Back to Journals » Risk Management and Healthcare Policy » Volume 17
Leading Causes of In-Hospital Death of Older Patients of Different Age Groups in Shanghai
Received 30 November 2023
Accepted for publication 21 February 2024
Published 1 March 2024 Volume 2024:17 Pages 435—453
DOI https://doi.org/10.2147/RMHP.S450864
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Yu Gong,1,* Qianxia Liu,2,* Qiang Hu3
1Department of Internal Medicine, Division of Nephrology, Telemedicine Center, Shanghai Municipal Eighth People’s Hospital, Shanghai, People’s Republic of China; 2Department of Medical Affairs Management, Division of Medical Record Management, Shanghai Municipal Eighth People’s Hospital, Shanghai, People’s Republic of China; 3Department of Surgery, Shanghai Municipal Eighth People’s Hospital, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yu Gong, Department of Internal medicine, Division of Nephrology, Telemedicine Center, Shanghai Municipal Eighth People’s Hospital, 8 Caobao Road, Shanghai, 200235, People’s Republic of China, Email [email protected] Qiang Hu, Department of Surgery, Shanghai Municipal Eighth People’s Hospital, 8 Caobao Road, Shanghai, 200235, People’s Republic of China, Email [email protected]
Background: Despite great achievements in clinical medicine, the in-hospital mortality of older patients remains high. How to reduce the in-hospital mortality of older inpatients is of great clinical value in clinical practice. This study is to analyze the leading causes of in-hospital death of older inpatients of different ages in Shanghai.
Methods: An observational study was conducted in Shanghai. A total of 3894 older inpatients (≥ 60 years old) were investigated. According to the age stratification standard of World Health Organization, they were divided into young older patients group (aged 60 to 74), old older patients group (aged 75 to 89) and very old patients group (aged ≥ 90). Diseases of in-hospital death of older inpatients in different age groups were classified according to the 10th edition of the International Classification of Diseases. Constituent ratio of causes of in-hospital death in each group was analyzed.
Results: The constituent ratio of pulmonary infection had the highest rate of in-hospital death in older patients. The constituent ratio of lung malignant tumors had the highest rate of in-hospital death in young older patients. The constituent ratio of pulmonary infection had the highest rate of in-hospital death in old older patients. The constituent ratio of pulmonary infection had the highest rate of in-hospital death in very old patients.
Conclusion: The leading cause of in-hospital death of young older patients group was lung malignant tumor. The leading cause of in-hospital death of old older patients group and very older patients group was pulmonary infection. Great importance should be attached to the prevention of lung tumor and lung infection in the elderly. Results of this study will provide a basis for health administrative departments to formulate corresponding health-care policies for older patients.
Keywords: causes of in-hospital death, older patients, age stratified analysis, lung malignant tumor, pulmonary infection
Introduction
Despite great achievements in clinical medicine, mortality of older patients remains high. The number of aging population has increased significantly which caused huge disease and economic burden. With the improvement of living standards including nutritional status and dietary structure, people’s average life expectancy has been generally prolonged. In the inpatient population, the number of older patients has increased significantly. How to reduce the in-hospital mortality of older inpatients is of great clinical value in clinical practice. Researches on the causes of death of older inpatients have been conducted in several countries.1–8 They studied the main diseases that lead to the death of older patients in different countries and found that malignant tumors of lung, pneumonia and bronchopneumonia were the leading causes of death of older patients. However, little is known about the cause of death in older inpatients of different age groups.
For older patients of different age groups, due to the different ages of each older patient, their function of immune system, function of main organs and body health status are different. Different age groups of older patients have different clinical characteristics and outcomes for the same disease. Therefore, it is necessary to conduct research to identify the main diseases leading to the death of older patients of different age groups.
Human beings have entered an aging society. How to improve the quality of life of the elderly and extend their life span is a very important problem that medical workers need to solve. Identifying the leading cause of in-hospital death of older inpatients of different age groups can improve the treatment level of older patients and reduce the mortality of older patients. It is of great value to conduct research on causes of in-hospital death of older inpatients of different age groups. This study is to analyze the leading cause of in-hospital death of older inpatients of different age groups in the central urban area of Shanghai. Results of the study can strengthen the prevention and treatment of diseases that lead to the death of older patients of different age groups, reduce the mortality rate and improve the quality of life of elderly patients of all age groups. The results will provide a basis for health administrative departments to formulate corresponding medical and health-care policies for older patients.
Methods
A retrospective study was conducted from July 1, 2013 to December 30, 2019 in a university affiliated hospital in the central urban area of Shanghai. A consecutive sample of 3894 older inpatients (aged ≥60) (mean age 80.51 ± 9.31 years old) was investigated by using the medical record management system of the hospital. The subject inclusion and exclusion criteria: older inpatients lived and worked in the central urban area of the mega city for over 60 years were included in this study. Older inpatients lived and worked in the central urban area of Shanghai less than 60 years and older inpatients did not live and work in the central urban area of Shanghai were excluded from the study.
Among these 3894 older inpatients, 2125 were males and 1769 were females. They were divided into young older patients group (aged 60 to 74), old older patients group (aged 75 to 89) and very old patients group (aged ≥90) according to the most recent age stratification for older people as defined by World Health Organization (WHO). Socio-demographic variables of these 3894 older inpatients, young older patients, old older patients and very old patients are shown in Table 1. The constituent ratios of causes of in-hospital death in older inpatients of different ages were analyzed by age stratification. All diseases that cause in-hospital death in older inpatients were classified according to the 10th edition of the International Classification of Diseases (ICD-10). Constituent ratio of death etiology of older inpatients in each age group was statistically analyzed. The causes of in-hospital of older inpatients in three age groups were analyzed.
Statistical Analyses
By using the IBM SPSS Statistics Version 20.0 (IBM Inc., Chicago, USA), statistical analysis of the study data was performed. Continuous variables were analyzed by Student’s t-test and expressed as the mean ± standard deviation (x±s) or median and interquartile range. Categorical variables were analyzed by chi-square test or Fisher’s exact test. p value < 0.05 was considered statistically significant.
The protocol for this research project has been approved by the Ethics Committee of Shanghai Municipal Eighth People’s Hospital, and the approval number is 2019–006. It conforms to the provisions of the Declaration of Helsinki in 1975 (as revised in Edinburgh 1983). Informed, written consent was obtained from every patient.
Results
In this study, a total of 3894 older inpatients (aged ≥60) were investigated. The average age was 80.51 ± 9.31 years, including 2125 males and 1769 females. The top 5 diseases of death in older inpatients were pulmonary infection, lung malignant tumors, chronic obstructive pulmonary disease, coronary heart disease, and gastric malignant tumors. The constituent ratio of the top 5 diseases was 13.8%, 7.5%, 7.3%, 6.0% and 5.9%, respectively (see Table 2).
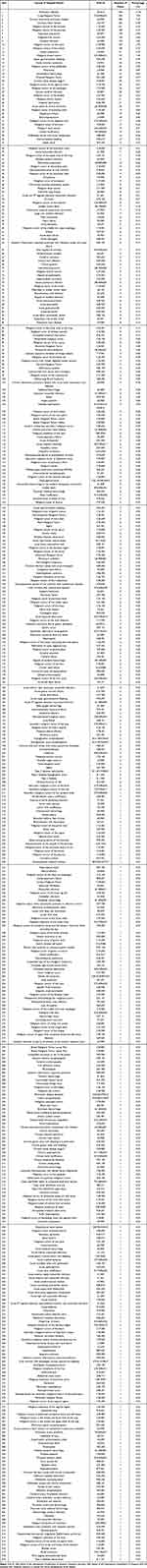 |
Table 2 Etiological Analysis of In-Hospital Death of Older Inpatients (≥60 Years Old) in Central Urban Areas of Shanghai |
The average age of young older patients group was 67.89 ± 4.65 years old, 689 males and 382 females. The top 5 diseases of death in young older patients group were lung malignant tumors, gastric malignant tumors, pancreatic malignant tumors, liver malignant tumors and pulmonary infection. The constituent ratio of the top 5 diseases was 12.2%, 11.3%, 6.9%, 6.8% and 5.2%, respectively (see Table 3).
 |
Table 3 Etiological Analysis of In-Hospital Death of Young Older Patients Group (Aged 60 to 74) in Central Urban Areas of Shanghai |
The average age of old older patients group was 83.24 ± 3.66 years old, 1186 males and 1037 females. The top 5 diseases of death in old older patients group were pulmonary infection, chronic obstructive pulmonary disease, coronary heart disease, lung malignant tumor and gastric malignant tumors. The constituent ratio of the top 5 diseases was 17.1%, 9.0%, 7.0%, 6.9% and 4.5%, respectively (see Table 4).
 |
Table 4 Etiological Analysis of In-Hospital Death of Old Older Patients Group (Aged 75 to 89) in Central Urban Areas of Shanghai |
The average age of very old patients group was 92.92 ± 2.79 years old, 250 males and 350 females. The top 5 diseases of death in very old patients group were pulmonary infection, chronic obstructive pulmonary disease, coronary heart disease, aspiration pneumonia and cerebral infarction. The constituent ratio of the top 5 diseases was 27.0%, 10.7%, 10.0%, 5.0% and 4.3%, respectively (see Table 5).
 |
Table 5 Etiological Analysis of In-Hospital Death of Very Old Patients Group (Aged ≥90) in Central Urban Areas of Shanghai |
Discussion
Human beings have entered an aging society. How to improve the quality of life of the elderly and extend their life span is a very important problem that medical workers need to solve. Different age groups of older patients have different health status and immune function. Identifying the leading cause of in-hospital death of older patients of different age groups can improve the treatment level of older patients. It is of great significance in reducing the mortality of older patients.
Central urban areas of Shanghai are densely populated among which the elderly population accounts for a high proportion and most of them are concentrated. These older patients have high retirement income, good economic conditions and pay more attention to their own health care in their daily life. And there are more large general hospitals in the central urban area of Shanghai, which makes it convenient for the elderly to go to large general hospitals with advanced medical equipment and well-known medical experts. They can have regular physical examination at ordinary times to find diseases in time. If the elderly are sick, they can get timely diagnosis and treatment. But, there is serious air pollution caused by automobile exhaust in the central urban area of super large city. Therefore, older people in the central urban area are more likely to suffer from lung diseases such as malignant tumor and pulmonary infection. The disease spectrum of older people in the central urban area has unique characteristics which is different from that of small and medium-sized cities.
In addition to the long-term lung injury of older patients caused by air pollution, smoking is also the leading cause of lung injury in older male patients in central urban area of mega city. China has high rates of lung cancer due to smoking. According to “China Smoking Hazards Report 2020”, the number of smokers in China exceeds 300 million. The smoking rate among people aged 15 and above is 26.6%, with a high male smoking rate of 50.5% in China. The smoking rate among teenagers is 6.0%, and the attempted smoking rate is 19.9%. Eighty percent of adolescent smokers will continue to smoke in adulthood and find it difficult to quit. According to report statistics, tobacco causes over 1 million deaths in China every year, with over 100,000 deaths due to exposure to second-hand smoke. In the study of Xu et al, it was found that smoking and environmental pollution combine to account for the elevated rates of lung cancer mortality in Shenyang, a mega city in northeast China.9
In the study of Wang et al, it was found that NO2 in the air was significantly associated with the risk of lung cancer, followed by SO2. Air pollutants have the strongest lag effect on the incidence and mortality of lung cancer within 2–3 years.10 Air pollution and smoking are the main reasons for older male patients to suffer from lung infection, lung tumor and chronic obstructive pulmonary disease. Therefore, young male citizens should be encouraged not to develop the unhealthy habit of smoking. Middle aged and elderly male citizens who have formed smoking habits should quit smoking in time. Quitting smoking can significantly reduce the risk of male citizens suffering from lung malignant tumor and pulmonary infection so as to reduce the mortality in older male patients.
In this study, it was found that pulmonary infection is the leading cause of death in old older patients with a constituent ratio of 15.3%, which is significantly higher than other diseases leading to death. Chronic obstructive pulmonary disease was the second cause, and lung malignant tumor was the fourth cause of death in old older patients. Pulmonary infection and chronic obstructive pulmonary disease have increased significantly in recent years. The increase in the number of smokers and the younger age of smokers are the main reasons. Prevention of pulmonary infection is more important than treatment. We should attach great importance to the prevention and treatment of pulmonary infection, especially for old older patients with long-term smoking history, advocate old older patients to quit smoking or minimize smoking.
Older patients are prone to lung infections due to their weakened immune system. Therefore, older patients should engage in physical exercise, enhance their immunity, pay attention to warmth, prevent coldness, and prevent lung infections. For older patients who are bedridden for a long time, it is easy to cause lung infections if the sputum in the lungs cannot be eliminated in a timely manner. It is necessary to strengthen the care of elderly patients, often turning over and patting their backs to help them expel phlegm. When eating, older patients should be careful to avoid choking and coughing to prevent food from entering the lungs which may cause lung infections.
Older patients should pay more attention to a balanced diet, eat more fresh fruits and vegetables, quit smoking and drinking, and avoid long-term exposure to dusty environments to prevent lung infections. If older patients experience uncomfortable symptoms such as coughing and fever, timely treatment should be given to avoid delaying the condition and leading to severe pneumonia, which may cause death in older patients.
Chronic obstructive pulmonary disease (COPD) is the result of the gradual onset of long-term inflammation of chronic bronchitis. This disease has a long course and cannot heal repeatedly which seriously affects the quality of life of older patients. The recurrence of chronic bronchitis should be controlled in the middle age of patients. At the same time, patients in this age group should change the bad living habits of smoking, avoiding the inhalation of second-hand smoke. The recurrence of chronic bronchitis should be controlled in the middle age of patients. It is also very important to control air pollution in the central urban area in Shanghai.
In this study, lung malignant tumor was the fourth cause of death in old older patients group which may be related to air pollution and smoking. Therefore, controlling air pollution and quitting smoking are of great importance for old older patients. We should also pay attention to the prevention and treatment of lung cancer.
In this study, the average age of hospitalized patients in very old patients group was 92.92 ± 2.79 years old, and pulmonary infection was found to be the top 1 cause of death in very old patients group, which was the same as that in old older patients group. More attention should be paid to the prevention of pulmonary infection for very old patients.
In this study, it was found chronic obstructive pulmonary disease was the second cause of death in old older patients and in very old patients group. Therefore, we should take timely and effective treatment measures to treat older patients with pulmonary infection and chronic obstructive pulmonary disease. Clinicians should attach great importance to prevent chronic obstructive pulmonary disease from developing into cor pulmonale and pulmonary encephalopathy which can result in the death of very old patients.
In this study, it was found that aspiration pneumonia is the fourth major cause of in-hospital death of very old patients group. This is because very old patients belong to the older patients in the super older group. Their nervous system function decreases significantly, resulting in insensitive swallowing reflex. It is easy for very old patients to inhale food into the trachea by mistake when eating food and resulting in aspiration pneumonia. The symptoms of aspiration pneumonia are very serious and the very old patient may have high fever, severe cough, and even bacteremia which can result in the death. Therefore, very old patients should pay great attention to avoid mistakenly inhaling food into the respiratory tract when eating. It is a better solution to placing a gastric tube in the patient’s esophagus and injecting food into the patient’s stomach through the gastric tube which can greatly avoid the occurrence of aspiration pneumonia in very old patients. It can improve the quality of life and prolong the life of very old patients. We found this is a very effective measure to prevent aspiration pneumonia in very old patients and may be popularized in daily clinical work of other regions.
Doctors usually decide whether to perform this invasive operation on very old patients after fully evaluating the potential benefits and damages of placing a gastric tube based on the actual situation of very old patients. Placing a gastric tube is mainly used in very old patients with senile dementia who are unable to swallow normally and patients who are unable to eat orally and critically ill individuals. Patients with upper gastrointestinal bleeding, nasopharyngeal cancer, acute inflammation, and heart failure are not suitable for inserting a gastric tube, which can easily worsen the disease. Inserting a gastric tube requires guidance from a doctor to avoid damage to the throat and stomach.
Gee et al conducted continuous autopsy on 3000 older inpatients and found bronchopneumonia and malignant tumors of digestive system and lung were the most common diseases leading to death of these older inpatients.4 They believed that there is an increased frequency of multiple pathological processes in a given subject and interactions play an important role in morbidity and mortality with the advancing age of older inpatients. Brandt et al conducted a prospective study on the diseases leading to the death of older inpatients and evaluated the direct causes of death of all older inpatients in the Netherlands. It was found most older inpatients died of pneumonia.5 They concluded that many older patients spent unconscious or conscious with one or more burdensome symptoms in the last days of life which suggests the potential for improvement of symptom management. The above two findings are the same as our findings. In our study, we found lung infection and lung malignant tumor and COPD are the top three leading causes of death of older inpatients. For old older patients group and very old patients group, pulmonary infection was the leading cause of death.
In the study of Goldberg et al, they studied the causes of the death of older patients in geriatric nursing homes in the United States and found the diseases leading to the death of older patients in geriatric nursing homes are Alzheimer’s/dementia, cardiac/cerebrovascular and pulmonary.6 This research result is different from ours since the geriatric nursing home in the United States is not a formal general hospital. There are less medical experts in various clinical disciplines and advanced medical equipment. Compared with the large-scale general hospital in our study, there is an obvious gap in the treatment level of various elderly diseases and medical equipment. In geriatric nursing homes in the United States, the nursing of older patients is conducted by nurses who cannot meet the medical needs of older patients since they have less clinical experience compared with doctors and nurses in large general hospitals and unable to treat older patients in time.
Abdel-Karim et al studied the causes of death of older patients receiving hospice care in San Antonio, Texas, USA and found pneumonia was the main cause of death of older patients receiving hospice care.7 The results of this study are the same as that of ours because the general condition of older patients who need hospice care is poor and these older patients usually suffered from cancer and other severe diseases with low immunity and mal-nutritional status. So, they are prone to severe lung infections such as pneumonia which can lead to death of these older patients.
In the study of Braggion et al, they conducted research on the diseases that led to the death of 19,392 older patients (≥65 years old) who were hospitalized in the elderly nursing home for a long time in the Veneto region of northeastern Italy. It was found that respiratory diseases and infections were the main causes of death of older patients hospitalized in the elderly nursing home.8 The results of this study are similar to our results because the older patients hospitalized for a long time in the elderly nursing home were in a state of low immune function and usually suffered from various complications. These older patients were prone to respiratory diseases and infections. Ferorelli et al found that the main causes of death of older patients in Italy are cardiovascular diseases and tumors, infectious diseases and parasitic diseases are the third leading causes of death, and the main reason is the high incidence of nosocomial infection in European hospitals.11 Among them, pulmonary infection was the main cause of death in older patients. In the study of Guido et al, they conducted a research on the main causes of death of older patients with COVID-19 (mean age 79.6 ± 0.9 years old). After multivariate analysis, it was showed that older patients with COPD were one of the most common risk factors for mortality of older patients with COVID-19.12 COPD is a chronic disease in the elderly caused by lung infection and inflammation. The results of the study of Guido et al demonstrated that chronic lung infection in the elderly may become one of the main risk factors for mortality of old patients with COVID-19.
Klima et al have studied the causes of death of older patients in the Czech Republic and found that infection and heart disease were the main causes of death of older patients, of which pulmonary infection is the main cause of death of older patients. They especially emphasize the importance of autopsy in identifying the causes of death of older patients.13 This result is similar to that of our study.
In the study of Bordin et al, they analyzed the main causes of death of extreme-aged hospitalized people (aged 97–106 years) in Italy retrospectively and found that pneumonia was the main cause of death of extreme-aged hospitalized people and clinicians significantly underestimated pneumonia on death in extreme-aged hospitalized people.14 The results of this study are similar to our results. In our study, it was found that pulmonary infection was the leading cause of death of very old patients group. This is because very old patients are in a state of hypoimmunity and the defense ability of respiratory tract is low. Once very old patients have pulmonary infection, it is difficult to control due to low immunity and are easy to lead to acute heart failure and acute renal failure which can further lead to multiple organ dysfunction syndrome (MODS) and death of very old patients.
Lung is an internal organ that directly contacts the external environment and is easy to be infected. The risk of pulmonary infection in very old patients is higher than that in young people, especially those very old patients with cardiovascular diseases, diabetes, cancer, and those who are in bed for a long time. If pulmonary infection of very old patients is not controlled timely and effectively, it can develop into severe pneumonia, leading to respiratory failure and death. Very old patients with pneumonia have a high probability of serious complications which is the main reason for the high mortality. If pulmonary infection is not controlled timely and effectively, it can develop into severe pneumonia and lead to respiratory failure and death. So, timely medical treatment should be taken immediately to control pulmonary infection in very old patients. The main treatment of pneumonia is anti-infection. Since the extensive use of antibiotics in recent years, bacteria have developed considerable drug resistance. Pneumococcal vaccination for the elderly can obtain immunity against pulmonary infection which has been considered as an important measure adopted by many developed countries.
Although vaccination against pneumonia is the most effective way to prevent pneumonia of older patients, the vaccination rate of pneumonia vaccine for the older people is relatively low in many countries. The older people have low awareness of pneumonia and have no awareness of the prevention of pneumonia. Older people should be actively vaccinated against pneumonia to prevent pneumonia to protect their health.
In the study of Berzlanovich et al, they studied the causes of death of older inpatients in Vienna, Austria. They found respiratory diseases were the second most common cause of death of older inpatients while urogenital and metabolic diseases are not common.15 This research result is similar to that of ours because Vienna is the capital and the most populous city in Austria. It is the main cultural center in Europe with dense population, which is similar to that of the central urban area in our study. Brook et al studied the causes of death of 1226 older psychiatric patients in the Netherlands and found respiratory diseases are the main cause of death.16 This result is similar to ours. Older psychiatric patients usually have low immunity and poor self-care ability and are prone to pulmonary infection. Although with different ICD-10 code, pulmonary infection, pneumonia, and severe pneumonia are difficult to distinguish in clinic. But they all belong to respiratory diseases. If these three diseases were combined and counted in ICD-10 code of respiratory diseases, it may increase the proportion of respiratory diseases in the study of inpatient deaths in older patients.
In the study of Ang et al, they found that the most common causes of death of non-hospitalized older people in Singapore after discharge are malignant tumors and cerebrovascular diseases.17 The result of this study is different from that of our study. This is because the object of this study is the non-hospitalized older people who were not treated in large general hospital or geriatric nursing homes, so it is impossible to make early diagnosis of tumor and carry timely treatment for the diseases leading to death of older patients. Therefore, malignant tumors and cerebrovascular diseases became the main causes of death for the non-hospitalized elderly in Singapore.
The above clinical studies were carried out in economically developed countries in Europe and Asia. They analyzed the causes of death of elderly patients in economically developed countries. Their research results were similar to ours. Pulmonary infection and cardiovascular disease are the main causes of death of older inpatients. This is because our research is carried out in the central urban area of mega city. The current economic development level and people’s living standard are the same as those of developed countries. However, compared with the developing countries, the main causes of death of older patients are significantly different and require further research. In the study of Alam et al, they studied the causes of death of older patients (≥60 years old) in a developing country and found that infectious diseases accounted for 18% and non-communicable diseases accounted for 66%. The main non-communicable diseases were circulatory diseases, tumors, respiratory diseases and digestive disease.18 The results of this study were different from ours. This may be mainly because this study was conducted in an economically underdeveloped region with relatively backward medical conditions and relatively poor sanitary conditions. Therefore, infectious diseases account for a high proportion of the causes of death of older patients.
In the study of Olubuyide et al, they conducted a ten-year study on the main causes of the death of older patients (≥60 years old) in a tropical African country (Nigeria) and found that the leading cause of death in older patients is cancer, heart disease and infectious diseases.19 This research result is different from ours. This is mainly because Nigeria is an underdeveloped country in Africa. The proportion of total national health expenditure in gross domestic product (GDP) is low, and the health-care system is imperfect. Therefore, cancer, heart disease and infectious diseases are the main causes of death in older patients. This may be due to the differences in economic development and the level of health-care system among different countries.
In the study of Huang et al, it was found that hypochloremia is mildly common in patients with coronary artery disease and is associated with increased short- and long-term mortality.20 In clinical practice, hypochloremia is generally not given enough attention by clinical doctors. This study found that hypochloremia increased short- and long-term mortality of patients. This is an important clinical research result with significant clinical value. Clinicians should attach great importance to the treatment of hypochloremia to avoid patients dying due to hypochloremia.
We analyzed the results of our study with other studies from other countries mentioned above and found some valuable results. It was found that lung malignant tumor and pulmonary infection including pneumonia were the leading cause of death of older patients, as shown in Table 6.
 |
Table 6 Comparison of Leading Causes of In-Hospital Death of Older Patients Between the Results in Our Study and Other Studies in Other Countries |
There are some limitations in this study. This study is a single-center study with a relatively small number of older patients and a relatively short observation time. More patients of multiple centers and longer observation time will be conducted in the future.
Conclusions
Lung malignant tumor was found to be the leading cause of in-hospital death of young older patients, and pulmonary infection was the leading cause of in-hospital death of old older patients and very old patients in central urban area of Shanghai. Great importance should be attached to the prevention of lung tumor and lung infection in the elderly. Results of this study will provide a basis for health administrative departments to formulate corresponding health-care policies for older patients. This study is a single-center study with a relatively small number of patients. Studies with more patients of multiple centers will be conducted in the future.
Funding
This work was supported by the Shanghai Municipal Xuhui Medical Research Project Fund [grant number SHXH201957].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Aronow WS. Clinical causes of death of 2372 older persons in a nursing home during 15-year follow-up. J Am Med Dir Assoc. 2000;1(3):95–96.
2. Cordeiro P, Martins M. Hospital mortality in older patients in the Brazilian unified health system, Southeast region. Rev Saude Publica. 2018;69. doi:10.11606/S1518-8787.2018052000146
3. Adebusoye LA, Owolabi M, Ogunniyi A. Predictors of mortality among older patients in the medical wards of a tertiary hospital in Nigeria. Aging Clin Exp Res. 2019;31(4):539–547. doi:10.1007/s40520-018-0997-7
4. Gee WM. Causes of death in a hospitalized geriatric population: an autopsy study of 3000 patients. Virchows Arch a Pathol Anat Histopathol. 1993;423(5):343–349. doi:10.1007/BF01607146
5. Brandt HE, Ooms ME, Deliens L, et al. The last two days of life of nursing home patients--a nationwide study on causes of death and burdensome symptoms in the Netherlands. Palliat Med. 2006;20(5):533–540. doi:10.1191/0269216306pm1164oa
6. Goldberg TH, Botero A. Causes of death in older nursing home residents. J Am Med Dir Assoc. 2008;9(8):565–567. doi:10.1016/j.jamda.2008.04.011
7. Abdel-Karim IA, Sammel RB, Prange MA. Causes of death at autopsy in an inpatient hospice program. J Palliat Med. 2007;10(4):894–898. doi:10.1089/jpm.2006.0240
8. Braggion M, Pellizzari M, Basso C, et al. Overall mortality and causes of death in newly admitted nursing home residents. Aging Clin Exp Res. 2020;32(2):275–280. doi:10.1007/s40520-019-01441-x
9. Xu ZY, Blot WJ, Xiao HP, et al. Smoking, air pollution, and the high rates of lung cancer in Shenyang, China. J Natl Cancer Inst. 1989;81(23):1800–1806. doi:10.1093/jnci/81.23.1800
10. Wang W, Meng L, Hu Z, et al. The association between outdoor air pollution and lung cancer risk in seven eastern metropolises of China: trends in 2006–2014 and sex differences. Front Oncol. 2022;12:939564. doi:10.3389/fonc.2022.939564
11. Ferorelli D, Donno F, De Giorgio G, et al. Study of determinants in deaths occurring in an Italian teaching hospital during a year. Clin Ter. 2020;171(3):e245–252. doi:10.7417/CT.2020.2222
12. Iaccarino G, Grassi G, Borghi C, et al. Age and multimorbidity predict death among covid-19 patients: results of the sars-ras study of the Italian society of hypertension. Hypertension. 2020;76(2):366–372. doi:10.1161/HYPERTENSIONAHA.120.15324
13. Klima MP, Povysil C, Teasdale TA. Causes of death in geriatric patients: a cross-cultural study. J Gerontol a Biol Sci Med Sci. 1997;52(4):M247–253. doi:10.1093/gerona/52A.4.M247
14. Bordin P, Da Col PG, Peruzzo P, et al. Causes of death and clinical diagnostic errors in extreme aged hospitalized people: a retrospective clinical-necropsy survey. J Gerontol a Biol Sci Med Sci. 1999;54(11):M554–559. doi:10.1093/gerona/54.11.M554
15. Berzlanovich AM, Missliwetz J, Sim E, et al. Unexpected out-of-hospital deaths in persons aged 85 years or older: an autopsy study of 1886 patients. Am J Med. 2003;114(5):365–369. doi:10.1016/S0002-9343(03)00049-4
16. Brook OH. Mortality in the long-stay population of Dutch mental hospitals. Acta Psychiatr Scand. 1985;71(6):626–635. doi:10.1111/j.1600-0447.1985.tb02558.x
17. Ang YH, Wong SF, Chan KM. Predictive factors of post-discharge mortality in the hospitalised older. Singapore Med J. 2000;41(3):98–102.
18. Alam N, Chowdhury HR, Bhuiyan MA, et al. Causes of death of adults and older and healthcare-seeking before death in rural Bangladesh. J Health Popul Nutr. 2010;28(5):520–528. doi:10.3329/jhpn.v28i5.6161
19. Olubuyide IO, Solanke TF. The causes of death in an older African population. J Trop Med Hyg. 1990;93(4):270–274.
20. Huang H, Mai Z, Chen L, et al. Prevalence and mortality of hypochloremia among patients with coronary artery disease: a cohort study. Risk Manag Healthc Policy. 2021;14:3137–3145. doi:10.2147/RMHP.S306125
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

