gautam R, et al. Perceived illness and treatment adherence to hypertension among patients attending a tertiary hospital in Kathmandu, Nepal. Patient Prefer Adherence. 2020;14:2287–2300. doi:10.2147/ppa.S270786
45. Rajpura JR, Nayak R. Role of illness perceptions and medication beliefs on medication compliance of elderly hypertensive cohorts. J Pharm Pract. 2014;27(1):19–24. doi:10.1177/0897190013493806
46. Hsiao CY, Chang C, Chen CD. An investigation on illness perception and adherence among hypertensive patients. Kaohsiung J Med Sci. 2012;28(8):442–447. doi:10.1016/j.kjms.2012.02.015
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
