Back to Journals » Journal of Healthcare Leadership » Volume 14
Medical Professionalism in the Provision of Clinical Care in Healthcare Organizations
Authors Bhardwaj A
Received 29 July 2022
Accepted for publication 17 October 2022
Published 26 October 2022 Volume 2022:14 Pages 183—189
DOI https://doi.org/10.2147/JHL.S383069
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Russell Taichman
Anish Bhardwaj
Departments of Neurology, Neurosurgery, and Neurobiology, University of Texas Medical Branch (UTMB), Galveston, TX, 77555, USA
Correspondence: Anish Bhardwaj, University of Texas Medical Branch (UTMB), 9.128 John Sealy Annex, Route 0539, 301 University Blvd, Galveston, TX, 77555, USA, Tel +1-409-772-8068, Email [email protected]
Abstract: Medical professionalism is critical toward provision of safe, effective, patient-centered, timely, efficient, and equitable clinical care delivery. The basic tenets of medical professionalism are deeply embedded in the historical context via oaths and expectations. However, standardization of professional conduct and its integration by providers have been a challenge due to the evolving complexity of healthcare organizations (HCOs) and academic medical institutions (AMIs). Increasing heterogeneity of the workforce leads to greater complexity in collaborative teamwork. In this evolving landscape, violations of professional conduct demand closer scrutiny along professional and personal lines. Likewise, actions among minority groups pose challenges between integration and inclusion of certain professional interactions and conduct. Recently, in American HCOs and AMIs, there has been a renewed emphasis on accountability and managing unprofessional behaviors in the delivery of clinical care. This descriptive literature-based treatise explicates the professionalism construct in its historical milieu, underscores key facets of professionalism, highlights principal drivers of unprofessional behaviors, and posits solutions for enhancing and nurturing professionalism in the delivery of clinical care in HCOs and AMIs by a diverse workforce of healthcare providers.
Keywords: professionalism, workforce, healthcare, diversity, inclusion
Introduction and Historical Context
For twenty-four centuries, the Hippocratic oath sworn by physicians has provided the broader precepts of medical professionalism in the delivery of clinical care-ie, “beneficence, non-maleficence, and confidentiality.”1,2 Rooted in the concepts of morality and virtue,3,4 these core components have been extrapolated to construct formal and informal frameworks that have been incorporated in mission statements, policies, and procedures of Health Care Organizations (HCOs) and Academic Medical Institutions (AMIs) and adopted by professional medical societies as well. The increasing complexity of healthcare delivery over the past few decades, due mainly to corporatization, has underscored the importance of more cohesive delivery of safe, effective, patient-centered, timely, efficient, and equitable clinical care5 that is longitudinal, comprehensive, and multidisciplinary. Additionally, rapidly disseminating new knowledge, data acquisition, and skills commensurate with technological advances have generated new demands and expectations from patients, HCOs and AMIs, as well as from the medical community in general.6–10 Other healthcare professionals (eg, nurses, pharmacists, physical and occupational therapists, etc.) have similarly developed guidelines for achieving these goals. However, the growing intricacies in healthcare delivery pose significant challenges.6,7 This literature-based descriptive treatise expounds the professionalism concept in its historical milieu and explores the elements of an evolving operational construct of professionalism for today. It further highlights the fundamental drivers of unprofessional behaviors and posits solutions for promoting a culture of professionalism in the delivery of clinical care in HCOs and AMIs in the context of a diverse workforce of healthcare providers.
Key Facets in the Rubric of Medical Professionalism
Since the times of Hippocrates and the Medical School of Cos, professionalism has been a foundational principle in the practice of medicine serving as “the basis of medicine’s contract with society.”1,2,11 This informal agreement was rejuvenated in the 1990s when leaders in the medical field delineated a more refined set of ethical values and competency standards that are to be expected in the delivery of clinical care.12–15 Incrementally, these core competencies have been included in medical education and training, both undergraduate and graduate, with an emphasis on acceptable professional behaviors and the pursuit of ethical principles in the effective and safe delivery of clinical care as well as for conduct in the public sphere.3,16,17 The core components of this framework of professionalism include altruism, dependability, responsibility, quest for excellence, appreciation of duty, agency, honesty, rectitude and integrity, collegiality, respect for others, continuous learning and improvement, and humility.3 A simplistic rubric and key facets of medical professionalism are depicted in Figure 1.
 |
Figure 1 Key facets of medical professionalism. |
With the increasing complexity of HCOs and AMIs, many institutions such as Vanderbilt University, Dartmouth Geisel School of Medicine, and the University of Chicago18–21 have incorporated professionalism charters in their institutional by-laws. The overarching focus has been on infrastructure in the pursuit of accountability and reliability centered on three areas: people (i.e., committed leadership, implementing teams, project champions), organization (i.e., vision, mission, values, policies and procedures, etc.), and systems. (i.e., tools, data, metrics, reliable review processes, and training)18,19
Some institutions have further enhanced this thematic paradigm by building a culture of “safety” that safeguards psychological wellbeing and nurtures trust among key team members and stakeholders. The Vanderbilt Center for Patient and Professional Advocacy established in 1989 has developed a stepwise iterative process shifting from reactive crisis management triggered by poor patient outcomes to preventive measures by preemptively identifying clinicians at risk for developing unprofessional behaviors and by pursuing professional accountability with well thought-out action-oriented systems.18,19 The critical facets of professionalism have been further refined to include effective communication, availability, teamwork, self-awareness, respect, and technical and cognitive competence.18
Major Drivers of Unprofessional Behaviors
The principal drivers of unprofessional conduct vary. Triggers may include extra workload due to limited staff, chronic fatigue and sleep deprivation leading to burnout and low self-esteem, and a variety of societal and personal stressors (eg, fractured relationships, etc.).22,23 Providers from certain subspecialties (eg surgery, critical care, emergency room, etc.) and locations (operating room, critical care units, etc.) may be susceptible to developing unprofessional behaviors owing to high-stress scenarios and physical environments. Although unproven, there is likely considerable correlation between the propensity for burnout syndrome and unprofessional behaviors associated with certain personality traits (eg, introversion and neuroticism). These behaviors may include severe self-criticism, over-commitment, naivete, pedantry, work-life imbalance, adjustment disorders, toxic and substance abuse, poor physical health, and cognitive decline.23
Factors attributable to HCOs and AMIs also play a significant role. These include unsupportive institutional leadership, poor organizational culture and work environment, tolerance of unprofessional behaviors, bigotry, unconscious bias, tolerance for micro-aggressions, scant recognition for superior performance and model behaviors, deficiencies in opportunities for professional growth and development, lack of social support systems, resource constriction, suboptimal operational procedures, stressors from discordance with hospital administrators, and loss of autonomy and decision-making capabilities23–25 (Figure 2).
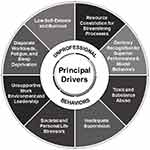 |
Figure 2 Principal drivers of unprofessional behaviors. |
Mitigating Unprofessional Behaviors
A plethora of evidence demonstrates that unprofessional behaviors by healthcare providers result in poorer outcomes including increased surgical site infections, readmissions, and medical complications, psychological and financial harm to patients, exposure to malpractice claims, diminished job satisfaction, and increased rates of attrition among team members. Thus, the costs of ignoring unprofessional behaviors can be high.26,27
Rather than a punitive approach to behavioral infractions, however, nurturing a culture of professionalism and crafting underpinnings that are highly supportive to all stakeholders should be the overall goals of an HCO or AMI. The overarching principle should be a focus on an iterative process of continuous improvement that typifies a “Learning Organization.” Collaboration among various departments and human resources to cultivate a supportive culture with preventive measures targeted to the specific individual-based and organizational-level solutions is crucial. Multimodal approaches focused on trustworthy institutional leadership, governance structure, operations, and processes in HCOs are also essential elements for promoting professionalism.18 Specific issues include addressing disparate workloads, redefining duty hour limits, suitable allocation of functional positions, shared decision-making at the organizational level, and addressing perceived loss of control and autonomy through team building and collaborative partnerships. At the individual level, the focus must be on mindfulness, coping approaches to stressful situations, fostering physician engagement and leadership in establishing work requirements, focusing on issues regarding life-work balance with attention to self-care and introspection on values and life priorities, and seeking support from staff assistance and wellness programs (eg, counseling).23
The commitment of institutional leadership to nurturing a culture of professionalism is paramount. Effective physician leaders have moved away from the “cult of personality” and traditional “autocratic or authoritative” style to a more collaborative, servant model of leadership with empathetic listening to diverse viewpoints, consensus-building and collective decision-making that enhance teamwork in healthcare delivery. High emotional intelligence, self-awareness, and humility are key characteristics that will ensure success for leaders in healthcare.3 Also of note, the Hippocratic tradition promotes paternalism which has been characterized by medical ethicists as “authoritarian and insensitive to social needs” and which has underscored the importance of patient autonomy in medical decision-making.1
As posited by Chestnut,3 on the individual level, medical professionalism is a competency (ie, a commitment and skill) that must be nurtured over a lifetime. Many of the specific actions involved can be processed in parallel or sequentially with collective professional self-regulation3 as operationalized by the Vanderbilt Center for Patient and Professional Advocacy Program.26 These steps should include the following (Figure 3):
- Periodic workshops, seminars, and rigorous, mandatory institutional compliance training programs (eg, unconscious bias, diversity, inclusivity, teamwork, etc.) for healthcare providers.
- Creating clear algorithms for reporting systems for breaches in professional behavior. This can be grouped according to those generated by patients and their families, triaged, and channeled through Patient Services for time-sensitive response and action. Unprofessional behaviors generated by healthcare team member(s) can be brought directly to the attention of a supervisor or through an anonymous reporting system for appropriate triage. The main advantage of anonymous reporting systems is deterrence from possible retaliation, while its disadvantage is that the credibility of complaints may be dubious and may propagate a culture of “distrust” within the organization via the “tyranny of anonymity.”
- Appointing an Institutional Professionalism Committee (ie, 8–10 members from various domains of clinical service) to address cases of recurrent professionalism issues. This committee should develop a milestone-driven plan of improvement (eg, referrals to and working closely with the Institutional Wellness and Staff Assistance Programs, neuropsychiatric and cognitive evaluation, medical consultation and evaluation, toxicology screen, etc). The committee would also recommend disciplinary action, probation, suspension, or dismissal to the Institutional Medical Board or reporting to State Medical Boards and other national databases for healthcare providers. Confidentiality in this process is paramount. A graded “pyramidal” or escalating approach includes informal conversation for isolated behavioral infractions, formal intervention if patterns of poor behavior persist, and disciplinary intervention for a recalcitrant provider with repeated misbehaviors. Such a stepwise system has been successfully instituted in several HCOs and AMIs (eg, Vanderbilt’s Center for Patient and Professional Advocacy Program).18,19,26
- Incorporating a professionalism charter into the institutional medical staff by-laws.
- Establishing a no-tolerance policy for sexual harassment and racial and gender discrimination commensurate with the institutional human resources policies and procedures.
- Role modeling for students and trainees by educators with adequate supervision and longitudinal evaluations of professionalism as part of core competencies during their training. Trainees in residency programs frequently perceive gaps in teaching professionalism, developing communication skills with patients from diverse cultural backgrounds, and interprofessional teamwork.17,28 In one study, residents noted that only 25% of their faculty modeled professional behaviors all the time and over 50% of faculty exhibited poor role modeling.28
- Nurturing formal mentor-mentee programs that will augment the growth of core leaders and ambassadors of professionalism with formal courses by senior healthcare providers such as the Academy of Master Clinicians and the Physician Leadership Academy.
- Establishing institution-wide recognition and awards for professionalism for model behaviors (ie, Respect, Work Ethic, Collegiality, Competence, Integrity, Positivity, Application to Task, Quest for Improvement and Excellence).
 |
Figure 3 Nurturing a culture of medical professionalism in HCOs. |
Challenges, Controversies and Evolving Issues
Despite its positive connotations, professionalism has become an elusive concept that risks being distorted or underused.11,29,30 Beyond its historical construct, professionalism in medicine has evolved to encompass a wide-ranging set of behaviors, verbal and non-verbal communication, affect, attire, and hierarchical reporting structures.8,30 A recent population-based survey that included 487 respondents from the general public in the US “rated physicians wearing casual attire as being less professional and experienced than those wearing a white coat.”31 Noted institutions (eg, Johns Hopkins University, Oregon Health and Science University) have codified institutional policies on dress codes, body art and tattoos, body odor and use of fragrance, and even nail care as Professional Appearance Standards for clinical healthcare providers.32,33 Some healthcare providers contend that rigid policies such as dress codes infringe on their basic human rights of freedom of speech and expression.
Secondly, it has been suggested that the present operative set of professional behavioral norms has been extrapolated from a more homogeneous population of physicians comprised predominantly of Caucasian males with relatively few females and cultural minority groups represented in positions of leadership and influence.8 With increasing diversity of the workforce, phenotypic behaviors (eg, tone and tenor of speech, sense of humor, loud laughter, verbal, and non-verbal communication, hairstyle and attire, visible tattoos, body piercings, etc.), that may be related to race, place of origin, religion, ethnicity, sexual orientation, gender identification, or individual views on freedom of speech and expression, may be erroneously labeled and perceived as disruptive and unprofessional behaviors. Stereotyping of such behaviors is not uncommonly encountered, further exacerbating perception of bias among subgroups in the healthcare team. At present, there is little consensus on integrating inclusion as it relates to operationalizing professionalism within the healthcare work and learning environments. In a recent prospective quantitative study utilizing the Diversity Engagement Survey, an effective tool to study the engagement of different groups in organizations while operationalizing professionalism, minority groups (eg, females, sexual orientation, racial and ethnic) were reported to manifest unprofessional behaviors through bias and discrimination.8 A significant proportion of individuals in these minority groups perceived greater infringements on their professional boundaries and increased scrutiny that culminated in their leaving a position.8 It has been postulated that the underlying substrate for these experiences by minority groups is decades of “systematic segregation, discrimination, culture, tradition, and elitism” in the practice of medicine.8,34–36 Whatever the cause, the disparate application of professional standards of conduct can be deleterious for delineating identity and individuality particularly among marginalized and minority groups, deter diversity among healthcare workforce, and augment conformity.37 It is proposed that healthcare environments must nurture an ethos that embraces a broad spectrum of cultural practices and traditions to enhance diversity and inclusivity while respecting the core values of professionalism.8 Ongoing and future research in this area will augment our understanding of complex interplay of heterogenous traditions and cultures in the rubric of medical professionalism.
Conclusions and Future Directions
Professionalism by healthcare providers has a profound effect across the continuum of delivery of clinical care to patients, their families, and the community in general. The basic tenets and expectations of professionalism for healthcare providers remain deeply embedded in tradition. Regulation of professional behaviors and their assimilation by providers has been challenging due to the multitude of environmental intricacies in healthcare delivery as well as to evolving sociocultural values and expectations. Professionalism is an aptitude that must be cultivated by healthcare providers through the course of a lifetime. HCOs and AMIs must promote a supportive and nurturing culture conducive to “continuous learning and improvement” while holding healthcare providers accountable for behavioral infractions. HCOs and AMIs should also promote inclusion and diversity by embracing different cultures, beliefs, and traditions and their associated behaviors to ensure that minority groups are not marginalized. Ultimately, professionalism in the delivery of healthcare is the key facet in fulfilling the Institute of Medicine’s5 goals of providing “safe, effective, patient-centered, timely, efficient, and equitable” care to patients and their families.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Askitopoulou H, Vgontzas AN. The relevance of the Hippocratic Oath to the ethical and moral values of contemporary medicine. Part I: the Hippocratic Oath from antiquity to modern times. Eur Spine J. 2018;27:1481–1490. doi:10.1007/s00586-017-5348-4
2. Askitopoulou H, Vgontzas AN. The relevance of the Hippocratic Oath to the ethical and moral values of contemporary medicine. Part II: interpretation of the Hippocratic Oath-today’s perspective. Eur Spine J. 2018;27:1491–1500. doi:10.1007/s00586-018-5615-z
3. Chestnut D. On the road to Professionalism. Anesthesiology. 2017;126:780–786. doi:10.1097/ALN.0000000000001545
4. Professionalism Initiative. KU school of medicine office of student affairs. Available from: https://www.kumc.edu/school-of-medicine/osa/policies-and-professionalism/professionalism.html.
5. Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001.
6. Barr DA. Introduction to US health policy. In: The Organization, Financing, and Delivery of Health Care in America.
7. Wilensky SE, Teitelbaum JB. Essential of Health Policy and Law.
8. Shi L, Singh DA. Delivering Health Care in America: A Systems Approach.
9. Marks L The landscape of academic medicine and health care in the United States. Pharos; 2020:2–8.
10. Bhardwaj A. What’s new in academic international medicine? The evolving terrain of 2019 American academic medicine. Int J Acad Med. 2019;5(2):85. doi:10.4103/IJAM.IJAM_25_19
11. Alexis DA, Kearney MD, Williams JC, et al. Assessment of perceptions of professionalism among faculty, trainees, staff, and students in a large university-based health system. JAMA Network Open. 2020;3(11):e2021452. doi:10.1001/jamanetworkopen.2020.21452
12. Lesser CS, Lucey CR, Egener B, et al. A behavioral and systems view of professionalism. JAMA. 2010;304:2732–2737. doi:10.1001/jama.2010.1864
13. American Board of Internal Medicine (ABIM) Foundation: American College of Physicians-American Society of Internal Medicine (ACP-ASIM) Foundation, European Federation of Internal Medicine. Medical Professionalism in the new millennium: a physician Charter. Ann Intern Med. 2002;136:243–246. doi:10.7326/0003-4819-136-3-200202050-00012
14. Egener BE, Mason DJ, McDonald WJ, et al. The charter on professionalism for health care organizations. Acad Med. 2017;92:1091–1099. doi:10.1097/ACM.0000000000001561
15. Dupree E, Anderson R, McEvoy MD, et al. Professionalism: a necessary ingredient in a culture of safety. Jt Comm J Qual Patient Saf. 2011;37(10):447–455. doi:10.1016/s1553-7250(11)37057-2
16. Hafferty FW. Academic Medicine and Medical Professionalism: a legacy and portal into an evolving field of educational scholarship. Acad Med. 2018;93:532–536. doi:10.1097/ACM.0000000000001899
17. Berger AS, Niedra E, Brooks SG, et al. Teaching professionalism in postgraduate medical education: a systematic review. Acad Med. 2020;95:938–945. doi:10.1097/ACM.0000000000002987
18. Vanderbilt center for patient and professional advocacy. Available from: https://prd-medweb-cdn.s3.amazonaws.com/documents/cppa/files/CPPA%20INTRO%20100119.pdf.
19. Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Aca Med. 2007;82:1040–1048. doi:10.1097/ACM.0b013e31815761ee
20. Humphrey HJ, Smith K, Reddy S, et al. Promoting an environment of professionalism: the University of Chicago “Roadmap”. Acad Med. 2007;82:1098–1102. doi:10.1097/01.ACM.0000285344.10311.a8
21. Dartmouth Geisel School of Medicine. Office of Faculty Affairs. Policy on expectations for professionalism for faculty, non-faculty academics, and staff of the Geisel School of Medicine at Dartmouth. Available from: https://c8y.doxcdn.com/image/upload/v1/Press%20Blog/Research%20Reports/Doximity-Compensation-Report-2021.pdf.
22. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences, and solutions. J Intern Med. 2018;283:516–529. doi:10.1111/joim.12752
23. Bhardwaj A. COVID-19 pandemic and physician burnout: ramifications for healthcare workforce in the United States. J Healthc Leadersh. 2022;14:91–97.
24. Bhardwaj A. Alignment between physicians and hospital administrators: historical perspective and future directions. Hosp Pract. 2017;45(3):81–87. doi:10.1080/21548331.2017.1327302
25. Bhardwaj A. Organizational culture and effective leadership in academic medical institutions. J Healthc Leadersh. 2022;14:25–30. doi:10.2147/JHL.S358414
26. Dmochowski RR, Cooper WO, Hickson DB. Professionalism, leadership, and a pilfered apple. Jt Comm J Qual Patient Saf. 2022;48:1–5. doi:10.1016/j.jcjq.2021.11.004
27. Cooper WO, Hickson GB, Guillamondegui OD, et al. Professionalism of admitting and consulting services and trauma patient outcomes. Ann Surg. 2022;275:883–890. doi:10.1097/SLA.0000000000005416
28. Reynolds PP, White C, Martindale JR. Residents’ perspective on professionalism in the learning environment. Curr Probl Pediatr Adolesc Health Care. 2019;49:84–91. doi:10.1016/j.cppeds.2019.03.004
29. Swick HM. Toward a normative definition of medical professionalism. Acad Med. 2000;75:612–616. doi:10.1097/00001888-200006000-00010
30. DeAngelis CD. Medical Professionalism. JAMA. 2015;313:1837–1838. doi:10.1001/jama.2015.3597
31. Xun H, Chen J, Sun AH, et al. Public perceptions of physician attire and professionalism in the US. JAMA Network Open. 2021;4:e2117779. doi:10.1001/jamanetworkopen.2021.17779
32. Johns Hopkins University School of medicine work rule-clinical operations. Available from: https://hr.jhu.edu/wp-content/uploads/2019/06/SignedWorkRuleAmbulatoryProfessionalorClinical.pdf.
33. Oregon health and science university healthcare professional appearance policy. Available from: https://www.ohsu.edu/sites/default/files/2018-10/professional-appearance-policy-HC-HR-101-RR.pdf.
34. Nivet MA. Minorities in academic medicine: review of the literature. J Vasc Surg. 2010;51:535–585. doi:10.1016/j.jvs.2009.09.064
35. Fang D, Moy E, Colburn L, Hurley J. Racial and ethnic disparities in faculty promotion in academic medicine. JAMA. 2000;280:1085–1092. doi:10.1001/jama.284.9.1085
36. Lee JH. The weaponization of medical professionalism. Acad Med. 2017;92:579–580. doi:10.1097/ACM.0000000000001647
37. Nurok M, Lee TH. Transforming culture in health care. N Eng J Med. 2019;381:2173–2175. doi:10.1056/NEJMms1906654
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
