Back to Journals » Integrated Blood Pressure Control » Volume 13
Magnitude and Associated Factors of Depression Among Hypertensive Patients Attending Treatment Follow Up in Chronic OPD at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia
Authors Gebre BB, Deribe B , Abeto M
Received 25 November 2019
Accepted for publication 11 March 2020
Published 23 March 2020 Volume 2020:13 Pages 31—39
DOI https://doi.org/10.2147/IBPC.S240015
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Bereket Beyene Gebre,1 Bedilu Deribe,1 Mintesnot Abeto2
1School of Nursing, College of Medicine and Health Science, Hawassa University, Hawassa, Ethiopia; 2College of Health Science, Hawassa University, Hawassa, Ethiopia
Correspondence: Bereket Beyene Gebre
Email [email protected]
Background: Hypertension and depression are among the most common public health issues affecting the population around the world. Like patients with other chronic medical conditions, hypertensive patients experience many intense emotions which increase their risk for the development of depression. Globally, depression is the leading cause of disability and 382 million people suffer worldwide.
Objective: The aim of this study was to assess the magnitude and factors associated with depression among hypertensive patients attending treatment follow up in the chronic OPD at Hawassa University Comprehensive Specialized Hospital (HUCSH) from March to May, 2019.
Methods: An institutional-based cross-sectional study was conducted with 310 hypertensive patients attending treatment follow up at the chronic Out-Patient Department of HUCSH at Hawassa from March to May, 2019. A validated patient health questionnaire (PHQ− 9) was used to assess depression. The data were entered using EPI-data version 3.1 and analyzed in SPSS version 22. Binary logistic regression was used to determine the association of independent variables with dependent variables.
Results: The magnitude of depression among hypertension (HPN) patients was found to be 73 (24.7%). The independent predictors were sex 2.6 (1.16, 5.83), age 11.2 (2.98, 42), educational status, social support 2.55 (1.09, 5.94), family history of depression 7.12 (1.48, 34.26), hypertension 7.57 (2.67, 21.44), and medication adherence 11.6 (4.23, 31.78).
Conclusion: The magnitude of depression among HPN patients was high. So, continuous health information dissemination at a different level regarding factors affecting them should be given. Strengthening a referral linkage with a psychiatric unit for psycho-behavioral therapy will bring good clinical outcome. Besides, controlling hypertension was crucial to bring good clinical outcome.
Keywords: depression, magnitude, associate factor, patient health questionnaire, PHQ-9
Introduction
The World Health Organization International Classification for Diseases and Related Disorders (ICD-10) describes the criteria for a depressive episode, where at least 4 items, such as unhappiness/sense of empty/depressed mood, exhaustion or energy loss, loss of interest in activities, lack of emotional reactions, sleep disturbance, motor retardation, loss of appetite, weight loss, and loss of libido are present for a duration of two weeks.1 Hypertension is elevated blood pressure of systolic, diastolic or both readings.2 Depression affects 350 million people around the world with a lifetime risk of 7%.
Depression is likely to cause a 5.7% increase in the global burden of disease by 2020 and is to become the leading cause of disability worldwide by the year 2030. Approximately one-quarter of the adults were diagnosed with hypertension, and the proportion will reach about one-third by 2025.3 Similarly, hypertension is one of the leading causes of global mortality and disability. In 2010, it had been estimated that 31.1% of the global population (1.39 billion) was hypertensive.4 Patients with depression and/or anxiety represent a particularly vulnerable population as they are at higher risk of developing hypertension. In addition, patients with co-morbid hypertension and mental health disorders are a higher-risk population for cardiovascular disease-related mortality.5 Depression and hypertension combined have a far more detrimental effect on health than individually and are reported to decrease the quality of life and cause an increased risk of myocardial infarction and stroke. Studies also suggest that the impact of co-morbid depression on patients with hypertension may have a major bearing upon physical functioning, quality of life, and healthcare utilization.6 It is well known that both hypertension and depression emerge from a complex interaction of social, biological, and behavioral factors.7 This study adds some behavioral and disease-related variables that have not yet been addressed. So, the aim is to fill the gap on the magnitude of depression among hypertensive patients and their associated factors in the study area.
Objective
General Objective
To assess the magnitude and associated factors of depression among hypertensive patients attending treatment follow up in the chronic Outpatient Department unit at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia, in 2019.
Specific Objective
To determine the magnitude of depression among hypertensive patients attending treatment follow up in the chronic Outpatient Department unit at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia, in 2019.
To identify associated factors of depression among hypertensive patients attending treatment follow up in the chronic Outpatient Department unit at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia, in 2019.
Methods
Study Design
An institutional-based cross-sectional study was conducted.
Study Area and Period
Hawassa University Comprehensive Specialized Hospital (HUCSH) is one of the teaching hospitals in Southern Ethiopia located in Hawassa town. This hospital serves more than 19 million people. The study was conducted from March 20 to May 20, 2019.
Population Source Population
The source population included all hypertensive patients attending treatment follow up in the chronic Outpatient Department unit at HUCSH during the data collection period.
The Study Population
The study population included sampled hypertensive patients attending treatment follow up in the chronic Outpatient Department unit at HUCSH during the data collection period.
Study Unit
The study unit included individual hypertensive patients who participated in the study.
Inclusion and Exclusion Criteria
Inclusion Criteria
All sampled hypertensive patients whose age was 18 and above who can give informed consent were included.
Exclusion Criteria
Sampled hypertensive patients who were mentally ill and seriously ill during the data collection period.
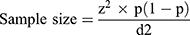
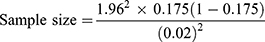
Sample Size Determination
The sample size was determined using a single population proportion formula. The p value from a previous study shows that the prevalence of depression in Northwest Ethiopia is 17.5%.8 The margin of error (d) is 0.02 since the pvalue is 17.5% to increase the sample size. The study population (N) is about 332. So,
ni=1386. Since the study population is <10,000 we used the population correction formula

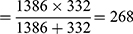
Adding 10% non-respondent rates = sample size × 10%
Non-respondent=268 × 0.1=27
So, the total sample size = 268 + 27 = 295
Sampling Technique
In Hawassa University Comprehensive Specialized Hospital, 332 patients were registered in the HPN registration book and the sampling frame has been made from the list of patients who had been appointed for follow up during the study period. The 295 patients were selected consequently since patients visiting the health facility for follow up were random in nature. So, an exit interview was done to collect data from patients while they visit the chronic outpatient clinic for follow up.
Variables
Dependent Variable
Depression.
Independent Variable
Socio-demographics: age, sex, educational status, marital status, monthly income, occupation, family history of psychiatric illness, social support.
Behavioral factors: alcohol intake, physical exercise, smoking, dietary intake, chewing chat.
Disease and medication-related factors: co-morbidity, medication adherence, HPN control, duration of illness, complication.
Operational Definition
No depression: Patient Health Questionnaire 9 score was 0–4.
Depression: Patient Health Questionnaire 9 score was 5–27.
Adherent: Those sampled individuals who took at least 4 and above consecutive days out of 7 days, which is greater than or equal to 90% adherence to drugs.20
Non-adherent: Those sampled individuals who took less than 4 consecutive days out of 7 days, which is less than 90% adherence to drugs.20
Data Collection and Analysis
The initial English version of the questionnaire was translated into Amharic. Then it was back-translated into English independently by language experts to maintain the equivalence of the test questionnaire in Amharic. The questionnaires have 4 parts. Socio-demographic information, WHO guideline to assess the adherence measuring scale, and behavioral factors and disease and medication-related factors were gathered from patients' recorded data and own word. To make the assessment tool valid, a group of experts approved the tool used to assess the individual patient.
Quality Control
To assure the quality of the study finding, training for 4 data collectors and 2 supervisors had been given. A pre-test on 5% on “Adare General Hospital” was carried out. In addition to this, checking, editing, clearing the data, and monitoring have been done by supervisors.
Data Processing and Analyzing
After checking the collected data visually for completeness, the responses were cleaned, edited, coded, and entered into the computer using Epic-data 3.1 version. The data were then exported to SPSS version 20.0. The data were checked for missing values before analysis. The descriptive analysis including frequency and cross tabs was used to assess the frequency of variables with independent variables. Binary logistic regression was carried out to assess the association of the dependent variable with independent variables and to determine predictors of poor adherence using odds ratios with 95% confidence interval. Finally, a forward stepwise logistic regression model with all independent variables having pvalue <0.05 was fitted and the adjusted odds ratio was calculated to identify independent predictors of adherence to medication among HPN patients.
Plan for Dissemination
It was disseminated to Hawassa University CBE office of the College of Medicine and Health Science and to the School of Nursing. It was also disseminated to the Hawassa Comprehensive Specialized Hospital.
Ethical Consideration
The study was conducted after approval of the ethical review committee of Hawassa University College of Medicine and Health Science. Permission to conduct the study was obtained from authorities at HUCSH. Written informed consent was obtained from each study participant by assuring privacy and confidentiality throughout the data collection period in the Hospital. An individual who was unwilling to participate from the beginning or at any part of the interview was allowed to withdraw. There was no risk or hazardous procedures putting the participants at harm.
Results
Socio-Demographic Characteristics
A total of 295 adult hypertensive patients were included in the study with a response rate of 100%. Among them, 189 (64.1%) were males (see Table 1).
 |
Table 1 Socio-Demographic Characteristics and Factors Associated with Depression Among Respondents of Hypertensive Patients in HUCSH, Hawassa, Southern Ethiopia, 2019 (n=295) |
Magnitude of Depression Among Hypertension
According to this study, the magnitude of depression among HPN patients was found to be 73 (24.7%).
Socio-Demographic Factors Associated with Depression
From the socio-demographic variables affecting depression among hypertensive patients, sex, age, marital status, residence, educational status, occupation, social support, and family history of depression were found to be associated in the binary logistic regression (BLR) (see Table 1).
Behavioral Characteristics and Factors Associated with Depression
From the total of 295 hypertensive patients, 261 (88.5%) did not smoke cigarettes/tobacco and 275 (93.2%) did not do regular physical activity. From the behavioral factors that affect depression among hypertensive patients, drinking alcohol and smoking cigarettes/tobacco were found to be associated in binary logistic regression (see Table 2).
 |
Table 2 Behavioral Characteristics and Factors Associated with Depression for Hypertensive Patients in HUCSH, Hawassa, Southern Ethiopia, 2019 (n=295) |
Disease and Medication-Related Characteristics and Factors Associated with Depression
From the respondents, 212 (71.6%) were found to have adhered to medication and their hypertension was also controlled. In our study from disease and medication-related characteristics and associated factors, those respondents having uncontrolled hypertension, not adhered to medication, and those who stay with the disease longer than 20 years were found to be associated significantly in binary logistic regression (see Table 3).
 |
Table 3 Disease and Medication-Related Characteristics and Factors Associated with Depression Among Hypertensive Patients in HUCSH, Hawassa, Southern Ethiopia, 2019 (n=295) |
Independent Factors of Depression
From 18 variables entered into BLR, 13 variables with p<0.05 were entered into forward logistic regression. Then, 8 variables were found to be independently associated. These were sex, age, marital status, educational status, social support, family history of depression, hypertension status, and medication adherence (see Table 4).
 |
Table 4 Independent Predictors Associated with Depression Among Hypertensive Patients in HUCSH, Hawassa, Southern Ethiopia, 2019 (n=295) |
Discussion
In this study, the prevalence of depression was found to be 24.19%. The finding was in line with the cross-sectional study done in Ebinet, Northwest Ethiopia (17.5%),9 Nigeria (26.7%),10 and Saudi Arabia (20.7%).11 In our study, females were 2 times more likely to be depressed than males. This is low when compared to that of studies done in Saudi Arabia12 and Nepal13 in which females were 4 times more likely to develop depression. This might be due to sociocultural variation of the respondents.
This study also indicated that increasing age is a predictor of depression among hypertensive patients. This study is also supported by 3 different studies done in Nepal.14–16 This is an implication that the physiologic change in an individual patient with increased age makes them depressed.
Concerning marital status, our study indicated that those who had widowed/divorced were found to be much more likely depressed than when compared to married ones. Our study result also confirmed that those who did not have social support had been found to be more depressed compared to those who responded that they had social support. This study result is higher than a study done in public hospitals of Eastern Ethiopia.17 The difference could be that the study participants involved in “Harar” hospitals were those admitted patients in a ward.
Regarding educational status, this study reveals that those illiterate and able to read and write were more likely found to be depressed than those having an educational level above primary school. This study result was much higher than the study done in China.18 This is due to difference in economic level and difference to use a cutoff point to diagnose depression.
Besides, this study also showed that those who had family history of depression, not adhered respondents, and those having uncontrolled hypertension were found to be 7, 7 and 11 times more likely depressed than those who had depressed respectively. This was higher than the study done in India in which those having family history of depression were AOR (95% CI) 3.562 (1.972–6.585), not adhered to medication were AOR (95% CI) 3.396 (1.809–6.375), and those having uncontrolled hypertension were AOR (95% CI) 4.334 (2.377–7.904)19 and this finding is low. This might be due to the socio-demographic characteristics of the respondents. So, provision of continuous health information dissemination at a different level and controlling those patients with hypertension were crucial to bring good clinical outcome. Additionally, psycho-behavioral therapy should be strengthened in patients having familial history of depression.
Limitation
Recall bias may exist as the respondents responded to the last two weeks' situation while depressed using PHQ-9.
Conclusion
The magnitude of depression among HPN patients was found to be high. The independent predictors were sex, age, marital status, educational status, social support, family history of depression, medication adherence, and hypertension.
Recommendation
So, continuous health information dissemination at a different level regarding factors affecting them and controlling those patients with hypertension was crucial to bring good clinical outcome. Besides, strengthening a referral linkage with the psychiatric unit for psycho-behavioral therapy will bring good clinical outcome.
Abbreviation
CBE, Community-based education; HPN, Hypertension; HUCSH, Hawassa University Comprehensive Specialized Hospital; PHQ-9, Patient Health Questionnaire with 9 items; WHO, World Health Organization.
Data Sharing Statement
The data supporting the findings were available in public repositories.
Ethics and Consent Statement
The study was conducted after approval of the ethical review committee of Hawassa University College of Medicine and Health Science. Permission to conduct the study was obtained from authorities at HUCSH. Written informed consent was obtained from each study participant by assuring privacy and confidentiality throughout the data collection period in the Hospital. An individual who was unwilling to participate from the beginning or at any part of the interview was allowed to withdraw. There was no risk or hazardous procedures putting the participants at harm.
Acknowledgments
First of all, I would like to acknowledge Hawassa University College of Medicine and Health Science Community-based education office (CBE) for provision of ethical clearance. I would also like to acknowledge Hawassa University Comprehensive Specialized Hospital for providing permission for the study to be conducted in the chronic outpatient clinic.
Author Contributions
The authors contributed in conception and design, acquisition of data or analysis and interpretation of data. They also take part in drafting the article or revising and approval of the manuscript before it has been published with accountability of the work done in the manuscript.
Disclosure
The authors report no funding and no conflicts of interest in this work.
References
1. Hussien G, Tesfaye M, Hiko D, Fekadu H. Assessment of prevalence and risk factors of depression among adults in Gilgel Gibe Field Research Center, South West Ethiopia. J Depress Anxiety. 2017;6(01):260. doi:10.4172/2167-1044.1000260
2. NICE. Hypertension: Clinical Management of Primary Hypertension in Adults. London: National Institute for Health and Care Excellence; 2011. Available from: http://www.nice.org.uk/guidance/cg127/chapter/key-priorities-for-implementation.
3. Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of depression in patients with hypertension: a systematic review and meta- analysis. Medicine (Baltimore). 2015;94:e1317. doi:10.1097/MD.0000000000001317
4. Kumar CS, Kulkarni VG. Prevalence of depression inpatients attending general medicine outpatient department for hypertension December 08, 2018.
5. Mahmood S, Hassan SZ, Tabraze M, et al. Prevalence and predictors of depression amongst hypertensive individuals in Karachi, Pakistan. Cureus. 2017;9:e1397.
6. Saboya PM, Zimmermann PR, Bodanese LC. Association between anxiety or depressive symptoms and arterial hypertension and their impact on the quality of life. Int J Psychiatry Med. 2012;40(3):307–320. doi:10.2190/PM.40.3.f
7. WHO Depression. Depression: A Global Public Health Concern. Geneva: World Health Organisation; 2012. doi:10.1002/da.22048.
8. WHO A. Global Brief on Hypertension. Geneva: World Health Organisation; 2013. doi: 10.1016/S0140-6736(13)60772-2.
9. Legas Molla G, Mulat Sebhat H, Nasir Hussen Z, Belete Mekonen A, Fekadu Mersha W, Mekonen Yimer T. Depression among Ethiopian adults: cross-sectional study. Psychiatry J. 2016;Article ID 1468120.
10. Igwe MN, Uwakwe R, Ahanotu CA, Onyeama GM, Bakare MO, Ndukuba AC. Factors associated with depression and suicide among patients with diabetes mellitus and essential hypertension in a Nigerian teaching hospital,2013.cross-sectional study. Afr Health Sci. 2013;13(1):68–77. doi:10.4314/ahs.v13i1.10
11. Al-Dabal BK, Koura MR, Al-Sowielem LS. Magnitude of depression problem among primary care consumers in Saudi Arabia. Institution Based Cross-Sectional study. Int J Med Sci Public Health. 2015;4(2):205–210. doi:10.5455/ijmsph.
12. Vivian Kapil V, Ramya Revathi R, Zubaida Sultana S. A cross sectional study of depression among patients with hypertension in a tertiary care. Hospital. 7(3):March-2018: ISSN No 2277-8179 | IF: 4.758 | IC Value: 93.98.
13. Neupane D, Panthi B, McLachlan CS, Mishra SR, Kohrt BA, Kallestrup P. Prevalence of undiagnosed depression among persons with hypertension and associated risk factors: a cross-sectional study in urban Nepal. PLoS One. 2015;10(2):e0117329. doi:10.1371/journal.pone.0117329
14. Kohrt BA, Hruschka DJ, Worthman CM, et al. Political violence and mental health in Nepal: prospective study. Br J Psychiatry. 2012;201(4):268–275. doi:10.1192/bjp.bp.111.096222
15. Luitel NP, Jordans MJ, Sapkota RP, et al. Conflict and mental health: a cross-sectional epidemiological study in Nepal. Social Psychiatry Psychiatric Epidemiol. 2013;48(2):183–193. doi:10.1007/s00127-012-0539-0
16. Kohrt BA, Speckman RA, Kunz RD, et al. Culture in psychiatric epidemiology: using ethnography and multiple mediator models to assess the relationship of caste with depression and anxiety in Nepal. Ann Hum Biol. 2009;36(3):261–280. doi:10.1080/03014460902839194
17. Tilahun H, Awoke N, Geda B, Mesfin F. Depression and associated factors among adult inpatients at public hospitals of Harari regional state, Eastern Ethiopia. Hindawi Psychiatry J. 2018;(Article ID 6743520):6. doi:10.1155/2018/6743520
18. Gan Z, Li Y, Xie D, et al. The impact of educational status on the clinical features of major depressive disorder among Chinese women. J Affect Disord. 2012;136(3):988–992. doi:10.1016/j.jad.2011.06.046
19. Ashok VG, Ghosh SS. Prevalence of depression among hypertensive patients attending a rural health centre in Kanyakumari. Natl J Community Med. 2019;10(3):172–175.
20. World health organization guideline (WHO), 2012. doi:10.1094/PDIS-11-11-0999-PDN
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
