Back to Journals » Patient Preference and Adherence » Volume 17
Low Prevalence of Use of Allied Health and Community Services for Patients with Cirrhosis in Australia: A Need for Greater Engagement
Authors Powell EE, Stuart KA, Finnigan S, Hinson J, Bernardes CM , Hartel G , Valery PC
Received 23 January 2023
Accepted for publication 22 March 2023
Published 20 April 2023 Volume 2023:17 Pages 1117—1130
DOI https://doi.org/10.2147/PPA.S405567
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Elizabeth E Powell,1,2 Katherine A Stuart,1 Simon Finnigan,3 Jan Hinson,4 Christina M Bernardes,5 Gunter Hartel,6 Patricia C Valery2,5
1Department of Gastroenterology and Hepatology, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia; 2Centre for Liver Disease Research, Faculty of Medicine, the University of Queensland, Woolloongabba, Queensland, Australia; 3Community and Oral Health, Metro North Health, Chermside, Queensland, Australia; 4Faculty of Health Sciences, School of Allied Health, Australian Catholic University, Banyo, Queensland, Australia; 5Population Health Department, QIMR Berghofer Medical Research Institute, Herston, Queensland, Australia; 6Statistics, QIMR Berghofer Medical Research Institute, Herston, Queensland, Australia
Correspondence: Patricia C Valery, QIMR Berghofer Medical Research Institute, 300 Herston Road, Herston, Queensland, 4006, Australia, Tel +61 07 3362 0376, Email [email protected]
Background: Psychosocial, lifestyle and practical needs are not routinely attended to during outpatient hepatology management, and little is known about the type and effectiveness of support services accessed by patients with cirrhosis. We quantified the type and use of community and allied health services in patients with cirrhosis.
Methods: The study included 562 Australian adults with a diagnosis of cirrhosis. Health service use was assessed via questionnaire and via linkage to the Australian Medicare Benefits Schedule. Patient needs were assessed using the Supportive Needs Assessment tool for Cirrhosis (SNAC).
Results: Although most patients (85.9%) used at least one community/allied health service for support with their liver disease, many reported requiring additional help with psychosocial (67.4%), lifestyle (34.3%) or practical needs (21.9%) that were not met by available services, or patients did not access services. A multidisciplinary care plan or case conference (in the 12 months prior to recruitment) was accessed by 48% of patients, 56.2% reported the use of a general practitioner for support with cirrhosis, and a dietician was the allied health clinician most accessed by patients (45.9%). Despite the high prevalence of psychosocial needs, there was relatively limited use of mental health and social work services (14.1% of patients reported the use of a psychologist), confirmed by a low prevalence of use of mental health services (17.7%) in the linked data.
Conclusion: Patients with cirrhosis who have unmet complex physical and psychosocial needs require better strategies to increase their engagement with allied health and community services.
Keywords: psychosocial needs, unmet needs, data linkage
Introduction
Healthcare use by patients with cirrhosis is rising, with resultant resource and economic implications.1 In Australia and the United States, the age-adjusted hospitalization rate for cirrhosis is comparable, at 9.54 (95% CI 9.43–9.65) and 10.01 (95% CI 9.03–10.98) per 10,000 person-years2,3 and has increased 1.6-fold over the last decade.3 Relative to other chronic diseases including congestive heart failure and chronic obstructive pulmonary disease, patients with chronic liver disease are significantly younger, have longer hospital admissions, and more readmissions.4 In addition, people with cirrhosis often have substantial practical and psychosocial needs,5 that may impact on health service use and costs. We have recently shown that, independent of liver disease aetiology and severity, patients with unmet supportive care needs have more cirrhosis-related hospital admissions and emergency presentations, along with higher total hospitalisation costs.6 Despite these concerns, data from a large, diverse health care system in the United States found that patients with chronic liver disease had less use of ancillary services or post-acute care compared to patients with congestive heart failure and chronic obstructive pulmonary disease.4
The multiple symptoms experienced by patients with cirrhosis (fatigue, difficulty concentrating, insomnia, anxiety/mood disturbance) can have a major effect on their activities of daily living and health-related quality of life (HRQOL).7 The development of decompensated cirrhosis with ascites and hepatic encephalopathy often impacts further on patients’ HRQOL through physical impairment along with a decrease in independence and social interactions.8,9 Living with these issues can be challenging, and many patients and their carers report the need for assistance with at least one physical, psychosocial or practical need.5 In a study of 458 Australian adults with cirrhosis, we found that more than 25% of patients reported a moderate-to-high need for help with “lack of energy”, “sleep poorly”,“feel unwell”, “worry about … illness getting worse (liver cancer)”, “have anxiety/stress”, and “difficulty with daily tasks”, and the specific items and level of unmet need differed, according to patient age and liver disease severity and etiology.5
Psychosocial care needs are not routinely attended to during outpatient hepatology management, and relatively little is known about the category and effectiveness of support services accessed by patients with cirrhosis. This study aimed to quantify the type and reported use of community and allied health services by patients with cirrhosis, and to explore whether patients were satisfied with the support received. We focussed on need items that could potentially be addressed by community and allied health services included in the study questionnaire. In addition, we compared self-reported data on health service use with data obtained from Medicare, Australia’s universal health care system that subsidises health services via the Medicare Benefits Schedule (MBS).
Materials and Methods
Study Sample
Consecutive adult patients attending Hepatology/Gastroenterology clinics or admitted with a diagnosis of cirrhosis were enrolled in the CirCare study. This multicentre longitudinal study of patients with cirrhosis recruited from five hospitals in Brisbane and Logan cities in Queensland, Australia, during Jun-2017 to Dec-2018 has been described.10 Briefly, the CirCare study examined the psychometric evaluation of the SNAC,10 reported the prevalence of supportive needs of people with cirrhosis,5 and examined the association between supportive care needs and hospitalization and patient outcomes.6 Here, we focused on the use of community and allied health services utilised by patients with cirrhosis. Clinical information at recruitment was extracted from patients’ medical records and severity of cirrhosis was classified using Child-Pugh class and by the absence (compensated cirrhosis) versus presence of cirrhosis complications. Sociodemographic data were reported at recruitment and place of residence was categorised according to rurality of residence11 and the Index of Relative Socioeconomic Advantage and Disadvantage.12 The study was approved by the Human Research Ethics Committees of the Metro South Health (HREC/16/QPAH/628) and QIMR Berghofer Medical Research Institute (P2207). All study participants provided informed written consent to participate in the study, including completion of the study questionnaire, and collection of clinical information from medical records and via linkage to the Australian Medicare Benefits Schedule. The study was conducted in accordance with the Declaration of Helsinki.
Self-Reported Service Use
Patients completed a self-administered questionnaire with the assistance of study personnel face-to-face at recruitment, or by self-administered questionnaire when practical time constraints prevented face-to-face completion. Reported service use was assessed by the question “Have you accessed any of the following community or allied health services for support with your liver disease”, and a tick box list, which enabled participants to indicate whether they had accessed any of the following services: Indigenous Hospital Liaison Officer, Aboriginal Health Services, Traditional Indigenous practitioner, Ethnic Community Council Queensland Health worker, Community Health Nurse, Home and Community Care Services, complementary medicine practitioner, respite care, patient travel subsidy scheme, other transport support service, peer support, community-based support group, internet-based support group, chaplain, information sheets/brochures, internet information, education program/workshop, liver disease support group, viral hepatitis support group, pain specialist, relaxation/meditation class, exercise physiologist, dietician, physiotherapist, social worker, psychologist, psychiatrist, mental health team, palliative care team.
Data Linkage
Data linkage was undertaken to the Australian Medicare Benefits Schedule and complete MBS histories during the 12-month period prior to CirCare recruitment were extracted. The MBS database contains information on services that qualify for a benefit under the Health Insurance Act 1973 and for which a claim has been processed. The database comprises information about MBS claims (including benefits paid), patients and service providers. Relevant to this study, MBS benefits are payable for: consultations with doctors, including specialists; consultations with psychologists; and allied health services for patients with a chronic or terminal medical condition and complex care needs (eg, social workers, occupational therapists). Patients with mental health issues, for example, are eligible to receive up to 10 individual and up to 10 group subsidised allied mental health services per calendar year.13 However, there are delays in accessing such services (eg, 38.9% of people who needed to see a health professional for their mental health had to wait or did not see one when needed)14 and subsidised sessions may not be adequate to facilitate patient’s improvement.15
Assessment of Physical, Psychosocial and Practical Needs
Patient needs were assessed via questionnaire at recruitment using the Supportive Needs Assessment tool for Cirrhosis (SNAC).10 This validated tool assesses patient needs across 39 items grouped in four subscales. The supportive care needs of the CirCare study participants have been described.5 Here, we focused on two selected need items included in the SNAC tool: items about transport and daily tasks around the house included in the “Practical and physical needs” subscale, and all items included in two subscales (“Psychosocial issues” and “Lifestyle changes”). Patients were grouped as “no need for help” for a particular item or subscale, “need was satisfied”, and “need was not satisfied” (needing “a little”, “some”, and “a lot” of help with one item or at least one item in a subscale). We compared patient responses to relevant need items included in the SNAC tool to self-reported consultation with appropriate community health services that could potentially address their needs. The selection of need items and corresponding health professionals or services were allocated in consultation with health professionals (social worker (JH), liver specialist nurse, pharmacist and hepatologist (EP)).
Statistical Methods
Analyses were conducted using Stata/SE (Version 17; Stata Corporation, College Station, TX). Summary statistics were used to describe the patient population and assess the prevalence of reported use of health services. Frequency and percentages were used for categorical variables, mean and standard deviation (SD) for continuous normally distributed data, and median and interquartile range (IQR) for continuous not-normally distributed data. Group comparisons used the chi-square test for categorical variables (Fisher exact test was used for sparse tables).
Multivariable logistic regression analysis assessed factors associated with reported use of health services. We built one model with use of any health service as endpoint. The variables sex, age group, Indigenous status, education, living arrangements, socioeconomic status, remoteness of residence, Child-Pugh class, primary liver disease aetiology, and diabetes were considered and we used stepwise selection of variables based on p-value<0.20, but also took into account our understanding of the relationships and dependencies among variables. The final model include sex, age group, Indigenous status, education, socioeconomic status, remoteness of residence, living arrangements, Child-Pugh class, and diabetes. Adjusted odds ratios (adj-ORs) with associated 95% confidence intervals (CIs) are reported. Statistical significance was set at alpha = 0.05, and all p values were 2-sided.
Results
Patient Characteristics
Details of the CirCare study have been previously reported.10 Briefly, 562 patients with cirrhosis were recruited and completed the questionnaire (78% response rate) and their characteristics are shown in Table 1. The mean age of participants was 59.8 years, 69.9% were male, 52.5% did not have a partner, 4.6% were First Nations Peoples, 44.2% had completed Junior High School or less, and 77.6% were currently unemployed.
 |
Table 1 Patient Sociodemographic and Clinical Characteristics and Reported Supportive Care Needs at Recruitment |
Alcohol-related cirrhosis was the primary liver disease aetiology in 35.2% of patients. Approximately two-thirds of patients had Child-Pugh A at recruitment (66.3%) and 31.1% had at least one cirrhosis complication documented in their medical notes at recruitment (decompensated disease). Comorbidities were common, with type 2 diabetes recorded in 42.0% of patients and obesity (defined by body mass index (BMI) ≥30 kg/m2 or ≥27 kg/m2 for Asian participants) recorded in 44.3%.
Most patients (85.9%) reported psychosocial needs; 18.5% reported having all psychosocial needs satisfied, and 67.4% reported needing additional help (“a little”, “some”, or “a lot”) with at least one item in the “Psychosocial needs” subscale. Over half of the patients (58.9%) reported having an issue with at least one item in the “Lifestyle changes” subscale; about one-in-three (34.3%) reported needing additional help with at least one item in this subscale. Regarding the selected items from the “Practical and physical needs” subscale, 27.9% patients reported needing additional help with daily tasks around the house, and 21.9% reported needing additional help with transport.
Reported Use of Selected Community and Allied Health Services
Table 2 shows the reported use of community and allied health services by patients with cirrhosis. Most patients (85.9%) reported utilizing at least one community or allied health service for support with their liver disease. 59.3% indicated they used at least one of the “Allied Health Workers/Services”, 56.2% accessed their general practitioner (GP) about their liver disease, 38.3% used “Information services”, 11.0% used “Home & Transport community services”, and 10.1% used “Support services”. Among First Nations patients, 30.8% (8 out of 26) accessed First Nations Peoples services; four non-Indigenous patients also accessed these services.
 |
Table 2 Health Services Utilization by Patients with Cirrhosis |
Overall, reported use of any of the selected community and allied health services did not differ by sex, age-group, Indigenous status, level of education, socioeconomic status, remoteness of residence, liver disease severity (Child-Pugh class) and primary liver disease aetiology. However, use of services (any) was slightly higher among patients with diabetes as a comorbidity (Table 3).
 |
Table 3 Proportion of People Self-Reporting Use of Health Services According to Sex, Age-Group, Level of Education, Disease Severity (Child-Pugh Class), Primary Liver Disease Aetiology |
Prevalence of reported use of specific groups of health services was examined according to the abovementioned sub-groups of patients. Use of “Home & Transport community services” was higher among females (p=0.006), lower quintiles of socioeconomic status (p=0.003), and patients who lived outside major city areas (p<0.001). Use of “Allied health workers/community health services” and use of “Support services” were significantly greater among patients with advanced cirrhosis (Child-Pugh class B and C vs A; p=0.038 and p<0.001, respectively). Use of “Allied health workers/community health services” was also higher among patients with higher education level (p=0.013). Use of “Information services” was higher among younger patients (p=0.001) and patients with higher education level (p=<0.001). While the use of “First Nations peoples services” was higher among First Nations Peoples (30.8% vs 0.7%, p<0.001), a small number of non-Indigenous patients accessed these services.
MBS Data on Use of Selected Health Services
Most patients with cirrhosis (97.3%) had at least one appointment with a GP or specialist visit in the 12 months prior to recruitment (median number of visits 12, IQR 6–19) (Table 1). About half the patients (48.0%) had at least one multidisciplinary care plan or case conference, 29.9% had after-hours consultations, and 17.7% accessed mental health services.
Need for Help with Selected Supportive Care Need Items and Corresponding Reported Access to Relevant Health Professionals
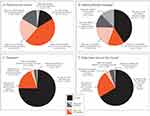
Psychosocial need for help was measured by 14 items in the SNAC tool included in the “Psychosocial issues” subscale.10 Corresponding reported consultation with a psychologist, psychiatrist, social worker or mental health team, were considered relevant psychosocial health professionals. Overall, 79 patients (14.1%) reported no need for help with psychosocial issues, and 483 patients (85.9%) reported at least one psychosocial need (Table 1). As displayed in Figure 1A and out of 562 patients, the need for additional help with at least one psychosocial need was reported by 125 (22.2%) patients who reported accessing relevant services and 254 (45.2%) patients who did not access relevant services. All psychosocial needs were met for 104 patients (18.5%), and 16 (2.9% of 562) of them reported having accessed relevant services.
Need for help with making lifestyle changes was measured by two items in the SNAC tool included in the “Lifestyle changes” subscale. Corresponding reported consultation with a dietitian, an exercise physiologist, or a physiotherapist were considered the relevant services to address this need. Overall, 231 patients (41.1%) reported no need for help with making lifestyle changes (eg, low salt diet, stopping alcohol, lose weight), and 331 patients (58.9%) reported at least one need with making lifestyle changes. The need for additional help with at least one need item in this subscale was reported by 109 (19.4%) patients who reported accessing relevant services and 84 (14.9%) who did not access relevant services. All needs with making lifestyle changes were met for 70 (12.5%) patients who reported accessing relevant services and 68 (12.1%) patients who did not access relevant services (Figure 1B).
Need for help with transport was measured by one item in the SNAC tool, and corresponding use of Patient Transport Subsidy Scheme or other transport services were considered the relevant services to address this need. Overall, 141 patients (25.1%) reported needing help with transport. The need for additional help with transport was reported by 108 (24.2%) patients who reported not accessing relevant services and 15 (2.6%) patients who accessed such services. Eighteen (3.2%) patients reported having their transport needs met (Figure 1C).
Need for help with daily tasks around the house was measured by one item in the SNAC tool, and corresponding use of Home and Community Care Services or other home care (eg, Blue Care, Respite Care) were considered the relevant services to address this need. One-third of patients (N=189, 33.6%) reported need for help with daily tasks around the house. The need for additional help with daily tasks around the house was reported by 136 (24.2%) patients who did not access relevant services and 21 (3.7%) patients who reported accessing such services. Thirty-two (5.7%) patients reported having their needs with daily tasks around the house met (Figure 1D).
Factors Associated with Reported Use of Health Services
The factors associated with reported use of health services are detailed in Table 4. Patients with diabetes were twice as likely to report the use of any health service for support with their liver disease (adj-OR=2.07, 95% CI 1.19–3.60), and they were 1.5-fold more likely to use “Allied Health Workers/Services” (adj-OR=1.48, 95% CI 1.02–2.14). Compared to patients with Child-Pugh A, patients with Child-Pugh B and C were more likely to use “Support services” (adj-OR=3.55, 95% CI 1.89–6.65 and adj-OR=2.64, 95% CI 1.12–6.25, respectively), and patients with Child-Pugh C were more likely to use “Allied Health Workers/Services” (adj-OR=2.28, 95% CI 1.20–4.32). Patients who lived outside major city areas were 5 times more likely to use “Home & Transport community services” (adj-OR=5.01, 95% CI 2.60–9.67). Older age (65+ years) and lower education level was associated with less use of “Information services” (adj-OR=0.58, 95% CI 0.39–0.87 and adj-OR=0.49, 95% CI 0.33–0.71, respectively). Male patients were less likely to report the use of “Home & Transport community services” (adj-OR= 0.46, 95% CI 0.26–0.82), and patients who identified as Indigenous Australians were less likely to report the use of “Allied Health Workers/Services” (adj-OR= 0.44, 95% CI 0.19–1.04).
 |
Table 4 Multivariable Logistic Regression Analysis Assessing Factors Associated with Reported Use of Health Services |
Discussion
This multicentre study of patients with cirrhosis recruited from five large public hospitals in Brisbane and Logan, Queensland, Australia shows that the majority of patients (85.9%) with cirrhosis used at least one community or allied health service for support. However, a substantial proportion of patients (67.4%) reported requiring additional help with psychosocial needs that were not met with use of available services or they did not access services. Many patients (21.9% to 34.3%) reported requiring additional help with lifestyle changes and practical needs that were also not met with use of available services or services were not used by them. Clinical factors (diabetes and advanced cirrhosis) were associated with use of “Allied Health Workers/Services” and “Support services”, while sociodemographic characteristics (being male, older age (65+ years), lower education level and Indigenous status) were associated with less use of selected services.
Analysis of linked data from the MBS found that virtually all patients (97.3%) with cirrhosis had at least one (and often multiple) visits to a GP or specialist in the 12 months prior to recruitment and 48% accessed a multidisciplinary care plan or case conference. In addition, at least half of the patients (56.2%) reported the use of a GP for support with their liver disease. This is important because GPs play a crucial role in chronic disease management and can coordinate the multidisciplinary team of medical specialists and allied health clinicians. In the UK, a strategy to implement chronic liver disease management in primary care is being developed, and key recommendations include
… to standardise and integrate management protocols, incorporate liver disease into multimorbidity care, define a clear role for GPs, and promote education and local champions to drive these changes.16
However, to our knowledge, in Australia there are no defined care pathways or quality indicators for the diagnosis and treatment of liver disease in primary care and many GPs report a lack of clear guidance regarding its management. One likely reason for this is the historical focus of medical education on more common chronic conditions (eg, type 2 diabetes, cardiovascular disease, chronic kidney disease).
Not surprisingly, the allied health clinician most accessed by our patients with cirrhosis (45.9%) was a dietician, and patients with Child-Pugh C and diabetes were more likely to report use of these services. Dietary changes are often necessary following a diagnosis of cirrhosis, to ensure adequate energy and protein intake along with a reduction in salt. In overweight patients, a high protein intake and increased physical activity is important to maintain muscle mass, while reducing fat and carbohydrate intake. Of concern, only a minority of participants reported use of an exercise physiologist (4.4%) or physiotherapist (11.6%), despite the high prevalence of frailty in patients with cirrhosis. Physical frailty is closely associated with reduced functioning and increased mortality risk,17,18 but muscle mass may potentially be improved with exercise and resistance training.19–21 Almost one-third of our patients (31%) reported a need for assistance with making lifestyle or dietary changes, and either did not access the relevant services (14%) or, the need persisted despite use of these services (17%). Improving access to, and optimizing the content and mode of delivery of these services is crucial for people with cirrhosis.
This study found that, despite the ongoing psychosocial needs reported by 85.9% of this patient cohort, there was relatively limited use of mental health and social work services. Only 14.1% of patients reported the use of a psychologist, confirmed by a low prevalence of use of mental health services (17.7%) in the linked MBS data. A recent study from Denmark found that 22% of 541 patients with cirrhosis reported low social support, loneliness (35%) and lived alone (48%), these being higher proportions than among 2157 matched comparators.22 Compared to patients with medium or high social support, those with low social support had a 5.1 (95% confidence interval (CI) 2.6–8.0, p<0.001) point lower mental HRQoL score and an adjusted HR risk of mortality of 1.4 (95% CI 1.1–1.9, p=0.011).22 In other chronic conditions (eg, hypertension, obesity, diabetes), an intervention to provide greater social support and address social determinants of health, led to reductions in hospital use and better perceived quality of care.23 Greater understanding by hepatologists, liver specialist nurses and other allied health professionals of the wide-ranging needs of patients and their families, besides their medical needs and treatments, may improve referral to and engagement with different specialties or support services. In the current environment, this level of care may not be possible due to time and cost constraints, and the need for additional resources. Published data from the CirCare study showed that patients with a higher level of unmet psychosocial, practical and physical needs had higher service use and cost related to their liver disease. There was a higher rate of hospital admissions (2.1-fold higher), emergency presentations (3.6-fold), and total cost of cirrhosis admissions (3.5-fold) compared to patients with low or no needs.6 Interventions that include additional health professionals working as part of a multidisciplinary clinical care team to assess and address patients’ support needs may promote a more cost-effective use of healthcare services.
Another key finding was the lower use of allied health and information services among patients with less education and older age. These demographic factors may contribute to lower health literacy,24 which influences how patients access and navigate health care services. We have previously shown that patients with “good knowledge” about cirrhosis (having at least 5 out of 8 correct answers to the knowledge questions) had fewer cirrhosis-related admissions (adjusted incidence rate ratio [adj-IRR]=0.59, 95% CI 0.35–0.99) and emergency presentations (adj-IRR=0.34, 95% CI 0.16–0.72), and lower total cost of cirrhosis admissions (adj-IRR=0.30, 95% CI 0.29–0.30).25 Strategies and resources to support people with cirrhosis and increase access to services need to be suitable to their health literacy needs in order to be effective.
The reasons underlying the limited access to and engagement with community and allied health services by patients with cirrhosis who have unmet practical and psychosocial needs are likely to be multifactorial. Firstly, patients’ supportive care needs may not have been assessed during clinical consultation, and therefore their unmet needs were not identified. Secondly, financial hardship due to the costs involved in managing cirrhosis is common,26 and can lead to delayed care-seeking particularly for health services that are non-subsidised. Thirdly, geographical accessibility is likely to affect the use of health services. Distance between the patient’s place of residence and the health service or limited transport options may influence patient use of such services. Lastly, in line with the epidemiology of chronic liver disease, the majority of patients included in the study were male. In general, males are less likely than females to access health services,14 potentially explaining, at least in part, the poor engagement with community and allied health services by patients with cirrhosis.
Study limitations must be considered when interpreting our findings. Patients were recruited from five liver specialist clinics located in large hospitals, and those with cognitive impairment, from a non-English-speaking background and those living in regional and remote areas were excluded. Patients managed in liver specialist clinics in public hospitals in a major city may have a different pattern of use of community and allied health services compared to those who are managed by private or regional hospitals and non-hepatologists. Consequently, findings from this multicentre study may not be directly generalizable to all patients with cirrhosis in Australia. The analysis was cross-sectional, therefore it was not possible to assess temporal associations between supportive care needs and access to services. Although supportive care needs were assessed using a validated tool, the question about reported service use was not validated. While the list of community and allied health services was comprehensive, it did not include some specific community health services used by patients with chronic liver disease (eg, alcohol and drug services). Health services not listed may be less likely to be recalled, likely explaining the small number of patients reporting these services. Finally, due to the small sample size in some of the patient sub-groups, our findings should be interpreted with caution as there may have been differences that the study did not detect.
Conclusions
Our data from mainstream liver specialist centres showed that while most patients with cirrhosis used at least one community or allied health service for support with their liver disease, for many patients their supportive care needs, in particular psychosocial needs, were not met by use of available services or they did not access services. Our study highlighted the need for greater access to and engagement with allied health and community services for patients with cirrhosis who have unmet complex physical and psychosocial needs. From an international perspective, our findings may be relevant to other high-income countries with universal health care systems and provide insight into potential areas for further research, in particular, whether better availability and use of community or allied health services leads to a reduction in hospital-related health care costs.
Abbreviations
BMI, Body mass index; CI, Confidence interval; GP, General practitioner; HRQOL, Health-related quality of life; IRR, Incidence rate ratio; IQR, Interquartile range; MBS, Medicare Benefits Schedule; SD, Standard deviations; SNAC, Supportive Needs Assessment tool for Cirrhosis.
Data Sharing Statement
The data that support the study findings may contain potentially identifying information that could compromise the privacy of the participants. Therefore, the data are not publicly available. Data may, however, be available from the authors upon reasonable request with approval from relevant ethics committees.
Acknowledgments
We thank the staff and patients of the participating hospitals for their assistance and cooperation in performing the current study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by a Metro South Health Research Support Scheme (MSH RSS) 2020 Project Grant. The funder had no role in study design, data collection, data analysis, interpretation, or writing of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sepanlou SG, Safiri S, Bisignano C.; Collaborators GBDC. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi:10.1016/S2468-1253(19)30349-8
2. Chirapongsathorn S, Krittanawong C, Enders FT, et al. Incidence and cost analysis of hospital admission and 30-day readmission among patients with cirrhosis. Hepatol Commun. 2018;2(2):188–198. doi:10.1002/hep4.1137
3. Powell EE, Skoien R, Rahman T, et al. Increasing Hospitalization Rates for Cirrhosis: overrepresentation of Disadvantaged Australians. EClinicalMedicine. 2019;11:44–53. doi:10.1016/j.eclinm.2019.05.007
4. Asrani SK, Kouznetsova M, Ogola G, et al. Increasing Health Care Burden of Chronic Liver Disease Compared With Other Chronic Diseases, 2004-2013. Gastroenterology. 2018;155(3):719–729 e714. doi:10.1053/j.gastro.2018.05.032
5. Valery PC, Bernardes CM, McKillen B, et al. The Patient’s Perspective in Cirrhosis: unmet Supportive Care Needs Differ by Disease Severity, Etiology, and Age. Hepatol Commun. 2021;5(5):891–905. doi:10.1002/hep4.1681
6. Valery PC, Stuart KA, Bernardes CM, et al. Higher levels of supportive care needs are linked to higher health service use and cost, poor quality of life, and high distress in patients with cirrhosis in Queensland, Australia. Hepatol Commun. 2023;7(3):e0066. doi:10.1097/HC9.0000000000000066
7. Younossi Z, Henry L. Overall health-related quality of life in patients with end-stage liver disease. Clin Liver Dis. 2015;6(1):9–14. doi:10.1002/cld.480
8. Orr JG, Homer T, Ternent L, et al. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61(5):1158–1165. doi:10.1016/j.jhep.2014.06.034
9. Rabiee A, Ximenes RO, Nikayin S, et al. Factors associated with health-related quality of life in patients with cirrhosis: a systematic review. Liver Int. 2021;41(1):6–15. doi:10.1111/liv.14680
10. Valery PC, Bernardes CM, Stuart KA, et al. Development and Evaluation of the Supportive Needs Assessment Tool for Cirrhosis (SNAC). Patient Prefer Adherence. 2020;14:599–611. doi:10.2147/PPA.S236818
11. Australian Institute of Health and Welfare (AIHW). Rural, Regional and Remote Health: A Guide to Remoteness Classifications. Canberra, Australia: AIHW; 2004.
12. Australian Bureau of Statistics (ABS). Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2006. Canberra, Australia: ABS; 2008.
13. Australian Government Department of Health. Better Access to Psychiatrists, Psychologists and General Practitioners Through the MBS (Better Access) Initiative. Canberra: Australian Government Department of Health and Aged Care; 2019.
14. Australian Bureau of Statistics (ABS). Patient Experiences: Reference Period 2021-22 financial year. Canberra: ABS; 2022.
15. Barr ML, Welberry H, Comino EJ, et al. Understanding the use and impact of allied health services for people with chronic health conditions in Central and Eastern Sydney, Australia: a five-year longitudinal analysis. Prim Health Care Res Dev. 2019;20:e141. doi:10.1017/S146342361900077X
16. Jarvis H, Sanders T, Hanratty B. Liver disease management as routine work in primary care: a qualitative interview study to guide implementation. Br J Gen Pract. 2022;72(725):e916–e923. doi:10.3399/BJGP.2022.0094
17. Lai JC, Dodge JL, McCulloch CE, Covinsky KE, Singer JP. Frailty and the Burden of Concurrent and Incident Disability in Patients With Cirrhosis: a Prospective Cohort Study. Hepatol Commun. 2020;4(1):126–133. doi:10.1002/hep4.1444
18. Lai JC, Rahimi RS, Verna EC, et al. Frailty Associated With Waitlist Mortality Independent of Ascites and Hepatic Encephalopathy in a Multicenter Study. Gastroenterology. 2019;156(6):1675–1682. doi:10.1053/j.gastro.2019.01.028
19. Lai JC, Dodge JL, Kappus MR, et al. A Multicenter Pilot Randomized Clinical Trial of a Home-Based Exercise Program for Patients With Cirrhosis: the Strength Training Intervention (STRIVE). Am J Gastroenterol. 2021;116(4):717–722. doi:10.14309/ajg.0000000000001113
20. Johnston HE, Takefala TG, Kelly JT, et al. The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: a Systematic Review. Nutrients. 2022;14(16):3365. doi:10.3390/nu14163365
21. West J, Gow PJ, Testro A, Chapman B, Sinclair M. Exercise physiology in cirrhosis and the potential benefits of exercise interventions: a review. J Gastroenterol Hepatol. 2021;36(10):2687–2705. doi:10.1111/jgh.15474
22. Askgaard G, Madsen LG, von Wowern N, et al. Social support and risk of mortality in liver cirrhosis: a cohort study. JHEP Reports. 2022;5. doi:10.1016/j.jhepr.2022.100600
23. Kangovi S, Mitra N, Norton L, et al. Effect of Community Health Worker Support on Clinical Outcomes of Low-Income Patients Across Primary Care Facilities: a Randomized Clinical Trial. JAMA Intern Med. 2018;178(12):1635–1643. doi:10.1001/jamainternmed.2018.4630
24. Beauchamp A, Buchbinder R, Dodson S, et al. Distribution of health literacy strengths and weaknesses across socio-demographic groups: a cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health. 2015;15:678. doi:10.1186/s12889-015-2056-z
25. Valery PC, Bernardes CM, Hayward KL, et al. Poor disease knowledge is associated with higher healthcare service use and costs among patients with cirrhosis: an exploratory study. BMC Gastroenterol. 2022;22(1):340. doi:10.1186/s12876-022-02407-6
26. Lago-Hernandez C, Nguyen NH, Khera R, Loomba R, Asrani SK, Singh S. Cost-Related Nonadherence to Medications Among US Adults With Chronic Liver Diseases. Mayo Clin Proc. 2021;96(10):2639–2650. doi:10.1016/j.mayocp.2021.02.026
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.