Back to Journals » Clinical Ophthalmology » Volume 15
Long-Term Suture Breakage After Scleral Fixation of a Modified Capsular Tension Ring with Polypropylene 10-0 Suture
Authors Kristianslund O , Sandvik GF, Drolsum L
Received 11 March 2021
Accepted for publication 23 April 2021
Published 14 June 2021 Volume 2021:15 Pages 2473—2479
DOI https://doi.org/10.2147/OPTH.S310648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Olav Kristianslund, Gunhild F Sandvik, Liv Drolsum
Department of Ophthalmology, Oslo University Hospital and Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Correspondence: Olav Kristianslund
Department of Ophthalmology, Oslo University Hospital and Institute of Clinical Medicine, Mailbox 4956 Nydalen, Oslo, 0424, Norway
Email [email protected]
Aim: To investigate the long-term risk of suture breakage after implantation of a modified capsular tension ring (MCTR) fixated to the sclera with polypropylene 10– 0 suture.
Methods: Retrospective case series of operations for subluxated phakic lenses in 2007– 2015 with implantation of an MCTR secured with a 10– 0 polypropylene suture as part of an intraocular lens (IOL)-capsular bag complex.
Results: We identified 132 eyes (92 patients) operated on with an MCTR. Of these eyes, 26 (20%) had suture breakage requiring re-operation, while another eight eyes (6%) had suture breakage that did not require surgery. The re-operations occurred after a mean 4.8± 3.3 years. Suture breakage occurred in patients with a mean age of 34.0± 23.3, as compared to 43.2± 26.0 years for patients who did not experience this complication (p=0.36). In patients aged 40 years or younger at the time of surgery, 47% experienced suture breakage in one or both eyes, as compared to 19% in the age group 41– 69 years and 13% in the age group 70 years and older (p=0.004). Of the 132 eyes that were operated on, we registered one case (0.8%) of possible suture-related late endophthalmitis.
Conclusion: The long-term risk of suture breakage was quite high after scleral fixation of the MCTR in this patient cohort, and it seems as the risk is increased with young age.
Keywords: modified capsular tension ring, MCTR, Cionni capsular tension ring, suture breakage, Marfan syndrome, ectopia lentis, subluxated lens, scleral suturing
Introduction
Ectopia lentis is an ocular condition associated with Marfan syndrome and some other genetic abnormalities.1,2 Lens surgery in these eyes is complicated by abnormal zonular strands and insufficient capsule support. In such cases, a modified capsular tension ring (MCTR) is used by several surgeons for fixating the capsule with one or two sutures to the sclera.3–6 This alternative may also be a viable option in eyes with a loose biological lens related to trauma or pseudoexfoliation syndrome.
One of the main disadvantages with scleral suturing is the risk of long-term complications. Several studies have described the occurrence of suture erosions and breakage;6–14 a few studies have reported rates as high as 18–28%.13,15,16 Some studies have also mentioned the risk of loosening of the knot.17 Often, the 10–0 polypropylene suture has been used for scleral fixation. However, due to the described risk of suture breakage, some authors have recommended 9–0 polypropylene or Gore-Tex instead.9,17
High rates of suture breakage have mainly been reported with fixation of only the IOL (not the capsule), and it further seems to occur particularly in younger patients.9,14,15 In a retrospective study by Cionni et al,4 suture breakage was identified in 10% of the eyes after scleral suturing of a Cionni MCTR with 10–0 polypropylene suture, of whom 7% were symptomatic. That study had a mean follow-up of 14.6 months. A review by Li et al6 of surgical implantation of MCTRs identified 10 case series with a mean follow-up from 12.9 to 48 months for a total of only 320 eyes. Studies with long follow-up after scleral suturing of a Cionni MCTR with 10–0 suture seem to be limited. Furthermore, there is a need for large samples to identify whether certain factors such as age may affect the risk of long-term complications.
We have applied the scleral fixation technique with 10–0 polypropylene suture for fixation of the MCTR in ectopia lentis/loose lens surgery for a longer time now. Our clinical experience is that the risk of suture breakage after this surgery is quite high, especially in younger patients. In this study, we searched for all eligible patients operated on up until 2015, to be able to have a follow-up of at least five years. The main aim was to examine the risk of suture breakage in eyes with scleral suturing of the MCTR and, secondarily, to identify the risk of late endophthalmitis.
Materials and Methods
In this retrospective study, we included patients operated on with scleral suturing of an MCTR in the period 2007–2015. All operations were performed at the Department of Ophthalmology at Oslo University Hospital. Data was obtained from medical records. This quality study was approved by the data protection officer and the local ethical committee at Oslo University Hospital, which waived the need for written informed consent and Regional Ethical Committee approval. The research adhered to the Declaration of Helsinki.
Patients were operated by one of two experienced surgeons (42% and 58%, respectively). A clear corneal incision was made, a viscoelasticum was applied and a manual continuous curvilinear capsulorhexis (CCC) was performed with forceps. Thereafter, iris hooks (usually five) were placed at the anterior capsule edge to stabilize the lens, and gentle hydrodissection and phacoemulsification with low infusion and careful aspiration was conducted. In children and young adults, the lens was removed with inspiration/aspiration only. Then, the conjunctiva was opened by scissors at the intended placement for the scleral suture. One of the surgeons also created a triangular scleral flap. All operations were performed with a Cionni MCTR 1L or 2C (Morcher GMBH, Stuttgart, Germany) with one eyelet and a diameter of 13 mm, and double-armed 10–0 polypropylene sutures (Prolene, Ethicon, New Jersey, US) placed through the eyelet outside the eye. First, the MCTR was implanted through the main incision into the capsular bag, and the eyelet was resting on the anterior surface of the CCC, followed by implantation of the IOL in the capsular bag. Then the first needle was introduced through the main incision into a 27-gauge cannula introduced through the scleral wall at the opposite site, and these were retracted out of the eye, followed by the same procedure for the other needle, creating a suture loop through the MCTR eyelet that was tightened with a knot outside the eye (placed underneath a scleral flap or rotated). Viscoelasticum was removed and intracameral antibiotics were applied.
A study period from 2007 was chosen because this was the year that the technique was introduced on a routine basis. By including patients until 2015, we assured at least five years of follow-up to January 2021 (or until the patient was deceased, which applied to a few patients). Patients were followed in our clinic, in the local eye department or by their private ophthalmologist, with the frequency depending on factors such as the cause of ectopia lentis, ocular comorbidity and age. As this is a tertiary referral clinic, we assumed that all the patients with suture breakage or suture-related late endophthalmitis operated on in our department were referred for treatment. Data on age, gender, and known reasons for a loose crystalline lens were also gathered.
The results are presented as mean ± standard deviation (range), calculated in SPSS (version 26, IBM Corp., Armonk, NY, USA). Mean age for patients with or without suture breakage was compared with independent samples t-test. The proportion of patients with suture breakage in one or both eyes in different age groups was compared with chi-square test (linear-by-linear association for trends). Age limits were defined as below 40 years, representing an age at which lens surgery is uncommon, and above 70 years, representing the cataract surgery population. A Kaplan-Meier plot was used to show the cumulative probability of suture breakage during the follow-up after implantation of the CTR. A p value of < 0.05 was considered statistically significant.
Results
This study included 132 eyes (92 patients) with implantation of the MCTR by scleral suturing in the period 2007–2015. The patients had a mean age of 40.8 ± 25.5 years at the time of the operation, and 59% were men. Of the patients operated on, 31 (34%) were diagnosed with Marfan syndrome according to the Ghent 2 criteria;18 18 (20%) had trauma as the assumed cause; six (7%) had pronounced pseudoexfoliation syndrome; five (6%) had congenital ectopia lentis, while the remaining patients were suspected to have Marfan syndrome, had an association with other syndromes, or the cause was unknown. Mean follow-up in all eyes was 9.3 ± 2.8 (3.5–13.5) years, and 62 eyes (47%) had follow-up of at least 10 years.
Altogether, 26 of the 132 eyes (20%) suffered from suture breakage that required a re-operation during the follow-up period. In addition, eight eyes (6%) had recognised suture breakage that had not been operated. The mean time until the re-operation was 4.8 ± 3.3 (1–12) years. A Kaplan-Meier plot is shown in Figure 1. Patients with suture breakage (n = 34) had a mean age of 34.0 ± 23.3 years versus 43.2 ± 26.0 years for those without this complication (p = 0.36). In patients aged 40 years or younger at the time of surgery, 47% experienced suture breakage in one or both eyes, as compared to 19% in the age group 41–69 years and 13% in the age group of 70 years and older (p = 0.004), as shown in more detail in Table 1. Thirteen (42%) of the Marfan syndrome patients experienced suture breakage, while this applied to one (6%) of the traumatic patients, one (17%) with pronounced pseudoexfoliation syndrome, one (20%) with congenital ectopia lentis, and 13 (41%) of the remaining patients. The suture breakage rate was similar for the two surgeons; 27% and 25%, respectively.
 |
Table 1 Suture Breakage* in Patients in Different Age Groups |
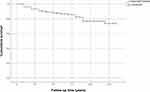 |
Figure 1 Cumulative probability of suture breakage after an operation with scleral suturing of a modified capsular tension ring: 132 eyes. The x-axis shows time of follow-up in years from surgery. |
One eye (0.8%) suffered from late endophthalmitis possibly related to suture exposure.
Discussion
Scleral suturing is a popular surgical technique used for several indications. Alternative fixation methods, including sutureless techniques, have increased in popularity in recent years. However, these are not suitable for all indications, such as when aiming for implantation of an IOL in the capsular bag in eyes with ectopia lentis that requires fixation, eg, of the MCTR. Hence, scleral suturing remains as an important technique that is still widely used. However, a main concern is the risk of suture breakage, especially with the 10–0 polypropylene suture. Based on results from previous studies, we speculated that this risk is highest in younger patients, which constitute a large portion of the group receiving the MCTR. In the present study, we found a suture breakage rate of 26% over the longer term after implantation of the MCTR. There was a trend towards a higher proportion in the younger age group.
Dislocated crystalline lenses occur in various conditions, of whom Marfan syndrome being prominent. In our department, these eyes have often been operated on with scleral suturing of a Cionni MCTR for fixation of an IOL implanted inside the capsule, as also described by several others.3,19 For many years, 10–0 polypropylene sutures have been used.6,20 However there have been controversies regarding this use, and some have claimed that the risk for suture breakage is too high. Rather, they have recommended using 9–0 polypropylene or Gore-Tex sutures,9,17 which are assumed to be less vulnerable to this complication due to their increased tensile strength. Nevertheless, thicker sutures may be more challenging in intraocular eye surgery.21 In addition, the availability of the Gore-Tex suture varies (off-label use),22 and neither these sutures are without complications,23 although the risk of suture breakage is possibly lower.6 Also, it has been speculated that this risk depends on the condition being treated as well as the patient characteristics–not least the patient’s age.14 Suture degradation has been suggested as part of the reason for the higher rates of breakage in younger age groups.6,23,24 In addition, whether the suture also passes through the lens capsule seems to be a relevant factor that may affect the risk.7,12
In a prospective trial of late in-the-bag IOL dislocation surgery, we found a re-dislocation risk of 3% in the two-year period after scleral suturing using 10–0 polypropylene.7,12 These patients had a mean age of more than 80 years, and the scleral suture loops around the IOL haptics were secured by the lens capsule. We hypothesize that these two factors are preventive in terms of suture breakage. A possible explanation is that the capsule prevents both suture slippage and direct friction between the suture and the (sharp) haptic edge in patients with late in-the-bag IOL dislocation, and that suture degradation is rare in the elderly. Nevertheless, an even longer follow-up on eyes with late in-the-bag IOL dislocation is preferable.
Based on our clinical experience, we have suspected that a considerable proportion of MCTRs fixated to the sclera with a 10–0 polypropylene suture suffer from suture breakage after some years. This has also been indicated in the literature,4 and would be in accordance with scleral suture fixation of the IOL without surrounding capsule.15 For scleral fixation of MCTRs with 10–0 polypropylene, Cionni et al4 found suture breakage in 10% of cases after a mean follow-up of 14.6 months. A review of MCTRs by Li et al6 identified 10 case series with a mean follow-up from 12.9 to 48 months (320 eyes altogether), reporting a total of 11 cases (3%) requiring re-suturing; nine after 10–0 suture and two after 9–0 suture. The review identified a lack of large studies with long follow-up, and further pointed out the heterogeneity between studies. The present study revealed that 26% of scleral-sutured MCTRs had suture breakage after some years (re-operations after 4.8 years on average). This is a high frequency, especially since many of these patients are young and thus expected to live with their IOL/CTR complex for many years. Following our clinical suspicions, we changed the routine some years ago to use the 9–0 suture in young patients. However, this is mainly later than the time period of the operations included in the present study. Future studies will hopefully show whether the use of 9–0 or Gore-tex sutures will decrease the risk of suture breakage, or at least prolong the time period until this adverse event occurs.22
The mean age was not significantly different between the patients with and without suture breakage in the present study, although we found a tendency, and there was a significant trend towards a higher proportion of suture breakage in the youngest age group. It has been hypothesized that young age is a risk factor for suture degradation.6,23,24 Another factor in younger patients that may increase the suture-related risk is a high activity level, which may result in more force against the suture.23 Furthermore, most of these patients have a long life expectancy, hence, a long-lasting surgical option is important. In contrast, the scleral fixation group in our previous trial of late in-the-bag IOL dislocation had an average remaining life expectancy of approximately six years.7,12,25 Different rates of suture breakage in various age groups may also be related to the underlying etiology for ectopia lentis.
Altogether, a third of the patients in the present study had a verified diagnosis of Marfan syndrome. A previous review of scleral suturing of MCTRs reported that 40% of the patients had Marfan syndrome, although there was heterogeneity between studies.6 Ectopia lentis is known to occur in about 60% of patients diagnosed with Marfan syndrome.1,26 The lens typically dislocates in the supero-temporal direction, stretching the inferior zonules. Ectopia lentis is usually seen from childhood, but it can also progress in adults.27,28 It often requires surgical treatment, and since the zonules are weakened, suture-fixated MCTR is usually recommended, if possible to retain the lens capsule for in-the-bag IOL placement.20 In the eyes of the Marfan patients in our study, the suture breakage rate was 42%.
Treatment of suture breakage was in most cases performed as surgical repositioning with suture re-fixation, which has been described by others as a suitable approach.29 This may be performed with a new suture through the eyelet of the MCTR, or with one or two suture loops 180 degrees apart through the capsule and around the IOL haptics and the MCTR. Using two sutures is similar as we perform repositioning surgery for late in-the-bag IOL dislocation surgery.12 Another possible option is explantation of the IOL/MCTR-complex, with implantation of a new lens fixated to the sclera or the iris. In older patients with late in-the-bag IOL dislocation, iris-claw has been shown as a safe and effective treatment option compared to repositioning by scleral suturing.7,12 However, in patients with Marfan syndrome, iridodonesis may be a concern, and thus one could argue that scleral fixation may be a better option. Marfan and pseudoexfoliation syndrome eyes may also have poor mydriasis, increasing the risk for traumatic iris damage when explanting a dislocated complex.
Another feared complication after scleral suturing is late endophthalmitis, which may have serious visual consequences. Although this complication has been described in a few case reports,30,31 it seems to be very rare,7 at least based on the existing literature. However, there seems to be a lack of comprehensive evaluations of this complication. In the present study, which had a mean follow-up of 9.3 years, one case (0.8%) of endophthalmitis occurred that were possibly related to the scleral suture. Due to the retrospective nature of the study, there may have been cases that were not registered. One may hypothesize that thicker sutures, such as 9–0 polypropylene or Gore-Tex, may increase the risk of late endophthalmitis, possibly by creating a canal in the scleral wall. However, comparisons of the risks associated with different types of sutures for scleral fixation remain to be performed.
As this was a retrospective quality study, we did not have detailed clinical data on all patients, which is a limitation. Furthermore, we did not follow all patients in our department, as many belonged to other local hospitals or private practicing ophthalmologists. However, our clinic has the main responsibility for more advanced surgery in this patient group, covering the largest health region in Norway, and in this study, we assumed that the vast majority of re-dislocations or other serious complications such as late endophthalmitis were referred to our clinic for treatment. Nevertheless, there may be patients with suture breakage who have not been operated on (so far) because of a more-or-less stable IOL and no serious visual deterioration, or that were not identified due to the lack of systematic follow-up. Thus, the true risk of suture breakage is probably even higher than what we have presented in this study.
Clinical implications from the present study are that the 10–0 polypropylene suture is associated with a significant risk of suture breakage in the long term when used for fixation of the MCTR, and there is a tendency for an even higher risk in the younger patients possibly related to the underlying etiology for ectopia lentis. This may be in contrast to the patient group of elderly with late in-the-bag IOL dislocation, in which 10–0 polypropylene seems to be an acceptable option for scleral suturing of the whole complex, including the capsule, at least within the perspective of a few years.7,12 However, long-term results for this latter group are lacking.
In conclusion, this study showed a quite high rate of suture breakage in the long term after scleral fixation of the MCTR with polypropylene 10–0 suture. Therefore, 9–0 polypropylene or Gore-Tex sutures should be considered for this type of surgery, at least in younger patients. Future studies can discover whether these options reduce the risk of suture breakage and are sufficient in a life time perspective, or if other methods should be chosen for primary surgery.
Abbreviations
MCTR, modified capsular tension ring; IOL, intraocular lens.
Funding
This study has received no financial support.
Disclosure
Sandvik has received a Ph.D. grant from the Norwegian Dam Foundation, Oslo, Norway. Dr Kristianslund has received a small presentation fee at a seminar about cataract surgery/IOL dislocations, arranged by Bausch&Lomb (Sept.2020), outside the submitted work. No other conflicting relationship exists for all authors and no author has any proprietary or commercial interest in any materials discussed in this article.
References
1. Maumenee IH. The eye in the Marfan syndrome. Trans Am Ophthalmol Soc. 1981;79:684–733.
2. Sadiq MA, Vanderveen D. Genetics of ectopia lentis. Semin Ophthalmol. 2013;28(5–6):313–320. doi:10.3109/08820538.2013.825276
3. Ahmed II, Crandall AS. Ab externo scleral fixation of the Cionni modified capsular tension ring. J Cataract Refract Surg. 2001;27(7):977–981. doi:10.1016/S0886-3350(01)00924-5
4. Cionni RJ, Osher RH, Marques DM, Marques FF, Snyder ME, Shapiro S. Modified capsular tension ring for patients with congenital loss of zonular support. J Cataract Refract Surg. 2003;29(9):1668–1673. doi:10.1016/S0886-3350(03)00238-4
5. Cionni RJ, Osher RH. Management of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixation. J Cataract Refract Surg. 1998;24(10):1299–1306. doi:10.1016/S0886-3350(98)80218-6
6. Li B, Wang Y, Malvankar-Mehta MS, Hutnik CM. Surgical indications, outcomes, and complications with the use of a modified capsular tension ring during cataract surgery. J Cataract Refract Surg. 2016;42(11):1642–1648. doi:10.1016/j.jcrs.2016.10.007
7. Dalby M, Kristianslund O, Drolsum L. Long-term outcomes after surgery for late in-the-bag intraocular lens dislocation: a randomized clinical trial. Am J Ophthalmol. 2019;207:184–194. doi:10.1016/j.ajo.2019.05.030
8. Jakobsson G, Zetterberg M, Sundelin K, Stenevi U. Surgical repositioning of intraocular lenses after late dislocation: complications, effect on intraocular pressure, and visual outcomes. J Cataract Refract Surg. 2013;39(12):1879–1885. doi:10.1016/j.jcrs.2013.06.023
9. Price MO, Price FW, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31(7):1320–1326. doi:10.1016/j.jcrs.2004.12.060
10. Dimopoulos S, Dimopoulos V, Blumenstock G, et al. Long-term outcome of scleral-fixated posterior chamber intraocular lens implantation with the knotless Z-suture technique. J Cataract Refract Surg. 2018;44(2):182–185. doi:10.1016/j.jcrs.2017.11.009
11. Kokame GT, Yanagihara RT, Shantha JG, Kaneko KN. Long-term outcome of pars plana vitrectomy and sutured scleral-fixated posterior chamber intraocular lens implantation or repositioning. Am J Ophthalmol. 2018;189:10–16. doi:10.1016/j.ajo.2018.01.034
12. Kristianslund O, Råen M, Østern AE, Drolsum L. Late in-the-bag intraocular lens dislocation: a randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology. 2017;124(2):151–159. doi:10.1016/j.ophtha.2016.10.024
13. Uthoff D, Teichmann KD. Secondary implantation of scleral-fixated intraocular lenses. J Cataract Refract Surg. 1998;24(7):945–950. doi:10.1016/S0886-3350(98)80048-5
14. Bausili Portabella MM, Nadal J, Alvarez de Toledo J, Fideliz de la Paz M, Barraquer RI. Long-term outcome of scleral-sutured posterior chamber intraocular lens: a case series. Br J Ophthalmol. 2020;104(5):712–717. doi:10.1136/bjophthalmol-2019-314054
15. Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141(2):308–312. doi:10.1016/j.ajo.2005.09.012
16. Asadi R, Kheirkhah A. Long-term results of scleral fixation of posterior chamber intraocular lenses in children. Ophthalmology. 2008;115(1):67–72. doi:10.1016/j.ophtha.2007.02.018
17. Chan CC, Crandall AS, Ahmed II. Ab externo scleral suture loop fixation for posterior chamber intraocular lens decentration: clinical results. J Cataract Refract Surg. 2006;32(1):121–128. doi:10.1016/j.jcrs.2005.06.050
18. Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47(7):476–485. doi:10.1136/jmg.2009.072785
19. Gimbel HV, Camoriano GD, Aman-Ullah M. Bilateral implantation of scleral-fixated cionni endocapsular rings and toric intraocular lenses in a pediatric patient with Marfan’s syndrome. Case Rep Ophthalmol. 2012;3(1):16–23. doi:10.1159/000335652
20. Konradsen T, Kugelberg M, Zetterstrom C. Visual outcomes and complications in surgery for ectopia lentis in children. J Cataract Refract Surg. 2007;33(5):819–824. doi:10.1016/j.jcrs.2007.01.032
21. Chee SP, Chan NS. Suture snare technique for scleral fixation of intraocular lenses and capsular tension devices. Br J Ophthalmol. 2018;102(10):1317–1319. doi:10.1136/bjophthalmol-2018-311868
22. Shen JF, Deng S, Hammersmith KM, et al. Intraocular Lens implantation in the absence of zonular support: an outcomes and safety update: a report by the American Academy of Ophthalmology. Ophthalmology. 2020;127(9):1234–1258. doi:10.1016/j.ophtha.2020.03.005
23. Kim EJ, Berg JP, Weikert MP, et al. Scleral-fixated capsular tension rings and segments for ectopia lentis in children. Am J Ophthalmol. 2014;158(5):899–904. doi:10.1016/j.ajo.2014.08.002
24. Buckley EG. Hanging by a thread: the long-term efficacy and safety of transscleral sutured intraocular lenses in children (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:294–311.
25. Kristianslund O, Dalby M, Moe MC, Drolsum L. Cost-effectiveness analysis in a randomized trial of late in-the-bag intraocular lens dislocation surgery: repositioning versus exchange. Acta Ophthalmol. 2019;97(8):771–777. doi:10.1111/aos.14108
26. Drolsum L, Rand-Hendriksen S, Paus B, Geiran OR, Semb SO. Ocular findings in 87 adults with Ghent-1 verified Marfan syndrome. Acta Ophthalmol. 2015;93(1):46–53. doi:10.1111/aos.12448
27. Pyeritz RE. Marfan syndrome: improved clinical history results in expanded natural history. Genet Med. 2019;21(8):1683–1690. doi:10.1038/s41436-018-0399-4
28. Sandvik GF, Vanem TT, Rand-Hendriksen S, Cholidis S, Saethre M, Drolsum L. Ten-year reinvestigation of ocular manifestations in Marfan syndrome. Clin Exp Ophthalmol. 2019;47(2):212–218. doi:10.1111/ceo.13408
29. Gimbel HV, Amritanand A. Suture refixation and recentration of a subluxated capsular tension ring-capsular bag-intraocular lens complex. J Cataract Refract Surg. 2013;39(12):1798–1802. doi:10.1016/j.jcrs.2013.10.002
30. Heilskov T, Joondeph BC, Olsen KR, Blankenship GW. Late endophthalmitis after transscleral fixation of a posterior chamber intraocular lens. Arch Ophthalmol. 1989;107(10):1427. doi:10.1001/archopht.1989.01070020501017
31. Schechter RJ. Suture-wick endophthalmitis with sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 1990;16(6):755–756. doi:10.1016/S0886-3350(13)81021-8
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
