Back to Journals » Clinical Epidemiology » Volume 14
Lipid Testing Trends Before and After Hospitalization for Myocardial Infarction Among Adults in the United States, 2008–2019
Authors Levintow SN , Reading SR, Noshad S, Mayer SE, Wiener C, Eledath B , Exter J, Brookhart MA
Received 5 February 2022
Accepted for publication 19 May 2022
Published 1 June 2022 Volume 2022:14 Pages 737—748
DOI https://doi.org/10.2147/CLEP.S361258
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Vera Ehrenstein
Sara N Levintow,1,2 Stephanie R Reading,3 Sina Noshad,3 Sophie E Mayer,1,2 Catherine Wiener,1 Bassim Eledath,1 Jason Exter,3 M Alan Brookhart1,4
1NoviSci, Inc., Durham, NC, USA; 2Department of Epidemiology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 3Amgen, Inc., Thousand Oaks, CA, USA; 4Department of Population Health Sciences, Duke University, Durham, NC, USA
Correspondence: Sara N Levintow, Department of Epidemiology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Email [email protected]
Background: Routine monitoring of low-density lipoprotein cholesterol (LDL-C) identifies patients who may benefit from modifying lipid-lowering therapies (LLT). However, the extent to which LDL-C testing is occurring in clinical practice is unclear, specifically among patients hospitalized for a myocardial infarction (MI).
Methods: Using US commercial claims data, we identified patients with an incident MI hospitalization between 01/01/2008-03/31/2019. LDL-C testing was assessed in the year before admission (pre-MI) and the year after discharge (post-MI). Changes in LDL-C testing were evaluated using a Poisson model fit to pre-MI rates and extrapolated to the post-MI period. We predicted LDL-C testing rates if no MI had occurred (ie, based on pre-MI trends) and estimated rate differences and ratios (contrasting observed vs predicted rates).
Results: Overall, 389,367 patients were hospitalized for their first MI during the study period. In the month following discharge, 9% received LDL-C testing, increasing to 27% at 3 months and 52% at 12 months. Mean rates (tests per 1000 patients per month) in the pre- and post-MI periods were 51.9 (95% CI: 51.7, 52.1) and 84.4 (95% CI: 84.1, 84.6), respectively. Over 12 months post-MI, observed rates were higher than predicted rates; the maximum rate difference was 66 tests per 1000 patients in month 2 (rate ratio 2.2), stabilizing at a difference of 15– 20 (ratio 1.2– 1.3) for months 6– 12.
Conclusion: Although LDL-C testing increased following MI hospitalization, rates remained lower than recommended by clinical guidelines. This highlights a potential gap in care, where increased LDL-C testing after MI may provide opportunities for LLT modification and decrease risk of subsequent cardiovascular events.
Keywords: low-density lipoprotein cholesterol, myocardial infarction, statin, ezetimibe, proprotein convertase subtilisin/kexin type 9 inhibitors
Introduction
Elevated levels of low-density lipoprotein cholesterol (LDL-C) play a central role in the development of atherosclerotic cardiovascular disease (ASCVD). Use of lipid-lowering therapies (LLT) has proven efficacy for decreasing LDL-C and the risk of ASCVD-related events.1–3 Common LLT regimens include the use of statins (of varying intensities) or statins plus ezetimibe (or other non-statin LLT), with the latter generally prescribed to achieve further LDL-C reductions compared to statins alone.4,5 Proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i), in particular, are a class of non-statin LLT comprising monoclonal antibodies that function to block the PCSK9 protein, and, in clinical trials, adding PCSK9i to a statin led to greater lowering of LDL-C than statin monotherapy and reduced the risks of myocardial infarction (MI), ischemic stroke (IS), and other ASCVD events.6,7 However, identifying the most appropriate LLT for a patient is contingent upon routine monitoring of LDL-C levels.
Cholesterol treatment guidelines recommend lipid measurement 4 to 12 weeks following statin initiation or dose adjustment, with follow-up testing every 3 to 12 months thereafter to assess therapeutic adherence and response.3,4 However, prior research suggests that the frequency of LDL-C testing may be suboptimal in populations who might benefit most from treatment. A previous study reported gradual declines in LDL-C testing rates among patients initiating LLT during 2008–2016, including patients at very high cardiovascular risk (ie, prior hospitalizations for MI or IS) who had lower rates of LDL-C testing than more general populations initiating statins or ezetimibe.8 Another study found lower than expected rates of LDL-C testing and high-intensity statin use for patients discharged from a MI hospitalization in 2007–2009.9 Only 21% of patients were discharged on a high-intensity statin, fewer than half received an LDL-C test within 90 days of discharge, and by one year, high-intensity statin use had decreased to 14%.
In this study, we sought to characterize real-world use of LDL-C testing using a large commercial healthcare insurance claims database, focusing on US adults hospitalized for incident MI. This population is at high risk for secondary ASCVD events and most likely to benefit from intensifying or modifying LLT regimens (vs individuals using LLT for primary ASCVD prevention).4,10 To understand the impact of a MI hospitalization on rates of LDL-C testing, we employed a modeling approach that estimated the expected rates of LDL-C testing (had no MI occurred in this population) for comparison with observed rates. While we expected LDL-C testing rates to increase after a MI hospitalization (as patients are started on high-intensity statins or non-statins are added), it is not known if increased testing is as frequent as clinical guidelines recommend, or in which subgroups or for how long patients undergo close LDL-C monitoring. More intensive testing in high-risk populations could help better assess ASCVD risk and provide opportunities for further therapeutic intervention.
Methods
Study Population
The study cohort was drawn from the MarketScan® Commercial Claims and Encounters and Medicare Supplemental administrative health insurance claims databases (IBM Corp.). The MarketScan® database captures health-care claims data in the US for privately insured individuals (aged <65 years) and individuals with Medicare Supplemental insurance (aged ≥65 years). Data were available on inpatient and outpatient diagnoses, procedures, and medications, which were identified using codes from the International Classification of Diseases, Clinical Modification, 9th and 10th Revision (incorporating changes from ICD-9-CM to ICD-10-CM), Healthcare Common Procedure Coding System (HCPCS), Current Procedural Terminology (CPT), and National Drug Codes (NDC). We used MarketScan® data from 01/01/2007 to 03/31/2020, limited to nearly 1.9 million patients who had ≥1 claim with any ICD diagnosis code for MI.
Patients were eligible for the study cohort at the time of their first recorded MI hospitalization occurring between 01/01/2008 (to allow one year of lookback) and 03/31/2019 (for one year of follow-up). Incident MI hospitalizations were identified by inpatient claims with ICD-9 410.xx (excluding 410.x2) or ICD-10 I21.xx, I22.x. Patients were required to be continuously enrolled in MarketScan® for the one year leading up to the MI hospitalization, aged ≥20 years on the date of admission, and discharged alive to the community (excluded if died during hospitalization or transferred to another facility). Baseline covariates were identified in the one year prior to the MI and consisted of demographics (age, sex, geographic region, type of insurance), medication use (statins, ezetimibe, PCSK9i), and a variety of comorbidities. These included chronic kidney disease, heart failure, diabetes, cancer, hypertension, dyslipidemia (including hypercholesterolemia), muscle events (rhabdomyolysis/myositis), pancreatitis, obesity, chronic obstructive pulmonary disease (COPD), asthma, cognitive impairment (dementia, Alzheimer’s disease, Pick’s disease, memory loss, amnesia, reactive confusion, psychotic disorders, intellectual disabilities, delirium, concussion), and indicators of frailty (oxygen use, wheelchair, hospital bed, rehabilitation services, and difficulty walking). We also assessed other ASCVD diagnoses, including IS, aneurysm, carotid/vertebral/basilar stenosis, carotid endarterectomy, cerebrovascular disease, coronary atherosclerosis/angina, coronary artery bypass grafting/percutaneous coronary intervention, carotid/vertebral/basilar stenting, endovascular stent graft, peripheral vascular disease, peripheral artery disease, transient ischemic attack, and unstable angina.
LDL-C testing was assessed in the year before MI hospitalization admission (pre-MI period) and for up to one year after MI hospitalization discharge (post-MI period), until the earlier of insurance plan disenrollment or end of one year. LDL-C test dates were identified using CPT codes (80061, 83721, 82465, 3011F, 3278F) and HCPCS codes (G8593, G8595, G8597, G8893, G8890, G8725, G8767) associated with inpatient or outpatient claims. In a secondary analysis, we identified subsequent MI hospitalizations during the year of follow-up from the first MI, defined as a second inpatient claim for MI occurring ≥2 days following discharge from the first MI hospitalization. Follow-up for LDL-C testing was extended in this subgroup for up to one year after discharge from the second hospitalization (with censoring for disenrollment or end of data).
Statistical Analysis
We evaluated the distribution of all covariates in the year leading up to the MI hospitalization, and for medications we also assessed prescription fills in the 30 days following hospitalization and during the remainder of the year. In the post-MI period, the time to first LDL-C test was estimated using a Kaplan–Meier estimator of the survival function that accounted for censoring due to disenrollment. Throughout the study period, LDL-C testing rates were estimated by fitting an over-dispersed Poisson model to the number of tests per 30-day interval, with intervals defined relative to the MI hospitalization event (ie, 12 intervals in the pre-MI period, 12 intervals in the post-MI period).
In the primary analysis, we sought to estimate counterfactual rates of LDL-C testing if the MI had not occurred. To do this, we fit a Poisson model to the pre-MI period and extrapolated the model to the post-MI period, accounting for person-time and seasonality. For the model fit, we excluded data from the 12th pre-MI interval (30 days immediately prior to MI) as the observed rate already began to diverge from pre-existing trends. We estimated the change in LDL-C testing as rate differences and ratios, contrasting the observed and model-predicted rates for each 30-day interval in the post-MI period. Empirical standard error was computed by predicting the number of tests per interval at the patient level, calculating patient-level rate differences and ratios, and then taking the standard error of those patient-level rate difference and ratio estimates across the cohort. These estimates of standard error were used to calculate 95% confidence intervals for the overall rate differences and ratios. We additionally reran this analysis stratified by the following variables: sex (male, female), age (<65 years, 65–74, ≥75 years), geographic region (Northeast, North Central, South, West), and calendar period corresponding to PCSK9i approval (before or after 24 July 2015). Models were re-estimated within the subgroup of interest to predict testing rates in the post-MI period.
In a secondary analysis, we subset the cohort to patients who experienced a second MI hospitalization in the one-year period following the first MI hospitalization. For this subset, we estimated LDL-C testing rates in three time periods: 1) one year prior to the first MI hospitalization, 2) up to one year between first and second MI hospitalizations, and 3) up to one year following the second MI hospitalization (with censoring for disenrollment or end of data). Due to substantial variability in time between the first and second MI, we computed a summary estimate of the LDL-C testing rate in the inter-MI period (using all available person-time) for comparison with pre-first MI and post-second MI rates.
This study was a secondary analysis of a limited data set and was approved by the Chesapeake Institutional Review Board, which ensured that all data accessed for the study complied with patient data privacy regulations. All statistical analyses were performed using R software, version 3.5.2.11
Results
A total of 389,367 patients were hospitalized for their first MI and met all inclusion criteria for the study cohort (Figure 1). Patients were admitted to the hospital for a median of 3 days (interquartile range [IQR]: 2, 5), with a small percentage either discharged the same day as admission (1.8%) or hospitalized for 14 days or longer (4.1%). In the year following discharge, 17,091 (4.4%) were admitted for a second MI hospitalization. The median time between first and second events was 87 days (IQR: 17, 193), with 32.1% of second events occurring within one month of discharge from the first hospitalization.
 |
Figure 1 Flow chart of inclusion and exclusion criteria to select the study cohort. |
Overall, the majority (60.3%) of cohort patients were aged <65 years, 64.4% were male, and 65.5% were from the South or North Central regions of the US (Table 1). Approximately 38.6% of the cohort had a history of non-MI ASCVD diagnoses. Other common comorbidities were hypertension (42.3%), hyperlipidemia/dyslipidemia (25.8%), and diabetes (24.8%); the prevalence of these conditions was higher in the subset of patients with a second MI. LLT use varied during the pre-MI period, in the month following discharge, and over the remainder of post-MI follow-up (Table 2). In the year leading up to the first MI hospitalization, approximately 35.5% of the cohort had evidence of statin use, with moderate-intensity statins being the most commonly used therapy; few patients used ezetimibe (4.1%) or PCSK9i (<0.1%). In the month following discharge from the first MI hospitalization, 51.3% filled a statin prescription (half of which were high-intensity statins), and very few patients filled prescriptions for ezetimibe (1.6%) or PCSK9i (<0.1%). Over the next 11 months (until one year post-MI), statin use increased to 60.6%, ezetimibe use was similar to the pre-MI period (3.7%), and although remaining rare, PCSK9i use increased to 0.2%.
 |
Table 1 Overall Characteristics of Patients Leading Up to First MI Hospitalization |
 |
Table 2 ASCVD Diagnoses and LLT Use Relative to MI Hospitalizations |
Fewer than half of all cohort patients (39.7%) received an LDL-C test in the year leading up to MI hospitalization, with 6.6% tested in the month prior to incident MI. Observed LDL-C testing rates were higher in the months following discharge from the first MI hospitalization compared to modeled rates (Figure 2). However, overall testing uptake remained relatively low. Only 9.4% of patients received an LDL-C test in the month following discharge, 27.1% by three months, and slightly over half (51.9%) by one year (Figure 3). Among patients with any testing in the post-MI period, 49.6% received only one test, 29.4% had two tests, 13.4% had three tests, and 7.7% had more than three tests. Comparing the entirety of the pre- and post-MI periods, observed rates of LDL-C testing increased from 51.9 (95% CI: 51.7, 52.1) to 84.4 (95% CI: 84.1, 84.6) tests per 1000 patients per month. The first 11 months of the pre-MI period showed a very slight upward trend in testing rates, followed by a steep increase in the month prior and two months following MI hospitalization. For the remainder of the post-MI period, observed rates appeared to stabilize, staying at a consistently higher level than model-predicted rates. Contrasting observed to model-predicted rates for each post-MI interval, rate differences ranged from 13.3 to 65.7 tests per 1000 patients per month, and rate ratios ranged from 1.2 to 2.2 (Table 3).
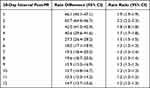 |
Table 3 Rate Differences (Tests per 1000 Patients) and Rate Ratios Contrasting Observed vs Model-Predicted LDL-C Testing Rates |
 |
Figure 2 Observed and model-predicted rates of LDL-C testing in the year before and the year after MI hospitalization in the study cohort. |
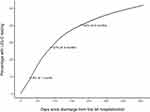 |
Figure 3 Cumulative incidence of LDL-C testing over one year following MI hospitalization, with censoring due to insurance disenrollment. |
In the secondary analysis of patients with a second MI, the rate of LDL-C testing observed between first and second MI (107.1 tests per 1000 patients per month, 95% CI: 102.3, 113.6) was similar to the rates observed in the early intervals post-second MI (eg, rates of 97.9 in first interval, 107.8 in second interval, 93.4 in third interval). Following this increase in rates, testing gradually leveled off. Patients with a second MI also had slightly higher rates of testing in the pre-first MI period (Figure 4), possibly reflecting their higher prevalence of baseline comorbidities.
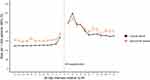 |
Figure 4 Observed rates of LDL-C testing in the overall cohort (pre- and post-first MI) and in the subset with a second MI (pre-first MI, post-second MI). |
In stratified analyses, some variability was observed by age, with the highest rates of testing and largest divergence between observed and model-predicted rates seen in the youngest (<65 years) age group (Figure 5). Results were similar across sex, region, and calendar period (Supplemental Figure 1).
 |
Figure 5 Observed and model-predicted rates of LDL-C testing rates by age group. |
Discussion
Using real-world data from a large commercially insured population, we found that rates of LDL-C testing increased following an incident MI hospitalization but remained lower than recommended by clinical guidelines. Testing rates began to diverge from pre-MI trends in the month leading up to hospitalization and into the first few months after discharge. Rates then remained slightly elevated throughout the one year of follow-up compared to model-predicted rates had no MI occurred. However, only one in four patients (27%) received an LDL-C test in the 90 days following discharge, and only one in two patients (52%) had at least one test within one year. Trends were similar for patients who experienced a recurrent MI within one year of the first hospitalization. In subgroup analyses, age appeared to have the most variation in testing, with patients 65 years of age and older having a lower rate of testing compared to those younger than 65.
Historically, cholesterol treatment guidelines have determined cardiovascular risk using scores based on a combination of LDL-C levels, existing cardiac conditions, and other risk factors (eg, cigarette smoking, hypertension). The recommendation for those with higher scores has traditionally been to use LLT (in addition to lifestyle interventions) until an LDL-C target is achieved.12 In practice, these goals can be challenging to achieve.13–15 Due to lack of robust evidence of clinical benefit, the 2013 ACC/AHA cholesterol treatment guidelines removed specific LDL-C treatment targets.3 However, the European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) treatment guidelines maintained LDL-C goals,16,17 and the 2018 American Heart Association (AHA)/American College of Cardiology (ACC)/Multi-Society cholesterol treatment recommended LDL-C thresholds for very high risk patients with ASCVD.4 Regardless of whether LLT regimens are titrated to specific LDL-C goals or thresholds, routine testing remains a key strategy for improving cardiovascular outcomes of high-risk patients.4,18
Our results highlight a potential gap in care, given this importance of LDL-C monitoring to inform treatment decisions and reduce the risk of future ASCVD events.4,18 Cholesterol treatment guidelines recommend high-intensity statin use (or maximally tolerated statin therapy) following MI and to consider the addition of a non-statin (such as ezetimibe or PCSK9i) for further lowering of LDL-C and subsequent cardiovascular risk reduction.4 If these guidelines translate to practice, LLT use should be near-universal after a MI hospitalization, with an LDL-C test 4 to 12 weeks after treatment initiation and follow-up testing every 3 to 12 months. Our study showed infrequent LDL-C testing and potentially suboptimal use of statins, ezetimibe, and PCSK9i in this high-risk population. Only half filled a statin prescription within one month of discharge, high-intensity statin use was observed for just one-third of the cohort by one year, and use of ezetimibe or PCSK9i remained rare. Despite the inclusion of more recent data (following the 2013 and 2018 releases of ACC/AHA guidelines), our results are consistent with previous studies showing that LDL-C testing and statin use remain much lower than clinical guidelines recommend.9,19–21
Possible explanations for our study findings include both physician- and patient-related factors. Physicians might not order LDL-C tests and initiate or intensity LLT due to lack of knowledge of guideline recommendations,22 underlying beliefs or biases regarding LDL-C goals and statin use,23 and clinical inertia.24 Even if physicians do order tests or prescribe LLT, patients may not complete follow-up due to the presence of clinical comorbidities, as suggested by the lower testing rates observed among older adults. Although all patients in this study had insurance coverage, financial barriers could also contribute to low LDL-C testing and suboptimal statin use. Recent work has found increases over time in the proportions of insured patients with cardiovascular disease who report they are unable to see a physician or receive recommended testing due to cost.25
Although LDL-C testing rates were lower than expected, the MI hospitalization did appear to trigger improved monitoring of lipids in the following year, particularly for the first few months from discharge. Interestingly, our results showed that this increase in testing rates began in the month leading up to hospitalization, sharply diverging from pre-existing trends. To our knowledge, this has not been reported in prior studies of LDL-C testing. A possible explanation may be that some patients present to a physician with chest pain, receive a lipid panel (including LDL-C testing), and are hospitalized for a MI soon thereafter. Rates of other ASCVD diagnoses and chest pain consultations are known to dramatically increase in the months prior to MI,26 which is consistent with baseline data on the study population. For example, among the 19,618 patients (5.0% of cohort) with an unstable angina diagnosis in the year before first MI, over half (10,935 patients; 2.8% of cohort) had this diagnosis in the month leading up to hospitalization. The rise in LDL-C testing in the month prior and further increases to rates following hospitalization – although not as high as expected – provide encouragement that the MI served as an opportunity for more regular LDL-C monitoring in some subsets of the study population.
Taken together, our findings provide important context for improving LDL-C testing and LLT use in a high-risk population that is likely to benefit from treatment modifications (eg, intensifying statin therapy or adding a non-statin). Strengths of this study were the inclusion of a large population of US adults over the last decade and the use of a counterfactually motivated approach to model changes to LDL-C testing, accounting for seasonal trends and loss to follow-up. Given that our study relied on commercial claims data to identify all variables, we minimized measurement error through use of validated algorithms to define variables when available, and LDL-C testing was identified with the CPT and HCPCS codes used in our prior research.8
Importantly, however, our findings represent a specific population (with employer-based insurance or Medicare supplemental insurance) and may not generalize to populations with other insurance coverage or who are uninsured. We could access only the dates of LDL-C testing, not lab values, and data on underlying lipid levels would have augmented our analysis by confirming that low testing rates were not simply due to well-controlled lipid levels. However, other studies have shown that lipid levels remain high following a myocardial infarction and that patients often do not receive statin therapy of adequate intensity.27–29 We also note that our study did not capture all LLT, instead focusing on statins, ezetimibe, and PCSK9i. Another limitation is that death could not be directly ascertained from the database, and some of the censoring events over follow-up (due to disenrollment) may have in fact resulted from death (rather than switching insurance plans). Censoring these patients could then overestimate LDL-C testing rates in the post-MI period if death, a competing event, was common. However, the proportion of patients censored during one year of follow-up was relatively low (88% of cohort continuously enrolled for at least half of post-MI period; 73% observed for the entirety of follow-up), making it unlikely that significant bias would result.
Conclusions
In conclusion, this study found that a MI hospitalization leads to an increase in LDL-C testing in the year after discharge, but overall testing rates remain low. This highlights the need for further improvements in lipid monitoring to maximize appropriate use of LLT. The frequency of LDL-C testing, use of LLT, and risk of ASCVD events are clearly interconnected, and disentangling these relationships (eg, estimating the effect of regular LDL-C testing on the risk of ASCVD events) is an important topic for future research. Our results shed light on the magnitude and duration of increased testing following an acute event and the patient subgroups in which regular monitoring is more common. An incident MI hospitalization provides an opportunity to engage the patient in appropriate care, more closely monitor and control lipids, and ultimately reduce the risk of cardiovascular morbidity and mortality.
Data Sharing Statement
Study data are available for purchase from IBM Corp. Readers can request R code for study analyses from the corresponding author.
Ethics Approval
This study was approved by the Chesapeake Institutional Review Board.
Acknowledgment
Portions of this study were presented at the European Society of Cardiology Congress 2021 as an oral presentation with interim findings.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This work was funded by Amgen, Inc.
Disclosure
S.N Levintow reports a contract from Amgen, Inc. to fund this study. S.R. Reading is an employee and stockholder of Amgen, Inc. S. Noshad was an employee and stockholder of Amgen, Inc. during the conduct of this study. S.E. Mayer has no competing interests to report. C. Wiener is an employee and owns equity in NoviSci, Inc./Target RWE. B. Eledath is an employee and owns equity in NoviSci, Inc./Target RWE. J. Exter was an employee and stockholder of Amgen, Inc. during the conduct of this study; he is currently an employee and stockholder of Merck & Co., Inc. M.A. Brookhart receives consulting fees and owns equity in NoviSci, Inc./Target RWE. He has served on scientific advisory committees for Amgen, AbbVie, Atara Biosciences, Brigham and Women’s Hospital, NIDDK, and Vertex.
References
1. Cleeman JI. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). J Am Med Assoc. 2001;285(19):2486–2497.
2. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681.
3. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. J Am Coll Cardiol. 2014;63(25):2889–2934. doi:10.1016/j.jacc.2013.11.002
4. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi:10.1016/j.jacc.2018.11.003
5. Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–2397. doi:10.1056/NEJMoa1410489
6. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–1722. doi:10.1056/NEJMoa1615664
7. Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–2107. doi:10.1056/NEJMoa1801174
8. Levintow SN, Reading SR, Saul BC, et al. Lipid testing trends in the US before and after the release of the 2013 cholesterol treatment guidelines. Clin Epidemiol. 2020;12:835–845. doi:10.2147/CLEP.S259757
9. Wang WT, Hellkamp A, Doll JA, et al. Lipid testing and statin dosing after acute myocardial infarction. J Am Heart Assoc. 2018;7:3. doi:10.1161/JAHA.117.006460
10. Muntner P, Orroth K, Mues K, et al. Evaluating a simple approach to identify adults meeting the 2018 AHA/ACC cholesterol guideline definition of very high risk for atherosclerotic cardiovascular disease. Cardiovasc Drugs Ther. 2021;36:475–481.
11. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2021.
12. Expert Panel On Detection, Evaluation, And Treatment Of High Blood Cholesterol In Adults. National Cholesterol Education Program (NCEP) Expert Panel. Executive summary of the third report of the NCEP expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). J Am Med Assoc. 2001;285(19):2486–2497.
13. Halcox JP, Tubach F, Lopez-Garcia E, et al. Low rates of both lipid-lowering therapy use and achievement of low-density lipoprotein cholesterol targets in individuals at high-risk for cardiovascular disease across Europe. PLoS One. 2015;10(2):e0115270. doi:10.1371/journal.pone.0115270
14. Toth PP, Grabner M, Punekar RS, Quimbo RA, Cziraky MJ, Jacobson TA. Cardiovascular risk in patients achieving low-density lipoprotein cholesterol and particle targets. Atherosclerosis. 2014;235(2):585–591. doi:10.1016/j.atherosclerosis.2014.05.914
15. Chinwong D, Patumanond J, Chinwong S, et al. Statin therapy in patients with acute coronary syndrome: low-density lipoprotein cholesterol goal attainment and effect of statin potency. Ther Clin Risk Manag. 2015;23(11):127–136.
16. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. 2016;23(11):NP1–NP96. doi:10.1177/2047487316653709
17. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41(1):111–188. doi:10.1093/eurheartj/ehz455
18. Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316(12):1289–1297. doi:10.1001/jama.2016.13985
19. Booth JN, Colantonio LD, Chen L, et al. Statin discontinuation, reinitiation, and persistence patterns among medicare beneficiaries after myocardial infarction: a cohort study. Circ Cardiovasc Qual Outcomes. 2017;10(10). doi:10.1161/CIRCOUTCOMES.117.003626
20. Colantonio LD, Huang L, Monda KL, et al. Adherence to high-intensity statins following a myocardial infarction hospitalization among medicare beneficiaries. JAMA Cardiol. 2017;2(8):890–895. doi:10.1001/jamacardio.2017.0911
21. Brooks JM, Cook E, Chapman CG, et al. Statin use after acute myocardial infarction by patient complexity are the rates right? Med Care. 2015;53(4):324–331. doi:10.1097/MLR.0000000000000322
22. Virani SS, Pokharel Y, Steinberg L, et al. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol. 2016;10(3):497–504.e4. doi:10.1016/j.jacl.2015.11.002
23. Lowenstern A, Navar AM, Li S, et al. Association of clinician knowledge and statin beliefs with statin therapy use and lipid levels (A survey of US practice in the PALM registry). Am J Cardiol. 2019;123(7):1011–1018. doi:10.1016/j.amjcard.2018.12.031
24. Phillips LS, Branch J, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. doi:10.7326/0003-4819-135-9-200111060-00012
25. Hawks L, Himmelstein DU, Woolhandler S, Bor DH, Gaffney A, McCormick D. Trends in unmet need for physician and preventive services in the United States, 1998-2017. JAMA Intern Med. 2020;180(3):439. doi:10.1001/jamainternmed.2019.6538
26. Herrett E, George J, Denaxas S, et al. Type and timing of heralding in ST-elevation and non-ST-elevation myocardial infarction: an analysis of prospectively collected electronic healthcare records linked to the national registry of acute coronary syndromes. Eur Hear J Acute Cardiovasc Care. 2013;2(3):235–245. doi:10.1177/2048872613487495
27. Schubert J, Lindahl B, Melhus H, et al. Low-density lipoprotein cholesterol reduction and statin intensity in myocardial infarction patients and major adverse outcomes: a Swedish nationwide cohort study. Eur Heart J. 2021;42(3):243–252. doi:10.1093/eurheartj/ehaa1011
28. Ray KK, Molemans B, Schoonen WM, et al. EU-Wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2021;28(11):1279–1289. doi:10.1093/eurjpc/zwaa047
29. Schleyer T, Hui S, Wang J, et al. Quantifying unmet need in statin-treated hyperlipidemia patients and the potential benefit of further LDL-C reduction through an EHR-based retrospective cohort study. J Manag Care Spec Pharm. 2019;25(5):544–554. doi:10.18553/jmcp.2019.25.5.544
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
