Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Low-density lipoprotein cholesterol of less than 70 mg/dL is associated with fewer cardiovascular events in acute coronary syndrome patients: a real-life cohort in Thailand
Authors Chinwong D, Patumanond J , Chinwong S, Siriwattana K, Gunaparn S, Joseph Hall J, Phrommintikul A
Received 5 December 2014
Accepted for publication 2 February 2015
Published 24 April 2015 Volume 2015:11 Pages 659—667
DOI https://doi.org/10.2147/TCRM.S78745
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Dujrudee Chinwong,1,2 Jayanton Patumanond,3 Surarong Chinwong,1 Khanchai Siriwattana,4 Siriluck Gunaparn,5 John Joseph Hall,6 Arintaya Phrommintikul5
1Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand; 2Clinical Epidemiology Program, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 3Center of Excellence in Applied Epidemiology, Faculty of Medicine, Thammasat University, Pathum Thani, Thailand; 4Division of Medicine, Nakornping Hospital, Chiang Mai, Thailand; 5Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 6Centre for Clinical Epidemiology and Biostatistics, School of Medicine and Public Health, Faculty of Health, University of Newcastle, Callaghan, NSW, Australia
Background: Elevated low-density lipoprotein cholesterol (LDL-C) is associated with an increased risk of cardiovascular disease or mortality; however, the LDL-C goal for therapy in acute coronary syndrome (ACS) patients is controversial and varies among guidelines. This study aimed to assess the effect of reaching an LDL-C goal of <70 mg/dL (<1.8 mmol/L) on first composite cardiovascular outcomes in routine clinical practice in Thailand.
Methods: A retrospective cohort study was conducted using medical charts and the electronic hospital database of patients diagnosed with ACS and treated with statins at a tertiary care hospital in Thailand between 2009 and 2012. After admission, patients were followed from the date of LDL-C goal assessment until the first event of composite cardiovascular outcomes (nonfatal ACS, nonfatal stroke, or all-cause death). Cox proportional hazard models adjusted for potential confounders were used.
Results: Of 405 patients, mean age was 65 years (60% males). Twenty-seven percent of the patients attained an LDL-C goal of <70 mg/dL, 38% had LDL-C between 70 and 99 mg/dL, and 35% had LDL-C ≥100 mg/dL. Forty-six patients experienced a composite cardiovascular outcome. Compared with patients with an LDL-C ≥100 mg/dL, patients achieving an LDL-C of <70 mg/dL were associated with a reduced composite cardiovascular outcome (adjusted hazard ratio [HR]=0.42; 95% confidence interval [CI]=0.18–0.95; P-value=0.037), but patients with an LDL-C between 70 and 99 mg/dL had a lower composite cardiovascular outcome, which was not statistically significant (adjusted HR=0.73; 95% CI=0.37–1.42; P-value=0.354).
Conclusion: ACS patients who received statins and achieved an LDL-C of <70 mg/dL had significantly fewer composite cardiovascular outcomes, confirming “the lower the better” and the benefit of treating to LDL-C target in ACS patient management.
Keywords: LDL-C goal attainment, achieving LDL-C goal, statins, acute coronary syndrome, composite cardiovascular events
Introduction
Coronary artery disease (CAD) is one of the leading causes of death worldwide1 and also in Thailand.2 Well-established research demonstrates that a reduction in low-density lipoprotein cholesterol (LDL-C) is associated with a reduced risk of developing cardiovascular events and of mortality.3–7 The main stem in LDL-C reduction is the 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor, also known as statins.4,7,8 Recommending a treatment target for LDL-C for patients at very high cardiovascular risk, such as patients with acute coronary syndrome (ACS), is based on substantial evidence. Many commonly used guidelines (eg, the National Cholesterol Education Program/Adult Treatment Panel III [NCEP/ATP III]4 and the guidelines of the European Society of Cardiology and the European Atherosclerosis Society [ESC/EAS])7 recommend a goal of <70 mg/dL in these very high-risk patients. By contrast, recent guidelines (the 2013 American College of Cardiology/American Heart Association [ACC/AHA] on cholesterol management,9 as well as the National Institute for Health and Care Excellence [NICE] guidelines on lipid modification released in July 2014)10 use the “fire and forget approach”, which does not recommend LDL-C goal attainment because of a lack of randomized controlled trials (RCTs) establishing the benefit of the effect of treating to LDL-C target on cardiovascular morbidity and mortality. These later guidelines recommend the use of high-intensity statins for secondary prevention in ACS patients, with repeated measurement of lipid profiles being used to monitor patient compliance rather than LDL-C goal attainment.
It is common that very high cardiovascular risk patients such as ACS patients have difficulty in achieving an LDL-C goal of <70 mg/dL. Less than 45% of high-risk patients can reach LDL-C of <70 mg/dL,11–24 with only 10% of patients achieving this goal in a study conducted in Greece.13 Patients not achieving the desired LDL-C goal are at greater risk of cardiovascular events. The treat to target approach has greater benefit in identifying those ACS patients who fail to attain the LDL-C goal. In contrast, the fire and forget approach fails to recognize those ACS patients not achieving the desired goal; these ACS patients are at higher risk of cardiovascular events. As per the 2013 ACC/AHA guidelines, which recommend treatment according to patient risk and statin potency, a reduction in LDL-C of at least 50% is expected with high-intensity statins; however, variations in response to medications from patient to patient are common. Without follow-up lipid profiles, there is difficulty in evaluating the patients’ cardiovascular risks. Elimination of the LDL-C goal target is perhaps the most controversial change among experts and physicans since the new 2013 ACC/AHA guidelines were released in November 2013.25,26 This study therefore aimed to assess the association between LDL-C goal attainment of <70 mg/dL and cardiovascular outcomes in ACS patients treated with statins in routine clinical practice in Thailand.
Methods
Study population and setting
This retrospective cohort study was performed at a university-affiliated hospital, the Maharaj Nakorn Chiang Mai Hospital, in northern Thailand. This hospital provides services to patients in Chiang Mai province (a population of 1,600,000) as well as those patients referred from hospitals from 17 other provinces in the north. The hospital has 1,400 patient beds and an average of 1,300,000 outpatients and 48,000 inpatients each year. The study protocol was reviewed and approved by the Research Ethics Committee, Faculty of Medicine, Chiang Mai University, before commencement of the study.
A study nurse aware of the protocol and a researcher retrospectively selected all patients (aged ≥18 years) hospitalized with a diagnosis of ACS according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, code of I20 (angina pectoris) and I21 (acute myocardial infarction [MI]) who were treated with statins from 2009 to 2012. The patients’ information, including demographic data, comorbidities, CAD risk factors, current medication, and laboratory results, including lipid profiles (total cholesterol, LDL-C, high-density lipoprotein, and triglycerides), was retrieved from medical charts and from the electronic hospital database. Patients were included in the analysis based on the following criteria: 1) admission date between January 1, 2009 and December 31, 2012; 2) diagnosis at discharge from medical charts as ACS patients, classified into three groups: unstable angina (UA), non ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI); 3) treated with statins during admission or on discharge date; 4) had LDL-C measurement both at admission (baseline) and at follow-up between 14 days and 1 year, as long as they remained on statins throughout this period of time; and 5) were followed for at least 12 months from the date of achieving the LDL-C goal of <70 mg/dL (index date) until the first event of cardiovascular outcomes occurred or until December 31, 2012, whichever came first, or the last entry on the medical record of a patient. Time to cardiovascular events was the interval between the dates of measuring the LDL-C goal to the date of the first cardiovascular event (Figure 1).
  | Figure 1 Flowchart of patient selection and study timeline. |
Achieved LDL-C levels and cardiovascular events
Patients were divided into three groups by lipid levels at 2 weeks to 1 year of follow-up after admission: <70 mg/dL, 70–99 mg/dL, and ≥100 mg/dL. According to the updated NCEP/ATP III4 and the ESC/EAS guidelines,7 those patients with LDL-C <70 mg/dL (<1.8 mmol/L) were classified as achieving LDL-C goal.
The primary end point was the first occurrence of any component of the composite of cardiovascular events, including nonfatal ACS (MI or UA), nonfatal stroke, or all-cause death.
Statistical analysis
We carried out all analyses with STATA software, version 12 (StataCorp LP, College Station, TX, USA). Using descriptive statistical methods, categorical variables were reported as counts and percentages, and continuous variables were presented as means with standard deviations. Differences between groups were compared using Fisher’s exact tests for categorical variables or one-way analysis of variance for continuous variables. Univariable and multivariable Cox proportional hazard models were used to determine the effect of LDL-C goal attainment on cardiovascular events. The multivariable analysis were adjusted with potential confounders (age, sex, diabetes mellitus, hypertension, serum creatinine, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, revascularization, and baseline LDL-C level) and stratified by spectrum of ACS (UA, NSTEMI, STEMI). Patients with LDL-C ≥100 mg/dL were the reference group. The two-tailed test was used, and P-value<0.05 was considered statistically significant.
Results
We identified a total of 1,089 patients diagnosed with ACS from 2009 to 2012. We excluded 684 patients from the analysis because of unavailable data of LDL-C level at baseline or follow-up, resulting in 405 patients in the final analysis. Comparison between patients included and excluded from the analysis indicated that the two groups were not significantly different in their baseline characteristics, except that included patients were younger than excluded patients (64.9±11.5 vs 67.2±12.9; P-value=0.003).
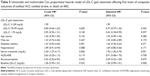
Of 405 patients, 403 patients (99.5%) were treated with statins for the whole follow-up period, which was from baseline until the dates of first cardiovascular event occurring or until December 31, 2012, whichever came first. Statin therapy in two patients (0.5%) was discontinued during their follow-up period because of their low LDL-C levels, about 40–45 mg/dL. Table 1 shows the baseline characteristics of the three groups as defined by their LDL-C level: <70 mg/dL, 70–99 mg/dL, and ≥100 mg/dL. Twenty-seven percent of the patients attained an LDL-C goal of <70 mg/dL, 38% had LDL-C between 70 and 99 mg/dL, and 35% had LDL-C ≥100 mg/dL. These three groups were similar in demographic characteristics, statin therapy, and coronary artery risk factors, except that patients with LDL-C <70 mg/dL were older and lower in total cholesterol and LDL-C levels at baseline compared with the other two groups (Tables 1–3).
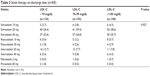  | Table 3 Statin therapy on discharge date (n=405) |
Forty-six patients experienced cardiovascular outcomes (35 nonfatal ACS, one stroke, ten deaths). Median follow-up time from the date of measuring LDL-C goal attainment (index date) to the date of occurrence of the cardiovascular event was 1.74 years (interquartile range of 0.74–2.53). The incidence rates (per 1,000 person-years) of cardiovascular outcomes were 43 in the LDL-C <70 mg/dL group, 66 in the LDL-C 70–99 mg/dL group, and 88 in the LDL-C ≥100 mg/dL group (Table 4). Multivariable Cox proportional hazard models showed that ACS patients treated with statins who achieved LDL-C of <70 mg/dL had fewer cardiovascular events compared with patients with an LDL-C ≥100 mg/dL (adjusted hazard ratio [HR]=0.42; 95% confidence interval [CI]=0.18–0.95; P-value=0.037). Similarly, patients with an LDL-C between 70 and 99 mg/dL were less likely to have cardiovascular events compared with patients with an LDL-C ≥100 mg/dL, but this was not statistically significant (adjusted HR=0.73; 95% CI=0.37–1.42; P-value=0.354) (Table 5).
Discussion
LDL-C goal attainment of <70 mg/dL has been used as a target for therapy to reduce further progression of cardiovascular events in ACS patients, as recommended by many guidelines since 2004. Recently, the treating to target approach has been a controversial issue in lipid management for physicians. Some guidelines – 2013 ACC/AHA guidelines on cholesterol management,9 as well as NICE guidelines on lipid modification10 – have abandoned the LDL-C goal due to the lack of RCT studies confirming the benefit of treating to LDL-C target on cardiovascular morbidity or mortality. Most RCTs of cholesterol-lowering medication were conducted testing drug treatment against a placebo control or a high-intensity drug with a lower-intensity drug.9,10 In contrast, some guidelines – the 2011 ESC/EAS guidelines for the management of dyslipidemias,7 as well as those of the 2014 National Lipid Association27 – support using an LDL-C goal as a target for therapy in ACS patients. This clinical-based study in Thailand demonstrates that achieving an LDL-C goal of <70 mg/dL is associated with a reduction in cardiovascular events, a finding that supports the treating to LDL-C target approach. The findings also highlight that lower LDL-C is associated with better clinical outcomes. Although this is an observational study, the results represent the real-world clinical practice of cardiologists taking care of patients with very high cardiovascular risk.
Interestingly, our findings, which support treating to LDL-C target and the lower the LDL-C the fewer the cardiovascular events, are in line with the recently released results of the study Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT).28–30 This study was conducted in 18,144 patients with post-ACS and conducted over 9 years in 39 countries. It was found that the mean LDL-C at baseline was reduced from 95 mg/dL to 53.2 mg/dL at 1 year in patients receiving ezetimibe 10 mg plus simvastatin 40 mg, compared with 69.9 mg/dL in patients who received simvastatin 40 mg alone. The primary end point – a composite of cardiovascular death, MI, UA requiring rehospitalization, coronary revascularization, or stroke – in the ezetimibe plus simvastatin group was decreased by 6.4% over 7 years when compared with only simvastatin 40 mg (P-value =0.016). Further, our findings are also consistent with the results from three post hoc analyses of data from two RCTs.31–33 A post hoc analysis of the Treating to New Target (TNT) study, where patients were divided into quintiles according to their LDL-C levels, revealed that the patients who attained LDL-C levels <64 mg/dL had the lowest rate of major cardiovascular events (ie, CAD death, nonfatal MI, and stroke).31 The risk was reduced in proportion to reductions in LDL-C levels.31 In a further post hoc analysis from the Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis In Myocardial Infarction 22 (PROVE IT-TIMI 22) study,32 ACS patients were divided by 4-month LDL-C levels into four groups (≤40, >40– 60, >60–80, and >80–100 mg/dL). The two groups with lower LDL-C values (≤40 mg/dL and >40–60 mg/dL groups) had fewer cardiac events (death, MI, stroke, recurrent ischemia, revascularization) when compared with the reference group (>80–100 mg/dL): ≤40 mg/dL, HR=0.61, and >40–60 mg/dL, HR=0.67.32 Another post hoc analysis of the PROVE IT-TIMI 22 study among elderly patients with ACS found that the achievement of LDL-C <70 mg/dL was associated with a 40% relative lower risk of events (acute cardiac clinical events of death, MI, or UA requiring rehospitalization): HR=0.60.33
In addition, an observational study reported by Rallidis et at16 found similar results that LDL-C goal attainment is associated with a reduction in cardiovascular events. Patients at very high risk with stable CAD who achieved an LDL-C goal of <70 mg/dL were less likely to have cardiovascular events (HR=0.34, 95% CI=0.17–0.70; P-value =0.003).16
Our findings underscore the importance of achieving LDL-C target goals for patients at very high risk of cardiovascular events. LDL-C goal attainment is associated with reduced cardiovascular outcomes; therefore, it is essential to continue using LDL-C <70 mg/dL as a target goal for treatment in very high cardiovascular risk patients. Moreover, the treat to target approach is beneficial for a patient-centered approach where physicians and patients discuss treatment objectives and use the treatment goal in order to follow patients’ progress and to maximize long-term adherence to the treatment plan.27 A study in Singapore found that >80% of CAD patients did not know their LDL-C target because of poor, or lack of, communication regarding LDL-C targets between physicians and patients, suggesting that patients may not achieve their treatment targets.34 Besides, many studies show a positive relationship between adherence to taking statins and achieving the LDL-C goal.35–37 However, adherence to statin therapy declines over time; ACS patients had a 2-year adherence rate with statins of about 40%.38 Therefore, discussion with the patient of the importance of achieving and maintaining the LDL-C goal to reduce the risk of a cardiovascular event is vital.
In addition, and similar to previous studies, our findings demonstrate the difficulty in achieving an LDL-C goal of <70 mg/dL in patients with ACS; these patients are at higher risk of further cardiovascular events. Although only 27% of ACS patients in our study achieved LDL-C levels <70 mg/dL, the success rate of patients achieving this goal was higher than in previous studies in Thailand that showed <20% attaining the goal.11,12 The finding is consistent with other studies that found that less than half of patients at very high risk for cardiovascular disease attain the LDL-C target.11–24 Failure to achieve the LDL-C goal in ACS patients is due to some factors as discussed in a previous study,39 such as inadequate lipid therapy,39 health care policy,39,40 or poor adherence to statin therapy.35–37 Since using the treat to target approach can identify ACS patients who fail to attain the LDL-C goal (about three-quarters in this study), these patients can be identified as at greater risk of cardiovascular events; thus, LDL-C goal attainment is essential and also a means for doctors to follow up patients’ progress.
Strengths and limitations
To the best of our knowledge, this study is possibly the first study in Asia to confirm that treating to LDL-C target of <70 mg/dL reduces cardiovascular events in very high cardiovascular risk ACS patients in real-world clinical practice.
However, the present study has some limitations. First, as it is a retrospective study, the results should be interpreted with caution due to possible confounders and lack of some information. Although we attempted to adjust for potential confounders in the statistical methods, residual unknown confounding factors could remain with this study design. No data on statin therapy prior to admission are available in about half of the patients because of various reasons (eg, some patients were referred from other hospitals in northern Thailand without information of statin therapy before their admission). However, all patients received statin therapy on their discharge dates. Second, it may not reflect the situation in other areas in Thailand or other countries because 1) all patients were from a university-affiliated hospital and 2) all patients were managed by cardiologists. Nevertheless, we believe that our finding – treating to LDL-C target of <70 mg/dL decreases cardiovascular events – is applicable for ACS patient management in other countries, because our findings are quite consistent with the IMPROVE IT study, which enrolled ACS patients from 39 countries with different clinical practice patterns as well as social and economic background.28–30 Finally, statin adherence, statin dose titration, and lifestyle therapies such as diet or exercise during treatment may have had an impact on LDL-C goal attainment and cardiovascular outcomes, but these were beyond the scope of our study. However, the effects of statin adherence, statin dose adjustment, and lifestyle therapies on cardiovascular outcomes warrant further analysis.
Conclusion
All in all, ACS patients who received statins and achieved an LDL-C of <70 mg/dL were more likely to have fewer cardiovascular outcomes, confirming the concept “the lower the better”. However, about three-quarters of ACS patients in this study had difficulty achieving the LDL-C target; patients not achieving the LDL-C target are at greater risk of cardiovascular events compared with those achieving the goal. The treating to LDL-C target approach is supported by our finding, the 2011 ESC/EAS guidelines for the management of dyslipidemias,7 and the 2014 National Lipid Association guidelines.27 Thus, the use of the LDL-C goal of <70 mg/dL should be continued for lipid therapy and as a means of communication of patients’ progress between physicians and patients.
Acknowledgments
This study was partially supported by the Graduate School, Chiang Mai University, Thailand. We thank the authorities of the Maharaj Nakorn Chiang Mai Hospital for their permission to use their data. The authors thank Claudia Koller for her assistance with editing this manuscript. Dujrudee Chinwong would like to express her gratitude to the Australian Government for awarding her with a 2014 Endeavour Research Fellowship undertaking at the University of Newcastle, Australia.
Disclosure
The authors report no conflicts of interest in this work.
References
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. | ||
Porapakkham Y, Rao C, Pattaraarchachai J, et al. Estimated causes of death in Thailand, 2005: implications for health policy. Popul Health Metr. 2010;8:14. | ||
Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–1278. | ||
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–239. | ||
Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001;285(13):1711–1718. | ||
Cannon CP, Steinberg BA, Murphy SA, Mega JL, Braunwald E. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48(3):438–445. | ||
Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32(14):1769–1818. | ||
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–2497. | ||
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. | ||
National Institute for Health and Care Excellence. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. London, UK: National Clinical Guideline Centre; 2014. | ||
Silaruks S, Sriratanasathavorn C, Rawdaree P, Kunjara-Na-Ayudhaya R, Thinkhamrop B, Sritara P. Lipid-lowering therapy using statins in patients with cardiovascular risk in clinical practice in Thailand. Heart Asia. 2011;3:99–103. | ||
Sukonthasarn A, Homsanit M, Prommete B, Chotinaiwattarakul C, Piamsomboon C, Likittanasombat K. Lipid-lowering treatment in hypercholesterolemic patients: the CEPHEUS Thailand survey. J Med Assoc Thai. 2011;94(12):1424–1434. | ||
Xanthopoulou I, Davlouros P, Siahos S, Perperis A, Zaharioglou E, Alexopoulos D. First-line treatment patterns and lipid target levels attainment in very high cardiovascular risk outpatients. Lipids Health Dis. 2013;12:170. | ||
Andrikopoulos G, Tzeis S, Nikas N, et al. Short-term outcome and attainment of secondary prevention goals in patients with acute coronary syndrome – results from the countrywide TARGET study. Int J Cardiol. 2013;168(2):922–927. | ||
Kim HS, Wu Y, Lin SJ, et al. Current status of cholesterol goal attainment after statin therapy among patients with hypercholesterolemia in Asian countries and region: the Return on Expenditure Achieved for Lipid Therapy in Asia (REALITY-Asia) study. Curr Med Res Opin. 2008;24(7):1951–1963. | ||
Rallidis LS, Kotakos C, Sourides V, et al. Attainment of optional low-density lipoprotein cholesterol goal of less than 70 mg/dL and impact on prognosis of very high risk stable coronary patients: a 3-year follow-up. Expert Opin Pharmacother. 2011;12(10):1481–1489. | ||
Hermans MP, Castro Cabezas M, Strandberg T, et al. Centralized Pan-European Survey on the Under-treatment of Hypercholesterolaemia (CEPHEUS): overall findings from eight countries. Curr Med Res Opin. 2010;26(2):445–454. | ||
Chin CW, Gao F, Le T, Tan R. Lipid goal attainment and prescription behavior in asian patients with acute coronary syndromes: experience from a tertiary hospital. Clin Med Insights Cardiol. 2013;7:51–57. | ||
Kauffman AB, Olson KL, Youngblood ML, Zadvorny EB, Delate T, Merenich JA. Attainment of low-density lipoprotein cholesterol goals in coronary artery disease. J Clin Lipidol. 2010;4(3):173–180. | ||
Kitkungvan D, Lynn Fillipon NM, Dani SS, Downey BC. Low-density lipoprotein cholesterol target achievement in patients at high risk for coronary heart disease. J Clin Lipidol. 2010;4(4):293–297. | ||
Karalis DG, Victor B, Ahedor L, Liu L. Use of lipid-lowering medications and the likelihood of achieving optimal LDL-cholesterol goals in coronary artery disease patients. Cholesterol. 2012;2012:861924. | ||
Karalis DG, Subramanya RD, Hessen SE, Liu L, Victor MF. Achieving optimal lipid goals in patients with coronary artery disease. Am J Cardiol. 2011;107(6):886–890. | ||
Park JE, Chiang CE, Munawar M, et al. Lipid-lowering treatment in hypercholesterolaemic patients: the CEPHEUS pan-Asian survey. Eur J Prev Cardiol. 2012;19(4):781–794. | ||
Melloni C, Shah BR, Ou FS, et al. Lipid-lowering intensification and low-density lipoprotein cholesterol achievement from hospital admission to 1-year follow-up after an acute coronary syndrome event: results from the Medications ApplIed aNd SusTAINed Over Time (MAINTAIN) registry. Am Heart J. 2010;160(6):1121–1129, 1129.e1. | ||
Ray KK, Kastelein JJ, Boekholdt SM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35(15):960–968. | ||
Lopez-Jimenez F, Simha V, Thomas RJ, et al. A summary and critical assessment of the 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: filling the gaps. Mayo Clin Proc. 2014;89(9):1257–1278. | ||
Jacobson TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: Part 1 – executive summary. J Clin Lipidol. 2014;8(5):473–488. | ||
Cannon CP, Giugliano RP, Blazing MA, et al. Rationale and design of IMPROVE-IT (IMProved Reduction of Outcomes: Vytorin Efficacy International Trial): comparison of ezetimbe/simvastatin versus simvastatin monotherapy on cardiovascular outcomes in patients with acute coronary syndromes. Am Heart J. 2008;156(5):826–832. | ||
Blazing MA, Giugliano RP, Cannon CP, et al. Evaluating cardiovascular event reduction with ezetimibe as an adjunct to simvastatin in 18,144 patients after acute coronary syndromes: final baseline characteristics of the IMPROVE-IT study population. Am Heart J. 2014;168(2):205–212.e1. | ||
O’Riordan M. IMPROVE-IT: ‘Modest’ Benefit When Adding Ezetimibe to Statins in Post-ACS Patients. Medscape Pharmacist Website. Available from: http://www.medscape.com/viewarticle/835030. Accessed February 23, 2015. | ||
LaRosa JC, Grundy SM, Kastelein JJ, Kostis JB, Greten H. Safety and efficacy of Atorvastatin-induced very low-density lipoprotein cholesterol levels in Patients with coronary heart disease (a post hoc analysis of the treating to new targets [TNT] study). Am J Cardiol. 2007;100(5):747–752. | ||
Wiviott SD, Cannon CP, Morrow DA, Ray KK, Pfeffer MA, Braunwald E. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol. 2005;46(8):1411–1416. | ||
Ray KK, Bach RG, Cannon CP, et al. Benefits of achieving the NCEP optional LDL-C goal among elderly patients with ACS. Eur Heart J. 2006;27(19):2310–2316. | ||
Tan NC, Ho SC. Treat-to-target approach in managing modifiable risk factors of patients with coronary heart disease in primary care in Singapore: what are the issues? Asia Pac Fam Med. 2011;10:12. | ||
Parris ES, Lawrence DB, Mohn LA, Long LB. Adherence to statin therapy and LDL cholesterol goal attainment by patients with diabetes and dyslipidemia. Diabetes Care. 2005;28(3):595–599. | ||
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–3035. | ||
Bermingham M, Hayden J, Dawkins I, et al. Prospective analysis of LDL-C goal achievement and self-reported medication adherence among statin users in primary care. Clin Ther. 2011;33(9):1180–1189. | ||
Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288(4):462–467. | ||
Chinwong D, Patumanond J, Chinwong S, et al. Statin therapy in patients with acute coronary syndrome: low-density lipoprotein cholesterol goal attainment and effect of statin potency. Ther Clin Risk Manag. 2015;11:127–136. | ||
Gizurarson S, Bjornsdottir LR, Einarsdottir R, Halldorsson M, Andersen K. Clinical consequences following regulatory changes in respect to reimbursement of statins cost by the Icelandic Social Insurance Administration. Scand J Public Health. 2012;40(7):663–667. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.