Back to Journals » Pragmatic and Observational Research » Volume 10
Management Of Community-Acquired Pneumonia: An Observational Study In UK Primary Care
Authors Launders N, Ryan D , Winchester CC , Skinner D , Konduru PR, Price DB
Received 4 April 2019
Accepted for publication 23 August 2019
Published 23 September 2019 Volume 2019:10 Pages 53—65
DOI https://doi.org/10.2147/POR.S211198
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Christoph R Meier
Naomi Launders,1 Dermot Ryan,2 Christopher C Winchester,3 Derek Skinner,4 Priyanka Raju Konduru,4 David B Price4
1Respiratory Effectiveness Group, Cambridge, UK; 2Allergy and Respiratory Research Group, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Medical School, Edinburgh EH8 9AG, Scotland; 3Oxford PharmaGenesis, Oxford, UK; 4Observational and Pragmatic Research Institute Pte Ltd, Singapore, Singapore
Correspondence: David B Price
Observational and Pragmatic Research Institute Pte Ltd (OPRI), 60 Paya Lebar Road, Paya Lebar Square, Level 5, Unit 33 and 34, Singapore 409051, Singapore
Tel +65 68029724
Email [email protected]
Purpose: In primary care, initial diagnosis of community-acquired pneumonia (CAP) is made on clinical judgment without radiological confirmation or knowledge of the causative organism. Use of CRB65 score has been recommended for assessing the severity of CAP and thereby determining clinical management, but it is not known how frequently these scores are used in primary care.
Patients and methods: Primary care consultations in adults with a diagnostic code for CAP between 1 January 2009 and 31 December 2016 were extracted from the Optimum Patient Care Research Database, which at the time of data extraction had over 3.4 million patients in the UK. Episodes without antibiotic prescription on day of diagnosis were excluded, as were records describing past events. Patients admitted to hospital on day of diagnosis were excluded, but were included in exploratory analysis of CRB65 recording.
Results: In total, 4734 episodes of CAP in adults managed in primary care between 1 January 2009 and 31 December 2016 were included. A range of investigations/observations were recorded, including pulse rate (10.7%), chest examinations (9.1%) and blood tests (5.4%). CRB65 scores were recorded in 19 (0.4%) episodes of CAP, 17 of which were after the publication of the NICE guidelines in December 2014. CRB65 recording was no more frequent in 3819 episodes referred to hospital (12, 0.3%; p=0.63), but where recorded, CRB65 scores were higher (Median: 1.0 [interquartile range: 0.5–1.0] vs 2.0 [interquartile range: 1.0–2.0], p=0.04). The most commonly prescribed antibiotic was amoxicillin (40.3%), and 85.9% of episodes had a prescription length of seven days.
Conclusion: CRB65 scores are seldom recorded in UK primary care. Given that these scores are embedded in UK guidelines, further work is required to assess feasibility and barriers to use of CRB65 scores in primary care.
Keywords: lower-respiratory tract infection, antibiotics, antimicrobials, guidelines adherence, CRB65
Introduction
Community-acquired pneumonia (CAP) is a leading infectious cause of death in the UK.1 In the primary care setting, initial diagnosis is typically made on clinical judgment without radiological confirmation or knowledge of the causative organism.2 For patients presenting in primary care, the decision to treat in the community or refer for hospital admission requires an assessment of CAP severity. In severe CAP, delays in admission to the intensive care unit are associated with increased mortality.3,4
Use of severity scores may act as an adjunct to clinical decision-making, aiding the identification of patients at high risk of death.5,7 However, many of these scores include parameters that cannot readily be assessed in primary care, such as urea included in the CURB65 score.8 Consequently, the CRB65 score has been developed for use in primary care.
The CRB65 score assigns one point to each of: confusion, raised respiratory rate (30 breaths per minute or more), low blood pressure (diastolic 60 mmHg or less, or systolic less than 90 mmHg) and age 65 years or more, and the total score can be used to predict 30-day mortality. CAP patients’ 30-day mortality risk is then calculated as 0 (low risk – less than 1% mortality risk), 1–2 (intermediate risk – 1–10% mortality risk) and 3–4 (high risk – more than 10% mortality risk).8
In 2009, the CRB65 score was recommended for use in primary care by the British Thoracic Society (BTS) guidelines and quality standards on the management of CAP in adults.9 In December 2014, the CRB65 score was incorporated into National Institute for Health and Care Excellence (NICE) guidelines Pneumonia in Adults: Diagnosis and Management.10 The guidelines suggest CRB65 scores be used alongside clinical judgment in primary care, and that hospital-based care be considered for all patients with a CRB65 score of one or more, and particularly for those with a score of two or more. Furthermore, the guidelines recommend a 5-day course of a single antibiotic for patients with low-severity CAP, while a 7- or 10-day course of antibiotic therapy is recommended for moderate- to high-severity CAP. The use of CRB65 scores is also included in the most recent NICE quality standards for the management of pneumonia in adults,11 which states that adults diagnosed with CAP in primary care “should have a mortality risk assessment using the CRB65 score”. Finally, in January 2019, NICE released draft guidance on antimicrobial prescribing for CAP,12 in which antibiotic prescription is based on severity as determined by clinical judgement and CRB65 scores.
Despite studies on the accuracy of CRB65 scores in determining severity,6,13 and these scores being embedded in UK guidance,9,12 it is not known to what degree these scores are used in UK primary care. We set out to assess the use of CRB65 scores in patients diagnosed with CAP in UK primary care.
Materials And Methods
This retrospective observational database study aimed to investigate the management of CAP in primary care in the UK, focusing on the recording of CRB65 scores and prescription of antibiotics. The study was performed using electronic medical records obtained from the Optimum Patient Care Research Database (OPCRD: https://opcrd.co.uk/). The OPCRD is a quality-controlled, longitudinal, primary care, respiratory-focused database containing pseudonymised data from general practices in the UK. At the time of this study, it contained data of over 3.4 million patients and now contains data of 6.3 million patients from over 600 general practices. Because in the UK, people are required to register with a primary care physician in order to receive health care, UK primary care databases are widely considered to be essentially population-based.14
The study protocol was approved by the Anonymised Data and Protocol Transparency (ADEPT) committee (ADEPT0817) and registered with the European Network of Centres for Pharmacoepidemiology and Phamacovigilance (ENCePP, EUPAS28667).
Record Selection
Primary care consultations in adults with a diagnostic code for CAP (Appendix 1) between 1 January 2009 and 31 December 2016 and with a minimum of 28 days of continuous medical record prior to and after the diagnoses were extracted from the OPCRD. The study period covered both the publication of the BTS CAP Guidelines in 20099 and the publication of the NICE Quality Standard in December 2014.10 To maintain our focus on newly diagnosed cases of CAP managed in primary care, consultations were excluded if they had no recording of an antibiotic prescription on the day of diagnosis (on the assumption that they led to a hospital referral) or were summaries of past events. Consultations resulting in hospitalization were excluded from the main analysis as the timing of their hospitalization and data on their management was not available. However, this subset of patients was included in exploratory analysis of clinical details and CRB65 recording.
Consultations were grouped into episodes of CAP per patient. A new episode was defined as a consultation for CAP at least 180 days after any prior consultation for CAP for an individual patient. For each episode, an evaluation period consisting of an index date of the day of diagnosis, a baseline period of 28 days prior to diagnosis and outcome period of 28 days after diagnosis was considered.
Data Analysis
Data were analysed using R (version 3.4.0) and RStudio (version 1.0.143). The primary outcomes were CRB65 recording and class and length of antibiotic prescription. Demographic and clinical characteristics were summarised for both included and excluded CAP episodes. Statistical analysis utilised Chi-squared test for categorical variables, one-way ANOVA for continuous variables and Wilcox for differences in medians. Kendall’s correlation was used to assess trends over time. Multivariable logistic regression was used to assess determinants of CRB65 recording. Variables showing an association with CRB-65 recording with a p-value of less than 0.2 in single variable analysis were included in the original logistic regression model. Variables showing no significant association (p>0.05) were removed in a stepwise fashion.
Results
A total of 49,863 new episodes of CAP were recorded in adults between 1 January 2009 and 31 December 2016, of which 36,011 had the minimum required continuous medical records (Figure 1). Of these, 21,802 (60.5%) were excluded because no antibiotic prescription was given in primary care and 5656 (15.7%) because the primary consultation was a summary of a past event. A further 3819 episodes had a referral to secondary care on the index date and so were only included in the exploratory analysis. The final study population, managed in primary care, consisted of 4734 discrete episodes of CAP from 4595 patients. Most patients had only one episode in the study period (4467, 97.2%) and the majority of episodes of CAP consisted of one consultation (3434, 72.5%). Of the 1300 episodes with more than one consultation, the majority had their second consultation in the outcome period (1134, 87.2%). The median time to second consultation in these episodes was 7 days (interquartile range [IQR]: 3–11). Of those with consultations for CAP in the outcome period, the majority had one (686, 60.5%) or two (263, 23.2%).
 |
Figure 1 Flowchart of inclusion and exclusion criteria. |
The incidence of CAP managed in primary care (n=4734) over the study period was 21.7 (95% confidence interval [CI]: 21.1–22.3) episodes per 100,000 patient-years in the database. Incidence of CAP managed in primary care declined over the study period (p<0.001), and the absolute number of episodes had marked seasonality, with winter peaks in all years (Figure 2).
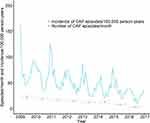 |
Figure 2 Trends in episodes of CAP in primary care from 2009 to 2016, n=4734. |
Patient Characteristics
The study population of adult patients diagnosed with CAP (n=4734) had a mean age of 61.6 (standard deviation [SD]: ±19.3), and 46.0% (n=2179) were male. The cumulative incidence of CAP per 100,000 over the study period was similar between genders (male: 100.8, 95% CI: 96.6–105.1; females: 105.3, 95% CI: 101.2–109.4, Figure 3).
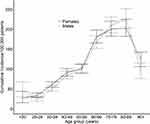 |
Figure 3 Cumulative incidence of episodes of CAP per 100,000 active patients in the OPCRD database, over the eight years of study. |
Obesity was recorded in 24.5% (n=1158) and overweight in 28.6% (n=1355), with missing BMI data in 14.0%. 19.1% (n=904) current smokers and 36.5% (n=1729) were ex-smokers. The most common comorbidities prior to CAP diagnosis were gastro-oesophageal reflux disease (30.1% of which 23.3% [1102/1427] had active disease in the baseline period), cardiovascular disease (26.7%, n=1263), eczema (26.6% of which 0.5% [23/1258] had active disease), rhinitis (23.0% of which 8.5% [401/1088] had active disease) and asthma (22.9%, n=1086; Table 1). A COPD diagnosis was recorded in 13.5% (n=639) of episodes.
 |
Table 1 Baseline Demographic And Clinical Information For The Study Population And Excluded Episodes Referred To Hospital |
Assessment Of CAP In Primary Care
On the index date, a suspected organism was recorded for 13.5% (n=637) episodes, and 57.4% (n=2719) had details on the location or type of pneumonia. Blood pressure (17.6%, n=832), pulse rate (10.7%, n=508) and chest examination (9.1%, n=432) were the most frequently recorded observations on index date. Oxygen saturation was recorded in 7.1% (n=337) of episodes, blood tests in 5.4% (n=257) of episodes and urine tests in 1.3% (n=62). Radiology requests were recorded in 4.8% (n=228) on the day of diagnosis and 7.5% (354) in the 14 days following diagnosis.
CRB65 Recording
CRB65 was not recorded in the evaluation period (28 days before and 28 days after the index date) in 4715 episodes of CAP. In 19 episodes (0.4%), CRB65 scores were recorded on index date, of which five episodes had a score of zero, 11 had a score of one and three had a score of two. Of these, 14 episodes also had CRB65 scores recorded in the baseline period (28 days before the index date) and one episode had a CRB65 score recorded in the outcome period (28 days after the index date).
In episodes where CRB65 scores were not recorded, 95 episodes had three components of CRB65 (confusion, respiratory rate, blood pressure and age) recorded individually, and one episode had all four components recorded. Further, two episodes for which CRB65 were recorded also had three or more components listed individually. The majority of episodes with three or more components recorded (79/98, 80.6%) had a calculated CRB65 score of less than two (range: 0–3). The least recorded components were presence/absence of confusion, recorded in 11 episodes (0.2%) and respiratory rate, recorded in 170 (3.6%) episodes.
The recording of both CRB65 and their components improved over time. The recording of CRB65 scores was significantly higher after the publication of the NICE guidelines in December 2014 (2015–2016: 17/740 [2.3%; 95% CI: 1.3–3.7%]) than beforehand (2009–2014: 2/3994 [0.1%; 95% CI: 0.001–0.2%]; p<0.001; Figure 4). The two episodes with CRB65 score recorded prior to 2015 occurred in January and December 2014. Similarly, recording of at least three components of CRB65 was significantly higher in 2015–2016 (32/740 [4.3%; 95% CI: 3.0–6.1%]) than in the years prior (66/3994 [1.7%; 95% CI: 1.3–2.1%], p<0.001, Figure 4).
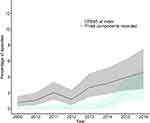 |
Figure 4 Percentage of episodes recording CRB65 or at least three components of CRB65 per year. Note: Shaded areas: 95% confidence intervals. |
In multivariable logistic regression, CRB65 scores or three or more components were more often recorded in episodes of CAP in older patients, those who had an LRTI consultation in the baseline period and those with eosinophilia (Tables 2 and 3).
 |  |  |
Table 2 Determinants Of Or Three Or More Components Of CRB65 Recording: Single Variable Analysis |
 |
Table 3 Results Of Logistic Regression Modelling Of Determinants Of CRB65 Or Three Or More Components Of CRB65 Recording |
Antibiotic Treatment
A consultation for lower respiratory tract infection (LRTI) was recorded in the baseline period in 11.2% of episodes, of which 79.4% (420/529) were prescribed antibiotics. On index date, 91.7% (n=4342) of episodes had a prescription for a single antibiotic and 8.3% (n=392) for multiple antibiotics. Amoxicillin was the most commonly prescribed single antibiotic (44.0%; 1908/4342), while amoxicillin plus clarithromycin was the most common combination where multiple antibiotics were prescribed (46.4%, 179/392, Table 4). While four of the five episodes with a CRB65 score of zero were prescribed antibiotics in line with the draft NICE guidelines,12 this was the case for only four of the 14 records with CRB65 scores of 1 or 2 (Table 5). Where the duration of antibiotic prescription on the day of CAP diagnosis was known, the mean duration was seven days (sd±2.6) and 76.5% (2599/3400) of episodes had a seven-day prescription.
 |
Table 4 Antibiotic Prescriptions On Day Of CAP Diagnosis By CRB65 Score At Index |
 |
Table 5 Antibiotic Prescribing In Line With Proposed NICE Guidelines |
Episodes where multiple antibiotics were prescribed were more likely to have a follow-on consultation in the outcome period for LRTI (38.3% [95% CI: 33.4–43.3%] vs 28.7% [95% CI: 27.3–30.0%], p<0.001) or CAP (32.1% [95% CI: 27.5–37.0%] vs 23.2% [95% CI: 22.0–24.5%], p<0.001) than those where single antibiotics were prescribed.
Exploratory Analysis Of Patients Managed In Primary Care And Those Referred To Secondary Care
Patient characteristics of the study population managed in primary care differed significantly to the 3819 patients referred to hospital on day of CAP diagnosis (Table 1). Those managed in primary care had a lower mean age, comprised a higher proportion of females and were more likely to be current or non-smokers than episodes referred to hospital, while those hospitalized were more likely to be ex-smokers (Table 1). Episodes managed in primary care also had a lower proportion of cardiovascular disease (26.7% [95% CI: 25.4–28.0%] vs 48.3% [95% CI: 46.7–49.9%]; p<0.001), pre-existing COPD (13.5% [95% CI: 12.5–14.5%] vs 21.1% [95% CI: 19.8–22.4]; p<0.001) and other chronic respiratory conditions (6.6% [95% CI: 5.9–7.3%] vs 14.3% [95% CI: 13.2–15.4%]; p<0.001) but a higher proportion pre-existing asthma (22.9% [95% CI: 21.7–24.2%] vs 19.0% [95% CI: 17.8–20.3%]; p<0.001) than in episodes referred to hospital. There was no significant difference in the proportion of episodes where CRB65 was recorded between those managed in primary care (19, 0.4% [95% CI: 0.24–0.63%]) and those resulting in a hospital referral (12, 0.3% [95% CI: 0.16–0.55%]; p=0.63), though the median score was greater in those referred to hospital (1.0 [IQR: 0.5–1.0] vs 2.0 [IQR: 1.0–2.0], p=0.04).
Discussion
This study demonstrates that, despite CRB65 scores being incorporated into BTS guidelines in 20099 and NICE guidelines in 2014,10 CRB65 scores are not well documented by primary care physicians for CAP patients managed in primary care. CRB65 scores were completed on the day of diagnosis in only 0.4% of episodes, in the 28-day baseline period prior to diagnosis for 0.3% of episodes and in the 28-day outcome period after diagnosis in one episode. No increase in CRB65 recording was observed following the introduction of the BTS guidelines in 2009, and despite improvements in CRB65 recording following the NICE guidelines in 2014, CRB65 recording remained low throughout the study period. The recording of the components of the CRB65 score was also low, particularly respiratory rate and confusion. The low level of confusion recorded may reflect a reluctance to record an absence of confusion, or the difficulties of determining mental status in a short consultation. While the CRB65 score has good predictive value,7,13 its utility may depend on the population. A score of 1 in an otherwise healthy 65-year old may not require consideration of hospitalization, while in the elderly population confusion may be hard to differentiate from other pre-existing conditions.15
The findings of our study are in line with a study of CRB65 use in admission decisions in a hospital in South Africa, where CRB65 was only being used in 1.6% of patients.16 This study concluded that, had CRB65 been used more frequently, fewer patients would have been hospitalized. Other studies have also shown that CAP severity scores are infrequently used in clinical practice.13
In our study, CRB65 was more likely to be recorded in patients who were diagnosed with an LRTI in the 28 days prior to CAP diagnosis, who were over 85 years, or had eosinophilia. It may be therefore that CRB65 scores are being used more frequently to stratify patients perceived to be at increased risk of mortality. In addition to CRB65, other indicators such as poor functional status,17 oxygenation18 and comorbidities19 are also predictive of severity. Therefore, while CRB65 score recording was low, primary care physicians are likely using a wide range of indicators to inform their clinical judgement, including social factors20 not captured in our study. In our study, clinicians recorded a variety of additional indicators on the day of diagnosis for patients managed in primary care: pulse rate was recorded in 10.7% of episodes, oxygen saturation was recorded in 7.1% and blood tests were performed or requested in 5.4%. Notably, performing a chest examination was poorly recorded in our study (9.1%) possibly as this was considered a routine investigation and physicians reported results (57.4%) of the investigation instead.
While there was little difference in the proportion of episodes with CRB65 recorded between episodes managed in primary care and those referred to hospital, episodes of CAP managed in primary care were less likely to have comorbidities and were younger and where recorded had lower CRB65 scores than episodes resulting in referral to hospitalisation. This suggests that despite the low level of CRB65 recording, pneumonia in patients with pre-existing risk factors for adverse outcomes in pneumonia is more likely to be hospitalized.
Currently, NICE recommends that a five-day course of amoxicillin is considered for treatment of low-severity CAP, while dual antibiotic therapy of amoxicillin and a macrolide and a 7–10-day duration should be considered for moderate severity.11 The newly published draft NICE guidelines for antimicrobial prescribing for CAP12 provide more detail, providing alternative therapy in the event of penicillin allergy, estimated to affect approximately 10% of the population,21 and embedding the CRB65 scores into the decision-making process. In our study, amoxicillin was prescribed on the day of diagnosis as single antibiotic in 40.3% of episodes and in combination with a macrolide in 4.4% of episodes. While only a small number of episodes had CRB65 scores recorded, the observed differences between the draft NICE guidelines12 and the prescribing patterns in this study suggest a change in practice may be required. The majority of episodes in our study consisted of one consultation, suggesting that follow-up after antibiotic prescription is uncommon.
A recent study has suggested that a substantial proportion of antibiotic prescriptions given for common infections in primary care are for longer duration than guidelines suggest.22 Despite the NICE guidelines recommending that a five-day course of amoxicillin for low-severity CAP, the majority of prescriptions in our study were for seven days, as is recommended for low-severity CAP in the 2009 BTS guidelines.9,23
The main limitation of this study is the observational nature. As an observational study based on medical records, this study is open to misclassification bias. A large proportion of identified CAP consultations (60.5%) did not have antibiotic prescriptions recorded on the day of diagnosis. Because prescriptions are generated automatically from the computer, antibiotic prescribing data are unlikely to be incomplete for such a large proportion of patients, although they may be missing for those treated at home or out of hours. Other potential reasons for the low rate of recorded antibiotic prescribing include misclassification of CAP or poor recording of hospital referral. It is the authors' belief that the latter is the most plausible, and therefore these cases were excluded from the analysis. Patients referred to secondary care may receive antibiotic therapy in secondary rather than primary care and therefore antibiotic prescriptions may not be recorded in primary care records. Antibiotic prescription was markedly less recorded in those with hospitalization recorded (95/3819; 2.5%) compared to those managed in primary care (4734/26,536; 17.8%). Furthermore, it is unknown whether the low recording of CRB65 scores and the components of CRB65 is due to physicians not using these scores in primary practice, or whether they are used but not routinely recorded.
Conclusion
While previous studies have shown that CRB65 scores are predictive of 30-day mortality, this is the first study in the UK to document the recording of CRB65 in primary care. We observed a low level of CRB65 recording in this study for patients managed in primary care and referred to secondary care. Further work is needed to assess feasibility of using CRB65 scores in primary care, GPs awareness of the inclusion of these scores in both the BTS and NICE guidelines and potential barriers to use of CRB65.
Acknowledgments
The authors would like to thank Anjan Nibber for her work on the original protocol and dataset for this study. This study was funded by the Respiratory Effectiveness Group, with data provided by Optimum Patient Care.
Disclosure
CCW is an employee and Director of Oxford PharmaGenesis Ltd and a shareholder and Director of Oxford PharmaGenesis Holdings Ltd. DR is a Consultant Strategic Medical Director of Optimum Patient Care. DBP has board membership with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Mylan, Mundipharma, Napp, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals; consultancy agreements with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mylan, Mundipharma, Napp, Novartis, Pfizer, Teva Pharmaceuticals, Theravance; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd) from AKL Research and Development Ltd, AstraZeneca, Boehringer Ingelheim, British Lung Foundation, Chiesi, Circassia, Mylan, Mundipharma, Napp, Novartis, Pfizer, Regeneron Pharmaceuticals, Respiratory Effectiveness Group, Sanofi Genzyme, Teva Pharmaceuticals, Theravance, UK National Health Service, Zentiva (Sanofi Generics); payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Mylan, Merck, Mundipharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals; payment for manuscript preparation from Mundipharma, Teva Pharmaceuticals; payment for the development of educational materials from Mundipharma, Novartis; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Circassia, Mundipharma, Napp, Novartis, Teva Pharmaceuticals; funding for patient enrolment or completion of research from Chiesi, Novartis, Teva Pharmaceuticals, Zentiva (Sanofi Generics); stock/stock options from AKL Research and Development Ltd which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 74% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); and is peer reviewer for grant committees of the Efficacy and Mechanism Evaluation programme, and Health Technology Assessment. The authors report no other conflicts of interest in this work.
References
1. Bender MT, Niederman MS. Improving outcomes in community-acquired pneumonia. Curr Opin Pulm Med. 2016;22(3):235–242. doi:10.1097/MCP.0000000000000257
2. Levy ML, Le Jeune I, Woodhead MA, Macfarlaned JT, Lim WS, Group BTSCAPiAG. Primary care summary of the British Thoracic Society Guidelines for the management of community acquired pneumonia in adults: 2009 update. Endorsed by the Royal College of General Practitioners and the Primary Care Respiratory Society UK. Prim Care Respir J. 2010;19(1):21–27. doi:10.4104/pcrj.2010.00014
3. Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137(3):552–557. doi:10.1378/chest.09-1547
4. Renaud B, Brun-Buisson C, Santin A, et al. Outcomes of early, late, and no admission to the intensive care unit for patients hospitalized with community-acquired pneumonia. Acad Emerg Med. 2012;19(3):294–303. doi:10.1111/j.1553-2712.2012.01301.x
5. Long B, Long D, Koyfman A. Emergency medicine evaluation of community-acquired pneumonia: history, examination, imaging and laboratory assessment, and risk scores. J Emerg Med. 2017;53(5):642–652. doi:10.1016/j.jemermed.2017.05.035
6. Akram AR, Chalmers JD, Hill AT. Predicting mortality with severity assessment tools in out-patients with community-acquired pneumonia. Qjm. 2011;104(10):871–879. doi:10.1093/qjmed/hcr088
7. Chalmers JD, Singanayagam A, Akram AR, et al. Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis. Thorax. 2010;65(10):878–883. doi:10.1136/thx.2009.133280
8. Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi:10.1136/thorax.58.5.377
9. Lim WS, Baudouin SV, George RC, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64 Suppl 3(Suppl 3):iii1–iii55. doi:10.1136/thx.2009.121434
10. NICE. Pneumonia in Adults: Diagnosis and Management; Clinical guideline [CG191]; 2014. Available from: https://www.nice.org.uk/guidance/qs11010. Accessed September 13, 2019.
11. NICE. Pneumonia in Adults: Quality standard [QS110]; 2016. Available from: https://www.nice.org.uk/guidance/cg191. Accessed September 13, 2019.
12. NICE. Draft Consultation: Pneumonia (community-acquired): Antimicrobial Prescribing; 2019. Available from: https://www.nice.org.uk/guidance/indevelopment/gid-ng10130/documents. Accessed September 13, 2019.
13. Chalmers JD, Rutherford J. Can we use severity assessment tools to increase outpatient management of community-acquired pneumonia? Eur J Intern Med. 2012;23(5):398–406. doi:10.1016/j.ejim.2011.10.002
14. Majeed A. Sources, uses, strengths and limitations of the data collected in primary care in England. Health Stat Q. 2004;21:5–14.
15. Ewig S, Torres A. Severity scores for CAP. ‘Much workload for the next bias’. Thorax. 2010;65(10):853–855. doi:10.1136/thx.2010.143297
16. Kabundji DM, Musekiwa A, Mukansi M, Feldman C. Determining need for hospitalisation: evaluation of the utility of the CRB-65 score in patients with community-acquired pneumonia presenting to an emergency department. S Afr Med J. 2014;104(11):769–772. doi:10.7196/samj.8150
17. Jeon K, Yoo H, Jeong BH, et al. Functional status and mortality prediction in community-acquired pneumonia. Respirology. 2017;22(7):1400–1406. doi:10.1111/resp.13072
18. Ochoa-Gondar O, Vila-Corcoles A, Rodriguez-Blanco T, et al. Validation of the CORB75 (confusion, oxygen saturation, respiratory rate, blood pressure, and age ≥75 years) as a simpler pneumonia severity rule. Infection. 2014;42(2):371–378. doi:10.1007/s15010-013-0565-1
19. Kolditz M, Ewig S, Schütte H, et al. Assessment of oxygenation and comorbidities improves outcome prediction in patients with community-acquired pneumonia with a low CRB-65 score. J Intern Med. 2015;278(2):193–202. doi:10.1111/joim.12349
20. Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282. doi:10.1007/s11606-012-2235-x
21. Macy E. The clinical evaluation of penicillin allergy: what is necessary, sufficient and safe given the materials currently available? Clin Exp Allergy. 2011;41(11):1498–1501. doi:10.1111/j.1365-2222.2011.03837.x
22. Pouwels KB, Hopkins S, Llewelyn MJ, Walker AS, McNulty CA, Robotham JV. Duration of antibiotic treatment for common infections in English primary care: cross sectional analysis and comparison with guidelines. Bmj. 2019;364:l440. doi:10.1136/bmj.l42
23. Lim WS, Smith DL, Wise MP, Welham SA, Society BT. British Thoracic Society community acquired pneumonia guideline and the NICE pneumonia guideline: how they fit together. Thorax. 2015;70(7):698–700. doi:10.1136/thoraxjnl-2015-206881
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
