Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Management and outcomes of hyperparathyroidism: a case series from a single institution over two decades
Authors Al-Thani H, El-Matbouly M, Al-Sulaiti M , Asim M, Majzoub A, Tabeb A , El-Menyar A
Received 27 December 2017
Accepted for publication 30 April 2018
Published 31 July 2018 Volume 2018:14 Pages 1337—1345
DOI https://doi.org/10.2147/TCRM.S160896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Hassan Al-Thani,1 Moamena El-Matbouly,1 Maryam Al-Sulaiti,1 Mohammad Asim,2 Ahmad Majzoub,1 Abdelhakem Tabeb,1 Ayman El-Menyar2,3
1Department of Surgery, Hamad General Hospital, Doha, Qatar; 2Clinical Research, Trauma & Vascular Surgery, Hamad General Hospital, Doha, Qatar; 3Clinical Medicine, Weill Cornell Medical College, Doha, Qatar
Background: Hyperparathyroidism is a frequent endocrine disorder with variable clinical manifestations and outcomes. We aimed to evaluate clinical presentations, management and outcomes of hyperparathyroidism.
Methods: A retrospective study was conducted to include all patients presented with hyperparathyroidism between 1995 and 2014 at a single tertiary hospital with an average follow-up period of 46 months. Data were reviewed for clinical presentations, diagnostic work-up, intraoperative findings, management, and outcomes.
Result: We identified 161 patients with hyperparathyroidism; 69% were females and the mean age was 49.4±15 years. Patients presented mainly with musculoskeletal (65.8%), renal (37.3%), gastrointestinal tract (53.8%) and neuropsychiatric (8.8%) manifestations. At presentation, mean serum calcium and parathyroid hormone levels were elevated while mean vitamin D level was lower. Sestamibi-99mTc (MIBI) scintigraphy was done for 134 patients (83.2%) and was positive in 94 (70%). Primary hyperparathyroidism (67.7%) was the most frequent diagnosis followed by secondary (29.8%) and tertiary hyperparathyroidism (2.5%). The frequent indication for surgery was hypercalcemia (67.3%), bone disease (35.6%) and renal calculi (28.9%). The main postoperative pathology was parathyroid adenoma (63.1%) followed by hyperplasia (37.3%). Fourteen (8.9%) and 18 (11.4%) patients had persistent and recurrent hyperparathyroidism, respectively. Autotransplantation of parathyroid tissue was done in 36 cases.
Conclusion: Primary hyperparathyroidism is the most frequent cause of the parathyroid disease. Parathyroidectomy is the effective surgical approach in symptomatic patients. Further studies are needed to establish the association between vitamin D levels, renal disorders and persistent or recurrent hyperparathyroidism.
Keywords: hyperparathyroidism, parathyroidectomy, renal disorders, Qatar
Introduction
Primary hyperparathyroidism is a frequent endocrine disorder manifested with elevated levels of parathyroid hormone (PTH) and serum calcium.1 It can be also sporadically diagnosed with disproportionately high or even normal PTH in combination with high or even normal calcium levels.2 The diagnostic assessment of patients with primary hyperparathyroidism is based on the clinical evaluation, laboratory, and radiological findings.3
As the clinical features of familial hypocalciuric hypercalcemia (FHH) may overlap significantly with those of primary hyperparathyroidism (PHPT), various diagnostic tools for differential diagnosis have been suggested. A combination of clinical suspicion, biochemical testing, and genetic analysis is required to differentiate PHPT from FHH and thus spare patients with FHH from nontherapeutic operative treatment. These tests include urinary excretion of calcium as well as calcium:creatinine clearance ratio.4
Several imaging modalities are in use for the preoperative localization of parathyroid lesion such as neck ultrasound, Tc-99m sestamibi (MIBI) imaging with single photon emission computed tomography, magnetic resonance imaging, 4-dimensional computed tomography scan (4-D CT), and positron emission tomography combined with CT scan.5
Surgical intervention is the preferred treatment for symptomatic primary hyperparathyroidism that includes neck exploration and minimally invasive parathyroidectomy (MIP).6 Therefore, recent advancements in perioperative MIBI scanning and rapid intraoperative PTH monitoring enable focused operation with limited neck exploration.6–8
It has been suggested that the geographic distribution and socioeconomic status might account for variability in hyperparathyroidism presentations.9 The aim of this study was to assess the clinical presentation, diagnosis, management and outcomes of hyperparathyroidism over two decades in a single institution.
Methods
A retrospective study was conducted to include all patients with biochemical confirmation of hyperparathyroidism that were presented to the surgical clinics at Hamad General Hospital (HGH) in Qatar between 1995 and 2014. HGH is the tertiary referral hospital that provides specialist and subspecialist healthcare services for patients in the state of Qatar. All patients with a diagnosis of hyperparathyroidism (primary, secondary, or tertiary) were included with clinical follow-up. Data were retrieved from charts and electronic medical records for all patients with hyperparathyroidism. Collected data included demographics, past medical history, comorbidities, body mass index (BMI), clinical characteristics (bone, gastrointestinal tract and neuropsychiatric diseases), diagnostic work-up based on laboratory examination and radiological findings, indications for surgery, intraoperative findings, operative approaches, histopathology complications and outcomes. Primary hyperparathyroidism is mainly caused by single active parathyroid adenoma (80%–85%), followed by parathyroid hyperplasia (10%–15%) and infrequently occurs due to parathyroid carcinoma (<1%).6,10 Secondary hyperparathyroidism is a severe progressive disorder with hyperplasia of more than one gland often observed in patients with early chronic kidney disease.11 Tertiary hyperparathyroidism occurs in patients with untreated secondary hyperparathyroidism that leads the overactive autonomous parathyroid function.12 Persistent hyperparathyroidism is defined as elevated calcium and PTH within 6 months of neck exploration for hyperparathyroidism, and recurrent hyperparathyroidism is defined as elevated calcium and PTH that occurs more than 6 to 12 months after a seemingly successful parathyroidectomy.13
The majority of the patients underwent preoperative scan with technetium MIBI scintigraphy, followed by ultrasound of the neck. Intraoperative or rapid parathyroid hormone (rPTH) assay was utilized from the end of 2001 in HGH. The diagnosis of primary hyperparathyroidism was made on the basis of elevated corrected serum calcium level and concurrent elevation or inappropriately normal serum intact PTH level.1
Ethical approval was obtained and a waiver of informed consent was granted from Research Ethics Committee at the Medical Research Center, Hamad Medical Corporation (HMC), Doha, Qatar (IRB#14197/14). There was no direct contact with patients and data were kept anonymously for patients’ privacy and confidentiality. The study was registered at http://www.researchregistry.com (researchregistry # 2459).
Statistical analysis
Data were presented as proportions, medians, or mean±SD, as appropriate. Correlations of parathyroid gland weight with the serum calcium, PTH, or vitamin D were analyzed using Pearson’s correlation coefficient. All data analyses were carried out using the SPSS version 18 (SPSS Inc, Chicago, IL, USA).
Results
A total of 161 patients were diagnosed with hyperparathyroidism across the study period; of them 111 (69%) were females (Table 1). The mean age at presentation was 49.4±15 years with an average BMI of 24.5±12.9 kg/m2 and 42.2% were Qataris. Most of the cases were reported between the year 2001 and 2007 (Figure 1). The frequently associated comorbidities included hypertension (55.3%), renal failure (31.8%), type II diabetes mellitus (27.5%), dyslipidemia (25.6%), and coronary artery disease (17.6%). None of patients was diagnosed with multiple Endocrine Neoplasia. Figure 2 shows the number of patients with hyperparathyroidism and renal failure (73 cases).
  | Table 1 Demographics and clinical assessment of patients with parathyroid disease (n = 161) |
  | Figure 1 Hyperparathyroidism cases per year in Hamad General Hospital, Qatar. |
  | Figure 2 Hyperparathyroidism in patients with renal disease. |
Clinical presentations of hyperparathyroidism
Most patients presented with various manifestations of musculoskeletal, renal, and gastrointestinal tract disease such as renal stones, peptic ulcer disease and generalized muscles weakness. At presentation, mean serum calcium (2.9±0.8 mmol/L), and median parathyroid hormone levels (289.5 [3−3,457] pg/mL) were elevated, whereas, the mean vitamin D level was low (13.6±8.5 ng/mL). Table 2 shows the clinical presentations, types, complications and mortality of hyperparathyroidism in females and males.
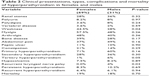  | Table 2 Clinical presentations, types, complications and mortality of hyperparathyroidism in females and males |
Preoperative localization by ultrasound was done in 95 patients, 37 patients (30.3%) had right parathyroid gland involvement, 25 (20.5%) had left, 23 (18.9%) had inferior, five (4.1%) had superior gland involvement and five patients (4.1%) had all glands involved.
Primary hyperparathyroidism (67.7%) was the most frequent diagnosis followed by secondary hyperparathyroidism (29.8%) and tertiary hyperparathyroidism (2.5%).
Table 3 demonstrates the indications of surgery and intraoperative findings.
  | Table 3 Indications for surgery, intraoperative findings, management and operative approaches |
A drop in PTH of 50% or more from the baseline PTH level 10 minutes postresection of the adenoma or hyperplastic glands indicates successful removal of the abnormal secreting parathyroid tissue.
MIP was successful with a combination of rPTH and 59 patients with significant drop of rPTH requiring no further intervention; in 37 patients, rPTH helped to direct the surgery for further exploration of the contralateral side of the neck, retroesophageal space, thymus gland, carotid sheaths and submandibular region for the ectopic glands resulting in a significant drop and confirming the completeness of parathyroid resection. Despite all of these maneuvers, in 14 patients, there was no significant drop in PTH and they continued to have a persistent hyperparathyroidism. Autotransplantation was performed for 36 (22.4%) patients.
Figure 3 shows patients who had total parathyroidectomy and auto-transplantation.
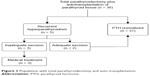  | Figure 3 Population with total parathyroidectomy and auto-transplantation. |
Vitamin D was given for 66 (42.9%) patients either pre- or postoperatively.
Patients on chronic renal replacement therapy, 27 of them were on calcium carbonate (54%) and 15 (30%) on Calcitrol. Sevelamer was given for six patients with a persistent hyperparathyroidism and in the year 2006, cinacalcet was given for eight patients with persistent hyperparathyroidism with good control of parathyroid hormone and calcium levels.
Table 4 shows surgical outcomes, pathology and postoperative complications.
  | Table 4 Postoperative pathology and complications |
Postoperatively, five patients had neck hematoma that was managed conservatively, two patients had wound infection, 12 (7.7%) had transient hypocalcemia and recurrent laryngeal nerve palsy was identified in two patients (1.2%). There was no mortality related to the surgical intervention and no 30-day mortality was reported. Overall mortality in the follow-up after 30 days was 18.6% (30 patients), nine patients in the group with primary hyperparathyroidism. Table 5 shows comorbidities differences in alive and deceased. Deceased patients were older and had more cardiovascular risk factors and renal failure.
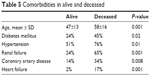  | Table 5 Comorbidities in alive and deceased |
Discussion
This was a unique study from a single nationally representative tertiary care institution to evaluate trends, presentations, management and outcomes in patients with hyperparathyroidism. In this study cohort, the mean age of patients was 49.4±15 years which is in agreement with earlier reports from Western countries.14 It has been noted that patients in the developing countries tend to be younger and symptomatic at their first presentation.15,16 We also observed female predominance which is in line with the current literature.17 Moreover, the prevalence of hyperparathyroidism was greater among elderly patients (>65 years) and was often observed in females of postmenopausal age (2.1%–3.4%).18 In our study, the clinical presentations, types, complications and mortality of hyperparathyroidism were comparable in females and males except for the more frequent presentation with weakness in females and occurrence of postoperative recurrent laryngeal nerve palsy in males.
Consistent with our findings, studies from South Africa and India showed that patients with primary hyperparathyroidism are mostly symptomatic on initial presentation.1,15 However, these findings are contrary to the western reports which showed predominance of asymptomatic disease, and hyperparathyroidism is often detected during routine biochemical screening.1,3
Most of our subjects had symptomatic presentation including symptoms of renal compromise and stones, musculoskeletal disorder, gastrointestinal complaints and psychiatric symptoms. Nephrolithiasis is the most frequent presentation in patients with renal disorders (20%–30%), whereas severe bone disease has been identified in less than 3% of cases; these findings are consistent with our observations.19 Hyperparathyroidism increases bone turnover and reduces bone mineral density with a subsequent loss of bone. Recent studies showed that surgery improves bone density in hyperparathyroidism.20 Osteoporosis and its radiologic diagnosis and follow-up were not documented in the present study.
Moreover, patients with hyperparathyroidism might also present with nonspecific symptoms like fatigue, irritability, memory loss and sleep disorders that are often improved after surgical management.21
A recent systematic review has identified vitamin D deficiency as a major health burden in Qatar with a weighted-average prevalence of low vitamin D status to be as high as 90.4%.22 The lower mean levels of vitamin D (13.6±8.5) in our study would further confirm these observations and also support the hypothesis that vitamin D deficiency might play a role in the pathogenesis of primary hyperparathyroidism. Furthermore, the occurrence of secondary and tertiary hyperparathyroidism could be speculated by the longstanding vitamin D deficiency in some cases of primary hyperparathyroidism that leads to disease progression.23 The current literature suggests that the frequent diagnosis of hyperparathyroidism involves single gland adenoma (75%–85%), followed by adenoma involving multiglands (1%–15% of cases) and parathyroid carcinoma in up to 1% of cases.6 Our findings also showed that primary hyperparathyroidism is the most frequent diagnosis followed by secondary and tertiary hyperparathyroidism.
Radiological imaging is used for preoperative localization of the hyperfunctioning lesions.19 MIBI scintigraphy has higher sensitivity and specificity for preoperative localization of affected parathyroid glands in patients with primary hyperparathyroidism and is often used to guide unilateral surgeries.24,25 MIBI scintigraphy can also be used for patients with secondary hyperparathyroidism with fair sensitivity but has lower specificity to detect all hyperactive glands with multiple hyperplasia.24 Therefore, it can be potentially used for preoperative localization of lesion that facilitates adoption of minimally invasive approach, thereby minimizing the need for wide neck surgical exploration involving all four-parathyroid glands.1 However, there are factors that affect the diagnostic accuracy of MIBI scans including regional perfusion and gland size and function particularly in multigland disease and when thyroid nodule presents.
Selective arteriography, venous sampling, and fine needle aspiration are invasive preoperative localization procedures that can be selectively opted in case of reoperation.5
It has been reported that the characteristic features of parathyroid gland such as size and color might influence the surgeon’s decisions to consider further exploration during surgical intervention.26 Some investigators have identified a correlation between the weight of parathyroid adenoma and the preoperative calcium and PTH levels, whereas others have failed to confirm such observation.27,28 In line with later observations, no significant correlation between adenoma weight, serum level of calcium, PTH and vitamin D has been identified in the present analysis.
Parathyroidectomy is the effective surgical management approach to treat primary hyperparathyroidism which is highly advocated for all symptomatic patients.5 Moreover, the current guidelines opt the operative approach for patients with asymptomatic primary hyperparathyroidism below 50 years, with an evidence of osteoporosis, vertebral fracture, nephrolithiasis, nephrocalcinosis, hypercalcemia, creatinine clearance (<60 cc/min) or failure to have adequate follow-up.29
The two surgical approaches include MIP and bilateral neck exploration planned from the outset.19 In our series, bilateral neck exploration was the standard treatment prior to 2001, following the introduction of intraoperative parathyroid hormone assay; MIP surgery was successfully utilized in 59 patients with primary hyperparathyroidism.
Postresection of the lesion, intraoperative cure should be affirmed by PTH measurement as an intraoperative adjunct as well as the biochemical profile.19 Intraoperative PTH measurement is considered as an important technological adjunct to assess the biochemical cure.30
A subset of patients with primary hyperparathyroidism (2%–5%) who undergo parathyroidectomy might require subsequent surgical intervention to treat the persistent or recurrent disease.31 Persistent primary hyperparathyroidism has been reported to occur in around 3.9% of cases which are diagnosed with hypercalcemia within 6 months of parathyroidectomy.32 It may be related to failure of identification and removal of all the hyperfunction glands.8 In the present study, persistent hyperparathyroidism attributed to renal failure, unrecognized hyperplasia, inadequate procedure or incomplete excision of involved glands or autotransplanted glands. Diagnosis of primary hyperparathyroidism due to single adenoma can be misleading especially in patients with a background of chronic renal disease or renal failure. Zavvos et al studied a subset of renal transplant patients who developed persistent hyperparathyroidism and found out that long-term treatment with cinacalcet was effective in controlling hypercalcemia and correcting hypophosphatemia.33 Such patients should be followed up for over 12–48 months and the levels of serum calcium and vitamin D as well as the presence of any symptoms of hyperparathyroidism should be monitored regularly and the possible addition of cinacalcet could be beneficial.
The prevalence of recurrent hyperparathyroidism has been reported in 2%–3% cases, which is speculated to occur due to regrowth of hyperactive lesions.31,34 In our study, we observed recurrent parathyroid disease in 11.4% of cases. The majority of these cases had unrecognized or regrowth of hyperplasia and some had renal failure which further altered the serum levels of calcium and vitamin D which influence the PTH levels and hence facilitate regrowth of hyperplasia in the remnant parathyroid glands. An earlier study suggested that recurrent disease is more evident in patients with elevated postoperative PTH and hypercalcemia (≥9.7 mg/dL).35 In a recent large study, Sadideen et al assessed 26 patients with renal disease who underwent total parathyroidectomy only without auto-transplantation. They found out that total parathyroidectomy without autotransplantation in renal transplant patients appeared to be protective against persistent and recurrent disease.36 To the best of our knowledge, this is the largest series with the longest follow-up available in the literature of this specific patient population. Based on this study, we can conclude that for our population with renal disease who underwent total parathyroidectomy, we could avoid persistent or recurrent hyperparathyroidism if we omitted transplanting any parts of the parathyroid gland for these patients.
Calcimimetic agents such as cinacalcet use for the treatment of primary hyperparathyroidism and secondary hyperparathyroidism effectively reduce PTH and calcium levels.37 In our study, a calcimimetic agent was used for 14 patients with a persistent hyperparathyroidism with good result. Moreover, vitamin D repletion could be a safe and effective approach to improve the bone mineral density which may help to prevent the progression of the disease severity. Also, appropriate hydration can minimize the risk of nephrolithiasis which is the predominant cause of renal disease in our cohort.
Overall mortality on the follow-up was 18.6% but significantly high for the patients on dialysis 21/47 (44.7%) and most of the mortality was related to cardiovascular disease and cancer.
Postoperative transient hypocalcemia could occur secondary to inhibition of the remaining parathyroid glands, devascularization or hungry bone syndrome.5 In the current study, the rate of postoperative hypocalcemia (7.7%) was lower than the reported rate in the literature ranging from 29.7%–59.4%.1 It is speculated that the observed lower rate was attributed to the unilateral neck exploration; however, transient hypocalcemia can still occur in patients with normal parathyroid glands secondary to chronic suppression.1
Limitations
The retrospective nature of the present study was one limitation. Moreover, we lacked information on the history, duration and treatment of vitamin D deficiency in patients with hyperparathyroidism which could be longstanding and might progress to secondary or tertiary hyperparathyroidism.
Conclusions
Primary hyperparathyroidism is the most frequent cause of parathyroid disease, with bone and renal disease being the main clinical presentation. Parathyroidectomy is the effective surgical management approach to treat parathyroid disease. High prevalence of vitamin D deficiency and kidney function derangement are major contributions to recurrent and persistent hyperparathyroidism. Further large studies are needed to establish the association of vitamin D levels and renal disorders with persistent and recurrent hyperparathyroidism.
Acknowledgments
We thank all the staff of surgery department for their cooperation. The Medical Research Center (IRB#14197/14) at Hamad Medical Corporation, Qatar, approved the study.
Author contributions
All authors (HA, ME, MA, MA, AM, AT and AE) contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Paruk IM, Esterhuizen TM, Maharaj S, Pirie FJ, Motala AA. Characteristics, management and outcome of primary hyperparathyroidism in South Africa: a single-centre experience. Postgrad Med J. 2013;89:626–631. | ||
Carneiro-Pla DM, Irvin GL 3rd, Chen H. Consequences of parathyroidectomy in patients with “mild” sporadic primary hyperparathyroidism. Surgery. 2007;142:795–799. | ||
Gasser RW. Clinical aspects of primary hyperparathyroidism: clinical manifestations, diagnosis, and therapy. Wien Med Wochenschr. 2013;163:397–402. | ||
Shinall MC Jr, Dahir K, Broome JT. Differentiating familial hypocalciuric hypercalcemia from primary hyperparathyroidism. Endocr Pract. 2013;19(4):697–702. | ||
Gawrychowski J, Bula G. Imaging diagnostics for primary hyperparathyroidism. Endokrynol Pol. 2013;64:404–408. | ||
Madkhali T, Alhefdhi A, Chen H, Elfenbein D. Primary hyperparathyroidism. Ulus Cerrahi Derg. 2016;32:58–66. | ||
Thielmann A, Kerr P. Validation of selective use of intraoperative PTH monitoring in parathyroidectomy. J Otolaryngol Head Neck Surg. 2017;46:10. | ||
Schneider DF, Mazeh H, Sippel RS, Chen H. Is minimally invasive parathyroidectomy associated with greater recurrence compared to bilateral exploration? Analysis of more than 1,000 cases. Surgery. 2012;152:1008–1015. | ||
Kirdak T, Canturk NZ, Korun N, Ocakoglu G; Parathyroid Study Group. Characteristics of patients operated for primary hyperparathyroidism at university hospitals in Türkiye: differences among Türkiye’s geographical regions. Ann Surg Treat Res. 2016;91(1):8–16. | ||
DeLellis RA, Lloyd RV, Heitz PU, Eng C, editors. Pathology and Genetics of the Tumours of Endocrine Organs, WHO Classification of Tumours. Lyon: IARC Press; 2004. | ||
Wetmore JB, Quarles LD. Calcimimetics or vitamin D analogs for suppressing parathyroidhormonein end-stage renal disease: time for a paradigm shift? Nat Clin Pract Nephrol. 2009;5:24–33. | ||
Kebebew E, Duh QY, Clark OH. Tertiary hyperparathyroidism: histologic patterns of disease and results of parathyroidectomy. Arch Surg. 2004;139:974–977. | ||
Smith GS, Prinz RA. Chapter 9. Persistent and recurrent hyperparathyroidism. In: Endocrine Surgery. New York: McGraw-Hill Manual. 2010. | ||
Misgar RA, Dar PM, Masoodi SR, et al. Clinical and laboratory profile of primary hyperparathyroidism in Kashmir Valley: a single-center experience. Indian J Endocrinol Metab. 2016;20:696–701. | ||
Shah VN, Bhadada S, Bhansali A, Behera A, Mittal BR. Changes in clinical & biochemical presentations of primary hyperparathyroidism in India over a period of 20 years. Indian J Med Res. 2014;139:694–699. | ||
Gopinath P, Mihai R. Hyperparathyroidism. Surgery. 2011;29:451–458. | ||
Gopal RA, Acharya SV, Bandgar T, Menon PS, Dalvi AN, Shah NS. Clinical profile of primary hyperparathyroidism from western India: a single center experience. J Postgrad Med. 2010;56:79–84. | ||
Lundgren E, Hagström EG, Lundin J, et al. Primary hyperparathyroidism revisited in menopausal women with serum calcium in the upper normal range at population-based screening 8 years ago. World J Surg. 2002;26:931–936. | ||
Callender GG, Udelsman R. Surgery for primary hyperparathyroidism. Cancer. 2014;120:3602–3616. | ||
Rajeev P, Movseysan A, Baharani A. Changes in bone turnover markers in primary hyperparathyroidism and response to surgery. Ann R Coll Surg Engl. 2017;99(7):559–562. | ||
Reiher AE, Mazeh H, Schaefer S, Gould J, Chen H, Sippel RS. Symptoms of gastroesophageal reflux disease improve after parathyroidectomy. Surgery. 2012;152:1232–1237. | ||
Badawi A, Arora P, Sadoun E, Al-Thani A-A, Thani MHA. Prevalence of Vitamin D insufficiency in Qatar: a systematic review. J Public Health Res. 2012;1(3):229–235. | ||
Priya G, Jyotsna VP, Gupta N, et al. Clinical and laboratory profile of primary hyperparathyroidism in India. Postgrad Med J. 2008;84:34–39. | ||
Saengsuda Y. The accuracy of 99m Tc-MIBI scintigraphy for preoperative parathyroid localization in primary and secondary-tertiary hyperparathyroidism. J Med Assoc Thai. 2012;95:S81–S91. | ||
Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol. 2007;188:1706–1715. | ||
Moretz WH 3rd, Watts TL, Virgin FW Jr, Chin E, Gourin CG, Terris DJ. Correlation of intraoperative parathyroid hormone levels with parathyroid gland size. Laryngoscope. 2007;117:1957–1960. | ||
Nasiri S, Sorush A, Mehrkhani F, Hedayat A. Could we predict adenoma weight and postoperative serum calcium level with preoperative serum biochemical markers in patients with primary hyperparathyroidism? Internet J Surg. 2007;16:1. | ||
Randhawa PS, Mace AD, Nouraei SA, Stearns MP. Primary hyperparathyroidism: do perioperative biochemical variables correlate with parathyroid adenoma weight or volume? Clin Otolaryngol. 2007;32:179–184. | ||
Bilezikian JP, Khan AA, Potts JT Jr; Third International Workshop on the Management of Asymptomatic Primary Hyperthyroidism. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab. 2009;94(2):335–339. | ||
Neves MC, Ohe MN, Rosano M, et al. A 10-year experience in intraoperative parathyroid hormone measurements for primary hyperparathyroidism: a prospective study of 91 previous unexplored patients. J Osteoporos. 2012;2012:914214. | ||
Schneider DF, Mazeh H, Chen H, Sippel RS. Predictors of recurrence in primary hyperparathyroidism: an analysis of 1386 cases. Ann Surg. 2014;259:563–568. | ||
O’Connell RL, Afors K, Thomas MH. Re-explorative parathyroid surgery for persistent and recurrent primary hyperparathyroidism. WJOES. 2011;3:107–111. | ||
Zavvos V, Fyssa L, Papasotiriou M, et al. Long-term use of cinacalcet in kidney transplant recipients with hypercalcemic secondary hyperparathyroidism: a single-center prospective study. Exp Clin Transplant. 2018;16:287–293. | ||
Kelly KJ, Chen H, Sippel RS. Primary hyperparathyroidism. Cancer Treat Res. 2010;153:87–103. | ||
Ning L, Sippel R, Schaefer S, Chen H. What is the clinical significance of an elevated parathyroid hormone level after curative surgery for primary hyperparathyroidism? Ann Surg. 2009;249:469–472. | ||
Sadideen HM, Taylor JD, Goldsmith DJ. Total parathyroidectomy without autotransplantation after renaltransplantation for tertiary hyperparathyroidism: long-term follow-up. Int Urol Nephrol. 2012;44(1):275–281. | ||
Khan A, Bilezikian J, Bone H, et al. Cinacalcet normalizes serum calcium in a double-blind randomized, placebo-controlled study in patients with primary hyperparathyroidism with contraindications to surgery. Eur J Endocrinol. 2015;172(5):527–535. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
