Back to Journals » Patient Preference and Adherence » Volume 17
Medical Conditions and Preference of Traditional Chinese Medicine: Results from the China Healthcare Improvement Evaluation Survey
Authors Zhao Q , Guo R , Fan Z , Hu L , Hu Z , Liu Y
Received 22 November 2022
Accepted for publication 14 January 2023
Published 24 January 2023 Volume 2023:17 Pages 227—237
DOI https://doi.org/10.2147/PPA.S398644
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Qi Zhao, Ran Guo, Zixuan Fan, Linlin Hu, Zhimin Hu, Yuanli Liu
School of Health Policy and Management, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, 100730, People’s Republic of China
Correspondence: Yuanli Liu, Chinese Academy of Medical Sciences and Peking Union Medical College, No. 9 Dongdansantiao, Dongcheng District, Beijing, 100730, People’s Republic of China, Email [email protected]
Purpose: Although complementary and alternative medicine (CAM) is used around the world, there has been a lack of comprehensive understanding of major factors affecting patients’ decision to use CAM. This study aimed to describe the preferences of Chinese patients regarding what conditions they will use Traditional Chinese Medicine (TCM) for and to determine the factors associated with these preferences.
Patients and Methods: This study used data from the China Healthcare Improvement Evaluation Survey in January 2021, a national cross-sectional survey conducted at 163 hospitals across 31 provinces. A convenient sampling method was used to conduct the patient satisfaction survey, and 28,993 patients in an ambulatory setting constituted our study sample on TCM use. A multiple-choice question regarding TCM listed nine medical conditions and asked the patient about what condition he/she and his/her family members would use TCM. In addition to descriptive statistics, we used a binary logistic regression model to investigate factors affecting the likelihood of patients’ decision to use TCM for multiple conditions.
Results: The majority of the surveyed patients (76.3%) would use TCM for the purpose of disease prevention, and more than half (67.3%) for multiple medical/health conditions, 34.0% for dealing with chronic diseases, 33.0% for common symptoms, 26.9% for rehabilitation, and 26.3% for sleeping disorder. Female and older patients, as well as patients with a higher education level, urban residency, and higher family income, were found to be associated with a higher probability of using TCM for multiple conditions than their counterparts (odd ratios [OR]> 1, P< 0.05).
Conclusion: This study reveals a preference for TCM in a large sample of Chinese patients, especially used for prevention. Generally, patients with a higher socioeconomic status had a more positive attitude toward TCM.
Keywords: use of traditional Chinese medicine, medical conditions, consideration
Introduction
Complementary and alternative medicine (CAM), which is an alternative to mainstream health care, is widely used worldwide as an integral part of the medical system. It includes treatments from a variety of histories and cultures. According to the WHO, CAM has a long history of use in health maintenance and disease prevention and treatment.1 It represents the sum total of the knowledge, skill, and practices of health maintenance as well as of the prevention, diagnosis, improvement, and treatment of physical and mental illness.2
The prevalence rates of CAM use can be expected to differ between countries because of economic, social, and cultural factors. In the past two decades, the prevalence of CAM used by the general populations was 10.0–48.7% in some European countries,3 while the rate was higher in Asian countries (South Korea: 45.8–69%, Japan: 76%, Lao PDR: 77%, Malaysia: 55.6%).3–5
As one form of CAM, Traditional Chinese Medicine (TCM) is one of the popularly used medical/health practices throughout the world.1 TCM is based on unique views on life, on fitness, on diseases, and on the prevention and treatment of diseases that have been formed during its long history of absorption and innovation.6 TCM combines the use of Chinese herbal medicines, acupuncture and moxibustion, massage (tuina), and therapeutic mind/body practices.7 In China, TCM is not considered an alternative form of treatment, as opposed to western medicine, but an integrative complement to western medicine,8 and it is emphasized that equal importance should be placed on both TCM and western medicine in China’s medical system.
In 2020, China counted 4426 TCM hospitals, which amounts to 12.5% of the total number of hospitals, while 86.7% among all types of hospitals in China had dedicated TCM departments. The number of clinical visits to TCM hospitals was approximately 518.5 million in 2020, about 15.6% of the total number of clinical visits to hospitals of all types.9 This proportion shows an upward trend year by year.
In previous studies, more attention has been paid to the application of TCM from the perspective of disease treatment, such as using TCM for cancer treatment10–12 or molecular studies of herbal drugs used to treat a particular disease.13,14 Some studies focused on the attitudes of physicians or medical students toward the TCM.15,16 In particular, there is no data on the opinions of patients with different medical conditions regarding the efficacy of TCM.17
Although TCM plays an important role in China’s medical system, there is a lack of comprehensive understanding of patients’ preferences regarding TCM, especially when it comes to patients with different medical conditions. This study thus aimed to fill this void in the literature.
We therefore mainly focused on the utilization and opinions of TCM in patients, especially regarding the medical conditions of the patients who were willing to use TCM, and assessed via interviews with patients at five different types of hospitals. Additionally, we aimed to reveal the patients’ beliefs in the multi-effectiveness of TCM and the social demographic factors that influence their opinions.
Materials and Methods
The Design and Setting of the Study
The Chinese Healthcare Improvement Action Plan has been implemented since 2015 by the National Health Commission. For evaluating the effects of this policy, Peking Union Medical College designed the China Healthcare Improvement Evaluation Survey (CHIES).18 The CHIES is intended to survey attitudes on the health and medical system and satisfaction regarding healthcare among patients and hospitals staff. The most recent CHIES was a national cross-sectional survey conducted in January 2021. This survey was conducted at public tertiary hospitals across 31 provinces in China, including provincial general hospitals, provincial TCM hospitals, and provincial Obstetrics and Gynecology hospitals (OB/GYN hospitals) as well as hospitals managed by the National Health Commission (including general hospitals and specialized hospitals such as stomatology hospitals and eye hospitals, etc.). All hospitals are in capital cities of every province. Every province employed a group of volunteers to help conduct this survey, led by professions at the medical universities or other survey institutions.
Sample Size and the Characteristics of Participants
This study used data from the CHIES outpatient questionnaire from 163 hospitals. According to a pre-survey, the mean composite measure score of the overall outpatient experience rating was 4.5. For reliable estimates of patient experience scores, we determined the required sample size based on the upper limit of the daily outpatient visits (10,000 patients per day) at the sample hospitals, with a 1.5% estimate range, a 5% significance level, and a standard deviation of 0.5. We thus set the targeted sample size at a minimum of 200 outpatients, which yielded a total sample of 31,599 patients. The overall response rate was about 90.0%.
Inclusion criteria: Outpatients who have completed all treatment procedures would be invited to participate the survey.
Exclusion criteria was applied at 2 stages (ie, the investigation stage and data cleaning stages).
At the investigation stage:1. Patient in the emergency department. 2. Patient in the psychiatric department or individuals with mental illness.
At the data cleaning stage:1. Excluded participants under the age of 18, because their guardian would have to help them complete the questionnaire and responses can therefore not be assumed to reflect the participant’s own attitude and feeling. 2. Excluded 51 participants who did not provide crucial demographic information, such as sex and age, which might affect the accuracy of our analysis.
Finally, 28,993 samples were entered into the analysis conducted in this study (Figure 1).
 |
Figure 1 Participant identification flowchart. #Obstetrics and Gynecology hospitals. |
Measurements and Data Collection
Using a convenient sampling method, survey conductors, including medical students and hospital interns who received uniform training in survey, administered a survey questionnaire on patients who completed their clinical visits at the outpatient department of a hospital. We used electronic questionnaire system and the system automatically checked for illogical or incongruous responses and determined the completeness of each record. Since this study focused on preferences for TCM in daily medical care, we asked the patients the following multiple-choice question:
Under which of the following medical conditions would your family members and you choose to use traditional Chinese medicine (including Chinese medicine treatment, health cultivation methods, acupuncture, moxibustion, massage (tuina), as well as other TCM methods and therapies)? You can choose more than one option.
The nine options were as follows: (1) prevention, (2) treatment of common symptoms such as cold and fever, (3) chronic diseases such as hypertension and diabetes, (4) complicated diseases (such as rare diseases or some other symptoms of unknown cause), (5) cancer, (6) rehabilitation, (7) skin problems, (8) sleeping disorder, and (9) other conditions such as pain relief and mental disorders.
In addition, we collected data on associated factors including hospital types visited for treatment and sociodemographic information. The latter was classified into age, sex, education level, employment, registered permanent residence, number of family members, family income, and health insurance.
Data Analysis
All data were downloaded into a database and analyzed with Stata 16. Descriptive statistics were used to describe patients’ sociodemographic characteristics and the medical conditions they would use TCM for. Categorical variables were expressed as percentages (%). The relationships between chosen medical conditions and variables were analyzed via multi-response χ2 tests.
Responses to a multiple choice question assessed patients’ beliefs in the effects of TCM, in particular, whether they thought TCM had a single function or multiple effects based on the number of medical conditions patients would use TCM for. Some sampled patients chose only one particular medical condition, while others chose more than one condition. Therefore, those who chose two or more medical conditions might be thought of believing that TCM has multiple effects.
Associations between the choices number of medical conditions and potential influencing factors, such as hospital types and sociodemographic characteristics, were estimated using binary logistic regression model. The effect of each variable was expressed as an odds ratio (OR) with a 95% confidence interval (95% CI). All tests for statistical significance were two-way, and the significance level was set as α=0.05.
Ethics
The Scientific Research and Ethics Committee of Peking Union Medical College approved the protocol (the ethical approval number: IPB-2020-23). All methods were carried out in accordance with relevant guidelines and regulations.
At the beginning of the survey, we introduced the procedure, and participants were informed that they had the right to end their participation at any time. All participants in our study provided informed consent to participate.
Results
Characteristics of the Participants
Table 1 presents the characteristics of all patients who took part in the study. The percentage of general hospital patients was the largest, at 42.4%. Moreover, 44.3% were young people (age of 18 to 34); 68.1% were female; 54.9% patients’ education level were undergraduate; 50.9% were employed at a company or at governmental or public institutions; 71.1% were living in urban areas; 56.3% were living in a family with 3–4 members; 42.7% of patients reported a family income below 60 thousand RMB (about 8900 USD) per year; 55.6% were subscribed to the Urban Employee Basic Medical Insurance (UEBMI) and 35.8% to the Urban and Rural Resident Basic Medical Insurance (URRBMI).
 |
Table 1 Characteristics of Participants |
The Utilization of TCM in Different Medical Conditions
Figure 2 shows the proportion of patients indicating they would use TCM for a certain medical condition, at different hospital types. A total of 22,122 patients (76.3%) voiced they would use TCM for disease prevention. The percentages of medical conditions that respondents would use TCM to treat, from the largest to the smallest, were chronic diseases (34.0%), common symptoms (33.0%), rehabilitation (26.9%), sleeping disorder (26.3%), complicated diseases (13.0%), skin problems (12.0%), other conditions (11.1%), and cancer (7.8%), respectively.
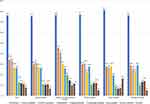 |
Figure 2 Traditional Chinese Medicine use in different medical conditions by hospital types. #Obstetrics and Gynecology hospitals. |
In addition, we also found that patients at different hospital types had different views on the effects of TCM (P<0.001). As can be seen in the higher proportions of patients choosing TCM for all medical conditions, compared to other types of hospitals, the attitude of patients at TCM hospitals was overall more positive. We compared the orders of options percentage in different types of hospitals. At cancer hospitals, the rankings of outpatients who would use TCM for rehabilitation (27.7%, order 2nd) and cancer treatment (16.3%, order 6th) were higher than those at other types of hospitals. Similarly, patients at OB/GYN hospitals (27.9%, order 4th) and specialized hospitals (29.1%, order 2nd) showed a preference to use TCM for sleeping disorder.
Views on Multiple Effects of TCM
Table 2 shows the number of options that patients chose according to different demographic factors. We found that 67.3% of patients chose two or more options, indicating that they thought TCM had multiple effects. This proportion ranged from 61.9% to 75.0% in groups of respondents with different characteristics. Particularly, patients at TCM hospitals believed in the multiple effects of TCM to an even higher degree (75.0%). In contrast, the number of patients at cancer hospitals who thought that TCM has a variety of effects was the lowest (61.9%).
 |
Table 2 Logistic Regression Result: Factors Associated with Multiple Effect of Traditional Chinese Medicine |
Factors Associated with the Views on the Multiple Effects of TCM
Table 2 also presents the results of binary logistic regression and the factors that were identified to be associated with beliefs regarding the multiple effects of TCM among patients. In this regression model, we set the dependent variable to 0 if the patients only chose one medical condition, and to 1 if the chosen options were two or more.
In terms of hospital types, compared with those at general hospitals, patients at TCM hospitals chose more medical conditions they would use TCM (OR: 1.630, 95% CI: 1.529–1.738, P<0.05). Generally, female and older patients, as well as patients with a higher education level, urban residency, and higher family income, were found to be associated with a higher probability of using TCM for multiple conditions than their counterparts (OR>1, P<0.05). In addition, compared with those who subscribed to the urban employee basic medical insurance, patients without health insurance did not think that TCM has multiple effects (OR: 0.793, 95% CI: 0.715–0.879, P<0.05).
Discussion
The Greatest Effect of TCM is Prevention
In this study, independently of the characteristics of different patient subgroups, the proportion of patient who chose “prevention” as their reason to use TCM was the highest. Prevention is the most economical and effective health strategy, and it is a core belief of users of TCM that it is effective for this purpose.6 As early as in the ancient book named “The Huang Di Nei Jing (Yellow Emperor’s Inner Canon)”,19 the oldest extant classic book of TCM, preventative treatment is emphasized Chinese medicine underscores “preventing a disease before it arises”,20 which means that doctors should prevent the occurrence of diseases. The theory of disease prevention refers to the use of multiple methods to improve one’s immunity and achieve a harmonious unity of body, environment, and nature. These methods include disease prevention methods, such as optimizing one’s diet, exercise, and living a healthy lifestyle, as well as the use of herbal medicines21 and physical therapies (such as acupuncture and massage). Therefore, Chinese people have the awareness and tradition of using TCM to prevent diseases before they need to be treated. Some previous studies have reported the same results. A meta-study analyzing papers from 1990 to 1997 showed that CAM/TCM was used for illness prevention and health promotion in some developed countries.22
TCM is Also Believed to Be Suitable for Dealing with Different Medical Conditions
Complicated diseases are those which exact pathogenesis or effective treatment is difficult to determine, such as cancer and some rare disease. Although using TCM for the treatment of complicated diseases represented the least popular choice in this study, Chinese medical experts have long held the idea that treating complicated diseases requires the integration of traditional Chinese and western medicine. A survey in China showed that more than 83% of cancer patients had used TCM since diagnosis,23 and 53% of patients in other studies also received TCM treatment during the course of cancer treatment as well as during rehabilitation.24 During the period of recovery from cancer, TCM focuses on symptoms or the prevention and treatment of recurrence and metastases,25,26 combined with various traditional treatment methods to help patients alleviate symptoms and improve their quality of life.27–29 This was also reflected by the percentage of patients at cancer hospitals in our study who chose TCM as an effective treatment method for rehabilitation.30,31 The results of other studies showed the use of TCM in all stages of prevention, diagnosis, treatment, and rehabilitation of complex diseases. In this study, using TCM in disease prevention, diagnosis, treatment, and rehabilitation were investigated separately, so the results were relatively lower than in other studies.
Patients with Higher Socioeconomic Status Would Like to Use TCM for More Medical Conditions
With a more positive attitude toward TCM, patients in TCM hospitals chose more medical conditions where they considered TCM the appropriate treatment method than those in other hospitals. This study also reveals that sex, age, education level, registered permanent residence, income, and medical insurance were factors associated with patients’ views on the multiple effects of TCM.
In China, TCM has always been considered simple, convenient, cheap, and effective.32–34 It is thus thought to be part of primary health care33 and used more among vulnerable groups,35 such as residents in rural areas and low-income groups. In contrast to this, this study and other current studies found that people with high socioeconomic status were more likely to use TCM. Studies have persistently shown that CAM/TCM users are more likely to be female,36–41 better educated,39,42,43 as well as to have higher income44,45 and occupational status.46 We found that patients with health insurance and those who lived in urban areas were more likely to think TCM is multi-effective, and other studies17,47 came to the same conclusion.
In the 1990s, researchers identified socioeconomic status as one of the most important determining factors in studies on different medical conditions and life expectancy.48 The WHO also found that countries at all levels of income, health, and illness follow a social gradient that: the lower the socioeconomic status, the worse the health.49 Therefore, we can assume that people with high socioeconomic status pay more attention to maintaining their health overall and therefore consider TCM a good way to prevent diseases, relieve pain, and improve their life quality.
Additionally, older people find TCM to be more useful than younger people.17,39,42–45 One reason for this finding might be that they have a higher recognition of traditional Chinese culture because they primarily used TCM when there was a shortage of doctors and medicine in China and TCM played an even more important role in primary health care in the 1950s. On the other hand, the medical conditions of older patients were worse, which seems to be one of the factors affecting their views on the use of TCM in our study.50
Limitations
Although we shed light on some significant factors of the preference and opinions of patients towards TCM in a large sample, it is important to keep in mind that our results only represent the patients’ attitudes, and great caution should be exercised when extrapolating these findings to the whole population. Whether people think TCM is more useful or not depends on the health problems they may face. If patients are experiencing a number of health problems, they may think TCM has multiple effects and can help all their symptoms. However, this study lacks personal medical information, such as diagnoses and treatment. We can therefore not draw conclusions about the association between utilization and opinions on the one hand, as well as real medical conditions and their treatment on the other. Further studies are needed to investigate how views on TCM relate to such medical information.
Conclusion
Patients in our large sample from different types of hospitals overall believed that TCM has multiple effects, especially for disease prevention and health maintenance, but patients in different types of the hospital expressed different views on these effects. Generally, patients with higher socioeconomic status had a positive attitude toward TCM.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The Scientific Research and Ethics Committee of Peking Union Medical College approved the protocol (the ethical approval number: IPB-2020-23) and adhered to the tenets of the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations. At the beginning of the survey, we introduced the procedure, and participants were informed that they had the right to end their participation at any time. All participants in our study provided informed consent to participate.
Acknowledgments
We thank all the volunteer groups in 31 provinces for helping us implement surveys and 163 hospitals’ managers for providing some necessary support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (2021-I2M-1-046). A Strategic Study on Healthy China Development and Health System Reform.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. WHO International Standard Terminologies on Traditional Chinese Medicine. Geneva: World Health Organization; 2022.
2. World Health Organization. Traditional, complementary and integrative medicine. WHO; 2021. Available from: https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine#tab=tab.
3. Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. Int J Clin Pract. 2012;66(10):924–939. doi:10.1111/j.1742-1241.2012.02945.x
4. Shin HK, Jeong SJ, Huang DS, Kang BK, Lee MS. Usage patterns and adverse experiences in traditional Korean medicine: results of a survey in South Korea. BMC Complement Altern Med. 2013;13:340. doi:10.1186/1472-6882-13-340
5. Sydara K, Gneunphonsavath S, Wahlstrom R, et al. Use of traditional medicine in Lao PDR. Complement Ther Med. 2005;13(3):199–205. doi:10.1186/1472-6882-8-48
6. China’s State Council Information Office. Traditional Chinese medicine in China. Xinhua; 2016. Available from: http://en.nhc.gov.cn/2016-12/06/c_74787.htm.
7. Wade C, Chao MT, Kronenberg F. Medical pluralism of Chinese women living in the United States. J Immigr Minor Health. 2007;9(4):255–267. doi:10.1007/s10903-007-9038-x
8. Chung VC, Ma PH, Lau CH, Wong SY, Yeoh EK, Griffiths SM. Views on traditional Chinese medicine amongst Chinese population: a systematic review of qualitative and quantitative studies. Health Expect. 2014;17(5):622–636. doi:10.1111/j.1369-7625.2012.00794.x
9. National Health Commission of PRC. Health Statistical Yearbook 2021. Beijing: Peking Union Medical College Press; 2022.
10. Jazieh AR, Abuelgasim KA, Ardah HI, Alkaiyat M, Da’ar OB. The trends of complementary alternative medicine use among cancer patients. BMC Complement Med Ther. 2021;21(1):167. doi:10.1186/s12906-021-03338-7
11. Hok J, Tishelman C, Ploner A, Forss A, Falkenberg T. Mapping patterns of complementary and alternative medicine use in cancer: an explorative cross-sectional study of individuals with reported positive “exceptional” experiences. BMC Complement Altern Med. 2008;8:48. doi:10.1186/1472-6882-8-48
12. Naja F, Fadel RA, Alameddine M, et al. Complementary and alternative medicine use and its association with quality of life among Lebanese breast cancer patients: a cross-sectional study. BMC Complement Altern Med. 2015;15:444. doi:10.1186/s12906-015-0969-9
13. Karsch-Völk M, Barrett B, Linde K. Echinacea for preventing and treating the common cold. JAMA. 2015;313(6):618–619. doi:10.1001/jama.2014.17145
14. Hinman RS, McCrory P, Pirotta M, et al. Acupuncture for chronic knee pain: a randomized clinical trial. JAMA. 2014;312(13):1313–1322. doi:10.1001/jama.2014.12660
15. James PB, Bah AJ, Kondorvoh IM. Exploring self-use, attitude and interest to study complementary and alternative medicine (CAM) among final year undergraduate medical, pharmacy and nursing students in Sierra Leone: a comparative study. BMC Complement Altern Med. 2016;16:121. doi:10.1186/s12906-016-1102-4
16. Joyce P, Wardle J, Zaslawski C. Medical student attitudes towards complementary and alternative medicine (CAM) in medical education: a critical review. J Complement Integr Med. 2016;13(4):333–345. doi:10.1515/jcim-2014-0053
17. Lyu Y, Hu M, Xu A. Investigation on the influential factors of TCM service utilized by outpatients in Jiangsu Province. China Pharm. 2021;32(21):2668–2672. doi:10.6039/j.issn.1001-0408.2021.21.18
18. Hu G, Chen Y, Liu Q, et al. Patient experience of hospital care in China: major findings from the Chinese patient experience questionnaire survey (2016–2018). BMJ Open. 2019;9(9):e031615. doi:10.1136/bmjopen-2019-031615
19. Zhu M. The Medical Classic of the Yellow Emperor. New Phoenix International Llc; 2001.
20. Gong J, Song W. Newly Edited: Treating Pre-Disease. Beijing: People’s Medical Publishing House; 2005.
21. Lorenzi EA. Complementary/alternative therapies. So many choices. Geriatr Nurs. 1999;20(3):125–133. doi:10.1016/s0197-4572(99)70003-0
22. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997 Results of a follow-up national survey. JAMA. 1998;280(18):1569–1575. doi:10.1001/jama.280.18.1569
23. McQuade JL, Meng Z, Chen Z, et al. Utilization of and attitudes towards traditional Chinese medicine therapies in a Chinese cancer hospital: a survey of patients and physicians. Evid Based Complement Alternat Med. 2012;2012(15). doi:10.1155/2012/504507
24. Zhang L, Yan J, Liu X, et al. Pharmacovigilance practice and risk control of traditional Chinese medicine drugs in China: current status and future perspective. J Ethnopharmacol. 2012;140(3):519–525. doi:10.1016/j.jep.2012.01.058
25. Sun L. Integrating Traditional Chinese Medicine into cancer survivorship care model based on Chinese cancer survivors? Needs and international practice [Doctor]. China Academy of Chinese Medical Sciences; 2017.
26. Yan J, Wei Y, Teng Y, et al. Physician preferences and shared-decision making for the traditional Chinese medicine treatment of lung cancer: a discrete-choice experiment study in China. Patient Prefer Adherence. 2022;16:1487–1497. doi:10.2147/ppa.S365109
27. Zeng L, Li Y, Fan L. Analysis of clinical effect of traditional Chinese medicine comprehensive rehabilitation on patients with cancer and their life quality during rehabilitation period. J Bethune Med Sci. 2016;14(02):156–158. doi:10.16485/j.issn.2095-7858.2016.02.010
28. Dong Q, Liu Y, Wu H. Clinical research of combined rehabilitation therapy with traditional Chinese medicine. Chin J Clin Oncol Rehabil. 2013;20(01):76–79. doi:10.13455/j.cnki.cjcor.2014.02.001
29. Olsson Möller U, Beck I, Rydén L, Malmström M. A comprehensive approach to rehabilitation interventions following breast cancer treatment - a systematic review of systematic reviews. BMC Cancer. 2019;19(1):472. doi:10.1186/s12885-019-5648-7
30. Dufter SA, Hübner J, Ahmadi E, Zomorodbakhsch B. Traits of cancer patients and CAM usage. J Cancer Res Clin Oncol. 2021;147(12):3685–3692. doi:10.1007/s00432-021-03605-7
31. Wang JW, Yang ZQ, Liu C, et al. Cancer survivors’ perspectives and experience on western medicine and traditional Chinese medicine treatment and rehabilitation: a qualitative study. Patient Prefer Adherence. 2015;9:9–16. doi:10.2147/ppa.S76617
32. The State Council of PRC. Guideline on developing traditional Chinese medicine (TCM) during the period of 2016-30; 2016. Available from: http://www.gov.cn/zhengce/content/2016-02/26/content_5046678.htm.
33. Chen M. Study On Development Strategy for Traditional Chinese Medicine of Basic Medical Institution in the Background of Medical Reform [Doctor]. Huazhong University of Science & Technology; 2011.
34. Guan H, Dai G, Wang N, Gao W, Ren L, Cai Z. Effect and safety of oral Chinese patent medicine for heart failure: a protocol for systematic review and network meta-analysis. Medicine. 2020;99(42):e22754. doi:10.1097/md.0000000000022754
35. Yan F, Uhlemann T, Weng Z, et al. Qualitative study on health problems of vulnerable people and how they cope with their problems. Chin Health Resour. 2001;05:208–210.
36. Featherstone C, Godden D, Selvaraj S, Emslie M, Took-Zozaya M. Characteristics associated with reported CAM use in patients attending six GP practices in the Tayside and Grampian regions of Scotland: a survey. Complement Ther Med. 2003;11(3):168–176. doi:10.1016/S0965-2299(03)
37. Featherstone C, Godden D, Gault C, Emslie M, Took-Zozaya M. Prevalence study of concurrent use of complementary and alternative medicine in patients attending primary care services in Scotland. Am J Public Health. 2003;93(7):1080–1082. doi:10.2105/ajph.93.7.1080
38. Kristoffersen AE, Quandt SA, Stub T. Use of complementary and alternative medicine in Norway: a cross-sectional survey with a modified Norwegian version of the international questionnaire to measure use of complementary and alternative medicine (I-CAM-QN). BMC Complement Med Ther. 2021;21(1):93. doi:10.1186/s12906-021-03258-6
39. Kebede EB, Tan J, Iftikhar S, et al. Complementary and alternative medicine use by patients from the gulf region seen in the international practice of a tertiary care medical center. Glob Adv Health Med. 2021;10:21649561211010129. doi:10.1177/21649561211010129
40. Molassiotis A, Fernadez-Ortega P, Pud D, Ozden G, Patiraki E. Use of complementary and alternative medicine in cancer patients: a European survey. Eur J Oncol Nurs. 2005;9(4):655–663 doi:10.1093/annonc/mdi110.
41. Ryan A, Wilson S, Taylor A, Greenfield S. Factors associated with self-care activities among adults in the United Kingdom: a systematic review. Bmc Public Health. 2009;9(1):96. doi:10.1186/1471-2458-9-96
42. Ong CK, Doll H, Bodeker G, Stewart-Brown S. Use of osteopathic or chiropractic services among people with back pain: a UK population survey. Health Soc Care Community. 2004;12(3):265–273. doi:10.1111/j.1365-2524.2004.00497.x
43. Ong CK, Petersen S, Bodeker GC, Stewart-Brown S. Health status of people using complementary and alternative medical practitioner services in 4 English counties. Am J Public Health. 2002;92(10):1653–1656. doi:10.2105/ajph.92.10.1653
44. Ernst E. The BBC survey of complementary medicine use in the UK. Complement Ther Med. 2000;8:32–36 doi:10.1016/S0965-2299(00)90833-1.
45. Thomas K, Coleman P. Use of complementary or alternative medicine in a general population in Great Britain. Results from the national omnibus survey. J Public Health. 2004;26(2):152–157. doi:10.1093/pubmed/fdh139
46. Furnham A, Beard R. Health, just world beliefs and coping style preferences in patients of complementary and orthodox medicine. Soc Sci Med. 1995;40(10):1425–1432. doi:10.1016/0277-9536(94)00263-s
47. Wang Z. Study on the influencing factors and cost-effectiveness of TCM in the treatment of cardiovascular diseases in middle-aged and elderly people in China based on CHARLS database [Master]. Beijing University of Chinese Medicine; 2021.
48. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35:80–94. doi:10.2307/2626958
49. World Health Organization. Social determinants of health; 2022. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1.
50. Wu J, Wang J, Liu X. Analysis of the willingness of first-visit of traditional Chinese medicine in rural elderly and its influencing factors. Chin Health Serv Manag. 2022;39(3):196–199, 226.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
