Back to Journals » Psychology Research and Behavior Management » Volume 16
Measuring Performance of Rural Mental Healthcare Services in Saudi Arabia
Authors Alblowi EA, Shujaa MA, Alonazi WB
Received 24 May 2023
Accepted for publication 12 September 2023
Published 20 September 2023 Volume 2023:16 Pages 3895—3905
DOI https://doi.org/10.2147/PRBM.S420662
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Eman A Alblowi, Mona A Shujaa, Wadi B Alonazi
Health Administration Department, College of Business Administration, King Saud University, Riyadh, 11587, Saudi Arabia
Correspondence: Wadi B Alonazi, Email [email protected]
Introduction: Recently, the Saudi government has proposed several initiatives to promote mental health, including the national program named Wazen. The objective of this study was to observe the performance of mental hospitals using a balanced scorecard through this federal program.
Methods: Secondary quantitative analysis was implemented utilizing the Wazen report program data in 2022. The report adopted a balanced scorecard (BSC) concept. The study focused on 19 mental health facilities (Eraddah Hospitals) in the Ministry of Health (MOH) regions. The MOH’s annual statistical report for 2018 and 2022 was reviewed to explore more about beds, staff, and the number of new mental disorder cases. Data were analyzed using Microsoft Excel 365 and the Statistical Package for Social Sciences (SPSS Version 25) software. Mental health hospitals were classified into three categories.
Results: Most rural hospitals had lower performance in the yellow threshold value that might need improvement. The data shows that the mean of all hospital performance in some domains ranged, yielding 70% staff engagement and 77% continued educational activity, indicating unsatisfactory performance across public mental health services. The means score of access to care was 97.0% and 94.7%, marking the better mental health services provided. Between 2018 and 2022, there was a significant rise in the prevalence of mental disorders, as evidenced by the number of new patients and outpatients indicated by specific mental diseases, including conditions of psychological development (F80-F98).
Discussion: The high quality of mental healthcare is manifested by therapeutic ethos with a high degree of interaction between professional careers and service users. The former is enhanced by highly educated, competent, compassionate, self-aware, and specialized healthcare professionals in mental health. When assessing mental healthcare services, we recommend considering providers’ and professionals’ conditions for successful implementation in alignment with patient experience.
Keywords: rural mental health services, Eraddah Hospitals, Ministry of Health, mental health system, people and development, patient experience
Introduction
Like the rest of the world, Saudi Arabia has some basic public health issues with mental illness. Mental illness is spreading across the globe as 450 million people worldwide suffer from mental health conditions, making it one of the top five disorders leading to disability in terms of global disability-adjusted life years (DALYs), according to the WHO report.1 The mental illness severely impairs personal, social, and occupational functioning.2 They result in significant societal costs related to productivity and healthcare utilization. Even though healthcare costs have grown at an average annual rate of 4.3% from 2000 to 2017, several mental disorder patients remain undertreated. In addition, many who seek mental health services discontinue treatment before completing the recommended course of care.3 In 2010, Saudi Arabia (SA) joined the World Mental Health (WMH) Survey Initiative, which is run in collaboration with Harvard University and has been conducted in over 33 countries. This initiative was launched to close the gap between the supply and demand for mental health services.2 Data from SA have concentrated on groups of people (such as students, patients at primary care facilities, or hospital patients), regional community samples, and particular disorders (eg, depression). There was a critical need in SA for a national community study of mental health to clarify the current state of mental health in the population and inform national mental health policy, treatment, and research. This was due to the well-documented effects and costs of various mental disorders on individuals and society.2
According to the WMH surveys, only 27.9% of participants diagnosed with a mental health disorder reported receiving adequate mental health treatment. Of those who did so, only 12.8% did not follow treatment recommendations. The most frequently cited reason for failure to initiate and continue treatment is lack of perceived need, followed by attitudinal barriers (such as stigma or wanting to handle the issue independently) and, less frequently, structural barriers (eg, financial problems, access).3 The two most prevalent mental illnesses, anxiety and depression, are difficult to be diagnosed in primary care due to complex barriers. These barriers are usually categorized as factors related to the patient, clinician, health system, or organizational factors. Some patients may believe their symptoms are not medically related and that a physician cannot cure them mentally.4
Development of Mental Health Services in Saudi Arabia
MOH is the leading provider of mental health services, with other government agencies providing psychiatric treatment for state employees. In the early 1980s, there were only two psychiatric hospitals in SA, and psychiatric training was only possible up to the diploma level. In 1983, the MOH began to decentralize psychiatric services. By 2010, over 700 psychiatrists and 1126 psychologists, social workers, and occupational therapists worked in the mental health sector. Senior staff members are increasing among Saudi nationals, yet most nursing staff are non-Saudis.5 The Saudi National Mental Health Survey (SNMHS) was started with a national initiative to improve overall mental health in SA.6 Then, by 2014, the MOH established 21 regional psychiatric hospitals, augmented by free-standing private psychiatric clinics and clinics based in many areas, including 125 private general hospitals. Thus, offering insights into behavioral patterns is crucial for psychology research professionals and behavioral management to understand and address.
As part of the SA Vision 2030, the MOH has begun developing a new patient-centered Model of Care (MoC) healthcare system to help people socially, mentally, and physically. Indeed, MoC design ensures that patients receive care tailored to their specific needs. Keep Me Well, Chronic Care, Urgent Care, Planned Care, Safe Birth, and Last Phase are the six patient-centered care systems that comprise the MoC. The system of chronic care includes mental healthcare.6 To achieve the 2030 vision, MOH released several initiatives to promote mental health, like the National Center for Mental Health Promotion, established in 2019 by the Honorable Council of Ministers Decision No. 685, dated July 30, 2019. Its mission is to develop national programs that enhance community life, promote positive participation, and support those most at-risk or with mental illnesses. One of the services provided by the center to improve mental health was the Call Center (937), one of the few government centers to offer free psychological counseling. The services included 116,323 psychological consultations. Patients and their families are assisted in dealing with the burden of mental disorders through the center’s efforts to raise awareness and provide psychological education. In addition to developing a text-based counseling service for psychologists, they also created the “Qareboon” application, which includes a mental health library that employs the most updated techniques and tools, including text materials, infographics, and visual content. In addition to providing education and awareness about mental illness, it aims to create a cohesive society with a robust mental health culture.7 The MOH also adopted more than one application to provide mental health services, like Labayh and Famcare. Both Applications offer psychological counselors for users to consult with while maintaining their privacy virtually. Indeed, these applications emotionally supported many individuals, especially during the COVID-19 curfew. Moreover, the MOH integrated platform, known as “Sehhaty”, offers a variety of health services to everyone, such as the 937 (free line) service, which provides voice calls for medical consultations.8 As one of the most recent initiatives to improve mental health in SA, the MOH implemented a severe initiative to assess, improve, and develop mental healthcare services through promoting the Wazen program.
Wazen Program
The Wazen program is one of the Ministry Agency for Therapeutic Service projects, represented by the assistant agency for hospital service at the general administration of hospital affairs. The program aims to measure the extent to which the mental-related strategic objectives of the MOH hospitals are achieved and provide a roadmap for decision-making at the executive and operational levels. The program is based on reports of hospital performance indicators through the BSC.9 Established in 2013, this program is considered one of the significant outcomes-based projects. The program aimed to specialize in developing highly efficient and easy-to-use database-enabled applications in Saudi Arabia and throughout the Arab region. Wazen has developed several industrial and commercial applications in addition to development tools. Toward achieving the Saudi Vision 2030, the Wazen program prepares reports on the performance of 100 hospitals. Reviewing and improving performance can be done using those reports. In addition, they can also be highly beneficial to decision-makers. Also, Wazen strives to facilitate hospitals’ achieving their objectives and strategic plans in line with their predetermined Kep Performance Indicators (KPIs). The Wazen program also aims to spread a culture of performance evaluation, promotion, and measurement in hospitals so that they can use their full potential in this area. The program is intended to cover all hospitals in the Kingdom. The Wazen program includes many essential criteria, like patient experience, health performance program, clinical privileges, quality and patient safety, medical records, and the development of financial resources. Wazen used the balanced scorecard as a quality tool to assess and monitor facility performance in healthcare organizations.10 The program depends on three domains to measure the mental health facility: human, process, and patient experience. The behaviors and attitudes surrounding mental health can influence societal dynamics, workplace environments, and overall community well-being. Understanding these impacts is crucial for professionals in psychology research and behavioral management seeking to create positive societal changes.
People and Development
The continued training of the mental healthcare workforce is crucial, as evidenced by statistics and academic institutions’ annual professionals. Graduation rates among medical students in SA are limited due to rigorous admission examinations. However, the graduation rate is still insufficient to meet the market needs (0.2% psychologists, 10% social workers, 3.8% other Doctor of Medicine, 1.8% nurses, and 0.4% psychiatrists). Again, continuing education in mental health is very limited to university courses, representing almost half of the psychiatrists’ official certificates. Indeed, a pedagogical reform for mental healthcare services, especially in Vision 2030, is well-established to improve mental services.4 Overall, cognitive learning outcomes had relatively low performance, ensuring a need to enhance mental services regarding professionals, curriculum, and settings.11 Still, medical practitioners did not know mental terminologies and proper diagnosis.4 As a significant recommendation in previous studies, physicians may also need extensive job training programs, ongoing medical education, and attending psychiatric courses.12 By highlighting the interplay between mental health services, behavioral barriers, and broader public health implications, the manuscript invites a multidisciplinary approach where professionals from various fields can cooperate to develop practical solutions for improving rural mental health outcomes.
Process of Mental Services in Rural Areas
Commonly, four concerns face any individuals in rural areas to attend mental services: accessibility, affordability, availability, and accessibility.13,14 Inequality and difficulty accessing mental health services, especially in rural areas, are two of the most cited challenges across SA. This may be attributed to financial and clinical affordability. Among 650 adults, two-thirds were likely to lack knowledge about the essence of mental illness. Some socio-demographic characteristics like gender and age do not necessarily impact such domains.15 Indeed, this ineffective service hurts patient safety and healthcare quality.16 Preventive measures allow for early intervention and increase better long-term outcomes for individuals diagnosed with mental disorders.17 Thus, the manuscript presents opportunities for behavioral management experts to devise strategies encouraging individuals to overcome barriers and engage in appropriate mental health services.
Patient Experience
The MOH offers a service free line service called 937. This is an automated system where all calls are received from patients about their health concerns. Full-time consultants offer 24/7 mental services anytime and anywhere.18 The Saudi healthcare system has utilized recent advanced technology to meet the patient’s expectations, including mobile applications and external evaluation, especially external assessment from a third specialized agency. In 2021, a study was conducted on users of the Self-Help Anxiety Management apps, and the results concluded a trust and usefulness in such applications. The most desired features included social support, motivational content, and relaxation.19 In 2017, a strong relationship was found between the young-generation group and utilizing mental health applications. Approximately half of the participants were willing to use the mobile application to control or monitor their health-related activities.20
The mental health services activities were not academically and practically fulfilled in concurrent literature, perhaps a deeper unraveling of what has been uncovered on the mental healthcare services movement, particularly in SA. Indeed, this research outcome motivates attitude to strengthen the power of psychology research and behavior management. The uniqueness of this research is based on its approach and design with respect to the study’s objectives, exploring the forgotten elements, and the scope of the research.
MOH called Mental Hospital Eraddah Mental Hospital to emphasize psychological power, connotating an individual self-power. A need to monitor mental health services from a macro level is essential to determine how Saudi mental health services may assist individuals in coping with their needs. The Wazen program proposed a continuous, systematic improvement of Saudi Arabia’s mental health system and measured changes in mental hospital services based on the Kingdom 2030 vision. This paper demonstrates a proactive approach to assessing the performance of mental hospitals, aligning with the Saudi government’s initiatives to promote mental health among the population.
Materials and Methods
Secondary quantitative data analysis was explored from the Wazen program report, in which such a project applied the BSC. The BSC performance measurement framework has two key objectives. The first objective was to convert BSC to gain popularity as an effective management tool that aligns employee actions and goals with corporate strategy. Second, it is essential to communicate the mental health strategy among all organization sections effectively.21 Based on data derived from the Wazen program and the MOH’s annual statistical reports, this approach allows for a comprehensive assessment of mental health facilities using reliable and authoritative data sources. The report adopted a balanced scorecard (BSC) concept. The BSC is usually applied in business settings, yet its application to the healthcare sector, particularly mental health, is limited. This national study employs innovative thinking in adapting a well-established managerial tool in a new context.
Setting: The study focused on 19 mental health facilities (Eraddah Hospitals) among the MOH’s 20 health regions.
As shown in Table 1, there are three categories of bed capacity used by the Wazan program for facilities included in this program for the classification of Erddah Mental Health hospitals: Mental Health Hospitals with more than 350 Beds, Mental Health Hospitals with 200 to 350 Beds, and Mental Health Hospitals with less than 200 Beds. This multidimensional approach provides a mutual understanding of strengths and areas demanding improvement within the mental health system.
 |
Table 1 Classification of Bed Categories at Eraddah Mental Hospitals* |
The Wazen program can measure hospital performance arranged under three domains, as shown in Figure 1.
 |
Figure 1 The three hospital performance domains associated with the Wazen program. |
However, Wazen threshold categories emphasized specific measures for each mental health service. The key performance indicators are depicted in Figure 2.
 |
Figure 2 The scores associated with each level of performance based on national mental health services measures. |
Other data were obtained from the MOH annual statistical book between 2018 and 2022. The book details all the MOH’s activities for the year. The study focused on the MOH mental hospital and the number of beds among 20 health regions. Also, the total number of psychiatric residents, registrars, and consultants in the country. Finally, the number of all new outpatients and inpatients with mental disorders is organized according to the International Classification of Diseases, 10th Revision (ICD-10) disease groups, as shown in Supplementary 1.
Data Analysis
Statistical Software (SPSS Version 25) and Microsoft Excel 365 were used to assess the average levels of change in MOH mental hospital bed capacity, staffing, and number between 2018–2022. Descriptive statistics were calculated for each domain’s mean and standard deviation scores. The percentage of hospitals with higher and lower Wazen scores in each domain and the ratio of hospitals in similar Wazen score categories. Furthermore, the maximum and minimum rates of staff from all health regions were traced.
For the other data, using Microsoft Excel 365, we calculated the percentage of changes in bed capacity, staffing, and the number of MOH mental hospitals between 2018 and 2022. The maximum and minimum rates of staff from all health regions and the percentage change in new mental disorders in Saudi Arabia were recorded.
Results
The overall results of the Wazen program show that 58% of hospitals were within the green threshold value, 32% were within the yellow threshold value, and 11% were within the blue threshold value. Furthermore, the number of mental hospitals remained constant.
Table 2 shows the difference in performance between high and low-performance mental hospitals serviced at Eradah mental hospitals. Most rural areas had lower performance in the yellow threshold value that might need improvement. The data shows that the mean of all hospitals has 70% staff engagement and 77% continued educational activity, indicating the worst performance across MOH’s mental health services.
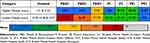 |
Table 2 The Distribution of Scores Based on the Three Domains of Mental Health Services |
At the same time, the mean access to care was 97% and 94.7% of 937 services, indicating better mental health services provided.
The results of the bed analysis are presented in Table 3. The best health services are found in the first group (mental health hospitals with more than 350 beds), followed by the second group (mental health hospitals between 200 and 350 beds), and then the third group (mental health hospitals with less than 200 beds). Furthermore, the mean and standard deviation of the results were converging.
 |
Table 3 Descriptive Statistics for Mental Health Hospitals Between Bed Categories |
As shown in Table 4, between 2018–2022, MOH mental hospitals had a slight increase. The bed capacity increased 2022 by 2% due to the Alhasa region increasing bed capacity to 100%. Furthermore, the staffing of mental health was controversial.
 |
Table 4 The Percentage of Changes in Bed Capacity, Staffing, and MOH Mental Health Services Between 2018–2022 |
The number of psychiatry residents has decreased, but the overall staffing for psychiatrists has increased. The maximum staff number of psychiatrists was recorded in the capital city of SA, followed by the third-largest province with 9.8%. At the same time, the minimum staff value was in the small rural town of SA. As shown in Figure 3, there was a massive increase in mental disorders.
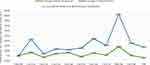 |
Figure 3 The percentage change in new mental disorder cases between 2018–2021 in Saudi Arabia. |
The expected increase was in the new patient and outpatients; this massive number was based on the International Classification of Disease (F80-F98) and followed by (F60-F69) and (F10- F19), which increased the new inpatients by more than 300%, and a slight decline in the new outpatient cases (less than 40%) in (F99), (F50-F59), and (F20-F29). New inpatient examinations had increased by 134%, especially in the total percentage of mental disorders. In comparison, new outpatients also increased by 23%.
Discussion
The study aimed to trace the performance of mental hospitals using a balanced scorecard from the Wazen program to evaluate the continuous, systematic improvement of Saudi Arabia’s mental health system. This study also attempts to measure mental hospital service changes due to implementing the Kingdom 2030 vision. This study’s results are consistent with other studies conducted in the Kingdom. More education and training in SA should be improved.3–5 The overall results are consistent with the concept that the psychiatry training environment needs more attention, especially from an integrated clinical point of view. Hence, most learning climate domains had inadequate performance, necessitating a comprehensive plan for reevaluation and improvement. As indicated earlier, many healthcare professionals may need to develop further skills in the transformational process and development in psychosociology, where most general practitioners incorrectly respond to at least 50% of the depression-related knowledge questions.4,11
Saudi Arabia is one of many countries to have medically understaffed, as the World Health Organization estimated a shortage of 15 million healthcare professionals by 2030 globally, impacting mental healthcare services severely.1,3,4,22 Less attention is paid to medical training, especially in rural areas. A successful mental healthcare program may mean sufficient quality while providing services. This shortage is exacerbated by pressures to implement more intensive and advanced mental care programs, prioritize stigma issues, and improve overall population health and wellbeing.23 Hence, initiatives to cross the disparities chasm in mental health professionals may be evaluated using standard methods for underserved individuals. This may include establishing new rural mental health services, residency support programs, utilizing telemedicine, especially in diagnosis and prognosis, and community engagement. Seeking continuous reduction of disparities among the cosmopolitan and rural areas should be a successful method of equity in mental healthcare services.24 Hence, it may be demanding to maintain competent healthcare professionals within mental healthcare services and ensure up-to-date activity within each domain.
The capital city provides the best health services in terms of bed capacity. It is located within a high number of bed capacity (mental health hospitals with more than 350 beds) and accounts for 20% of the total staff. Surprisingly, the number of licensed staff is more than doubling the percentage found in other regions. The findings of this study were consistent with those of other studies in terms of the variation of services provided in mental health facilities across the area due to inequity in health service delivered.15,24 Globally, this inequity issue is attributed to underpopulation in those regions.
As a result of the 2030 Vision, MOH focuses on developing telemedicine and telecare systems, such as enforcing 937 free-tool services and psychological and mental counseling (Qareboon) to maintain healthcare quality and equity services that may lead to efficient, quick, and free of medical errors. Wazen’s scores for call centers were among the highest, indicating that practical mobile applications were effective tools to improve mental health services. More patients were willing to utilize such services to monitor and manage their mental health and practice relaxation exercises, like Self-Help Anxiety Management apps.19,20,25 Since its inception in 2019, the Qareboon application has serviced many psychological consultations. Such results concluded that internet self-efficacy and proxy efficacy were significant determinants of intent to use digital health and social care services.
On the other hand, there has been a significant increase in mental disorder cases among new inpatients from one year to the next, as shown in this study, where the percentage of new inpatients was 134% higher in 2022 than among new inpatients in 2018. This massive increase in the number of inpatients and repeat patients in psychiatric hospitals is evidence of the development of the disease due to the delay in therapeutic intervention, which will lead to the worst outcome for the individuals, caregivers, community, and financial burdens, as well as societal problems. Most people are still embarrassed and ashamed of going to a mental health facility for treatment, believing that time will heal the disease.3 Affecting young people, the F80–F89 mental disorders had the highest prevalence of new inpatient and outpatient cases and increased significantly. This increase reflects the need to improve family and community awareness of the importance of early psychological interventions and the need for more focus on staff engagement and continued educational activity, which had the most negative domains for all hospitals.15
Recommendations
This study provides comprehensive mental health services in public and private hospitals for medical insurance that covers non-pharmacological psychological treatment. It established community psychological care centers in various regions, focused on prevention, educated the public on healthy lifestyle choices, and empowered graduates with specializations in social work and psychology. Furthermore, a recommendation is to provide employee training courses and rotating internships.
Limitations
The study has limitations, such as the unavailability of data and measurements of subdomains Wazen report. Some KPI measurements could not be analyzed; some data had been used from open-access data that needed to be updated. Finally, the limitations were the unavailability of data on bed capacity per hospital and the need for more variability in each area for the research domain and data.
Conclusion
A therapeutic ethos and a high degree of interaction between health professional cadres can manifest the quality of mental healthcare services. Many mental health facilities need more continuous educational activities and credentials while providing tertiary mental services. Our findings suggest a more focus on healthcare professionals rather than providers. This focus may include highly educated, competent, compassionate, self-aware, and specialized in mental healthcare services. Contextually, the focus on quality and therapeutic ethos is an advanced approach in mental health service evaluation.
Data Sharing Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below:
https://od.data.gov.sa/Data/ar/organization/ministry_of_health
The accumulative data supporting this study’s findings are available from the corresponding author upon request.
Ethics Statement
The study complied with the Declaration of Helsinki and was exempted by the Research Ethics Review Committee of King Saud University’s Health Administration. The ethics review approval was on 17 January 2023.
Acknowledgment
The authors extend their appreciation to Researchers Support Project number (RSP2023R332), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization (WHO). The World Health Report 2001: Mental Health: New Understanding, New Hope. World Health Organization; 2001.
2. Saudi National Health & Stress Survey (SNHSS). Available from: http://www.healthandstress.org.sa/Results/Saudi%20National%20Mental%20Health%20Survey%20-%20Technical%20Report.pdf.
3. Alangari AS, Knox SS, Innes KE, et al. Drop out from mental health treatment in the Saudi national mental health survey. Int J Ment Health. 2022;51(1):61–76. doi:10.1080/00207411.2021.1965406
4. Qureshi NA, Al-Habeeb AA, Koenig HG. Mental health system in Saudi Arabia: an overview. Neuropsychiatr Dis Treat. 2013;1121. doi:10.2147/ndt.s48782
5. Carlisle J. Mental health law in Saudi Arabia. BJPsych Int. 2018;15(1):17–19. doi:10.1192/bji.2017.10
6. Al‐Subaie AS, Al‐Habeeb A, Altwaijri YA. Overview of the Saudi national mental health survey. Int J Methods Psychiatr Res. 2020;29(3):e1835. doi:10.1002/mpr.1835
7. Alkhalifah JM, Seddiq W, Alshehri BF, Alhaluli AH, Alessa MM, Alsulais NM. The role of the COVID-19 pandemic in expediting digital healthcare transformation: Saudi Arabia’s experience. Inform Med Unlocked. 2022;33:101097. doi:10.1016/j.imu.2022.101097
8. Ministry Of Health (MOH). 937 services, Ministry of Health Saudi Arabia. Available from: https://www.moh.gov.sa/en/937/Pages/default.aspx.
9. Al Rowily A, Aloudah N, Jalal Z, Abutaleb MH, Paudyal V. Views, experiences and contributory factors related to medication errors associated with direct oral anticoagulants: a qualitative study with physicians and nurses. Int J Clin Pharm. 2022;44(4):1057–1066. doi:10.1007/s11096-022-01448-x
10. Ministry Of Health (MOH). MOH organizes the 1st Wazen program forum, Ministry of Health Saudi Arabia. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-01-23-004.aspx.
11. Alshomrani AT, AlHadi AN. Learning environment of the Saudi psychiatry board training program. Saudi Med J. 2017;38(6):629–635. doi:10.15537/smj.2017.6.18164
12. Al-Atram AA. Physicians’ knowledge and attitude towards mental health in Saudi Arabia. Ethiop J Health Sci. 2018;28(6):771–778. doi:10.4314/ejhs.v28i6.12
13. Van Gaans D, Dent E. Issues of access to health services by older Australians: a review. Public Health Rev. 2018;39(1):1–16. doi:10.1186/s40985-018-0097-4
14. Mindu T, Mutero IT, Ngcobo WB, Musesengwa R, Chimbari MJ. Digital mental health interventions for young people in rural South Africa: prospects and challenges for implementation. Int J Environ Res Public Health. 2023;20(2):1453. doi:10.3390/ijerph20021453
15. Fitzpatrick SJ, Perkins D, Luland T, Brown D, Corvan E. The effect of context in rural mental health care: understanding Integrated Services in a small town, health & place. US National Library of Medicine. Available from: https://pubmed.ncbi.nlm.nih.gov/28288445/.
16. Eriksen AA, Fegran L, Fredwall TE, Larsen IB. Patients’ negative experiences with health care settings brought to light by formal complaints: a qualitative meta-synthesis. J Clin Nurs. 2023;32(17–18):5816–5835. doi:10.1111/jocn.16704
17. Abolfotouh MA, Almutairi AF, Almutairi Z, et al. Attitudes toward mental illness, mentally ill persons, and help-seeking among the Saudi public and socio-demographic correlates. Psychol Res Behav Manag. 2019;Volume 12:45–54. doi:10.2147/prbm.s191676
18. Ministry Of Health (MOH). 937 services, Ministry of Health Saudi Arabia. Available from: https://www.moh.gov.sa/en/937/Pages/default.aspx.
19. Alqahtani F, Winn A, Orji R. Co-designing a mobile app to improve mental health and wellbeing: focus group study. JMIR Form Res. 2021;5(2):e18172. doi:10.1177/1460458219896492
20. Atallah N, Khalifa M, El Metwally A, Househ M. The prevalence and usage of mobile health applications among mental health patients in Saudi Arabia. Comput Methods Programs Biomed. 2018;156:163–168. doi:10.1016/j.cmpb.2017.12.0022196/18172doi:10.4314/eggs.v28i6.12doi:10.1080/
21. National Center for Mental Health Promotion (NCMHP). Available from: https://ncmh.org.sa/view/16/3th.
22. Liu JX, Goryakin Y, Maeda A, Bruckner T, Scheffler R. Global health workforce labor market projections for 2030. Hum Resour Health. 2017;15(1):1–12. doi:10.1186/s12960-017-0193-4
23. Merwin E, Hinton I, Dembling B, Stern S. Shortages of rural mental health professionals. Arch Psychiatr Nurs. 2003;17(1):42–51. doi:10.1053/apnu.2003.1
24. Hailemariam M, Fekadu A, Medhin G, et al. Equitable access to mental healthcare integrated into primary care for people with severe mental disorders in rural Ethiopia: a community-based cross-sectional study. Int J Ment Health Syst. 2019;13(1). doi:10.1186/s13033-019-0332-5
25. Chandran D, Aljohani N. Adoption of M-Health applications: the Saudi Arabian healthcare perspectives. ACIS Proc. 2019;180–186. doi:10.1192/bji.2017.1000207411.2021.1965406
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
