Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Lung ultrasound for the diagnosis of childhood pneumonia: a safe and accurate imaging mode
Authors Hendaus M, Jomha F, Alhammadi A
Received 11 September 2015
Accepted for publication 12 November 2015
Published 9 December 2015 Volume 2015:11 Pages 1817—1818
DOI https://doi.org/10.2147/TCRM.S96222
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Mohamed Ata Hendaus,1,2 Fatima Ahmed Jomha,3 Ahmed Hassan Alhammadi1,2
1Department of Pediatrics, Academic General Pediatrics Division, Hamad Medical Corporation, Doha, 2Weill Cornell Medical College-Qatar, Al Rayyan, Qatar; 3School of Pharmacy, Lebanese International University, Khiara, Lebanon
Abstract: Pneumonia is the most common infectious cause of mortality in children worldwide. Chest x-ray (CXR) has been used as a supplementary mode in the diagnosis of pneumonia in children, but its frequent use might expose children to unnecessary ionizing radiation. In this review, we present up-to-date data of an alternative mode of imaging other than CXR in the diagnosis of pneumonia in children. We found that lung ultrasound is a safe and accurate mode of imaging that can be used by a health care provider in the cases of suspected pneumonia. It is more sensitive than CXR in the diagnosis of pneumonia and obviates the need for irradiation.
Keywords: lung ultrasound, children, pneumonia
Introduction
Pneumonia is the most common infectious cause of mortality in children worldwide. The World Health Organization predicts that pneumonia has a universal annual incidence of almost one million mortality cases in children, comprising approximately 15% of all deaths of individuals under 5 years of age.1 Despite the introduction of the pneumococcal conjugate vaccine, community-acquired pneumonia is still considered as a common cause of morbidity among children aged ≤5 years in developed countries, where the incidence reaches from 10–40 cases per 1,000 subjects.2 The presentation of pneumonia in children varies according to the child’s age group and the culprit microorganism, creating a diagnostic challenge among clinicians.3
Imaging
Chest x-ray (CXR) has been used as a supplementary mode in the diagnosis of pneumonia in children.2 However, CXR has major limitations. For instance, it exposes children to ionizing radiation, which may have tardive effects.2–3 Moreover, deficiency of abnormalities on CXR does not eliminate the diagnosis, especially in cases when there is a high index of suspicion of clinical pneumonia.3 In addition, it has been reported that CXR is not sensitive in detecting lung consolidations of ≤1 cm.4 The lack of findings on CXR results in the over diagnosis of bacterial pneumonia and leads to a number of secondary problems, the most important of which is the overuse of unwarranted antibiotics.2 Chest computed tomography scan is known to be more accurate than CXR for the diagnosis of pneumonia; however, its use has been discouraged due to high radiation, cost, and perhaps the need for sedation.3
Lung ultrasound
There has been enthusiasm among researchers in developing new devices designed to augment the usefulness and accuracy of the diagnosis of pneumonia, while concurrently reducing exposure to ionizing radiation. Lung ultrasound (LUS) has been shortlisted as an option for the diagnosis of pneumonia because it is safe, inexpensive, portable, and uncomplicated to learn and teach.2
Several authors studied the sensitivity and specificity of LUS compared to CXR in the diagnosis of pneumonia in children. Pereda et al3 performed a meta-analysis to summarize evidence on the diagnostic accuracy of LUS for childhood pneumonia. A total of 765 children were included in the meta-analysis. The authors concluded that LUS had a sensitivity of 96% (95% confidence interval [CI], 94%–97%) and specificity of 93% (95% CI, 90%–96%) in accurately diagnosing pneumonia in children. In addition, the positive and negative likelihood ratios (LRs) were 15.3 (95% CI, 6.6–35.3) and 0.06 (95% CI, 0.03–0.11), respectively. Copetti et al5 compared the diagnostic accuracy of LUS and CXR in children with suspected pneumonia. The study included 79 children with clinical pneumonia, who were subjected to both LUS and CXR. The results of the study showed that CXR was positive for the diagnosis of pneumonia in 53 patients, while LUS was positive in 60. Computed tomography of the chest verified the diagnosis of pneumonia in four patients with positive LUS and negative CXR. In a prospective study, Esposito et al2 compared the sensitivity, specificity, and positive and negative predictive values of LUS with CXR in the diagnosis of pneumonia in children. The study, which included 103 children, concluded that the sensitivity, specificity, and positive and negative predictive values of LUS in comparison to CXR were 97.9%, 94.5%, 94.0%, and 98.1%, respectively. In addition, LUS showed higher caliber in the diagnosis of pleural effusion. Shah et al4 conducted a prospective observational cohort study to assess the accuracy of point-of-care LUS for the diagnosis of pneumonia in 200 children and young adults up to 21 years of age. The authors calculated the specificity and positive LR to detail for lung consolidation of 1 cm or less with ultrasound air bronchograms not seen in CXR. The study concluded that LUS has a specificity of 89% (95% CI, 83%–93%), sensitivity of 86% (95% CI, 71%–94%), positive LR of 7.8 (95% CI, 5.0–12.4), and negative LR of 0.2 (95% CI, 0.1–0.4) for diagnosing pneumonia by visualizing lung consolidation with ultrasound air bronchograms. Table 1 summarizes the advantages of LUS.
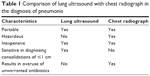  | Table 1 Comparison of lung ultrasound with chest radiograph in the diagnosis of pneumonia |
Conclusion
LUS is a safe and accurate mode of imaging that can be used by a health care provider in the cases of suspected pneumonia. It is more sensitive that CXR in the diagnosis of pneumonia and obviates the need for irradiation. Mastering the use of an ultrasound and identifying lung abnormalities lacks complexity, therefore, it is highly recommended that residency programs introduce an intensive short course of radiology as part of the core curriculum.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Pneumonia. Fact Sheet No 331. Geneva, Switzerland. Available from: www.who.int/mediacentre/factsheets/fs331/en/. Accessed March 22, 2015. | ||
Esposito S, Papa SS, Borzani I, et al. Performance of lung ultrasonography in children with community-acquired pneumonia. Ital J Pediatr. 2014;40:37. | ||
Pereda MA, Chavez MA, Hooper-Miele CC, et al. Lung ultrasound for the diagnosis of pneumonia in children: a meta-analysis. Pediatrics. 2015;135(4):714–722. | ||
Shah VP, Tunik MG, Tsung JW. Prospective evaluation of point-of-care ultrasonography for the diagnosis of pneumonia in children and young adults. JAMA Pediatr. 2013;167:119–125. | ||
Copetti R, Cattarossi L. Ultrasound diagnosis of pneumonia in children. Radiol Med. 2008;113(2):190–198. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
