Back to Journals » Clinical Ophthalmology » Volume 16
Maximal Levator Resection Beyond Whitnall’s Ligament in Severe Simple Congenital Ptosis with Poor Levator Function
Authors Wuthisiri W , Peou C, Lekskul A , Chokthaweesak W
Received 23 September 2021
Accepted for publication 26 January 2022
Published 17 February 2022 Volume 2022:16 Pages 441—452
DOI https://doi.org/10.2147/OPTH.S340781
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Wadakarn Wuthisiri,1 Channy Peou,2 Apatsa Lekskul,1 Weerawan Chokthaweesak1
1Department of Ophthalmology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Department of Ophthalmology International University, Phnom Penh, Cambodia
Correspondence: Weerawan Chokthaweesak, Department of Ophthalmology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Ratchatewi, Bangkok, 10400, Thailand, Tel +66 2 201 2729, Fax +66 2 201 1516, Email [email protected]
Purpose: To evaluate the functional and cosmetic outcomes, as well as factors that influence surgical success of maximal levator resection beyond Whitnall’s ligament in patients with poor levator function (LF) and severe simple congenital ptosis.
Methods: This retrospective interventional study included patients with severe simple congenital ptosis and LF of ≤ 4 mm who had undergone maximal levator resection beyond Whitnall’s ligament with a minimum of 12 months follow-up. Postoperative marginal reflex distance-1 (MRD1) was assessed for functional outcomes as excellent, good, fair and poor. Eyelid contour and the difference in MRD1 between eyes were assessed for symmetrical cosmetic outcomes as excellent, good and poor. Demographic data, factors influencing surgical success and postoperative complications were analyzed.
Results: A total of 38 ptotic eyelids in 31 patients were included. Successful surgical outcomes (at least good functional and cosmetic outcomes) were achieved in 26 patients (83.87%) with the mean MRD1 of +3.61 ± 0.27 mm and +3.51 ± 0.17 mm at 1 week and 12 months after surgery, respectively. There were no significant differences in demographic and preoperative data between the successful and unsuccessful surgical outcome groups, mean preoperative ptosis measurements were 4.19 ± 0.20 mm versus 4.72 ± 0.36 mm (p = 0.242) and mean pre-operative LF were 3.16 ± 0.15 mm versus 2.29 ± 0.61 mm (p = 0.561), respectively. The only factor that significantly influenced the surgical success rate was the length of the resected levator muscle. The mean lengths in successful and unsuccessful groups were 18.15 ± 0.44 mm and 14.29 ± 0.94 mm, respectively (p = 0.011).
Conclusion: Maximal levator resection beyond Whitnall’s ligament is an effective procedure for severe simple congenital ptosis with poor LF. Refinement of surgical techniques and careful assessment of the optimal resected length for the levator muscle grants successful surgical outcomes.
Keywords: simple congenital ptosis, poor levator function, maximal levator resection, Whitnall’s ligament
Introduction
Congenital ptosis is defined as a vertical narrowing of the palpebral fissure caused by an abnormal drooping of upper eyelid from birth. It is usually persistent and generally non-progressive. Congenital ptosis can occur in isolation or associated with a spectrum of other oculopalpebral disorders or as a part of complex syndromic diseases.1,2
The main pathophysiology of simple congenital ptosis is levator palpebrae superioris (LPS) muscle dysgenesis which leads to the classic triad of ptosis in the primary position, lagophthalmos, and a poorly formed eyelid crease. The degree of striated muscle fiber deficiency and fibro-fatty substitution in this poorly developed muscle usually serve as a direct indicator of its function and the disease severity.2–4
Traditionally, levator resection has been reserved for patients with levator function (LF) >4 mm.2–4 Frontalis muscle suspension or frontalis muscle flap transfer was considered as the preferred surgical techniques for patients with poor LF and severe ptosis. Frontalis suspension has previously been reported as the most effective treatment in this circumstance.1,2,5 However, suspensory material-related problems continue to be the major weakness of this procedure.2,5 Moreover, undercorrection and treatment failure in unilateral suspension is also another drawback.2
Various reports have confirmed favorable surgical outcomes for levator muscle surgeries in patients who exhibit severe simple congenital ptosis with poor LF.6–10 Several levator muscle strengthening techniques have been reported in the literature.6–12 However, the advantages and disadvantages of resection or preservation of the levator horns along with Whitnall’s ligament (WL) remain controversial.6–12
After with confronting problems associated with frontalis muscle suspension technique for several years, we have made substantial changes in our surgical practice to levator muscle procedures. This study highlights the surgical approach, functional and cosmetic outcomes, factors influencing surgical success and safety profile of full thickness, maximal levator resection beyond Whitnall’s ligament in patients who have severe simple congenital ptosis with poor LF performed by a single surgeon (WW).
Materials and Methods
This retrospective study reviewed electronic medical records of all patients who exhibited severe simple congenital ptosis with poor LF and had undergone maximal levator resection beyond Whitnall’s ligament by a single surgeon (WW) at Ramathibodi Hospital (a tertiary referral center in Bangkok, Thailand) from January 1st, 2015 to December 31st, 2019. The study protocol adhered to the tenets of the Health Insurance Portability and Accountability Act and the Declaration of Helsinki. The Human Research Ethics Committee, Faculty of Medicine, Ramathibodi Hospital, Mahidol University approved the study, the ethics approval number MURA2020/262. Patient informed consent was waived for this study.
Patients
This study included patients who had unilateral or bilateral severe simple congenital ptosis with LF ≤ 4 mm. Patients were excluded if they met any of the following criteria: postnatally acquired ptosis, syndrome-associated ptosis, neurogenic disturbances, the Marcus Gunn phenomenon, a history of previous trauma or eyelid surgery, LF > 4 mm and postoperative follow-up period <12 months.
Clinical Evaluations
All patients had undergone a thorough ophthalmic evaluation. Preoperative and postoperative evaluations (at 1 week, followed by 1, 3, 6, and 12 months postoperatively) were performed at the Ramathibodi hospital by the same single surgeon (WW).
Data were recorded regarding demographic characteristics, ptosis laterality, pre- and postoperative marginal reflex distance-1 (MRD1), amount of preoperative ptosis, LF, Bell’s phenomenon, extraocular movement, ocular alignment, pupils, amount of resected levator muscle, eyelid contour, and all postoperative unfavorable outcomes.
Clinical MRD1 measurements and eyelid contour assessments were performed and photographs were acquired (Figure 1). In accordance with the approach described by Berk and Wadsworth,4 the severity of ptosis was classified as mild, moderate, and severe when the extent of upper eyelid margin drooping in the primary gaze were ≤2 mm, 3 mm, and ≥4 mm, respectively. These values were compared with the average MRD1 in the general population which has been reported as +4 mm.3,4
The extent of upper eyelid excursion from maximum downgaze to maximum upgaze with the eyebrow immobilized to limit frontalis muscle function (as Beard advocated)3 was used to classified LF as good LF (8–16 mm), fair LF (5–7 mm), and poor LF (≤4 mm).
Evaluation of Postoperative Outcomes
Postoperative outcomes were divided into two categories: functional and cosmetic (symmetrical correction with respect to the fellow eye). Postoperative MRD1 was used for functional outcome assessment. It was considered excellent if MRD1 ≥ +3 mm, good if MRD1 +2 mm, fair if MRD1 +1 mm, and poor if MRD1 ≤0. Eyelid contour and the difference in MRD1 between eyes were assessed for symmetrical cosmetic outcomes. These were defined as excellent, good, and poor when the differences were ≤1 mm, 1–2 mm, and >2 mm, respectively. At 12 months postoperative period, surgical outcomes were considered successful in patients who had at least good functional outcome (MRD1 ≥ +2 mm) and at least good symmetrical cosmetic outcome (difference in MRD1 ≤2 mm) combined with a favorable eyelid contour. Factors influencing surgical success and postoperative complications were also analyzed.
Statistical Analysis
Descriptive statistics are reported as means ± standard deviations for continuous variables and frequencies (percentages) for categorical variables. Statistical analysis was performed using SPSS software, version 18.0. Paired-samples t-tests were used for comparisons of age at surgery, amount of ptosis, preoperative LF, and length of resected LPS muscle parameters to identify factors associated with successful and unsuccessful surgical outcomes. Differences were considered statistically significant when p < 0.05.
Surgical Procedure
Full-thickness maximal levator resection beyond Whitnall’s ligament was performed using a modified version of the procedure described by Berke.13 (Figure 2) All surgeries were performed under general anesthesia. The desired upper eyelid crease was marked and 1% lidocaine with 1:100,000 epinephrine was then subcutaneously injected for hemostasis. An incision was made in the previously marked line, and then a skin and pre-septal orbicularis oculi muscle flap was raised to reach orbital septum (Figure 2A). The orbital septum was horizontally opened to expose pre-aponeurotic fat (Figure 2B). Beneath the pre-aponeurotic fat, the levator aponeurosis was carefully identified and gently dissected superiorly until the level above Whitnall’s ligament was reached (Figure 2C). Next, the upper one-third of the tarsus was then cleaned and clearly exposed (Figure 2D). Subsequently, two small full-thickness incisions were made through the levator aponeurosis, Muller’s muscle and conjunctiva and these incisions were created close to the superior tarsal border at either end of the skin incision. Using these two small incisions, the Berke ptosis clamp was placed (Figure 2E) to include levator aponeurosis, Muller’s muscle and conjunctiva. These were freed from their attachments at the superior tarsal border (Figure 2F). To achieve the desired length of the levator-Muller muscle flap, in the cephalad direction, the medial and lateral horns of the levator aponeurosis together with the superiorly oriented Whitnall’s ligament were released. A straight upward cut was performed, to avoid damage to the superior oblique muscle nasally and the lacrimal gland temporally.12 This allowed substantial flap mobilization (Figure 2G). At this stage of the surgery, we believe that this is an important step to gain sufficient levator muscle length while also reducing the likelihood of postsurgical lagophthalmos. Next, the palpebral conjunctiva was ballooned with an injection of 1% lidocaine with 1:100,000 epinephrine (Figure 2G) and fully separated from the posterior surface of Muller’s muscle. This was then re-attached to the superior tarsal border with a 7–0 Vicryl running suture (Figure 2H and I). Subsequently, the levator-Muller’s muscle flap was returned to the anterior surface (not below superior 1/3) of the tarsus, using 6–0 Vicryl sutures (Figure 2J). At this step of surgery, we estimated the desired length of levator-Muller’s muscle flap resection as previously described by Berke.13 The preoperative LF was used as a guide to determine the level of eyelid height during surgery. The eyelid margin position was adjusted intraoperatively to achieve the desired level at the superior limbus in accordance with Berke’s recommendation regarding surgical candidates with LF < 8 mm11,12 The first central fixation suture was usually placed at or above the level of Whitnall’s ligament. For suitable eyelid contour adjustment, two additional fixation sutures were placed nasally and temporally (Figure 2K). The length of the redundant levator-Muller’s muscle flap was measured before resection (Figure 2L). The eyelid crease was established by fixing the subcutaneous tissue and pre-tarsal orbicularis oculi to the previously resected levator muscle border using 6–0 vicryl sutures in an interrupted manner. The skin was closed with a 6–0 nylon suture (Figure 2M).
 |
Figure 2 Surgical procedure; full-thickness maximal levator resection beyond Whitnall’s ligament, modified from Berke technique.13 (A) eyelid crease skin incision. (B) orbital septum was opened to exposed preaponeurotic fat. (C) preaponeurotic fat was separated from the underlying levator aponeurosis. (D) superior 1/3 of tarsal plate was clearly exposed. (E) The Berke ptosis clamp was placed. (F) levator aponeurosis, Muller’s muscle, and conjunctiva were entirely detached from tarsus. (G) straight upward cuts to release the horns of the levator aponeurosis together with Whitnall’s ligament, and 1% lidocaine with 1:100,000 epinephrine was subconjunctivally injected. (H and I), palpebral conjunctiva was freed from the levator-Muller’s muscle flap, and reattached to superior boarder of tarsus. (J) the levator-Muller’s muscle flap was reinserted to the anterior surface (not below superior 1/3) of the tarsus (K) two additional fixation sutures were placed nasally and temporally for good eyelid contour. (L) the length of the redundant levator-Muller’s muscle flap was measured before resection. (M) the eyelid crease was created, and skin was closed. |
Results
A total, 38 eyes from 31 patients were enrolled. All patients were of Asian ethnicity. Eighteen patients (58%) were male and 24 patients (77.42%) had unilateral disease. Table 1 shows the comparative analyses of demographic and clinical parameters between successful and unsuccessful surgical outcome groups. The mean age of the successful and unsuccessful surgical outcome groups on the day of surgery were 5.66 ± 0.82 years and 4.04 ± 0.63 years, respectively (p = 0.363). The mean amount of preoperative ptosis were 4.19 ± 0.20 mm and 4.72 ± 0.36 mm (p = 0.242) and the mean preoperative LF were 3.16 ± 0.15 mm and 2.29 ± 0.61 mm, respectively (p = 0.561). The only factor that significantly influenced surgical success was the mean length of resected levator muscle. The mean lengths in successful and unsuccessful groups were 18.15 ± 0.44 mm and 14.29 ± 0.94 mm, respectively (p = 0.011).
 |
Table 1 Comparison of Demographic and Clinical Data Between Outcome Groups (31 Patients, 38 Eyelids) |
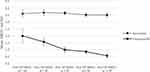
Successful surgical outcomes (Figure 1) were achieved in 26 patients (83.87%) with the mean MRD1 of +3.61 ± 0.27 mm at 1 week postoperatively. Respective mean MRD1 of +3.68 ± 0.22 mm, +3.65 ± 0.16 mm, +3.52 ± 0.17 mm, and +3.51 ± 0.17 mm were maintained at 1, 3, 6 and 12 months postoperatively in the successful surgical outcome group. In the unsuccessful surgical outcome group, the mean MRD1 at 1 week postoperatively was +2.00 ± 0.49 mm, significantly lower than the MRD1 in the successful group. This mean value gradually declined to +1.57 ± 0.30 mm, +1.00 ± 0.22 mm, +0.86 ± 0.14 mm, and +0.57 ± 0.20 mm at 1, 3, 6 and 12 months postoperatively, respectively (Table 2, Figure 3).
The results of functional outcome assessment are shown in Table 3. Excellent and good functional outcomes were achieved in 31 of 38 eyes (81.58%) at 12 months postoperatively. The results of symmetrical cosmetic outcomes are shown in Table 4 (only patients with unilateral disease were included in this analysis). Notably, excellent and good symmetrical cosmetic outcomes were achieved in 21 of 24 patients (87.5%) at 12 months postoperatively.
 |
Table 2 Comparison of Postoperative Results (MRD1) Between Outcome Groups, Assessed Over Time |
 |
Table 3 Postoperative Functional Outcomes Assessed Over Time in 38 Eyelids |
 |
Table 4 Postoperative Symmetrical Cosmetic Outcomes in Patients with Unilateral Disease, Assessed Over Time in 24 Patients (MRD1 Compared Between Eyes) |
Surgical complications (Table 5) included lagophthalmos (81.58%) and found that the severity of lagophthalmos and ocular surface exposure gradually decreased overtime (Figure 4), exposure keratopathy (26.31%) which controlled by artificial tears and ointment without further surgical correction, postoperative corneal astigmatism (31.58%), undercorrection or recurrence of ptosis; MRD1 ≤ +1 mm at 12 months postoperatively (18.42%) and 57.14% of the recurrent ptotic eyelids required ptosis revision surgery by the same surgical technique and the results were satisfactory, redundant and prolapsed conjunctiva (2.6%) which required surgical resection and rearrangement, and disparity of eyelids in down gaze (77.41%). Although the incidence of preoperative amblyopia in this study was high (45.16%), most affected patients exhibited only mild amblyopia (32.26%). Furthermore, most patients with amblyopia responded to treatments which included glasses and/or postoperative eye patching.
 |
Table 5 Complications of Maximal Levator Resection Beyond Whitnall’s Ligament in Patients Who Had Severe Simple Congenital Ptosis with Poor Levator Function |
 |
Figure 4 Photographs demonstrated improvement in postoperative lagophthalmos over time. Abbreviation: Post op, postoperative. |
Discussion
Simple congenital ptosis is the most common ptosis in children and constitutes approximately 69–84% of all pediatric patients who presented with ptosis.5,14,15 Overall, the most common manifestation is unilateral disease (approximately 65–72%).1,3,14,15 We found a similar distribution pattern in the present study (77.42% of the included patients exhibited unilateral disease).
In patients with severe ptosis, visual axis obstruction threatens normal visual development potentially leading to stimulus deprivation or astigmatic refractive amblyopia. Therefore, appropriate and timely management is essential for the maintenance of normal visual development and function. Moreover, normal aesthetic appearance and psychosocial development are important considerations in pediatric patients.
To achieve an optimal surgical outcome, while minimizing potential unfavorable results, factors associated with surgical selection should depend entirely upon the severity of ptosis, LF, and ptosis laterality, as well as the surgeon’s expertise and preference.3
There are currently several surgical options proposed for patients with severe simple congenital ptosis and poor LF with variable outcomes and complications, the most appropriate surgical approach continues to be a difficult challenge and continues to be controversial.5–12
As mentioned previously, in patients with poor LF (≤4 mm), the common surgical approach involves the creation of the frontalis muscle suspension. This requires direct attachment of the frontalis muscle to the tarsal plate and therefore completely bypasses the poorly functioning levator muscle. This method had gained favorable outcomes.1,2,5 However, several problems related to alloplastic suspensory materials had been reported, including material exposure, extrusion, infection, granuloma formations, and recurrence of ptosis. Autogenous fascia lata may allow better biocompatibility with the fewer potential problems.2,5 However, harvesting surgery may not be appropriate in patients younger than 3 years of age, as adequate length of fascia lata may be unobtainable and there is also a risk of donor-site scar formation.2 Eyelid lag or disparity between the eyelids on downgaze in unilateral frontalis suspension is another disadvantage. In order to reduce the potential asymmetry between the two eyes, the creation of bilateral frontalis suspension by disinsertion of the healthy levator muscle (as recommended by Beard)3 remains an argumentative procedure. This can hardly be accepted by most of the parents as this procedure can lead to iatrogenic severe ptosis, in a previously normal eyelid. Although the modified classic Beard technique16 involves bilateral suspension without disinsertion of the healthy levator muscle, most parents still prefer unilateral surgery that solely involves the abnormal eyelid. Moreover, the spontaneous brow elevation is always needed to pull the upper eyelid up after frontalis muscle procedures. Patients with unilateral ptosis who are susceptible to develop amblyopia might fail to do one-side spontaneous brow elevation which can lead to insufficient eyelid elevation and frequent undercorrection or treatment failure.5
Over the past several decades, various reports have confirmed the satisfactory and successful surgical results of levator muscle surgeries in patients who exhibit severe simple congenital ptosis with poor LF.6–12 There are many advantages including no suspensory materials required, a lack of dependency on brow elevation for eyelid opening, fewer complications, lower recurrence rate, more physiological elevation and evidence of postoperative LF improvement.6–9
Traditionally, levator resection is often reserved for patients with LF >4 mm.2–4 In order to achieve optimal results in patients with poor LF, Whitnall sling procedure8,9 or even maximal levator resection beyond Whitnall’s ligament which is also known as super- or supra maximal levator resection6,7 is required. However, controversy remains regarding the preservation or resection of the levator horns combined with Whitnall’s ligament. In the past conceptual framework, the Whitnall’s ligament was defined as a superior supportive ligament of the upper eyelid and orbit, as well as orbital support of the lacrimal gland. This structure is also believed to function as a fixed fulcrum for changing the direction of force of the LPS from anteroposterior to a vertical direction, and may be an important structure responsible for elevation of the upper eyelid7,9 and thus, should be preserved in ptosis surgery.17,18 Recent studies have modified the classical conceptual framework through anatomical dissection and images analysis (MRI) in particular, Whitnall’s ligament is situated anterior to the culminating point of the LPS and thus, is not responsible for the curved course of the levator muscle.17–19 According to these studies, along with author’s experience, support the fact that severing of Whitnall’s ligament does not cause an adverse consequence and there is no lacrimal gland prolapse resulting from the same.6,19,20 For successful surgical outcomes, Whitnall’s ligament releases at its attachments will provide sufficient length of levator muscle for resection, and substantial mobilization of LPS after the Whitnall’s ligament resection should decrease the occurrence of postoperative lagophthalmos. However, the elastic properties of the eyelid are severely impaired after resection of the large sections of LPS muscle with downward saccadic movements restriction leading to lid lag and lagophthalmos will eventually occur.12 The superficial keratopathy related to diminish spontaneous blinking amplitude will be notable in the early postsurgical period and intensive lubrication is needed. The ocular surface will adjust to new eyelid kinetic over time,12 and the same was found in this study.
In our study, successful surgical outcomes which refer as at least good functional outcome (MRD1 ≥ +2 mm) and at least good symmetrical cosmetic outcomes (within 2 mm of symmetry between both eyelids) were achieved in a manner similar to previous studies.1,7,10,12,21–24
In pediatric patients, an intraoperative assessment of the optimal amount of levator muscle resection to achieve a satisfactory postoperative result is challenging, as patient cooperation during surgery is not possible, while general anesthesia may alter extraocular muscle tone and globe position.11 In an attempt to overcome this problem Berke13 developed a system which used the preoperative LF as a guide to determine the eyelid margin position during surgery. More specifically, for LF of 8 mm, the eyelid margin was set at the desired height (2 mm covering limbus) intraoperatively; for LF of <8 mm, the eyelid margin was set higher than the desired height; for LF of >8 mm, the eyelid margin was set lower than the desired height.11–13,25 This intraoperative clinical adjustment system was used for all patients in our study. Also, note that the mean preoperative LF in the successful and unsuccessful surgical outcome groups were similar (3.16 ± 0.15 mm and 2.29 ± 0.61 mm (p = 0.561), respectively), and we found that the actual lengths of the resected levator muscle were unequal even in patients with the same LF (18.15 ± 0.44 mm in successful and 14.29 ± 0.94 mm in unsuccessful surgical outcome group, p = 0.011). Thus, the length of levator muscle resection was not determined solely by the preoperative LF. The only factor that appeared to significantly influence surgical success was the length of the resected levator muscle. The use of a single intraoperative clinical adjustment algorithm may be insufficient for an accurate prediction of the postoperative lid position. In the present study, we attempted to establish the correlation between the severity of ptosis, the preoperative LF and the length of levator muscle resection. However, due to small sample size, the correlation did not reach statistical significance.
Compared with previous studies,7,10,12,22,24 the length of levator muscle resection in this study was shorter. This could be explained by the differences in measurement methods along with the differences in intraoperative traction exerted on the LPS muscle during the measurement.
The normal vertical palpebral fissure height is narrower in the eyes of Asian individuals (8–8.5 mm) than in the eyes of Caucasian individuals (8–10 mm).26–28 Suhk et al29 reported that MRD1 in Asian individuals were 3–3.5 mm whereas Caucasian individuals were 4–4.5 mm. With this reference in mind, the criteria for an excellent functional outcome and a successful surgical outcome were taken as MRD1 ≥ +3 mm and ≥ +2 mm (as this eyelid level does not cover the visual axis which is sufficient for amblyopia correction), respectively.
The optimal timing of surgical correction in congenital ptosis is controversial, especially in patients with non-amblyogenic ptosis. However, children who develop deprivation amblyopia (particularly in unilateral cases) may require early surgical intervention before 6 months of age.2 Previous reports30–32 showed that earlier surgical intervention was associated with a greater rate of ptosis recurrence. Quaranta-Leoni et al30 reported no ptosis recurrence when surgical correction was performed in children aged 2–4 years compared with 22% recurrence in other age groups. Harvey et al11 recommended delaying levator resection until a child is at least 3 years of age as this would allow full anatomical development of the eyelid. In the present study, we found a slightly younger mean age in the unsuccessful surgical outcome group, but this difference was not statistically significant. Notably, the youngest patient with a successful outcome was 1 year old at the time of surgery.
Complications of surgery in our study included undercorrection or recurrence of ptosis in 18.42% (seven eyes) and four eyes required reoperation. Along with the same surgical technique, additional length of the LPS muscle was resected and the successful outcomes were achieved. Most patients (81.58%) developed lagophthalmos and the explanation of the reasons for its occurrence have been discussed previously; however, the severity of ocular surface exposure gradually decreases over time. Ten eyes (26.31%) developed mild to moderate exposure keratopathy that was sufficiently controlled with artificial tears and ointment. This confirms the assumption of the adaptation of ocular surface to new eyelid kinetic over time. Theoretically, a significant shortening of posterior lamellar after supra-maximal levator resection should induce postoperative entropion or lash ptosis.12 Probably, with the eye lashes rotating sutures (fixation of the pretarsal skin-muscle flap on the resected LPS muscle margin) that was performed in all patients eradicated this unfavorable outcome. Twelve eyes (31.58%) in nine patients developed postoperative corneal astigmatism as eyelid tightening after maximal levator resection may have caused pressure on the cornea. Furthermore, fourteen patients (45.16%) developed preoperative amblyopia either from refractive astigmatism or deprivation ptosis. However, most patients developed only mild amblyopia (10 patients, 32.26%) which responded to treatment comprising optical correction and eye patching after surgery. Only one patient exhibited conjunctival prolapse that required surgical resection and rearrangement. All patients with unilateral disease (24 patients, 77.41%) developed eyelid disparity in downgaze. Fortunately, this gradually decreased over time and found that it was not as pronounced as compared to post unilateral frontalis suspension surgery in our experience.
All preoperative clinical evaluations and surgical steps were performed by a single surgeon (WW) who used the same technique throughout the procedures. However, there were several limitations in this study because of its retrospective study design and incomplete data collection. As all patients were children this might have led to errors in preoperative and postoperative measurements. Furthermore, we included both unilateral and bilateral ptotic patients which in clinical practice should be approached in different way with regard to treatment response. Finally, the sample size was small and future studies with larger sample sizes and longer follow-up periods are needed to provide further validation of treatment safety, efficacy and possibly refine the previous surgical algorithm.
Conclusion
This study demonstrates the effectiveness of maximal levator resection beyond Whitnall’s ligament in patients who have severe simple congenital ptosis with poor LF. This confirms competency of the procedure as a good alternative to frontalis suspension. Refinement of the surgical techniques could further enhance the surgical success. The release of Whitnall’s ligament at its attachments followed by levator resection beyond this level and careful assessment of the optimal extent of levator muscle resection can provide satisfactory and successful surgical outcomes in terms of functional and cosmetic aspects with an acceptable safety profile.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee JH, Kim YD. Surgical treatment of unilateral severe simple congenital ptosis. Taiwan J Ophthalmol. 2018;8(1):3–8. doi:10.4103/tjo.tjo_70_17
2. Weaver DT. Current management of childhood ptosis. Curr Opin Ophthalmol.2018;29(5):395–400. doi:10.1097/ICU.0000000000000508
3. Beard C. The surgical treatment of blepharoptosis: a quantitative approach. Trans Am Ophthalmol Soc. 1966;64:401–487.
4. Berke RN, Wadsworth JAC. Histology of levator muscle in congenital and acquired ptosis. AMA Arch Ophthalmol. 1955;53(3):413–428. doi:10.1001/archopht.1955.00930010415017
5. Bernardini FP, Cetinkaya A, Zambelli A. Treatment of unilateral congenital ptosis: putting the debate to rest. Curr Opin Ophthalmol. 2013;24(5):484–487. doi:10.1097/ICU.0b013e328363861a
6. Pak J, Shields M, Putterman AM. Superior tarsectomy augments super-maximum levator resection in correction of severe blepharoptosis with poor levator function. Ophthalmology. 2006;113(7):1201–1208. doi:10.1016/j.ophtha.2006.01.032
7. Epstein GA, Putterman AM. Super-maximum levator resection for severe unilateral congenital blepharoptosis. Ophthalmic Surg. 1984;15(12):971–979.
8. Anderson RL, Jordan DR, Dutton JJ. Whitnall’s sling for poor function ptosis. Arch Ophthalmol. 1990;108(11):1628–1632. doi:10.1001/archopht.1990.01070130130043
9. Holds JB, McLeish WM, Anderson RL. Whitnall’s sling with superior tarsectomy for the correction of severe unilateral blepharoptosis. Arch Ophthalmol.1993;111(9):1285–1291. doi:10.1001/archopht.1993.01090090137032
10. Lee JH, Aryasit O, Kim YD, Woo KI, Lee L, Johnson ON. Maximal levator resection in unilateral congenital ptosis with poor levator function. Br J Ophthalmol. 2017;101(6):740–746. doi:10.1136/bjophthalmol-2016-309163
11. Harvey DJ, Iamphongsai S, Gosain AK. Unilateral congenital blepharoptosis repair by anterior levator advancement and resection: an educational review. Plast Reconstr Surg. 2010;126(4):1325–1331. doi:10.1097/PRS.0b013e3181ebe1e9
12. Cruz AA, Akaishi PM, Mendonca AK, Bernadini F, Devoto M, Garcia DM. Supramaximal levator resection for unilateral congenital ptosis: cosmetic and functional results. Ophthalmic Plast Reconstr Surg. 2014;30(5):366–371. doi:10.1097/IOP.0000000000000105
13. Berke RN. Results of resection of the levator muscle through a skin incision in congenital ptosis. Trans Am Ophthalmol Soc. 1958;56:
14. El Essawy R, Elsada MA. Clinical and demographic characteristics of ptosis in children: a national tertiary hospital study. Eur J Ophthalmol. 2013;23(3):356–360. doi:10.5301/ejo.5000239
15. Griepentrog GJ, Diehl NN, Mohney BG. Incidence and demographics of childhood ptosis. Ophthalmology. 2011;118(6):1180–1183. doi:10.1016/j.ophtha.2010.10.026
16. Callahan A. Correction of unilateral blepharoptosis with bilateral eyelid suspension. Am J Ophthalmol. 1972;74(2):321–326. doi:10.1016/0002-9394(72)90553-3
17. Goldberg RA, Wu JC, Jesmanowicz A, Hyde JS. Eyelid anatomy revisited. Dynamic high-resolution magnetic resonance images of Whitnall’s ligament and upper eyelid structures with the use of a surface coil. Arch Ophthalmol. 1992;110(11):1598–1600. doi:10.1001/archopht.1992.01080230098030
18. Ettl A, Zonneveld F, Daxer A, Koornneef L. Is Whitnall’s ligament responsible for the curved course of the levator palpebrae superioris muscle? Ophthalmic Res. 1998;30(5):321–326. doi:10.1159/000055491
19. Anderson RL, Dixon RS. The role of Whitnall’s ligament in ptosis surgery. Arch Ophthalmol. 1979;97(4):705–707. doi:10.1001/archopht.1979.01020010357015
20. Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Arch Ophthalmol. 1979;97(6):1123–1128. doi:10.1001/archopht.1979.01020010577015
21. Mauriello JA, Wagner RS, Caputo AR, Natale B, Lister M. Treatment of congenital ptosis by maximal levator resection. Ophthalmology. 1986;93(4):466–469. doi:10.1016/s0161-6420(86)33714-x
22. Press UP, Hubner H. Maximal levator resection in the treatment of unilateral congenital ptosis with poor levator function. Orbit. 2001;20(2):125–129. doi:10.1076/orbi.20.2.125.2631
23. Park DH, Choi WS, Yoon SH, Shim JS. Comparison of levator resection and frontalis muscle transfer in the treatment of severe blepharoptosis. Ann Plast Surg. 2007;59(4):388–392. doi:10.1097/01.sap.0000258456.24810.c8
24. Mete A, Cagatay HH, Pamukcu C, Kimyon S, Saygili O, Gungor K. Maximal levator muscle resection for primary congenital blepharoptosis with poor levator function. Semin Ophthalmol. 2017;32(3):270–275. doi:10.3109/08820538.2015.1068339
25. Cates CA, Tyers AG. Outcomes of anterior levator resection in congenital blepharoptosis. Eye. 2001;15(Pt 6):770–773. doi:10.1038/eye.2001.247
26. Park DH, Choi WS, Yoon SH, Song CH. Anthropometry of asian eyelids by age. Plast Reconstr Surg. 2008;121(4):1405–1413. doi:10.1097/01.prs.0000304608.33432.67
27. Saonanon P. Update on Asian eyelid anatomy and clinical relevance. Curr Opin Ophthalmol. 2014;25(5):436–442. doi:10.1097/ICU.0000000000000075
28. Ho YF, Wu SY, Tsai YJ. Factors associated with surgical outcomes in congenital ptosis: a 10-year study of 319 cases. Am J Ophthalmol. 2017;175:173–182. doi:10.1016/j.ajo.2016.12.013
29. Suhk JH, Kiranantawat K, Nguyen AH. Physical evaluation of the Asian blepharoplasty patient. Semin Plast Surg. 2015;29(3):145–157. doi:10.1055/s-0035-1556851
30. Quaranta-Leoni FM, Sposato S, Leonardi A, Iacoviello L, Costanzo S. Timing of surgical correction for the treatment of unilateral congenital ptosis: effects on cosmetic and functional results. Orbit. 2017;36(6):382–387. doi:10.1080/01676830.2017.1337191
31. Skaat A, Fabian D, Spierer A, Rosen N, Rosner M, Ben Simon GJ. Congenital ptosis repair-surgical, cosmetic, and functional outcome: a report of 162 cases. Can J Ophthalmol. 2013;48(2):93–98. doi:10.1016/j.jcjo.2012.09.010
32. Wu SY, Ma L, Huang HH, Tsai YJ. Analysis of visual outcomes and complications following levator resection for unilateral congenital blepharoptosis without strabismus. Biomed J. 2013;36(4):179–187. doi:10.4103/2319-4170.113854
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.