Back to Journals » Journal of Asthma and Allergy » Volume 13
Longitudinal Association Between Diet Quality and Asthma Symptoms in Early Adult Life in a Brazilian Birth Cohort
Authors Menezes AMB , Schneider BC , Oliveira VP , Prieto FB , Silva DLR , Lerm BR , da Costa TB , Bouilly R , Wehrmeister FC , Gonçalves H, Assunção MCF
Received 9 May 2020
Accepted for publication 13 August 2020
Published 14 October 2020 Volume 2020:13 Pages 493—503
DOI https://doi.org/10.2147/JAA.S261441
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Ana Maria Baptista Menezes,1 Bruna Celestino Schneider,1 Vânia Pereira Oliveira,1 Fernanda Barros Prieto,1 Deisi Lane Rodrigues Silva,1 Beatriz Raffi Lerm,1 Thielen Borba da Costa,1 Roberta Bouilly,1 Fernando C Wehrmeister,1 Helen Gonçalves,1 Maria Cecília Formoso Assunção1,2
1Epidemiology Postgraduate Program, Federal University of Pelotas, Pelotas, Brazil; 2Public Health Postgraduate Program, Federal University of Rio Grande, Rio Grande, Brazil
Correspondence: Bruna Celestino Schneider
Postgraduate Program in Epidemiology, Federal University of Pelotas, Mal.Deodoro Street, 1160, 3rd Floor, Pelotas CEP: 96020- 220, RS, Brazil
Tel/Fax +55 53 3284 1300
Email [email protected]
Background: The role of diet in the etiology of asthma is still inconclusive. This paper evaluated the longitudinal association between diet quality and chest wheezing in young adults.
Methods: This is a longitudinal study with follow-up information from 18- and 22-year-olds (18y and 22y) of the 1993 Pelotas (Brazil) Birth Cohort. Chest wheezing occurrence and number of events in the last year were reported at 22y. Diet quality was measured with a revised version of the Healthy Eating Index (IQD-R) for the Brazilian population at 18y and 22y by food frequency questionnaire referring to the last 12 months. The diet quality continuity was classified as good (always 1st IQD-R tertile), intermediate (always 2nd tertile/change tertile) and poor (always 3rd tertile).
Results: A total of 2986 young individuals were evaluated; 51.4% were female. Prevalence of wheezing at 22y was 10.1% (95% CI: 9.1– 11.2), and of these patients, 10% reported at least one event in the past year. Better IQD-R score, both at 18y and at 22y, the lower the odds of wheezing in the past year. Regarding the diet quality continuity from 18y to 22y, staying on a poor diet increased by more than three-fold the odds of chest wheezing (OR=3.28; 95% CI: 1.84– 5.84) and of wheezing events (OR=3.32; 95% CI: 1.89– 5.85) compared to staying on a good diet, after adjustment for confounding variables.
Conclusion: The overall quality of the diet seems to be more important than the individual components in the effect on asthma symptoms. Low-quality diet persistence increased the odds of chest wheezing and the number of events.
Keywords: diet, wheezing, asthma, longitudinal studies
Introduction
Chronic wheezing, caused by reversible bronchospasm, is the main characteristic of asthma, a chronic inflammatory disease that affects more than 300 million people worldwide.1 In Brazil, asthma is considered a public health problem, and 4.4% (95% CI: 4.1–4.7)2 of individuals aged 18 years or older, especially women and young adults, reported a medical diagnosis of asthma in a representative sample of the country; in Rio Grande do Sul (RS), this prevalence was approximately 7% (95% CI: 6.8 to 7.2).2
Although asthma is a common chronic disease, its etiology and exacerbation mechanisms are poorly understood.1 The increased prevalence in recent decades has been associated with environmental and behavioral changes,1,3-5 especially changes in dietary habits, with the increase in the consumption of ultra-processed foods together with the decline in the consumption of fruits and vegetables.4,6–9 The role of diet is related to complex mechanisms underlying the modulation of the acquired or innate immune response, and the effect of the diet varies according to the antioxidant and lipid components of foods.7,10
A cross-sectional study conducted in Portugal concluded that asthmatics who consumed at a Mediterranean diet (high consumption of vegetables, legumes, fruits, nuts, whole grains, and unsaturated fatty acids and low meat intake) have reduced risk of exacerbations of the disease.3 In France, a longitudinal study concluded that a good diet is associated with fewer exacerbations and greater asthma control.6
The role of foods and nutrients in the etiology of asthma is still inconclusive, probably due to the complexity of both exposure and disease and therefore their association. It is believed that eating habits are more likely to trigger symptoms rather than to be an etiological factor for the onset of asthma among adults.3 Most studies assess specific foods or nutrients, and few studies evaluate food consumption as a whole. Since foods are not consumed in isolation, but rather in combination, a complete dietary assessment is needed.11
Diet scores have been used to investigate the role of food intake in the prevention of chronic diseases; therefore, the use of diet scores seems to be relevant to the assessment of food intake and exacerbation of asthma symptoms among adults.6 Specific nutrients or food have not been identified as responsible for exacerbations of asthma.7,10 Thus, the analysis of diet scores may provide some information on the simultaneous effects of foods and nutrients in asthma-related wheezing events.
The present study aimed to longitudinally evaluate the association between diet quality and wheezing and the number of events in the past year in young adults from the 1993 Pelotas (Brazil) Birth Cohort.
Methodology
Type of Study and Population
This was a longitudinal study that used data from the 1993 Pelotas (Brazil) Birth Cohort. More details on the method and follow-ups of the 1993 Cohort can be found in other studies.12,13
The original 1993 Cohort consisted of 5249 participants. At 18 years and at 22 years of age, 4106 and 3810 participants were interviewed, respectively. The eligible individuals in this analysis were the participants with valid outcome information at 22 years of age and exposure in the follow-ups at 18 and 22 years of age.
Dependent Variable
Chest wheezing was measured at 22 years of age. Every time a participant reported having had a wheezing in his/her lifetime (answering “Yes” to “Have you ever had wheezing in your chest?”), they were asked “Since <MONTH> of last year, have you had wheezing in your chest?” (No/Yes). The occurrence of wheezing in the last 12 months was also assessed by the question: “Since last year, how many wheezing events did you have?” and the responses were classified into: none event/1 to 3 events/4 to 12 events/more than 12 events. For this study, the categories were categorized as: none event/1 to 3 events/4 or more events.
Revised Brazilian Healthy Eating Index (IQD-R)
IQD-R was used to measure diet quality. For this purpose, data on dietary intake, collected using two digital and self-administered semi-quantitative food frequency questionnaires (FFQ) referring to the last 12 months of consumption, were used. A trained instructor guides the participant on how to fill in, on the computer, the FFQ. At age 18, the instrument consisted of 88 food items, and at age 22, of 92 foods. Only foods present in both instruments, which are available at [http://www.epidemio-ufpel.org.br/site/content/coorte_1993/questionarios.php], were used in the present study.
The IQD-R was constructed from the revised proposal for the Brazilian population of Previdelli et al (2011)14 and adapted for the present study as done by Castilhos et al (2015).15 The score consisted of 10 dietary components, the first seven based on the food groups available in the 2006 Brazilian Dietary Guidelines16 (total grains; milk and dairy products; total fruits; total vegetables; dark-green and orange vegetables; meats, eggs and legumes; oils, oilseeds and fish fat), two nutrient-based components (sodium and saturated fat), and one component on specific dietary items (solid saturated and trans fat, alcohol, and added sugar—called SoFAAS). The score was calculated by summing the scores assigned to all of the components (0 to 10 points), for a maximum total score of 100 points. The higher the IQD-R score, the closer the individual’s diet was to the recommended diet (Table 1).
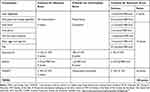 |
Table 1 Score of the Revised Version of the Brazilian Healthy Eating Index (IQD-R) |
To evaluate the longitudinal association between diet quality and wheezing in the past year and the number of wheezing events, the first step was to categorize the IQD-R score (at 18 and 22 years of age) into tertiles. Tertile 1 of the score was represented by individuals with the lowest scores in the index, being classified as having a poor diet. Tertile 2 consisted of individuals with intermediate scores, who were classified as having an intermediate diet. Tertile 3 consisted of participants whose consumption was close to the ideal according to the recommendations, classified as a good diet. Then, diet quality was assessed longitudinally according to three “continuity” categories (how their category changed or not over time) based on the IQD-R tertiles from age 18 to age 22: 1) poor diet, for those who stayed in tertile 1 of the IQD-R score from 18 to 22 years of age; 2) intermediate diet, for those who at 18 years of age were in the 2nd tertile of the IQD-R score and were in this tertile at age 22 or who changed tertiles in any way (from 1st, 2nd, or 3rd to any other tertile); and 3) good diet, for those who stayed in the 3rd tertile of the IQD-R score from 18 to 22 years of age.
Confounding Variables
Besides diet, other independent variables were evaluated at 18 years of age: sex (male/female), skin color (white/black/brown/other), schooling of the participant and of the head of household in years (0–4/5-8/9-11/>12), maternal history of asthma (no/yes), asset index (in quintiles, quintile 1 being the poorest and quintile 5 being the richest), smoking at some point in life (smoking at least once a week—no/yes), alcohol abuse (no/yes) was measured using the Alcohol Use Disorder Identification Test (AUDIT).17 This test evaluates the alcohol consumption pattern in the last 12 months, through 10 items with response alternatives ranging from 1 to 4 points. Higher scores indicate problems; we used the cutoff point >7 points to indicate alcohol abuse according to Babor et al.17,18 Physical activity (insufficiently active: <300 minutes per week/active: ≥300 minutes per week), and body mass index (BMI) by age according to WHO 200719 criteria and classified in low weight/normal 2At 22 years of age, the use of corticosteroids was also investigated—“In the past three months, did you use any corticosteroid or cortisone for allergy or asthma?” (no/yes)—as was the use of an inhaler for relief of wheezing—“How many times have you used an inhaled medication (or inhaler) to relieve wheezing in the last month?”, with the following response options: none, once a week or less, a few times a week, 1 or 2 times a day, and 3 or more times a day (asked only of those who answered “Yes” to inhaler usage).
Statistical Analysis
Statistical analyses were performed using Stata software version 15. In the descriptive analyses, Pearson’s or Fischer’s chi-squared test was performed. Logistic regression was used to assess associations between diet and wheezing, and the relationship between diet and the number of wheezing events was analyzed using ordinal logistic regression. P<0.05 was considered to signify statistically significant risks (as shown by the odds ratio—OR). In the adjusted analysis, the confounding variables were all inserted at the same hierarchical level, and p<0.20 was adopted to keep them in the final model.
Results
Of the 2986 individuals with complete information at both follow-ups, the majority were female (51.4%), white (65.3%), 9 to 11 years of schooling (55.5%), and physically active (60.3%) – Table 2. Approximately 20.0% of the young people reported smoking in their lifetime, and 14.1% of them reported smoking at 18 years of age (Table 1). Table 2 also presents information about the differences between our sample and the number originally at 18 years of age. Our sample has a slight reduction in the proportion of non-white individuals, who studied between 0 and 8 years, the lowest quintile of the goods index and who smoked. The proportion of overweight/obesity was also slightly lower.
 |
Table 2 Characteristics of 1993 Pelotas (Brazil) Birth Cohort Study Participants |
Chest wheezing in the past year was reported by 10.1% (95% CI 9.1–11.2) (n=301) of the study sample, with no statistically significant difference between men and women. Approximately 7.0% reported between one and three wheezing events in the past year, and 3.0% reported four or more (data not shown in Table).
Diet quality was assessed by the median and mean scores of the total IQD-R and its components for the entire sample (n=2986) at 18 and 22 years of age, as shown in Table 3. The mean IQD-R was similar at 18 and 22 years of age (62.0 and 61.3, respectively). The lowest IQD-R score was observed for the “dark-green and orange vegetables” component (3.0 points) at 18 years of age, whereas at 22 years of age, the lowest score was observed for the “fruits” component (1.5 points). In regards to tertiles of diet quality, at 18 years, the mean score in the 1st tertile was 48.9 (SD±6.1), in the 2nd tertile was 62.3 (SD±3.1) and in the 3rd tertile was 75.2 (SD±5.4), whereas at 22 years of age, the mean score was 49.4 (SD±5.0), 61.0 (SD±3.1), and 73.6 (SD±5.2), respectively.
 |
Table 3 Median and Mean of Score Total, Components and Tertiles of Revised Brazilian Healthy Eating Index (IQD-R) at 18 and 22 Years of Age. 1993 Pelotas (Brazil) Birth Cohort. (n=2986) |
The mean score for total IQD-R was lower among participants who reported wheezing in the last year (59.2 [SD±11.5] at age 18 vs 59.1 [SD±10.9] at age 22) (Table 4). The same was observed for the variable “number of wheezing events”, whose mean score decreased as the category increased. The means of each component of the IQD-R were also evaluated according to the report of wheezing in the chest and number of events in the last year, and it was found that the only component of the index related to the outcomes, at both 18 and 22 years of age, was the SoFAAS, which was lower among those who presented wheezing and those with a higher number of wheezing events (Table 4).
Table 5 shows the effect of diet quality at 18 years of age, at 22 years of age, and from 18 to 22 years, along with the occurrence of wheezing and the occurrence of wheezing events in the past year as reported by the 22-year-olds. With each 1-point increase in the total IQD-R, both at 18 and at 22 years, there was a reduction of approximately 13% in the odds of presenting with wheezing and having a higher number of wheezing events, respectively. In the analysis of the tertiles of diet quality, there was a 1.97-fold (95% CI: 1.33–2.91) higher odds of having wheezing among those who had a poor diet (1st tertile) than in those who had a diet considered good (3rd tertile) at 18 years of age, and a 1.98-fold higher odds (95% CI: 1.36–2.87) at age 22. Higher odds of wheezing events in the past year were also found in the young adults with diet quality classified as poor at 18 (OR=2.06; 95% CI: 1.40–3.04) and at 22 years of age (OR=1.97; 95% CI: 1.36–2.85).
Regarding the association between continuity in the same tertile of diet quality and the outcomes studied, it was found that staying on a poor diet from ages 18 and 22 increased the odds of having wheezing by more than three-fold (OR=3.28; 95% CI: 1.84–5.84) when compared to the group that was always on a good diet. Regarding the increase in the number of wheezing events in the past year, it was observed that staying on a poor diet increased by 3.3-fold the odds of a higher number of wheezing events compared with the group who stayed on a good diet (Table 5).
Supplementary materials are available with results on the relationship between quality diet and chest wheezing and events number at 22 years of age stratified by BMI (Supplementary Table 1), smoking status at 18 years of age (Supplementary Table 2) and sensitivity analysis of that association (Supplementary Table 3).
It was observed that among participants with low weight/adequate BMI, a poor diet at 22 years of age or remaining on a poor diet or intermediate diet from age 18 and 22, increased the odds of having chest wheezing by 1.88-fold (95% CI: 1.21–2.90), 2.52-fold (95% CI: 1.30–4.87), respectively - Supplementary Table 1. Among participants with overweight/obesity BMI, a poor diet at 18 or a poor diet at 22 increased the odds of having chest wheezing by 3.33 (95% CI: 1.53–7.25) and 2.15 (95% CI: 1.01–4.59) compared to participants with a good diet, respectively. Remaining on a poor diet from ages 18 and 22 increased the odds of chest wheezing by more than six-fold at 22 years of age. The increase in the wheezing events number (Supplementary Table 1) was significantly associated with a poor diet at 18, at 22 or persistence from 18 to 22 years of age in low weight/adequate BMI and overweight/obesity BMI individuals.
As for smoking status (Supplementary Table 2), it was seen that among nonsmokers, the chance of wheezing at 22 years of age was higher among those who reported a poor diet at 18 (OR=1.74; 95% CI: 1.11–2.72) and at 22 (OR=2.01; 95% CI: 1.30–3.11), in relation to young people with a good diet. In addition, persistence on a poor or intermediate diet increased the odds of wheezing in the chest by approximately 3.5 and 2 times in the last year, respectively. Among smokers, only a poor diet at 18 years of age was associated with higher odds for wheezing at 22 years of age. In relation to the increase in the wheezing events number among non-smokers, it was associated with a poor diet at 18 and 22 years of age, as well as the continuity in it from 18 to 22 (Supplementary Table 2). Among smokers, a poor diet or an intermediate diet only at the age of 18 increased the odds of increasing the number of wheezing events by approximately 3.5 and 2.5 times (Supplementary Table 2).
Additionally, in supplementary material, we show sensitivity analyses about the effect of quality of diet on the effect of the association between quality diet and chest wheezing and events number for participants without the outcome at 18 years of age (Supplementary Table 3). It was noted that a poor diet at 18 or 22 years of age increased the odds of having chest wheezing at 22 by almost twice. The continuity in a poor diet from 18 to 22 years of age increased the odds of having chest wheezing by approximately three times (OR=2.81; 95% CI: 1.46–5.42). Similar effects were observed for the increase in the number of wheezing events in the last year.
Discussion
In this study, diet quality in late adolescence and early adulthood was associated with current symptoms of asthma in young adults. A lower score of the component SoFAAS at 18 and 22 years of age was observed among individuals who reported chest wheezing in the 12 months before the interview and among those who reported a higher number of wheezing events (≥4) in this period. Similarly, persistence at the lowest tertile of the diet quality score (poor diet) increased the odds of reporting chest wheezing and having a higher number of wheezing events in the past year compared to staying at the highest tertile of diet quality (good diet).
Food intake has been shown to be an important modifiable factor in the development and progression of chronic conditions.10,20–22 An unbalanced diet increases the risks of obesity and other health complications, as well as of respiratory problems.20,21,23–25 On this background, the influence of food consumption on the risk of asthma in the various stages of life has been examined in recent decades.21,22
Changes in Brazilian food consumption have been experienced in recent decades. Between 2002/03 and 2017/18 there were stability level of purchase of vegetables and an increase in the levels of purchase of prepared foods.26,27 In parallel, analysis from National Household Sample Survey/PNAD in 2003 and National Health Survey/PNS in 2013 with participants between 18 and 45 years of age showed that the prevalence of self-reported physician diagnosis of asthma increased from 3.6% in 2003 to 4.5% in 2013.2,28
There is evidence that adherence to a Western diet, characterized by a high intake of refined grains, processed foods, red meats, and desserts, and which is rich in (proinflammatory) saturated fats and omega-6 fatty acids, hinders the management of asthma.7,29–31 Conversely, a Mediterranean-like diet, rich in fruits and vegetables which increases the dietary complement of micronutrients, antioxidants (such as carotenoids and flavonoids), and dietary fibers—and in omega-3 fatty acids has been positively correlated with the control of asthma due to its anti-inflammatory effects.7,9,21,32
Despite environmental factors, genetic susceptibility, smoke exposure, indoor and outdoor air pollution have a critical role in asthma pathophysiology the oxidative stress and inflammation are central processes in the clinical manifestation of asthma, and diet might be a key factor in this modulation. Low intake of saturated fat in the diet and high intake of dietary fiber have been associated with low neutrophilic and eosinophilic airway inflammation in individuals with asthma.3,7 A balance in gut microbiota, in particular through an increase in short-chain fatty acids produced by bacteria in the gut during fermentation of insoluble fiber, reduces the airway inflammation.32 A greater intake of dietary fiber is largely due to the consumption of fruits and vegetables.
Guilleminault et al32 conducted a literature review on the relationship between diet and asthma symptoms and concluded that a higher intake of fruits and vegetables is a protective factor for the development of asthma, especially in children. A meta-analysis33 found that fruit intake was inversely associated with chest wheezing and asthma, with relative risks (RRs) of 0.81 (95% CI: 0.74–0.88) and 0.90 (95% CI: 0.86–0.94), respectively. Vegetable intake was also inversely associated with those outcomes: RR=0.88 (95% CI: 0.79–0.97) and RR=0.91 (95% CI: 0.82–1.00), respectively. In the present study, no relationship was found between the mean score of the components “fruits”, “total vegetables”, and “dark-green and orange vegetables” at 18 and 22 years of age and the report of wheezing in the past year at 22 years of age.
In the present study, the component SoFAAS showed lower means at 18 and at 22 years among the young people who reported wheezing in the past year and among those who reported a larger number of wheezing events (≥4) in this period. This finding agrees with previous literature. Park et al30 analyzed the data from the 2013 Behavioral Risk Factor Surveillance System for 146,990 adults (≥18 years of age) in the United Kingdom and found that the odds of having current asthma were higher among those who consumed sugary drinks ≥2 times/day (OR=1.66; 95% CI: 1.39–1.99) than those who did not consume them. Excessive consumption of foods rich in fats and simple sugars, associated with insufficient physical activity, leads to increased body weight. A study in the same birth cohort of Pelotas found that being obese or belonging to the highest tertile of adiposity at two time-points showed a cumulative positive association with chest wheezing. Being in the highest tertile of total fat mass percentage at both follow-ups (measured by dual-energy X-ray absorptiometry) conferred an OR of 1.58 (95% CI: 1.14–2.20) for wheezing, and it conferred an OR of 1.16 (95% CI: 0.92–1.47) for atopy.34
The Global Initiative for Asthma Guidelines1 includes among its recommendations a healthy diet for the primary prevention of asthma. Many studies have focused on the effects of individual foods or nutrients on respiratory outcomes.9,22,31,32,35 However, this information may not fully capture the overall effect of diet on respiratory health or reflect real-life conditions, where foods or nutrients are consumed in various combinations. According to Varraso et al,3 dietary components only have an effect on asthma in the context of the overall diet because foods are consumed in complex combinations, which include various nutrients and bioactive substances that interact with each other and influence each other’s bioavailability and absorption. People consume a variety of foods and food groups in a meal instead of individual nutrients or food groups.20,32
In this context, the diet quality scores are based on the existing nutritional knowledge and have been proposed to evaluate the overall quality of the diet, providing a quantitative measure that takes into account the synergistic effects between nutrients and foods consumed. Similar to the present study, the NutriNet-Santé cohort study in France6 with 34,766 French adults found that the highest scores in the Alternate Healthy Eating Index-2010, the Literature-based Adherence Score to Mediterranean Diet, and the modified Program National Nutrition Santé Guideline Score were associated with a lower score of asthma symptoms.
Additionally, because the overall quality of the diet seems to be more important than the individual components, keeping up a given diet quality had a significant impact in this study, as the exposure to a low-quality diet over time increased the odds of the participant having wheezing symptoms and recurrence.
To date, few epidemiological studies have been conducted on the association between overall diet scores and the diagnosis of asthma/wheezing in adults, and the level of evidence on this topic is still low. The heterogeneity of dietary assessment between studies hinders the production of strong and consistent evidence. Longitudinal information on the type of dietary exposure that young people experience at the beginning of adulthood is a strength of this study; we were able to assess the exact same information at both time points, using a food frequency questionnaire, which despite being the most frequently used method in epidemiological studies is susceptible to errors (daily variations in food intake, recall bias, the semi-quantitative nature of the evaluation, etc.).
Furthermore, although we have adjusted our statistical model for many factors, including the socioeconomic, we do not measure environmental factors that may increase the chance of triggering asthma symptoms such as live in poor areas with high densities of people or of roadways – that increase pollution air; working conditions and housing for individuals – that can increase contact with allergenic agents.
Conclusion
Better diet quality was longitudinally associated with a lower occurrence of wheezing and of the number of wheezing events in the 12 months before the interview. Staying on a good diet reduced the occurrence of exacerbations/events of wheezing, while staying on a poor diet increased the odds of having wheezing and the number of wheezing events.
Given the high prevalence of asthma and its effect on individuals and society, it is necessary to identify interventions that can be used to complement conventional therapy and, more importantly, interventions to reduce the likelihood of asthma complications. Dietary interventions, consisting mostly of the encouragement of healthier eating and lifestyle habits based on current guidelines, should be incorporated into the routine clinical management of patients with asthma to achieve general benefits for health and management of the disease. Longitudinal studies should analyze dietary aspects to better understand the mechanisms involved in the relationship between diet and the occurrence of asthma and its complications.
Ethics and Consent Statement
All the follow-ups of the Pelotas (Brazil) Birth Cohorts were submitted to and approved by the Ethics Committee of the School of Medicine of the Federal University of Pelotas, and the process number of the follow-ups at 18 and 22 years of age were 5/11 and 1.250.366, respectively. Individuals who agreed to participate signed an informed consent form. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The 1993 Birth Cohort study is currently supported by the Wellcome Trust through the programme entitled Major Awards for Latin America on Health Consequences of Population Change. The European Union, National Support Program for Centers of Excellence (PRONEX), the Brazilian National Research Council (CNPq), the Foundation for Research Support of the State of Rio Grande do Sul (FAPERGS), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES – Finance Code 001), and the Brazilian Ministry of Health supported phases of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Ana Maria Baptista Menezes reports personal fees from AstraZeneca, outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
1. Gina. ATER, Global D. Strategy for asthma management and prevention is AT ER - D. Glob strateg asthma manag prev [internet]; 2018. 32. Available from: https://ginasthma.org/wp-content/uploads/2018/04/wms-GINA-2018-report-tracked_v1.3.pdf.
2. Menezes AMB, Wehrmeister FC, Horta B, Szwarcwald CL, Vieira ML, Malta DC. Prevalência de diagnóstico médico de asma em adultos brasileiros: pesquisa nacional de saúde, 2013. Rev Bras Epidemiol. 2015;18:204–213. doi:10.1590/1980-5497201500060018
3. Varraso R, Camargo CA. Can dietary interventions improve asthma control? Prim Care Respir J [Internet]. 2012;21(4):367–368. doi:10.4104/pcrj.2012.00095.
4. Li Z, Kesse-Guyot E, Dumas O, et al. Longitudinal study of diet quality and change in asthma symptoms in adults, according to smoking status. Br J Nutr [Internet]. 2017;117(4):562–571. doi:10.1017/S0007114517000368
5. Lieberoth S, Backer V, Kyvik KO, et al. Intake of alcohol and risk of adult-onset asthma. Respir Med [Internet]. 2012;106(2):184–188. doi:10.1016/j.rmed.2011.11.004
6. Andrianasolo RM, Kesse-Guyot E, Adjibade M, Hercberg S, Galan P, Varraso R. Associations between dietary scores with asthma symptoms and asthma control in adults. Eur Respir J [Internet]. 2018;52(1):1702572. doi:10.1183/13993003.02572-2017.
7. Han -Y-Y, Forno E, Holguin F, Celedón JC. Diet and asthma. Curr Opin Allergy Clin Immunol [Internet]. 2015;15(4):369–374. doi:10.1097/ACI.0000000000000179.
8. Garcia-Larsen V, Del Giacco SR, Moreira A, et al. Asthma and dietary intake: an overview of systematic reviews. Allergy [Internet]. 2016;71(4):433–442.
9. Hosseini B, Berthon BS, Wark P, Wood LG. Effects of fruit and vegetable consumption on risk of asthma, wheezing and immune responses: a systematic review and meta-analysis. Nutrients [Internet]. 2017;9(4):341. doi:10.3390/nu9040341.
10. Scoditti E, Massaro M, Garbarino S, Toraldo DM. Role of diet in chronic obstructive pulmonary disease prevention and treatment. Nutrients [Internet]. 2019;11(6):1357. doi:10.3390/nu11061357.
11. Fisberg RM, Slater B, Barros RR, et al. Índice de qualidade da dieta: avaliação da adaptação e aplicabilidade. Rev Nutr [Internet]. 2004;17(3):301–318. doi:10.1590/S1415-52732004000300003
12. Gonçalves H, Assunção MC, Wehrmeister FC, et al. Cohort profile update: the 1993 pelotas (Brazil) birth cohort follow-up visits in adolescence. Int J Epidemiol. 2014;43(4): 1082–1088.
13. Gonçalves H, Wehrmeister FC, Assunção MCF, et al. Cohort Profile Update: The 1993 Pelotas (Brazil) Birth Cohort follow-up at 22 years. Int J Epidemiol. 2018;47(5):1389–1390e. doi:10.1093/ije/dyx249
14. Previdelli ÁN, Andrade SCD, Pires MM, Ferreira SRG, Fisberg RM, Marchioni DM. Índice de qualidade da dieta revisado para população brasileira. Rev Saude Publica [Internet]. 2011;45(4):794–798. doi:10.1590/S0034-89102011000400021.
15. Castilhos CBD, Schneider BC, Muniz LC, Assunção MCF. Qualidade da dieta de jovens aos 18 anos de idade, pertencentes à coorte de nascimentos de 1993 da cidade de Pelotas (RS), Brasil. Cien Saude Colet [Internet]. 2015;20(11):3309–3318. doi:10.1590/1413-812320152011.17822014.
16. BRASIL. Ministério da Saúde. Guia alimentar para a população brasileira: promovendo a alimentação saudável. Brasília: Ministério da Saúde, 2006. 210p. (Série A. Normas e Manuais Técnicos). Disponível em: http://nutricao.saude.gov.br/docs/geral/guia_alimentar_conteudo.pdf.
17. Saunders JB, Aasland OG, TF Babor, DE LA FUENTE JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804.
18. Lawford BR, Barnes M, Connor JP, Heslop K, Nyst P, Young RMD. Alcohol use disorders identification test (AUDIT) scores are elevated in antipsychotic-induced hyperprolactinaemia. J Psychopharmacol. 2012;26(2):324–329. doi:10.1177/0269881110393051
19. de Onis M. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ [Internet]. 2007;85(09):660–667. doi:10.2471/BLT.07.043497.
20. Wood LG. Diet, obesity, and asthma. Ann Am Thorac Soc. 2017;14(Supplement_5):S332–8.
21. Forte GC, da Silva DTR, Hennemann ML, Sarmento RA, Almeida JC, de Tarso Roth DP. Diet effects in the asthma treatment: a systematic review. Crit Rev Food Sci Nutr. 2018;58(11):1878–1887.
22. Fogarty B. The role of diet in the aetiology of asthma. Clin <html_ent Glyph=“@amp;” Ascii=“&”/> Exp Allergy. 2000;30(5):615–627.
23. Varraso R, Camargo CA. Diet and asthma: need to account for asthma type and level of prevention. Expert Rev Respir Med. 2016;10(11):1147–1150.
24. Oliveira PDD, Wehrmeister FC, Pérez-Padilla R, et al. Relationship between body composition and pulmonary function in early adult life: a cross-sectional analysis nested in two birth cohort studies. schooling CM, editor. PLoS One. 2016;11(9): e0163428.
25. Noal RB, Menezes AMB, Macedo SEC, et al. Is obesity a risk factor for wheezing among adolescents? A prospective study in Southern Brazil. J Adolesc Heal [Internet]. 2012;51(6):S38–45. doi:10.1016/j.jadohealth.2012.08.016
26. Canella DS, Louzada MLDC, Claro RM, et al. Consumo de hortaliças e sua relação com os alimentos ultraprocessados no Brasil. Revista De Saúde Pública. 2018;52:50. doi:10.11606/S1518-8787.2018052000111
27. Inácio L, Ibge E, Côrtes C, Tai DW. Pesquisa de orçamentos familiares 2017–2018 - primeiros resultados [internet]. vol. 46. Am J Cardiol. 2003;Available from:, 983–987. http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Pesquisa+de+Or?amentos+Familiares#0.
28. Santos FMD, Viana KP, Saturnino LT, et al. Trend of self-reported asthma prevalence in Brazil from 2003 to 2013 in adults and factors associated with prevalence. J Bras Pneumol [Internet]. 2018;44(6):491–497. doi:10.1590/s1806-37562017000000328
29. Thorburn AN, Macia L, Mackay CR. Diet, metabolites, and “western-lifestyle” inflammatory diseases. Immunity [Internet]. 2014;40(6):833–842. doi:10.1016/j.immuni.2014.05.014.
30. Park S, Akinbami LJ, McGuire LC, Blanck HM. Association of sugar-sweetened beverage intake frequency and asthma among U.S. adults, 2013. Prev Med [Internet]. 2016;91:58–61. doi:10.1016/j.ypmed.2016.08.004
31. Litonjua AA. Dietary factors and the development of asthma. Immunol Allergy Clin North Am [Internet]. 2008;28(3):603–629. doi:10.1016/j.iac.2008.03.005.
32. Guilleminault L, Williams E, Scott H, Berthon B, Jensen M, Wood L. Diet and asthma: is it time to adapt our message? Nutrients [Internet]. 2017;9(11):1227. doi:10.3390/nu9111227.
33. Seyedrezazadeh E, Pour Moghaddam M, Ansarin K, Reza Vafa M, Sharma S, Kolahdooz F. Fruit and vegetable intake and risk of wheezing and asthma: a systematic review and meta-analysis. Nutr Rev. 2014;72(7):411–428.
34. Baptista Menezes AM, de Oliveira PD, Blumenberg C, et al. Longitudinal association of adiposity with wheezing and atopy at 22 years: the 1993 Birth Cohort, Pelotas, Brazil. J Asthma Allergy [Internet]. 2018;11:283–291. doi:10.2147/JAA.S183699
35. Allan K, Devereux G. Diet and asthma: nutrition implications from prevention to treatment. J Am Diet Assoc [Internet]. 2011;111(2):258–268. doi:10.1016/j.jada.2010.10.048.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


