Back to Journals » Clinical Ophthalmology » Volume 18
Long-Term Refractive Outcomes and Visual Quality of Multifocal Intraocular Lenses Implantation in High Myopic Patients: A Multimodal Evaluation
Authors Castro C , Ribeiro B , Couto IMC, Abreu AC , Monteiro S , Pinto MDC
Received 2 November 2023
Accepted for publication 24 January 2024
Published 5 February 2024 Volume 2024:18 Pages 365—375
DOI https://doi.org/10.2147/OPTH.S447827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Catarina Castro,1 Bruno Ribeiro,1 Inês Maria Campos Couto,1 Ana Carolina Abreu,1,2 Sílvia Monteiro,1,2 Maria do Céu Pinto1
1Department of Ophthalmology, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Department of Ophthalmology, Instituto de Ciências Biomédicas Abel Salazar – Universidade do Porto, Porto, Portugal
Correspondence: Catarina Castro, Tel +351222077500, Email [email protected]
Purpose: To perform a multimodal assessment of refractive outcomes and quality of vision (QoV) in patients with high myopia submitted to multifocal intraocular lens (IOL) implantation.
Methods: Retrospective study that included consecutive eyes with high myopia (axial length [AL] > 26.00mm) submitted to multifocal IOL implantation between January 2014 and February 2020. Minimum follow-up time was 3 years. QoV was evaluated with the Objective Scatter Index (OSI) and the Modular Transfer Function (MTF) by HD Analyzer®. Two QoV questionnaires were applied to patients in which both eyes were included: the McAlinden and the Catquest-9 SF.
Results: We included 50 eyes (28 patients). The mean follow-up time was 5.4± 1.0 years. Comparing to month 1 after surgery, at the last follow-up visit, there was a decrease in the uncorrected visual acuity (0.14± 0.13 vs 0.08± 0.09 LogMAR, p=0.024), a negative increase in the spherical equivalent (− 0.31± 0.60 vs − 0.02± 0.20, p=0.006) and no changes in the best-corrected visual acuity (p> 0.999). An uncorrected near visual acuity of at least J2 was achieved in 89% of eyes one month after surgery and in 91% of eyes at the last follow-up visit (p=0.829). At the last follow-up, the mean OSI was 5.1± 1.8 and the mean MTF was 17.5± 10.6. Some degree of near vision difficulty was reported by 91% of patients, and 74% of patients reported photic phenomena (halos, glare, starbursts). However, most patients reported that these symptoms caused none to little bothersome. At the last follow-up, 87% of patients were at least fairly satisfied with the surgery.
Conclusion: Even after a mean follow-up time of 5 years, patients maintained good uncorrected visual acuity. Even though most patients experienced some degree of near vision difficulty and visual symptoms, globally, our patients were satisfied with their current vision, and the experienced symptoms did not have a significant impact on their daily lives.
Keywords: refractive surgery, multifocal intraocular lens, high myopia
Introduction
Myopia is a common refractive error. In 2010, it was estimated that it affected 1950 million people, around 28% of the world’s population, with projections indicating that this value could increase to 4758 million people by 2050, affecting near 50% of the population. Regarding high myopia, it was estimated that it affected 277 million people in 2010 (4.0% of the global population) and that it will affect 938 million people by 2050 (9.8% of the global population).1
Refractive correction of myopia can be achieved by the use of spectacles or contact lenses and with refractive surgery.1 In patients with myopia and presbyopia, the procedure of choice for refractive correction is usually Refractive Lens Exchange (RLE), which consists of removing the clear lens followed by the insertion of an intraocular lens (IOL) in the capsular bag.2 Multifocal IOLs are an option often considered.3
Previous studies have reported good visual and refractive outcomes after multifocal IOL implantation.4 However some studies showed worsening of contrast sensitivity and more visual symptoms (such as glare, halos or starbursts) compared to monofocal IOLs.5,6 In patients with high myopia, further questions may be raised. In long axial lengths, biometric formulas are not as accurate, increasing the risk of postoperative errors, especially hyperopic.4,7,8 This is particularly important in the setting of multifocal IOLs, as even small residual refractive errors can limit visual performance.9 In patients who require toric IOLs, the outcomes may also be affected by the presence of larger capsular bags, which increase the risk of lens rotation.7 Postoperative complications may also limit the success of the intervention. Both younger ages and high myopia have been previously associated with an increased risk of retinal detachment after lens surgery.10 Finally, most cases of pathological myopia happen in eyes with high myopia, and its development may compromise the long-term visual results.11 Hence, all these factors need to be weighted when considering the implantation of multifocal IOLs in high-myopic patients, as they may lead to postoperative unsatisfaction.
With the increasing prevalence of myopia, it is expected that the number of patients looking for surgical correction will also increase. Our purpose is to evaluate the long-term outcomes of correction of high myopia with RLE and multifocal IOL implantation and to evaluate the quality of vision of these patients.
Methods
We performed a retrospective study that included consecutive eyes with high myopia submitted to RLE with multifocal IOL implantation between January 2014 and February 2020 in Centro Hospitalar Universitário de Santo António. High myopia was defined as an axial length (AL) equal to or superior to 26.00 mm. Only patients with a minimum follow-up of 3 years were included. Eyes with a previous history of refractive surgery were excluded.
In our center, all patients who wish for eyeglass independence undergo a careful preoperative study that includes, in addition to a complete ophthalmological examination, corneal endothelial assessment, corneal tomography, and an optic disc and macular optical coherence tomography (OCT) scan. The inclusion criteria for multifocal IOL implantation are the presence of a distance refractive error associated with presbyopia, the absence of anterior or posterior segment pathology that might compromise visual potential (such as glaucoma, myopic tractional maculopathy, corneal leucomas, among others), the presence of a posterior vitreous detachment, and realistic expectations in relation to the surgical outcomes. Previous history of amblyopia, retinal detachment in the same or contralateral eye, or the presence of multiple peripheral retinal degenerative changes contraindicate multifocal IOL implantation. Prior to surgery, all myopic patients were observed with a 3-mirror Goldmann lens under mydriasis to exclude the presence of retinal holes or other lesions that increase the risk for rhegmatogenous retinal detachment.
The surgical procedure consisted of the creation of two clear cornea incisions (the main port with 2.4mm at 140° degrees), followed by continuous circular capsulorhexis, hydrodissection, lens phacoaspiration, and insertion of the multifocal IOL in the capsular bag. As the wounds were self-sealing, no sutures were used. The choice of the IOL was based on the patient’s social and work context, visual needs, psychological profile and expectations. In the presence of astigmatism equal to or superior to 1 diopter (D), a toric IOL was implanted. All surgeries were performed by three experienced refractive surgeons.
The IOLs implanted were the bifocal or trifocal ATLISA® (Models 809M, 909MP, 909M, 839 MP; 939 MP; Carl Zeiss Meditec AG, Jena, Germany) and the Tecnis® ZLB00 (Johnson & Johnson Vision, USA).
This study was performed in accordance with the Declaration of Helsinki in its latest amendment and is in accordance with the ethical requirements of the Institutional Review Board of Centro Hospitalar Universitário de Santo António (Departamento de Ensino, Formação e Investigação). All patients gave written informed consent after explanation of the study purpose and design.
We analyzed patients’ medical records at three timepoints: at baseline, 1 month after surgery and at the last follow-up visit. Distance (6m) uncorrected (UCVA) and best corrected visual acuity (BCVA) were evaluated with the Snellen chart and converted to the LogMAR scale for statistical purposes.12 Near vision (33 cm) was evaluated with the Jaeger chart. The spherical equivalent (SE) was also recorded. The safety and efficacy indexes were calculated. The safety index was calculated as the postoperative BCVA divided by the preoperative BCVA. The efficacy index was defined as the postoperative UCVA divided by the preoperative BCVA. The cut-offs considered were 0.85 for the safety index and 0.80 for the efficacy index. For both indexes, values below the cut-off indicate loss of more than two lines of visual acuity.13
Demographic data (age and gender) and the AL at the time of surgery were recorded. In the last visit, the AL, the presence of posterior capsular opacification or posterior capsulotomy, the macular status, history of complications after surgery (such as retinal detachment), and the vision quality were also evaluated. AL was measured with the IOL Master 500® or 700® (Carl Zeiss Meditec, Jena, Germany), in accordance with the device used for preoperative assessment. Macular status was assessed with a spectral domain OCT (SD-OCT, Spectralis®, Heidelberg Engineering, Heidelberg, Germany).
Vision quality at the end of follow-up was objectively evaluated with the Objective Scatter Index (OSI) and the Modular Transfer Function (MTF) with the HD Analyzer® (Visiometrics S.L., Terrassa, Spain). Additionally, two quality of vision questionnaires were applied to patients in which both eyes were included in this study: the McAlinden and the Catquest-9 SF.
The McAlinden questionnaire is a 30-item instrument that evaluates 10 symptoms (glare, haloes, starbursts, hazy vision, blurred vision, distortion, double vision, fluctuation, focusing difficulties, and depth perception) rated on each of three scales (frequency, severity, and bothersome).14 Due to the small number of answers on the scale severity and bothersome (patients that answered “never” in the frequency scale do not answer the other two scales), Rasch analysis was not performed.
The Catquest-9 SF is a 9-item short form of the Catquest questionnaire, which was designed to evaluate the benefits of cataract surgery. The questionnaire is divided into two parts. The first one contains seven questions related to experienced difficulties in daily tasks (reading, recognizing faces, seeing prices, walking on uneven ground, doing needlework/handicraft, reading text on television, or performing a hobby). The second part has two global assessment questions related to experienced difficulties in daily life caused by the present vision and to general satisfaction with the present vision.15
A sub-analysis was performed, comparing trifocal and bifocal IOLs, the ATLISA® with the Tecnis IOLs® and toric and non-toric IOLs.
Statistical analysis was performed using IBM® SPSS® Statistics version 26. The normality of the data was assessed using the Shapiro–Wilk test. Descriptive statistics are shown as mean±standard deviation. For categorical variables, descriptive statistics are shown as relative frequencies. For comparisons over time, repeated measures analysis and paired tests were performed, followed by a post-hoc Bonferroni correction when appropriate. For comparison between groups, independent sample tests were used. For comparisons between categorical variables, the Fisher’s exact test was used. For correction of baseline differences, an analysis of covariance with Bonferroni correction was performed. Statistical significance was considered in the presence of a p-value inferior to 0.05.
Results
This study included 50 eyes of 28 patients. Baseline characteristics and IOL type are described in Tables 1 and 2, respectively. The mean follow-up time was 5.4±2.1 years after surgery.
 |
Table 1 Baseline Characteristics |
 |
Table 2 Multifocal Intraocular Lens Characteristics |
Postoperative Complications
None of the eyes developed retinal detachment or neovascular membranes during follow-up. Two eyes developed an epiretinal membrane, one of which with intraretinal cysts. One eye developed pigmented retinal epithelium changes.
At the last follow-up visit, 42% of eyes had already undergone Nd: YAG posterior capsulotomy, and 14% had mild posterior capsule opacification. There was no association between the IOL type and the development of posterior capsule opacification (p=0.750).
Visual and Refractive Results
One month after surgery, the UCVA was 0.08±0.09 LogMAR (p<0.001). The mean safety index was 1.2±0.3, with 93% of eyes having ≥0.85, and the mean efficacy index was 1.2±0.3, with 98% of eyes having ≥0.80. At the last follow-up, the UCVA decreased slightly to 0.14±0.13 LogMAR (p=0.024). Changes in BCVA and UCVA are summarized in Table 3. An UCVA equal to or better than 0.1 logMAR was achieved in 76% of eyes at month 1 and in 63% at the last follow-up visit (p=0.072). At the last follow-up visit, 22% of eyes had a better UCVA compared to month 1, and 46% of eyes had a worse UCVA (26% - 1 logMAR line, 9% - 2 logMAR lines, 4% - 3 logMAR lines, 7% - 4 logMAR lines). Of the eyes that had worse UCVA at the last follow-up visit, 72% had a refractive error, 14% had retinal changes, and 14% had posterior capsular opacification.
 |
Table 3 Distance Visual Acuity |
An uncorrected near visual acuity of at least J2 was achieved in 89% of eyes one month after surgery and in 91% of eyes at the last follow-up visit (p=0.829). The near visual acuity is summarized in Table 4.
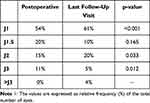 |
Table 4 Near Uncorrected Visual Acuity (Jaeger Scale) |
The mean SE decreased after surgery (p<0.001) but had a slight negative increase at the last follow-up visit, compared to month 1 (−0.31±0.60 vs −0.02±0.20, p=0.006). Changes in SE are summarized in Table 3.
All patients obtained eyeglass independence in the first month after surgery. At the end of follow-up, 3 (11%) patients required eyeglasses. Two required eyeglasses for distance and near vision, and one patient only for near activities.
At the last follow-up, there was an increase in the AL (∆=0.13±0.37 mm, p=0.038), and no changes in the K1 (∆=0.06±0.35 D, p=0.279) and K2 (∆=0.02±0.05 D, p=0.831).
Quality of vision
Twenty-three patients had both eyes included in this study and answered the quality of vision questionnaires at the last follow-up visit.
In the Catquest-9SF, 52% of patients were very satisfied with their current vision, 35% of patients were fairly satisfied, and 13% of patients were rather dissatisfied. Some degree of difficulty in a near vision activity was reported by 91% of patients. Most patients rated that difficulty at the lowest level (some). The detailed data is represented in Figure 1.
In the McAlinden questionnaire, 74% of patients reported photic phenomena (halos, glare, or starbursts). The frequency of experienced visual symptoms and their severity, according to the McAlinden questionnaire, are detailed in Figures 2 and 3, respectively. Regarding the bothersome these symptoms caused, most patients reported it to be none to mild (Figure 4).
At the last follow-up visit, the mean OSI was 4.8 ± 1.8 and the mean MTF was 17.5 ± 10.6.
Comparison Between Different Intraocular Lenses
A trifocal IOL was implanted in 42% of eyes and a bifocal in 58%. Patients submitted to trifocal IOL implantation had better preoperative BCVA (0.09±0.09 vs 0.17±0.14 LogMAR, p= 0.018) and less negative SE (−7.6±2.7 vs −10.4±5.1 D, p=0.021). The preoperative UCVA was similar between groups (1.12±0.52 vs 1.22±0.37 LogMAR, p=0.134). After correcting for preoperative differences, there were no statistically significant postoperative differences between IOLs (p>0.110).
An ATLISA® IOL was implanted in 71% and a Tecnis® IOL in 29% of eyes. When comparing the ATLISA® and Tecnis® IOLs, there were no statistically significant differences in the preoperative BCVA (0.14±0.14 vs 0.14±0.08 LogMAR, p=0.741), UCVA (1.14±0.36 vs 1.18±0.25 LogMAR, p=0.463) and SE (−8.9±4.9 vs −10.1± 3.3 D, p=0.093). There were no differences between IOLs in both postoperative timepoints (p>0.098).
Comparing toric (48%) IOLs with non-toric (52%), there were no preoperative differences in the BCVA (0.14±0.12 vs 0.13±0.14, p=0.479), UCVA (1.19±0.12 vs 1.14±0.25 LogMAR, p=0.384) and SE (−10.2±5.2 vs −8.3±3.3, p=0.136). There were no postoperative differences between IOLs (p>0.076).
These results of these comparisons are detailed in Table 5.
 |
Table 5 Comparison Between Different Intraocular Lenses |
Discussion
In our study, patients with high myopia who underwent multifocal IOL implantation obtained a good postoperative UCVA, with good safety and efficacy indexes. After a mean time of 5 years, most patients still maintained a good UCVA and eyeglass independence. A worse UCVA, compared with the first month after surgery, was observed in 46% of eyes. However, most of these cases had a decrease inferior to 2 logMAR lines and remained spectacle independent. This decrease in the mean UCVA is probably multifactorial, with contributions from posterior capsule opacification, possible changes in the lens position, and variation of the AL. Despite not reaching statistical significance, small changes in keratometry, may have an additive effect as well.
Concerning near vision, 91% of eyes had at least J2 at the last follow-up visit. Some patients had an improvement in their near visual acuity, due to an increase in the negative spherical equivalent. Most patients reported difficulties in some near vision activity, however, most also rated that difficulty at the lowest level.
Most of our patients had visual complaints, mostly hazy or blurred vision and photic phenomena. The reported incidence of visual phenomena varies significantly in the literature. A previous study that compared two multifocal IOLs in patients with a mean AL of 24 mm showed that the presence of photic phenomena was superior to 90%, higher than in our study.16 Another study also found a very high prevalence of postoperative visual phenomena (>80%).17 However, in these studies, the analysis was performed a few months after surgery. In our study, long-term neuroadaptation may have contributed to slightly better results. Nonetheless, in these studies, most patients had mild to moderate symptoms, and most did not find them very bothersome, as found in our patients.16,17 Multifocal IOLs were previously associated with higher rates of photic phenomena, compared to monofocals.5,18 Interestingly, another study in high-myopic patients did not find significant differences in the presence of visual symptoms (halos and glare) between the monofocal and multifocal IOLs evaluated.19
Regarding visual quality, our patients had a low MTF and a high OSI mean value. In general, lower MTF and higher OSI values are associated with worse optical quality and higher intraocular scatter, respectively.20 Nevertheless, in our study, we had a high myopic population, and previous studies suggested that these patients have lower quality of vision.20,21 Studies reporting the effect of multifocal IOL implantation on the optical system quality are lacking. Alfonso et al19 showed in their study that, compared to low myopic eyes, high myopic eyes had lower contrast sensitivity, mainly at higher spatial frequencies, under photopic conditions, and at all spatial frequencies under mesopic conditions. This could be a contributing factor to the near vision difficulties experienced by our patients. Ogawa et al22 also observed that patients with high myopia had lower contrast sensitivity; however, the authors considered that it had almost no effect on visual function. Furthermore, in our study, diffractive IOLs were used. These IOLs have concentric rings that bend the light rays, directing portions of the light to distant and near focal points, resulting in either two or three retinal images, in the case of bifocal and trifocal IOLs, respectively.23 However, there is also a percentage of loss of light, which contributes to lower quality of vision, especially in scotopic and mesopic conditions.24,25 Further studies comparing the outcomes of multifocal IOL implantation in high, moderate, and low myopia are needed to understand its impact on the vision quality.
Previous studies showed that the risk of retinal detachment is higher in eyes submitted to phacoemulsification, with high myopia being an additional contributing factor.26 In our study, none of the eyes developed retinal detachment. We believe that preoperative retinal evaluation under fundus dilation with a 3-mirror lens to detect lesions that predispose to retinal detachment and assess the presence of posterior vitreous detachment is important to minimize the risk. Regarding myopic neovascular membranes, a previous study reported an incidence of 12.5% following cataract surgery.27 In our study, none of the eyes developed myopic neovascularization after surgery.
We performed a subgroup analysis, comparing the two different types of IOLs implanted (ATLISA® and Tecnis®), trifocal and bifocal IOLs, and toric and non-toric IOLs. In our study, after correcting for baseline differences when appropriate, similarly good results were found (no statistically significant differences). However, our study was not designed for this comparison, the number of eyes in each group was small (particular in the evaluation of photic phenomena, that only included patients with bilateral IOL implantation) and the groups were not well balanced due to the non-random choice of IOL. Thus, these results must be interpreted with caution.
Few studies evaluate the outcomes of multifocal IOL implantation in patients with high myopia. A previous study by Ogawa et al22 evaluated the outcomes of multifocal TECNIS IOL (ZMA00 and ZMB00, Abbott Medical Optics) implantation in patients with low and high myopia up to 12 months after surgery. After surgery, there were no differences in the distance and near uncorrected and corrected visual acuities, or spherical equivalent between both groups. Spectacle use was still necessary in 19% of patients in the high myopic group and 18% in the low myopic group. Furthermore, patients were satisfied with the surgical procedure and the reduced dependence on spectacles.22 The results of this study seem to suggest that the implantation of multifocal IOL in high myopes does not lead to worse results than the implantation in lower refractive errors. However, in turn, Alfonso et al,19 who compared the 6-month outcomes of the AcrySof ReSTOR SN60D3 IOL in eyes with high and low myopia, found that despite leading to good refractive and visual results in both groups, the UCVA and uncorrected and best-corrected near visual acuity were statistically better in eyes with low myopia.19
Wang et al28 compared the outcomes of the AcrySof IQ ReSTOR SN6AD3 multifocal IOL, the AcrySof IQ ReSTOR SN6AD1 multifocal IOL, and the AcrySof IQ SN60WF monofocal IOL, 6 months after surgery, in eyes with high myopia. As expected, the multifocal IOLs led to significantly better near visual acuity and superior eyeglass independence. The VF-7 questionnaire scores were higher in patients with multifocal IOLs. The results of this study show that implanting a multifocal IOL in high myopes may have advantages over monofocal IOL in selected cases and does not lead to worse patient satisfaction.28
Martiano and Cochener29 evaluated high myopic eyes 6 years after AT LISA bifocal IOL implantation. As in our study, most patients (85%) achieved spectacle independence and 9% needed glasses for near vision. Visual symptoms, such as halos and glare, were reported by most patients (90%). Complaints of nocturnal halos and glare were worse during the first 6 postoperative months, with subsequent improvement. Two eyes developed a rhegmatogenous retinal detachment approximately 20 months after surgery, and one eye developed macular atrophy due to cystoid macular edema. Similar to our results, posterior capsulotomy was needed in 52% of eyes.29
Shen et al30 compared the AT LISA Tri 839MP and the LS-313 MF30 IOLs in eyes with high myopia. Both IOLs led to good visual and refractive outcomes, with a mean postoperative SE of −0.52±0.48 D in the MF30 group and −0.08 ± 0.16 D in the 839MP group. The 839MP group showed significantly better 3-month UCVA, BCVA and uncorrected near visual acuity. The MF30 group had a significantly higher VF-14 score but lower satisfaction with near vision quality.30
Alfonso-Bartolozzi31 et al found that implantation of a trifocal IOL led to good visual results in high-myopic eyes, 6 months after surgery, with a pre-operative BCVA of 0.74 ± 0.20 and a postoperative UCVA of 0.91 ± 0.10 (Snellen).
Overall, the existing studies seem to suggest that, despite the consequent visual phenomena and possible reduced contrast sensitivity, implantation of multifocal IOL in high myopes leads to good visual and refractive outcomes and patient satisfaction.
Our study has some limitations, particularly the small number of participants. Furthermore, quality of vision assessment (questionnaires, OSI, and MTF) was not performed in the 1st month evaluation, so we could not evaluate its evolution over time. Some eyes had posterior capsule opacification. Despite being mild and not yet having an indication for posterior capsulotomy, it could affect the patient’s reported quality of vision. Regardless, as posterior capsule opacification is part of the natural course of an RLE surgery, we decided to include these patients. Another limitation is that our patients had different types of IOL implanted. However, this study aims to evaluate the long-term outcomes of multifocal IOL implantation in a real-life setting, in which the most appropriate IOL is chosen for each patient based on the preoperative individual assessment. Finally, in our study patients were operated by three different surgeons, which could lead to differences in surgical outcomes. However, the number of eyes with high myopia submitted to multifocal IOL implantation it usually small, and using the data of only one surgeon would significantly decrease of sample size. Regardless of these limitations, this is, to our best knowledge, one of the studies with the longest follow-up evaluating the outcomes of multifocal IOL implantation in patients with high myopia that also evaluated the objective and subjective quality of vision.
In conclusion, our patients obtained excellent postoperative UCVA, with good efficacy and safety indexes. Despite a slight decrease in the UCVA, after a mean follow-up time of 5 years, most patients remained eyeglass independent. Even though most patients experienced some degree of near vision difficulty and visual symptoms, globally, patients were satisfied with their current vision, and the experienced symptoms caused them none to little bothersome. Thus, multifocal IOL implantation seems to be a good option in patients with high myopia who wish for eyeglass independence, after proper selection.
Data Sharing Statement
Data is available upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The present work did not receive any funding.
Disclosure
The authors have no conflicts of interest to report for this work.
References
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi:10.1016/j.ophtha.2016.01.006
2. Kim T, Alió Del Barrio JL, Wilkins M, Cochener B, Ang M. Refractive surgery. Lancet. 2019;393(10185):2085–2098. doi:10.1016/S0140-6736(18)33209-4
3. Kanclerz P, Toto F, Grzybowski A, Alio JL. Extended Depth-of-Field intraocular lenses: an update. Asia-Pac J Ophthalmol. 2020;9(3):194–202. doi:10.1097/APO.0000000000000296
4. Wan KH, Lam TCH, Yu MCY, Chan TCY. Accuracy and precision of intraocular lens calculations using the new Hill-RBF Version 2.0 in eyes with high axial myopia. Am J Ophthalmol. 2019;205:66–73. doi:10.1016/j.ajo.2019.04.019
5. Schallhorn JM, Pantanelli SM, Lin CC, et al. Multifocal and accommodating intraocular lenses for the treatment of presbyopia. Ophthalmology. 2021;128(10):1469–1482. doi:10.1016/j.ophtha.2021.03.013
6. Grzybowski A, Kanclerz P, Tuuminen R. Multifocal intraocular lenses and retinal diseases. Graefes Arch Clin Exp Ophthalmol. 2020;258(4):805–813. doi:10.1007/s00417-020-04603-0
7. Chong EW, Mehta JS. High myopia and cataract surgery. Curr Opin Ophthalmol. 2016;27(1):45–50. doi:10.1097/ICU.0000000000000217
8. Moshirfar M, Durnford KM, Jensen JL, et al. Accuracy of six intraocular lens power calculations in eyes with axial lengths greater than 28.0 mm. J Clin Med. 2022;11(19):5947. doi:10.3390/jcm11195947
9. Bohac M, Barisic A, Patel S, Gabric N. Multifocal intraocular lenses: postimplantation residual refractive error. In: Alió JL, Pikkel J, editors. Multifocal Intraocular Lenses. Essentials in Ophthalmology. Springer International Publishing; 2019:93–101.
10. Daien V, Le Pape A, Heve D, Carriere I, Villain M. Incidence, risk factors, and impact of age on retinal detachment after cataract surgery in France. Ophthalmology. 2015;122(11):2179–2185. doi:10.1016/j.ophtha.2015.07.014
11. Ohno-Matsui K, Wu PC, Yamashiro K, et al. IMI pathologic myopia. Invest Ophthalmol Vis Sci. 2021;62(5):5.
12. Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13(4):388–391. doi:10.3928/1081-597X-19970701-16
13. Gomel N, Negari S, Frucht-Pery J, Wajnsztajn D, Strassman E, Solomon A. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS One. 2018;13:12.
14. McAlinden C, Pesudovs K, Moore JE. The Development of an instrument to measure quality of vision: the quality of vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–5545. doi:10.1167/iovs.10-5341
15. Lundström M, Pesudovs K. Catquest-9SF patient outcomes questionnaire: nine-item short-form Rasch-scaled revision of the Catquest questionnaire. J Cataract Refract Surg. 2009;35(3):504–513. doi:10.1016/j.jcrs.2008.11.038
16. Lee YW, Choi CY, Moon K, et al. Clinical outcomes of new multifocal intraocular lenses with hydroxyethyl methacrylate and comparative results of contrast sensitivity, objective scatter, and subjective photic phenomena. BMC Ophthalmol. 2022;22(1):379. doi:10.1186/s12886-022-02600-x
17. Ison M, Scott J, Apel J, Apel A. Patient expectation, satisfaction and clinical outcomes with a new multifocal intraocular lens. Clin Ophthalmol. 2021;15:4131–4140. doi:10.2147/OPTH.S327424
18. De Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;2016:12.
19. Alfonso JF, Fernández-Vega L, Ortí S, Ferrer-Blasco T, Montés-Micó R. Differences in visual performance of Acrysof ReSTOR IOL in high and low myopic eyes. Eur J Ophthalmol. 2010;20(2):333–339. doi:10.1177/112067211002000212
20. Miao H, Tian M, He L, Zhao J, Mo X, Zhou X. Objective optical quality and intraocular scattering in myopic adults. Invest Ophthalmol Vis Sci. 2014;55(9):5582–5587. doi:10.1167/iovs.14-14362
21. Vilaseca M, Padilla A, Ondategui JC, Arjona M, Güell JL, Pujol J. Effect of laser in situ keratomileusis on vision analyzed using preoperative optical quality. J Cataract Refract Surg. 2010;36(11):1945–1953. doi:10.1016/j.jcrs.2010.05.029
22. Ogawa T, Shiba T, Tsuneoka H. Usefulness of implantation of diffractive multifocal intraocular lens in eyes with long axial lengths. J Ophthalmol. 2015;2015:1–9. doi:10.1155/2015/956046
23. Rampat R, Gatinel D. Multifocal and extended depth-of-focus intraocular lenses in 2020. Ophthalmology. 2021;128(11):e164–e185. doi:10.1016/j.ophtha.2020.09.026
24. Portney V. Light distribution in diffractive multifocal optics and its optimization. J Cataract Refract Surg. 2011;37(11):2053–2059. doi:10.1016/j.jcrs.2011.04.038
25. Lee S, Park G, Kim S, et al. Geometric-phase intraocular lenses with multifocality. Light Sci Appl. 2022;11(1):320. doi:10.1038/s41377-022-01016-y
26. Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification—a review of the literature. Eye. 2020;34(4):616–631. doi:10.1038/s41433-019-0575-z
27. Hayashi K, Ohno-Matsui K, Futagami S, Ohno S, Tokoro T, Mochizuki M. Choroidal neovascularization in highly myopic eyes after cataract surgery. Jpn J Ophthalmol. 2006;50(4):345–348. doi:10.1007/s10384-006-0335-z
28. Wang Q, Zhao G, Wang Q, Jia W. Visual quality after Acrysof IQ ReSTOR intraocular lens implantation in eyes with high myopia. Eur J Ophthalmol. 2012;22(2):168–174. doi:10.5301/EJO.2011.8357
29. Martiano D, Cochener B. Implants multifocaux chez le grand myope, résultats à 6ans. J Fr Ophtalmol. 2014;37(5):393–399. doi:10.1016/j.jfo.2013.08.009
30. Shen J, Zhang L, Ni S, Cai L, Guo H, Yang J. Comparison of visual outcomes and quality of life in patients with high myopic cataract after implantation of AT LISA Tri 839MP and LS-313 MF30 intraocular lenses. J Ophthalmol. 2022;2022:1–9. doi:10.1155/2022/5645752
31. Alfonso-Bartolozzi B, Villota E, Fernández-Vega-González Á, Fernández-Vega-Cueto L, Fernández-Vega Á, Alfonso JF. Implantation of a trifocal intraocular lens in high myopic eyes with nasal-inferior staphyloma. Clin Ophthalmol. 2020;14:721–727. doi:10.2147/OPTH.S227670
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.