Back to Journals » Clinical Ophthalmology » Volume 18
Magnitude of Active Trachoma Among Host and Refugee Children in Gambella Regional State, Ethiopia
Received 28 November 2023
Accepted for publication 6 March 2024
Published 11 March 2024 Volume 2024:18 Pages 777—789
DOI https://doi.org/10.2147/OPTH.S448870
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Lissanu Senbete,1 Girmay Adhena2
1College of Medical and Health Science, Mettu University, Mettu, Ethiopia; 2Department of Reproductive Health, International Medical Corps, Gambella, Ethiopia
Correspondence: Girmay Adhena, Email [email protected]
Background: Trachoma is a serious public health concern and cause of blindness globally. Despite its vulnerability to all ages, children are more vulnerable to its adverse outcomes and devastating complications. This study assessed the magnitude of trachoma among children in host and refugee communities in Gambella, Ethiopia.
Methods: A community-based comparative survey was done among 743 participants. Multistage sampling technique was used to select participants. Selected children were examined for trachoma using a 2.5x binocular loupe and graded using the World Health Organization (WHO) simplified grading system. A standardized, structured, and pretested tool was used to collect the data. Data were collected through interviews and observation. Bivariable and multivariable logistic regression analyses were done to identify the associated factors. Variable with a p-value < 0.05 was considered statistically significant.
Results: The magnitude of active trachoma was 119 (16.5%; 95% CI: 13.5, 21.4) with 36 (14.5%; 95% CI: 11.9, 18.8) and 83 (17.5%; 95% CI: 14.3, 22.7) from refugees and host communities, respectively. Poor knowledge of caregiver about trachoma [AOR = 3.55, 95% CI: (1.48, 8.85)], presence of human feces near the house [AOR = 4.57, 95% CI: (1.84, 11.34)], presence of garbage near the house [AOR = 4.07, 95% CI: (1.34, 12.36)], and the presence of flies on the face of the child [AOR = 3.42, 95% CI: (1.32, 8.84)] were significantly associated factors with active trachoma.
Conclusion: Overall, one-sixth of children had experienced active trachoma. The magnitude of trachoma was higher in the host community compared to the refugees. Proper waste disposal and personal hygiene measures are important measures that should be addressed to tackle the problem.
Keywords: active trachoma, children, host communities, refugees, Gambella, Ethiopia
Background
Trachoma is a chronic keratoconjunctivitis disease caused by the bacterium Chlamydia trachomatis serovars A, B, Ba, or C and it is among the leading cause of blindness in the globe.1 It is a major public health problem in more than forty-two countries and resulted for 1.9 million people visually impaired.1,2 It is endemic in the world’s poorest populations, in which access to basic services such as water, sanitation and health care is inadequate.1,2
Globally, about 154.5 million people lived in the areas of trachoma follicular (TF) prevalence in children aged 1–9 years was ≥5%. Out of this number, 87% were in WHO’s African Region, with 49% in Ethiopia.3 About 6 million people in the world are blind due to its devastating complications. It is endemic in many countries from Africa, the Middle East, Central and South America, Asia, and Australia.4 Africa remains the most affected continent with the highest prevalence of trachoma and people live in at-risk areas.4,5 South Sudan and Ethiopia are among the countries where the prevalence of trachoma is high.1 In Ethiopia, more than 76 million people live with active trachoma across the country. More than 9 million children aged 1–9 years live with active trachoma.6 In South Sudan, half the population is at risk, with the prevalence of active trachoma as high as 80% in some communities with very low diagnosis and treatment due to they are living in hard to reach areas.7,8 The prevalence of active trachoma ranges from 60% to 90% among preschool children.1
The World Health Organization (WHO) in collaboration with other national health services and nongovernmental organizations (NGOs) started the implementation of SAFE (Surgery for Trichiasis, Antibiotics for infectious trachoma, facial cleanliness to reduce transmission and Environmental improvement) program to eliminate trachoma as a public health problem.3 The initiative to eliminate trachoma was also signed by Ethiopia in 2002 and developed 20 years strategic plan.9
Factors that increases the transmission of chlamydia trachomatis are poor sanitation, inadequate access to water for face-washing, poor environmental hygiene, and overcrowding.10,11 The lack of appropriate latrines, lack of waste disposal facilities, absence of separate room for animals, a high population of flies, and common usage of fomites are also among the factors that favor the transmission of trachoma.12–14
Even though there is a good progress to eliminate trachoma as a public health problem increasing displacement of high populations from trachoma endemic areas could impact the global progress.3 South Sudan and Ethiopia are among endemic countries where millions of people particularly children attacked by trachoma.6–8 Assessing the magnitude of active trachoma in the host and refugee communities helps the government and non-governmental organizations to evaluate the problem and to local decision-makers for the intervention of trachoma in the study area. In addition to that, there is also limited evidence in the host and refugee communities in the study area. This study aimed to assess the magnitude of active trachoma among the host and refugee children aged 1–9 years old in Itang district, Gambella, Ethiopia.
Method
Study Area and Period
The study was conducted in the Itang district (both host and Refugee communities). Itang is one of the districts which is found in Gambella regional state, Ethiopia. It is located around 820 kilometers away from Adis Ababa, the capital city of Ethiopia. The district has 23 kebeles (2 urban and 21 rural), the smallest administrative unit of Ethiopia. There are 7 refugee Camps and one entry point serving the refugees of South Sudanese in Gambella. An estimated population of 338,673 were settled in all Gambella refugee camps. Among those three refugee camps were serving the South Sudan refugee communities in the Itang district. The estimated total population size of the Itang district was 75, 000 from the host communities and 195,000 were from the refugees of South Sudan (Itang district office and UNHCR annual report of 2020). The study was conducted from November 1-December 5, 2021.
Study Design
A comparative community-based cross-sectional study was used.
Population
All children aged 1–9 years old in the Itang district (both host and refugees) were the source population. Children aged 1–9 years old from the selected kebeles of the host community and selected refugee camps consisted of the study population. Children who were unable to undergo physical examination due to severe medical condition such as mental illness, unconsciousness and depression were excluded.
Sample Size Determination and Sampling Procedure
The sample size was calculated by using a single population proportion formula, assuming a 95% confidence interval, 80% power, and 1 to 2 ratios. By taking the prevalence of trachoma (p) 14.6% in the host community and 15.7% in the refugee communities from the previous studies done in Gambella for the host community and study done in South Sudanese refugees in the White Nile state in Sudan for the refugees, respectively.15,16 By using the EP-INFO-7 and entering the values by considering a design effect of 1.5 and 10% non-response rate, the calculated sample size was 248 for the refugee and 495 for the host community. The final sample size used for this study was 743.
For the sampling procedure, all kebeles of the host community and three refugee camps were taken. The district has 2 urban kebeles and 21 rural kebeles holding 5212 households (HH) in the host community and three refugee camps were sheltering 18,376 households. Eight kebeles (1 from urban and 7 from rural) were selected by lottery method for the host community. Out of the three camps, two were selected by using the lottery method. The total number of households in each selected kebele (8 kebeles) and the 2 refugee camps were considered in the host and refugees, respectively. The number of households was 2675 and 10,624 in the host community (8 selected kebeles) and refugees (2 selected camps), respectively. The proportional allocation to sample size was done for each kebele and refugee camp. Households from each kebele were selected by using a systematic random sampling technique with a k-value of five for the host community and forty-two for refugees. The first household was selected by simple random sampling for both host and refugee and continued the next household based on their k-value. The next household was taken for the household that has no 1–9 years old child. For the household that had more than one child aged 1–9, a lottery method was used to select the child.
Data Collection Tool
A structured, pretested and adapted from different literatures questionnaire was used to collect the data.9,10,17–19 The questionnaire was first prepared in English and translated into Amharic, Nuer, and Agnuwa by three language experts for each language, and again translate back to English to check the consistency. Pretest was done for 25 (5%) samples to the host community in Elia, which was among the not selected kebele. For the refugee community, a pretest was done for 12 (5%) samples in the Nuegyiel refugee camp which was not among the selected study sites. Appropriate modifications were done after discussing with the supervisor and data collectors before starting the actual data collection. The questionnaire consisted of socio-economic, background, household status, environment, facility, knowledge, water source, and lifestyle, and other related characteristics of the caregiver and the child. The data were collected through face-to-face interviews and observation. Three clinical nurses and three midwives (degree holders) were recruited as data collectors. Two public health officer professionals have supervised the data collection process. Three trained clinical nurses by wearing 2.5x loupes assessed each eye for signs of active trachoma using the WHO simplified grading scheme.20 Close follow-up was done daily throughout the data collection period.
Operational Definition
Active trachoma: This was measured as the presence TF or TI in at least one eye of the child.17–21
Trachomatous inflammation follicular (TF): This was defined as the presence of five or more follicles in the upper tarsal conjunctiva and follicles must be at least 0.5mm in diameter.17–19
Itang district: Includes both the host and refugee communities.
Trachomatous inflammation intense (TI): Inflammatory thickening of tarsal conjunctiva that obscures more than half of the normal deep tarsal vessels.17–19
Clean face: A child with no eye discharge/nasal discharge, and no flies on the face at the time of interview and observation.22
Knowledge: This was measured by twelve knowledge-related items of trachoma. Those caregivers who responded with the correct answer were given a score of one point and zero otherwise. Those who scored mean (6.7) and above were categorized as they have good knowledge, and those who scored less than the mean (below 6.7) were categorized as they have poor knowledge about trachoma.17
Data Quality Control
Pretest was done on 5% of the study population in the non-selected kebeles (host community), and refugee camp and appropriate modifications were done. Two days training was given for data collectors and supervisors on the method of data collection, ethical issues, COVID-19 prevention, and confidentiality. The questionnaire was translated into local languages (Amharic, Angua, and Nuer) for each language by three language experts (persons). The collected data were cross-checked for its completeness and consistency. Close follow-up was done from the beginning of data collection to the end.
Data Processing and Analysis
The data were coded, cleaned, and checked for its completeness. The completed data were entered into EP-INFO version 7.2 and then exported to SPPS version 25 for analysis. Frequencies, percentages, narrative, and summary statistics were used for descriptions of the findings. Binary regression was done to assess the association of factors with the outcome variables. Variables with a p-value ≤0.25 were candidates for multivariate analysis. Hosmer and Lemeshow test was checked to assess the model fit by using standard error. Variables significant in the binary regression were entered into the final model (multivariable analysis). The odds ratio of 95% CI was used to show the strength and direction of the association. Variable with p-value <0.05 in the final model was considered statistically significant.
Ethical Considerations
Ethical clearance was secured from Mettu University Institutional Health Research Ethics Review Committee. A formal letter was written to Gambella regional health bureau and the Itang district health office for the host communities. The official letter was also written to the Agency for Refugee and Returnee Affairs (ARRA) zonal office. Informed written consent was obtained from the parents/guardians and confidentiality of information was maintained. Tetracycline ophthalmic ointment was given for children with active trachoma. All children suffering from trachoma were given a referral slip to the health center. All the COVID 19 prevention and control measures were applied throughout the data collection period.
Result
Background Characteristics of Participants/Caregivers
Among a total of 743 expected participants, 722 have participated which makes a response rate of 97.2%. Out of this number, 248 were refugees and 474 were from the host community. The majority, 509 (70.5%) of mothers/caregivers did not attend formal education. Out of this number, 320 (44.3%), and 189 (26.2%) were from host and refugees’ communities, respectively. More than half, 396 (54.8%) children were females. About 572 (79.2%) mothers/caregivers were Protestants in their religion. Out of this, 353 (74.5%) and 219 (88.3%) were from host and refuges respectively. Three hundred ninety mothers/caregivers (82.3%) from the host community and 207 (83.5%) from refuges were married in their marital status. Regarding the employment status of the caregivers, 379 (80%) from the host community and 238 (96%) from the refugees were housewives (Table 1).
 |
Table 1 Background Characteristics of the Child and Caregivers Among Host and Refugees’ Communities of Itang District, Gambella, Ethiopia, (N=722) |
Environmental, Housing Conditions and Other Related Characteristics
More than half, 425 (58.9%) children did not wash their face using soap. Of them, 260 (54.9%) were from the host, and 165 (66.5%) were from refugees. Near to half, 344 (47.6%) of children had eye discharge with 204 (43%) from the host and 140 (56.5%) were from refugees. About 568 (78.7%) had no solid waste pit. Six hundred sixty (88.6%) had no liquid waste disposal pit with 408 (86.1%) from host and 232 (93.5%) in the refugees. Six hundred twenty (85.9%) were used for food cooking inside the house with 384 (81%) were from the host and 236 (95.2%) were from the refugees. Near one-fourth, 176 (24.4%) had an animal in their house with 158 (33.3%) from the host and 18 (7.3%) from the refugees. More than one-fifth, 156 (21.6%) had human feces near their house with 97 (20.5%) were from the host community and 59 (23.8%) were from refugees. More than half, 469 (65%) have garbage near their house. Of this number, 325 (68.6%) were from the host community and 144 (58.1%) were from the refugees. More than half, 424 (58.7%) had liquid waste around their house. Of these, 272 (57.4%) were from the host, and 152 (61.3%) were from refugees. Regarding knowledge of the caregiver about trachoma, 305 (42.7%) had poor knowledge. Of this, 149 (31.4%) and 159 (64.1%) were from host and refugees, respectively. More than half, 448 (62%) reported they drink water from the pipe with 201 (42.4%) were from the host and 247 (99.6%) were from refugees (Table 2).
 |
Table 2 Environmental, Housing, Knowledge of Caregiver, and Other Related Characteristics Among Host and Refugee Communities of Itang District, Gambella, Ethiopia, (N=722) |
Magnitude of Active Trachoma Among 1–9 Years Old Children in Itang District
Among the total of 722 participants, 119 (16.5%; 95% CI: 13.5–21.4) had active trachoma. Out of this number, 36 (14.5%; 95% CI: 11.9–18.8) were from the refugees, and 83 (17.5%; 95% CI: 14.3–22.7) were from the host communities (Figure 1). The magnitude of TF was 12.3%, TI was 4.2%, and TI and TF were found to be 5%.
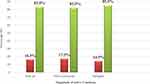 |
Figure 1 Magnitude of active trachoma among 1–9 years old host and refugee children in Itang district, Gambella, Ethiopia, (N=722). Legends in the figure (color). Red= Yes. Green= No. |
Factors Associated with Active Trachoma Among the Host Community
In the bivariable logistic regression, eye discharge, animal in the household, condition of child’s face, mother’s education, number of flies on the face, human feces around the main house, garbage near the main house, latrine availability, latrine utilization, liquid waste near the main house, solid waste disposal pit; and mother’s/caregiver’s knowledge about trachoma were associated factors. However, in the final model (multivariable logistic regression) liquid waste near a house, having an animal in their house, and knowledge of mother/caregiver about trachoma were significantly associated factors (Table 3).
 |
Table 3 Factors Associated with Active Trachoma Among Host Community Children in Itang District, Gambella, Ethiopia (N= 474) |
Factors Associated with Active Trachoma Among Refugees Children
In the bivariable logistic regression, condition of the child’s face, having animal in the house, eye discharge, number of flies on the child’s face, human feces near the main house, garbage near the main house, latrine availability, livestock; liquid waste near the main house, use of media, use soap, room number, time to fetch water; and a number of the sleeping area (room) were significantly associated factors. But, in the multivariable logistic regression analysis flies on the face, livestock in the house, feces near the house, number of rooms, time is taken to fetch water, and using media were significantly associated factors (Table 4).
 |
Table 4 Factors Associated with Active Trachoma Among Refugee Children in Itang District, Gambella, Ethiopia (N=248) |
Factors Associated with Active Trachoma Among Children in Itang District (Both Refugees and Host Community)
In the bivariable logistic regression, sex, use of soap, having animal living conditions, eye discharge, latrine availability, human faces near the house, livestock, garbage near the house liquid waste in the house, use of media (radio), number of flies in the face of the child, solid waste disposal pit, liquid waste disposal pit, number of rooms and knowledge of mother/caregiver about trachoma were significantly associated factors. However, in the final model (multivariable logistic regression) human faces near in the house, garbage near in the house, number of flies in the face of the child, and knowledge of the mother/caregiver were significantly associated factors (Table 5).
 |
Table 5 Factors Independently Associated with Active Trachoma Among Children in Refugee and Host Communities of Itang District, Gambella, Ethiopia (N=722) |
Discussion
Among the total 722 participants, 119 (16.5%, 95% CI: (13.5, 21.4)) have experienced active trachoma with 36 (14.5%; 95% CI: (11.9, 18.8)) from the refugees, and 83 (17.5%; 95% CI: (14.3, 22.7)) from the host communities. The magnitude of TF was 12.3%, TI was 4.2%, and TI and TF were found to be 5%. The presence of human feces near the house, presence of flies in the child’s face, poor knowledge of caregivers about trachoma, presence of garbage near the house were significantly associated factors with active trachoma.
The magnitude of active trachoma in this study (16.5%) is in line with the findings from Burundi (19.5%), Dembia (18%), Gambella (14.6%), South Sudan (15.7%), Lemo district (15.2%), Afar (17.1%), Arba Minch (17.8%), and Dera (15.6%).11,12,15,16,22–25 However, the finding is lower than the studies done in Systemic review in Ethiopia (26.9%), Kaffa (26.9%), Baso-Liben (24.1%), Degua-Temben (21.5%), Medawelabu (22%), Gonji Kolella (23.1%), Areka (37.9%), Waghimira (52.4%), Zalla (36.7%), and Kiritimati Island (28%).10,14,17–19,26–30 The discrepancy might be due to the duration of the study, sample size, and sampling techniques. The variation could also be due to the difference in the study subjects. For example, the study done in Medawelabu was focused on rural residents whereas this study included both rural and urban children. In which those who are living in rural may have a hygienic problem and low access to information about the disease compared to those who are living in urban this might be the reason for the discrepancy.
The finding is higher than from studies in Pakistan (1.9%), Brazil (8.2%), Darfur-Sudan (8%), Mozambique (10%), Senegal (5%), Uganda (3.9%), Yonan (0.02%), Shanghai (5.2%), Metema (11.8%), and Northwest Amhara (8.3%).13,31–39 The reasons might be due to the difference in the study area where the socioeconomic status of the countries might be varied. It could also be due to the variation in study subjects. For instance, studies done in Brazil, Yonan, and Amhara region included primary school children and children whose ages from 6 to 9 years old, but this study includes children aged 1–9 years old. Those children whose age 6 and above years old may keep their hygiene as compared to those below 6 years old. The study in Northwest Amhara was also included in the mass drug administration graduated districts which may decrease the magnitude. The difference may also be due to environmental and housing conditions and SAFE implementing strategy in the study areas.
The magnitude of active trachoma was higher in the host compared with refugee communities in this study. A possible reason for the variation might be due to poor environmental sanitation and poor housing conditions. Latrine utilization and availability might be the reason to increase the magnitude in the host community. Non-governmental organizations’ efforts that were working strongly in sanitation and hygienic practice might be the reason to decrease the magnitude of trachoma in the refugees compared to the host community.
This study tried to assess factors associated with active trachoma among children. Those children who have human feces near their houses were 4.6 times more likely to have active trachoma than those who did not have human feces near their house. This is consistent with the study done in Lemo, Dera, Gonji Kolella, Darfur (Sudan), and Mozambique.22,25,26,32,33 This could be due to the poor hygienic practice in their environment that leads them to be vulnerable to trachoma. If there are feces near to the house it allows the growth of bacteria and leads to the people being risky for not only trachoma but also for other communicable diseases.
Children whose mothers/caregivers have poor knowledge about trachoma were 3.6 times more likely to have trachoma as compared to those whose mothers/caregivers have good knowledge about trachoma. This is consistent with the findings from the Baso Liben, Degua Temben, Areka, and Zalla.17,18,27,29 The possible explanation might be those caregivers who have good knowledge may know about the mode of transmission and the other characteristics of the disease and caring for their children including a hygienic practice that helps them for early prevention and treatment than those who have poor knowledge about trachoma.
The presence of garbage near the home was significantly associated with trachoma in this study. Those who have garbage near their house were four times more likely to have active trachoma as compared to those who have no garbage near their house. This is supported by the findings from Dembia, Kaffa, Lemmo, Arba Minch, Gonji Kolla, and Areka.12,14,22,24,26,27 The possible reason for this might be due to the presence of garbage near the house may increase an opportunity for the growth of many microorganisms in that garbage and children may also touché and play in that environment which increases contamination. As is obviously known, trachoma is a disease due to sanitation and hygienic problems. So, this might increase the likelihood of being infected by this disease.
The presence of more flies in the face of the child was significantly associated with active trachoma. A child with more flies seen in his/her face was 4.5 times higher to have active trachoma as compared to those who have no flies on his/her face. This is consistent with studies done in Kaffa, Baso Liben, Zalla, and Northwest Amhara.14,17,29,39 The possible explanation for this might be due to the role of eye seeking fly in trachoma transmission and the hygienic practice of the child. This is because flies are attracted to children who have unclean faces. Eye-seeking flies from children’s faces are more likely to disseminate Chlamydia trachomatis-infected ocular secretions among themselves, and unclean face creates eye discharge that attracts flies.
Limitation
It is a cross-sectional study which only provides a snapshot of data in time. Self-report of complex hygiene behaviors may have been subject to social desirability and recall bias. However, the study benefited from direct observation of proxies for behaviors and other environmental variables, which strengthens the methodology.
Conclusions
One-six of the children have active trachoma with 14.5% from the refugees, and 17.5% from the host communities. The presence of human feces near the house, presence of flies in the child’s face, poor knowledge of the mother/caregiver about trachoma, presence of garbage near the house were significantly associated factors. Strengthening measures on enhancing community awareness on the environmental and personal hygienic practices are an important measure to tackle the problem. Longitudinal studies are also recommended for further investigation.
Abbreviations
ARRA, Agency for Refugee and Returnee Affairs; HH, Household; NGO, Nongovernmental organization; TF, Trachomatous inflammation follicular; TI, Trachomatous inflammation intense; TT, Trachoma Trichiasis; UNHCR, United Nations higher commission for refugees; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted following the declaration of Helsinki on human subjects. After the purpose, benefit and risk were briefed, informed consent was obtained from the caregivers of study participants. Ethical clearance was secured by Mettu University Institutional Health Research Ethics Review Committee (IHRERC) and official permission was obtained from the Gambella regional health bureau and Itang district health office and ARRA municipal. All WHO COVID-19 prevention and control measures were followed throughout the study period.
Acknowledgments
The authors would like to thank data collectors and supervisors for their cooperation during the data collection period.
Author Contributions
Both authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there is no conflicts of interest in this work.
References
1. World Health Organization. Validation of elimination of trachoma as a public health problem, Fact Sheet Geneva: World Health Organization, 2016.
2. World Health Organization. Eliminating trachoma, sustained progress with hundreds of millions of people no longer at risk of infection; 2019.
3. World Health Organization. WHO Alliance for the Global Elimination of Trachoma by 2020: progress report on elimination of trachoma; 2020.
4. Light for the World. Trachoma and human resource development: vision and development ophthalmology in the development cooperation issue. 2017.
5. Ramadhani AM, Derrick T, Macleod D, Holland MJ, B MJ. Eliminating trachoma: accelerating towards 2020. Geneva: WHO Alliance for the Global Elimination of Trachoma by; 2020.
6. Federal Ministry of Health. National Neglected Tropical Diseases Master Plan 2015/16 – 2019/20.
7. Edwards T, Smith J, Sturrock HJW, et al. Prevalence of trachoma in Unity State, South Sudan: results from a Large-Scale Population-Based Survey and Potential Implications for Further Surveys. PLoS Negl Trop Dis. 2012;6(4):e1585. doi:10.1371/journal.pntd.0001585
8. Thornton J. Hopes for trachoma control in South Sudan. Lancet. 2021;397(10273):461. doi:10.1016/S0140-6736(21)00297-X
9. Berhane Y, Worku A, Bejiga A, et al. National survey on blindness, low vision and trachoma in Ethiopia: methods and study clusters profile. Ethiop J Health Dev. 2007;21(3):185–203.
10. Gebrie A, Alebel A, Zegeye A, et al. Prevalence and associated factors of active trachoma among children in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):1–12. doi:10.1186/s12879-019-4686-8
11. Ndisabiye D, Gahungu A, Kayugi D, et al. Association of environmental risk factors and trachoma in Gashoho Health District, Burundi. Afr Health Sci. 2020;20(1):182–189. doi:10.4314/ahs.v20i1.23
12. Ferede AT, Dadi AF, Tariku A, et al. Prevalence and determinants of active trachoma among preschool-aged children in Dembia District, Northwest Ethiopia. Infect Dis Poverty. 2017;6(1). doi:10.1186/s40249-017-0345-8
13. Ochani RK, Shaikh A, Batra S. Active trachoma among children of District Dera Ghazi Khan, Punjab, Pakistan: a cross-sectional study. J Pak Med Assoc. 2019;69(3):456.
14. Tsegay T, Mengistu Y, Nigussie T. Application of ordinal logistic regression analysis in determining risk factors of active trachoma among rural children of aged 1–9 years old in Kaffa Zone, Southwest Ethiopia. ARC J Public Health Community Med. 2019;4(1):20–28.
15. Abashawl A, Macleod C, Riang J. Prevalence of trachoma in gambella region, Ethiopia: results of Three Population-Based Prevalence Surveys Conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2016;23(sup1):77–83. doi:10.1080/09286586.2016.1247875
16. Sanders AM, Abdalla Z, Elshafie BE, et al. Prevalence of trachoma within refugee camps serving South Sudanese refugees in White Nile State, Sudan: results from population-based surveys. PLoS Negl Trop Dis. 2019;13(6):e0007491. doi:10.1371/journal.pntd.0007491
17. Ketema K, Tiruneh M, Woldeyohannes D, et al. Active trachoma and associated risk factors among children in Baso Liben District of East Gojjam, Ethiopia. BMC Public Health. 2012;12(1):1105. doi:10.1186/1471-2458-12-1105
18. Reda G, Yemane D, Gebreyesus A. Prevalence and associated factors of active trachoma among 1–9 years old children in Deguatemben, Tigray, Ethiopia, 2018: community cross-sectional study. BMC Ophthalmol. 2020;20(1):1–9. doi:10.1186/s12886-020-01394-0
19. Kassim K, Kassim J, Aman R, et al. Prevalence of active trachoma and associated risk factors among children of the pastoralist population in Madda Walabu rural district, Southeast Ethiopia: a community-based cross-sectional study. BMC Infect Dis. 2019;19(1):353. doi:10.1186/s12879-019-3992-5
20. National Institute of Health. WHO simplified the trachoma grading system. Community Eye Health. 2004;17(52):68.
21. Solomon AW, Zondervan M, Kuper H, Buchan JC, Mabey D, Foster A. Trachoma Control: A Guide for Programme Managers. Geneva: World Health Organization; 2006.
22. Woldekidan E, Daka D, Legesse D, et al. Prevalence of active trachoma and associated factors among children aged 1 to 9 years in rural communities of Lemo district, southern Ethiopia: community-based cross-sectional study. BMC Infect Dis. 2019;19(1):886. doi:10.1186/s12879-019-4495-0
23. Negash K, Macleod C, Adamu Y, et al. Prevalence of trachoma in the Afar Region of Ethiopia: results of seven population-based surveys from the Global Trachoma Mapping Project. Ophthalmic Epidemiol. 2018;25(sup1):3–10. doi:10.1080/09286586.2017.1362008
24. Glagn Abdilwohab M, Hailemariam Abebo Z; Mustefa Glagn Abdilwohab, Zeleke Hailemariam Abebo. High Prevalence of Clinically Active Trachoma and Its Associated Risk Factors Among Preschool-Aged Children in Arba Minch Health and Demographic Surveillance Site, Southern Ethiopia. Clin Ophthalmol. 2020;14:3709–3718. doi:10.2147/OPTH.S282567
25. Alemayehu M, Koye DN, Tariku A, et al. Prevalence of active trachoma and its associated factors among rural and urban children in Dera woreda, Northwest Ethiopia: a comparative cross-sectional study. Biomed Res Int. 2015;8:570898.
26. Nigusie A, Berhe R, Gedefaw M. Prevalence and associated factors of active trachoma among children aged 1–9 years in rural communities of Gonji Kolella district, West Gojjam Zone, North West Ethiopia. BMC Res Notes. 2015;8(1):1–9. doi:10.1186/s13104-015-1529-6
27. Alambo MM, Lake EA, Bitew Workie S, Wassie AY. Prevalence of Active Trachoma and Associated Factors in Areka Town, South Ethiopia, 2018. Interdiscip Perspect Infect Dis. 2020;10:8635191.
28. Anteneh ZA, Getu WY. Prevalence of active trachoma and associated risk factors among children in Gazegibela district of Wagehemra Zone, Amhara region, Ethiopia: community-based cross-sectional study. Trop Dis Travel Med Vaccines. 2016;2(1):5. doi:10.1186/s40794-016-0022-0
29. Mengistu K, Shegaze M, Woldemichael K, et al. Prevalence and factors associated with trachoma among children aged 1–9 years in Zala district, Gamo Gofa zone, Southern Ethiopia. Clin Ophthalmol. 2016;10:1663–1670. doi:10.2147/OPTH.S107619
30. Cama A, Mu¨ller A, Taoaba R, et al. Prevalence of signs of trachoma, ocular Chlamydia trachomatis infection, and antibodies to Pgp3 in residents of Kiritimati Island, Kiribati. PLoS Negl Trop Dis. 2017;11(9):e0005863. doi:10.1371/journal.pntd.0005863
31. Lopes MD, Luna EJ, Medina NH, et al. Prevalence of trachoma in Brazilian schoolchildren. Rev Saúde Pública. 2013;47(3):1–8.
32. Macleod CK, Binnawi KH, Elshafie BE. Unimproved water sources and open defecation are associated with active trachoma in children in internally displaced persons camps in the Darfur States of Sudan. Trans R Soc Trop Med Hyg. 2019;113(10):599–609. doi:10.1093/trstmh/trz042
33. Abdala M, Singano CC, Willis R, et al. The epidemiology of trachoma in Mozambique: results of 96 population-Based Prevalence Surveys. Ophth Epidemiol. 2018;S1:201–210.
34. Sarr B, Sissoko M, Fall M. Prevalence of Trachoma in Senegal: results of base line surveys in 17 districs. Ophth Epidemiol. 2018;25(S1):41–52. doi:10.1080/09286586.2017.1418897
35. Baayenda G, Mugume F, Turyaguma P, et al. Completing Baseline Mapping of Trachoma in Uganda: results of 14 Population-Based Prevalence Surveys Conducted in 2014 and 2018. Ophth Epidemiol. 2018;S1:162–170.
36. Wu M, Hu ZL, He D, Xu WR, Li Y. Trachoma in Yunnan province of southwestern China: findings from trachoma rapid assessment. BMC Ophthalmol. 2018;18(1):97. doi:10.1186/s12886-018-0759-5
37. Xue W, Lu L, Zhu J, et al. A cross-sectional population-Based Survey of Trachoma among Migrant School-Aged Children in Shanghai, China. Biomed Res. Int. 2016;8:8692685.
38. Ayelgn K, Guadu T, Getachew A. Low prevalence of active trachoma and associated factors among children aged 1– 9 years in rural communities of Metema District, Northwest Ethiopia: a community-based cross-sectional study. J Paediatr. 2021;47:114.
39. Melkie G, Azage M, Gedamu G, Peters RP. Prevalence and associated factors of active trachoma among children aged 1–9 years old in mass drug administration graduated and nongraduated districts in Northwest Amhara region, Ethiopia: a comparative cross-sectional study. PLoS One. 2020;15(12):e0243863. doi:10.1371/journal.pone.0243863
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
