Back to Journals » International Medical Case Reports Journal » Volume 12
Lemierre Syndrome. A Forgotten Disease. Case Report and Review of Literature
Authors Pokharel A , Basnet P, Sharma B, Thapa K
Received 10 June 2019
Accepted for publication 16 November 2019
Published 29 November 2019 Volume 2019:12 Pages 367—371
DOI https://doi.org/10.2147/IMCRJ.S218895
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Apar Pokharel,1 Prabhat Basnet,2 Bibek Sharma,1 Kripesh Thapa2
1Department of Otorhinolaryngology and Head and Neck Surgery, College of Medical Sciences, Chitwan, Nepal; 2Department of Radiodiagnosis, College of Medical Sciences, Chitwan, Nepal
Correspondence: Apar Pokharel
Department of Otorhinolaryngology and Head and Neck Surgery, College of Medical Sciences, Chitwan, Nepal
Tel +9779841558234
Email [email protected]
Introduction: Lemierre syndrome is a serious condition that associates oropharyngeal infection and thrombosis of the internal jugular vein (IJV) with subsequent distant septic emboli, most frequently in the lungs.
Case presentation: A 70-year-old female with retropharyngeal abscess developed features of Lemierre syndrome. The condition was managed with serial aspiration of the abscess and prolonged usage of intravenous antibiotics.
Discussion: Lemierre syndrome is most frequently caused by the anaerobic bacterium, Fusobacterium necrophorum. Although rare, there is evidence of a resurgence in the condition in recent years, most probably due to reduced use of antibiotic therapy for sore throats. Although there is a characteristic clinical picture, many clinicians are unaware of this condition, leading to delayed diagnosis with potentially fatal consequences.
Conclusion: Early diagnosis of this condition and prompt treatment with intravenous broad spectrum antibiotics results in a complete resolution of this condition. Surgery is indicated in the case of abscess formation.
Keywords: Lemierre syndrome, Fusobacterium necrophorum, septic thrombophlebitis, retropharyngeal abscess
Introduction
The first description of anaerobic septicemia or necrobacillosis was by Courmont and Cade in 1900.1 In 1936, Andre Lemierre first published a case series of 20 patients having anaerobic septicemia secondary to oropharyngeal infection with cervical extension and multiple pulmonary abscess.2 These features were reported under the name of Lemierre syndrome. The infection first occurs in the throat and spreads via septic thrombophlebitis of the tonsillar vein and internal jugular vein. The impending bacteraemia is complicated by septic emboli to different parts of the body like lung, joints, and bones. The most frequent site of involvement is the lungs. The frequently isolated pathogen is Fusobacterium necrophorum. In the antibiotic era, the incidence and mortality of this disease had drastically reduced. Now-a-days, Lemierre syndrome is not a well-known illness because of its rarity.3
We report a 70-year-old female diagnosed with Lemierre syndrome with retropharyngeal abscess, and this resulted in thrombophlebitis of the internal jugular vein and metastatic septic emboli in the lungs. Written informed consent was taken from the patient to report this case along with the photographs. Approval from the Institutional Review Board of College of Medical Sciences, Chitwan, Nepal, was also taken for this case report.
Case Presentation
A 70-year-old female came to the emergency department with the chief complaints of sore throat for 7 days. The pain was continuous and was radiating to the left ear and the left side of the neck. The pain was aggravated by swallowing both solid and liquid diet. The pain was also aggravated by neck movements. The patient complained of a severe headache and neck stiffness. The patient was also having fever for the same duration. There was no change in the patient voice. There was no breathing difficulty (Figure 1). The patient was on Amoxycillin-Clavulanic acid (625mg three times a day for 1 week) for suspected streptococcal pharyngitis. However, her relatives were concerned as the fever and sore throat were not improving despite medications.
 |
Figure 1 Lemierre syndrome patient with neck stiffness, cervical lymphadenopathy and tenderness along the course of external jugular vein. |
On examination, the patient was alert and conscious with no signs of respiratory distress. The patient had high fever. Her temperature was 39.8°C. Her general physical examination was normal. On chest examination, bilateral crepitation with bronchial breath sounds was heard. Examination of her cardiovascular system, abdomen and skin were normal. Ear examination showed normal tympanic membrane with no mastoid tenderness bilaterally. On the oral cavity examination, the posterior pharyngeal wall was erythematous with a minimal bulge. The uvula was in midline. There was no evidence of facial nerve palsy nor trismus. On neck examination, tender lymph nodes were palpable in cervical level 1b and 2. Upon physical examination, the left external jugular vein had become a palpable strand with severe tenderness.
The blood picture showed a total white blood cell count of 30,930/mm3 with left shift and consisted of 92% neutrophils. The C-reactive protein (CRP) was abnormally elevated (13mg/L). The serum electrolytes were within normal limits. She was a patient of diabetes and her blood glucose control was poor with HbA1C of 12.8. The blood culture was done in Brain Heart Infusion (BHI) broth. It did not show any growth. Lumbar puncture was done but it was negative for meningitis. Urine analysis was negative for any signs of infection. Sputum culture showed Enterobacter species sensitive to gentamicin, meropenem and levofloxacin. X-ray neck anteroposterior and lateral view showed increase in prevertebral shadow at the 4th cervical vertebral region. Cervical lordosis was lost. Diffuse pulmonary infiltrates were present (Figure 2). To rule out deep neck abscess, computed tomography of the neck and chest with intravenous contrast was done. CT scan showed peripheral enhancing collection in the neck in the prevertebral region measuring approximately 10×2 cm and extending from C4 to T3 region. Nasopharynx, oropharynx and hypopharynx appeared normal. The left internal jugular vein showed filling defect extending from the jugular foramen to the common jugular confluence, suggestive for high-grade partial occlusion due to thrombus formation. The cavitary lesion was seen in the left lower lobe of the lung peripherally due to metastatic septic emboli. Bilaterally, multiple nodules were seen in the lung with mild pleural effusion (Figures 3–5).
 |
Figure 2 X-ray AP and lateral view of the neck showing increase in prevertebral shadow at 4th cervical vertebral region. Cervical lordosis is lost. Diffuse pulmonary infiltrates present. |
 |
Figure 3 CECT neck showing peripheral enhancing hypodense area in the prevertebral space compressing trachea and oesophagus. |
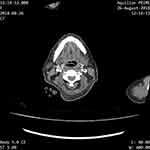 |
Figure 4 CECT neck showing non-occluding filling defect in left internal jugular vein. |
 |
Figure 5 Axial CECT lung window showing well-defined subpleural nodules with central cavity and feeding vessel. Minimal bilateral pleural effusion noted. |
The patient was kept on intravenous meropenem (1gram 8 hourly via intravenous route), metronidazole (500mg 8 hourly via intravenous route) and gentamicin (80mg 8 hourly via intravenous route). The pus in the retropharyngeal space was aspirated by inserting a 10-ml syringe through the oral cavity into the posterior pharyngeal wall. Around 10ml of pus was aspirated. Daily aspiration was done. There was no pus collection on the fourth day. The pus was sent for culture and sensitivity. However, no growth was seen. Anticoagulation therapy with enoxaparin (40mg subcutaneous injection once a day) was also started to the patient. The intravenous antibiotic treatment was given for two weeks. The patient’s condition gradually improved. After two weeks, the patient was discharged on a six weeks course of oral antibiotics and anticoagulation. The antibiotics given were Levofloxacin (500mg once a day) and Clindamycin (300mg three times a day) and the anticoagulant used was warfarin (1mg once a day orally for 6 weeks). On the follow-up visit, the patient was doing well. The patient was followed up to 3 months. She was doing perfectly well.
Discussion
Lemierre syndrome is often characterized by acute oropharyngeal infection, suppurative thrombophlebitis of the internal jugular vein, sepsis and occasionally metastatic septic embolus to different parts of the body, most frequently to lungs. During Lemierre’s time, the diagnosis was made based on clinical findings as Lemierre himself had pointed out:
[...] The appearance and repetition several days after the onset of a sore-throat [...] of severe pyrexial attacks with an initial rigor, or still more certainly the appearance of pulmonary infarcts and arthritic manifestations, constitute a syndrome so characteristic of that mistake is almost impossible [...].2
Since the advent of antibiotics, the prevalence of this disease had dramatically decreased. It is believed that the widespread use of penicillin for oropharyngeal infection is responsible for the dramatic decrease in the incidence with this condition.4 The decrease in the prevalence of this condition had resulted in the waning exposure and familiarity to this condition. Morbidity and potential mortality associated with this condition warrants a review of the literature and its management to facilitate prompt diagnosis and treatment.
In this case report, the patient developed Lemierre disease despite getting oral antibiotics. This might be due to her poorly controlled blood sugar level which contributed to the propagation of a suspected streptococcal pharyngitis into Lemierre disease. The time difference between oropharyngeal infection to onset of septicemia is usually 1 week. The hallmark of this syndrome is thrombophlebitis of the internal jugular vein (IJV). The clinical evidence of IJV thrombophlebitis is progressive severe neck pain at an angle of the mandible and along the anterior border of the sternocleidomastoid muscle. The clinical findings must always be confirmed radiologically. Contrast-enhanced CT scan of the neck will reveal distended internal jugular veins with enhancing wall, low attenuation intraluminal filling defects, and swelling of the adjacent soft tissues. It also differentiates a thrombosed IJV from cervical lymphadenitis.5
There are different hypothesized mechanisms for the spread of oropharyngeal infection leading to IJV thrombosis. Oropharyngeal infection can cause thrombophlebitis of tonsillar veins which can propagate thrombus formation in the internal jugular vein. Direct extension of the infection through the fascial planes can also cause thrombophlebitis of the IJV. Once the infection reaches IJV, it will lead to phlebitis, thrombophlebitis and subsequently septic thromboembolic metastasis. The most common site for septic embolus is lungs. However, other sites like joints, bone, meninges, and liver are also reported in the literature.6 In the Lemierre report, septic embolus was seen in all cases.2 Sinave et al reported pleuropulmonary septic emboli in 97% of the cases.7 Dyspnea, pleuritic chest pain and hemoptysis are common presentations when the lung is involved.8
Fusobacterium necrophorum is the primary pathogen in Lemierre disease. Other causative organisms isolated in Lemierre disease include Streptococcus species, Bacteroides species, Peptostreptococcus species and Eikenella corrodens.7
Treatment of this condition depends on the severity of the infection. IJV thrombosis without thrombus propagation or septic emboli formation should be treated with intravenous antibiotics. While giving antibiotic therapy, close observation for the signs of continued sepsis, propagation of thrombus and septic emboli formation is vital.7 If deep neck abscess is present, surgical drainage should be considered. If the patient continues to have continuous sepsis or repeated septic embolus to the lung, surgical ligation or excision of the IJV should be performed.9 Anticoagulation therapy is reserved for a select group of patients who do not respond to initial antibiotic therapy or if there is a progression of thrombosis or retrograde cavernous sinus thrombosis.10
Conclusion
Lemierre disease is suppurative thrombophlebitis of internal jugular vein secondary to oropharyngeal infection and can be complicated by septic pulmonary emboli. The diagnosis can be confirmed by CT or MRI. Early diagnosis and prompt treatment with long term, high dose intravenous antibiotics with beta-lactamase anaerobic activity results in complete resolution of the condition.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Courmont P, Cade A. Sur une septico-pyohemie de l'homme simulant la peste et causee par un streptobacille anaerobie [Septico-pyaemia simulating human plague caused by a bacillus anaerobic streptococci]. Arch Med Exp Anat Pathol. 1900;4:17–28.
2. Lemierre A. On certain septicaemias due to anaerobic organisms. Lancet. 1936;227(5874):701–703. doi:10.1016/S0140-6736(00)57035-4
3. Sara Z, Beard G, Furey W. Insight into a forgotten disease: Lemierre’s syndrome. Resid Staff Physician. 2005;51:37–40.
4. Bartlett JG, Gorbach SL. Anaerobic infections of the head and neck. Otolaryngol Clin North Am. 1976;9(3):655.
5. Albertyn LE, Alcock MK. Diagnosis of internal jugular vein thrombosis. Radiology. 1987;162(2):505–508. doi:10.1148/radiology.162.2.3541033
6. Yau PC, Norante JD. Thrombophlebitis of the internal jugular vein secondary to pharyngitis. Arch Otolaryngol Chic Ill 1960. 1980;106(8):507–508. doi:10.1001/archotol.1980.00790320059016
7. Sinave CP, Hardy GJ, Fardy PW. The Lemierre syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Medicine (Baltimore). 1989;68(2):85–94. doi:10.1097/00005792-198903000-00002
8. Vogel LC, Boyer KM. Metastatic complications of Fusobacterium necrophorum sepsis: two cases of Lemierre’s postanginal septicemia. Am J Dis Child. 1980;134(4):356–358. doi:10.1001/archpedi.1980.04490010014005
9. Moreno S, Altozano JG, Pinilla B, et al. Lemierre’s disease: postanginal bacteremia and pulmonary involvement caused by Fusobacterium necrophorum. Rev Infect Dis. 1989;11(2):319–324. doi:10.1093/clinids/11.2.319
10. Lu MD, Vasavada Z, Tanner C. Lemierre syndrome following oropharyngeal infection: a case series. J Am Board Fam Med. 2009;22(1):79–83. doi:10.3122/jabfm.2009.01.070247
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
