Back to Journals » Journal of Healthcare Leadership » Volume 14
Leadership Curriculum in Medical Education: Exploring Student and Faculty Perceptions in a US Medical School in Qatar
Authors Keluth Chavan A , Bendriss R
Received 7 June 2022
Accepted for publication 27 September 2022
Published 4 October 2022 Volume 2022:14 Pages 163—173
DOI https://doi.org/10.2147/JHL.S370645
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Pavani Rangachari
Akash Keluth Chavan,1 Rachid Bendriss2
1Medical Education, Weill Cornell Medicine-Qatar, Doha, Qatar; 2Premedical Education, Weill Cornell Medicine-Qatar, Doha, Qatar
Correspondence: Rachid Bendriss, Premedical Education Division, Weill Cornell Medicine-Qatar, P.O. Box 24144, Doha, Qatar, Tel +974 4492 8221, Email [email protected]
Purpose: Leadership has long been recognized as a core competency required to excel in medical practice. This qualitative study investigates the extent to which leadership competencies are incorporated in the curriculum of a US medical college in Qatar and examines the perceptions of medical students and faculty about leadership in the medical curriculum.
Methods: The study uses a student survey, faculty interviews, and a student focus group to gather data.
Results: The study found that 79% of the survey respondents perceive leadership as a core competency while 55% feel that leadership skills are not adequately taught to students. The focus group and interviews revealed that students believe more importance should be given to leadership training whereas faculty assert that, while leadership can be beneficial, leadership training is implicit, and more research is required for further implementation.
Conclusion: This study shows the need for an increased emphasis on developing leadership curricula in undergraduate medical education and highlights ways to address certain obstacles to implementation. Further research on exploring medical alumni’s perceptions and optimal teaching methods to implement leadership training is needed.
Keywords: leadership in medical curriculum, leadership training, future doctors, Qatar, medical education
Introduction
Leadership has long been recognized as a core competency required to excel as medical students and physicians.1 In fact, clinicians in leadership positions have been shown to display more credibility and place more emphasis on patient care.2 As a result, multiple research studies and organizational boards have stressed the need to integrate leadership training into medical education.3 Given the strain on the healthcare system caused by the covid-19 pandemic, leadership skills such as ethical decision-making, communication, teamwork, and flexibility have been paramount in dealing with the pandemic.4 However, research points out that there are limited curricula that explicitly develop such leadership skills.4 Rouhani et al point out that there has been an increase in clinicians that have stepped into management and leadership roles, thereby bridging the gap between clinicians and managers.5 Although leadership training is essential for such managerial roles, as Varkey et al put it,
Regardless of career track or field of specialization, physicians function in leadership roles in healthcare teams and are considered to be ultimately responsible for the overall outcomes of patient care.6
A systematic review of the literature revealed that there is yet to be a standardized definition of “clinical leadership”. Such standardization is important since it revolves around developing a framework to evaluate leadership training for further research and improvement across medical schools.7 Moreover, the review points towards the heterogeneous nature of leadership training integration in medical curricula across four countries: the US, Canada, Sweden, and Switzerland. Similar findings are seen from a national survey carried out in 2014 intended to assess leadership education in US allopathic medical schools. The study revealed that approximately half (n = 88) of the medical schools offer formal leadership education. However, the study highlights the considerable variation in program format, student participation, and delivery methods as reported by the survey respondents, who are deans or associate deans for medical education.8
In the UK, the NHS and the Academy of Medical Royal Colleges developed the Medical Leadership Competency Framework (MLCF). This framework encompasses five domains: demonstrating personal qualities, setting direction, working with others, improving services, and managing services. Webb et al concluded that the MLCF is the “most comprehensive and detailed model for leadership education in medicine” they could find.9 They used this framework in their systematic review to evaluate studies that described curricular interventions related to leadership training. They then categorized the interventions and assessed their effectiveness with Kirkpatrick’s four-level training evaluation model and a Best Evidence Medical Education guide. Nevertheless, the study concluded that most of the 24 curricula (spread across the United States, United Kingdom, Canada, Switzerland, and Israel) did not contribute to behavioral change. According to Hackman, effective clinical leadership is defined as the ability to optimize individuals’ strengths and skills in a team by setting a clear direction and working together to achieve the desired patient outcomes.10 Inspired by this definition and the MLCF definition, this study adopts key components of the MLCF framework to provide an operational definition of medical leadership: showing personal qualities, laying out a direction, collaborating with others, enhancing services, and managing them.
The American Association of Medical Colleges states that medical graduates are expected to “provide leadership skills that enhance team functioning, the learning environment, and/or the healthcare delivery system”, yet there is still a dearth of formal training methods to teach students medical leadership during undergraduate medical education (UME), an ideal time to build the foundation of leadership competencies.1 In their scoping review of leadership curriculum and competency frameworks in US undergraduate medical education, Matsas et al concluded that a small portion of leadership development curricula was consistent with MLCF. The review also ascertained the ongoing debate on the conceptual nature of leadership in medicine and varying approaches to teaching it.11
However, advancements are being made as evidenced by schools implementing or integrating leadership themes into their curricula. For instance, students at the University of Massachusetts medical school designed and implemented a course to develop first-year medical students’ leadership skills.12
Therefore, given the importance of leadership skills and the vast amount of information on the frameworks and training methods to teach such skills, medical schools need to re-envision their curricula and consider integrating optimal training methods and certain, if not all aspects, of leadership curricula. A cross sectional study conducted in 2016 assessed UK medical students’ views toward medical leadership and showed that 63% (n = 114) would have liked more leadership training during medical school. More striking is the result that a little over half (54.5%) the students rated their leadership training as “very poor” or “poor”.5
This study’s goal is similar to that of Webb et al’s, which is to “understand how best to incorporate leadership training into an already-crowded UME curriculum”.9 We believe that a starting point would be to explore the perceptions of medical students and faculty in order to determine how to best optimize a leadership training curriculum by building on previous studies’ methodologies.6,13 Specifically, this study sought to find out to what extent leadership training is incorporated into the curriculum of a medical program at an American college located in Qatar and to investigate students’ and faculty perceptions of this training.
Study Context
Weill Cornell Medicine-Qatar (WCM-Q) was established in 2001 as a branch campus of Cornell University located in New York, bringing its partnership with Qatar Foundation to fruition. WCM-Q enrolled its first batch of medical students in 2002 and graduated the first cohort in 2008. The college offers an integrated six-year program starting with a two-year premedical curriculum followed by a four-year medical curriculum. The college also offers a one-year foundation program. In the 2021–2022 academic year, WCM-Q enrolled 323 students, including Qatari citizens, long term residents of Qatar, and international students from other parts of the world. Faculty are also as diverse as the students. WCM-Q has 82 faculty from various nationalities and cultural backgrounds. (WCM-Q Fact Sheet 2021–2022) Patient care, interpersonal and communication skills, professionalism, and healthcare systems, among other topics, are listed as the program’s core competencies and learning objectives of the medical curriculum. Leadership is explicitly mentioned only under “Interpersonal and communication skills”: “communicate, consult, collaborate, and work effectively as a member or leader of healthcare teams”.
Materials and Methods
This qualitative study employed a case study methodology using a mixed-methods approach that began with a student survey, followed by faculty leaders’ interviews, and a student focus group. The quantitative data derived from the survey were used to formulate questions which were asked in the interviews and focus group.
This sequential explanatory design consists of two distinct phases: a quantitative phase followed by a qualitative phase. The quantitative data (survey) were collected and analyzed using NVivo. The qualitative data (interviews and focus group) were then collected to help explain and elaborate on the quantitative results. This specific sequential explanatory design is consistent with the follow-up explanations model.14 The rationale for this model is based on using the results of the survey to build upon the questions to ask during the qualitative phase and connect the two phases to build a refined and in-depth understanding.
IRB approval [IRB 21–00012] from WCM-Q was obtained for this study, classified as human subjects research with minimal risk. An informed consent form was shared with participants through email describing the aim of this research and requesting their consent to participate in the study.
Student Survey
A 16-question survey (see Appendix A) was built with Qualtrics XM software and sent out by email to medical students in their third and fourth years of medical school at Weill Cornell Medicine - Qatar. Medical students in the first two years of the four-year medical curriculum were excluded from the study since they were still early on in their medical school journey and had minimal exposure to the clinical setting. The questions were constructed based on a review of previous literature on gauging medical students’ perceptions of leadership and leadership training in their curriculum.6 Additionally, the medical school’s core competencies and learning objectives list, curriculum structure, and its components were used to tailor questions specific to the school’s curriculum and its students.
Participants were asked to select their responses on a Likert scale and had the opportunity to elaborate on their responses with the option of free-text responses.
The survey was piloted to four students to identify and correct any mistakes and enhance the clarity and ease of reading. The responses gathered from this survey were then used to formulate interview and focus group questions that would explain the results and provide an in-depth understanding of faculty and students’ perceptions.
Faculty Interviews and Student Focus Group
An invitation for an interview was sent by email to two medical faculty leaders. Then
each interview was conducted via Zoom. A sample of four students was randomly selected from the pool of survey respondents to participate in a focus group session conducted via Zoom. The two interviews and the focus group session were both recorded for transcription and analysis.
In order to ensure consistency across the interviews and focus group session, the same set of questions was asked:
- Is leadership a core competency? Should it be explicitly stated in the “WCM-Q Program Core Competencies and Constituent Learning Objectives” list?
- Where does leadership training take place?
- How are leadership qualities being assessed?
- Is the amount of leadership training adequate?
- Is leadership training seen as a priority by students? What about faculty?
Qualitative Data Analysis
Interviews were recorded, transcribed, and exported to Nvivo 12 (QSR International). Three stages of analysis were performed as outlined by a previous mixed-methods study analyzing interviews.13
Familiarization and Coding
The transcripts were read and keywords, phrases, and/or paragraphs were highlighted to a certain code. A distinction was made between students’ responses and faculty responses. After coding, the texts pertaining to their respective codes were reread, and the codes were proofread and revised accordingly for improved clarity and reduced redundancy.
Categorizing and Grouping
The coding framework was organized around the trigger questions. The questions guided the grouping of certain codes to succinctly summarize the responses. A mixture of two approaches was used to analyze the data at this stage. The first approach is described as ‘systematic coding via data analysis10 in which, the units of analysis, ie, students and faculty, were identified, and the researchers took note of whether every participant mentions a code, therefore placing higher emphasis on the idea derived from the code. The second approach, described as the “ethnographic analysis”,15 involves purely qualitative elements focused on producing a detailed and interpretative account of the focus group and interviews. The challenge of accurately presenting such material was addressed by framing data around the trigger questions, which provided the context and the meaning it carries to this inherently qualitative data.
Interpretation and Depiction of Themes
In order to deepen the analysis and interpretation, tools such as mind maps, concept maps, and hierarchy charts were employed to not only identify but also illustrate important overarching themes. This stage of analysis also focused on comparing and contrasting the categories of students’ and faculty responses.
Results
Student Perceptions (Survey)
The survey, sent out to the third and fourth-year medical students, resulted in a total of 34 responses, divided between 14 males (41%) and 20 females (59%). The age distribution consists of 29 respondents who were between 18–24 (85%) and five respondents whose ages were between 25–34 (15%). Finally, 17 students (50%) were in their third medical year while the fourth medical year was represented by 17 (50%) as well.
The survey results pertaining to leadership skills, leadership training, and the barriers of its implementation can be summarized as follows:
- 49% of the respondents agree that leadership skills could be better assessed in students.
- Clerkships are somewhat effective but need to be improved for better implementation of leadership training through improving recognition of leadership, assigning more responsibility, and prioritizing the learning of leadership skills (based on students’ additional comments).
- 82% of the respondents believe that possessing more leadership skills would improve their skills as physicians.
- 61% of respondents do not agree that leadership training is unified across the medical curriculum.
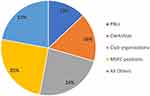
Figures 1-4 provide a visual summary of student participants’ answers. The figures depict select responses from the survey that are further consolidated by assigning them under two broad questions:
- To what extent is leadership training incorporated into WCM-Q’s medical curriculum? Figure 1 shows participants’ responses to this question while Figure 2 shows that students encounter leadership training (in descending order) when participating in MSEC (Medical Student Executive Council) positions, club organizations, and clerkships.
- How do medical students perceive their leadership training in the WCM-Q medical curriculum? Figure 3 demonstrates students’ attitudes about the need for leadership training, which ultimately has an impact on their perception of the leadership training provided to them at their institution. As illustrated in Figure 4, the majority of students perceive lack of importance and a packed medical curriculum as obstacles to implementing leadership training at their institution.
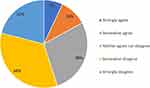 |
Figure 1 Breakdown bar of responses to whether leadership skills are adequately taught. |
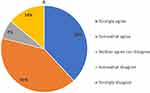 |
Figure 3 Breakdown bar of responses to whether leadership is a core competence. |
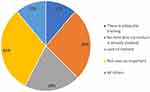 |
Figure 4 Participants’ responses about obstacles to implementing leadership training (All others: inadequate budget, other (unspecified)). |
 |
Figure 5 Concept map of leadership training in light of students’ and faculty’s perceptions. |
Faculty Interviews and Student Focus Group
Interviews and focus group results were analyzed in Nvivo. Table 1 below provides a summary of the codes extracted from the qualitative data followed by an analysis of each trigger question.
 |
Table 1 Codes Extracted from Qualitative Data |
Is Leadership a Core Competency and Should It Be Explicitly Stated as Such?
The value of leadership as a core competency was widely agreed upon. Physicians need to “assume that leadership role” in which they are responsible for a patient’s well-being and need to effectively “facilitate and coordinate that care for the patient”. Additionally, being a physician is essentially a “managerial position” which requires one to know “how to manage [one’s] team”. Consequently, leadership should be explicitly stated in the core competencies list and should be integrated into the curriculum.
“It’s important that some people who don’t have this intrinsic skill get explicit training to develop that skill”.
One faculty interviewee states leadership is key “only because [physicians] are often working as part of the health care team” and “there will be instances where both the physicians and the medical students have to take on the positions or a situation where there are leaders”.
This skill is alluded to in terms like interpersonal communication, cultural competency, professionalism, etc. Since the concept of leadership is alluded to, there is no necessity to explicitly state it.
Where Does Leadership Training Take Place?
Students mentioned that during their Anesthesia and Critical Care clerkship, they participated in a simulation exercise that assigned roles such as leader and helper to students, and they stated that this experience was one of the ways leadership training takes place. They also referred to the level of responsibility assigned during clerkships and in clinical electives and sub-internships but noted
That decisions are almost never made by us. We simply suggest a decision and it’s taken by somebody else. And I think there is a critical difference between that and making a decision under oversight.
Another student suggested that leadership roles in extracurricular activities are an extracurricular and optional source of honing one’s leadership skills.
The clinical sciences faculty also mentioned the simulation exercise that took place in the clerkship, and that in the Transition to Residency (TTR) module, students get an “appetizer about how to be a team leader”. The TTR module is a brief set of didactic lectures and workshops given to fourth year medical students towards the end of the year. It encompasses interactive sessions about activities that medical residents are required to perform, such as consulting subspecialties, breaking bad news, understanding team dynamics, and optimizing workflow.
Stressing that it is implicit training, one faculty cited that leadership training occurs through exposure to the leadership of an attending physician or the dean and their practices.
How are Students’ Leadership Qualities Assessed?
Students had the initial impression that leadership qualities are not assessed. They are definitely not explicitly assessed, but leadership qualities are alluded to. One specific instance where they are alluded to is in the clinical evaluation forms for clerkships, specifically, about patient ownership.
“There are aspects in the clinical evaluation that incorporate leadership and ownership of patients”.
PBLs, or problem-based learning sessions, were also mentioned. Some of the roles that students take during these sessions “clearly involved more of a leadership position”.
PBL is a place where people who are leaders are going to act like leaders, and people who don’t necessarily have a good baseline level of leadership ability don’t get to develop it because they’re never formally made into a discussion facilitator.
Faculty stated that the priority is not on leadership skills. The evaluations do not emphasize leadership skills but do allude to certain elements, such as professionalism, communication, teamwork.
Is the Amount of Leadership Training Adequate?
Students clearly expressed that leadership training is inadequate. One student cited his experience during an elective that involved a leadership position, stating that they felt underprepared.
It’s just the case that when you have full responsibility for your patients, and there are so many different factors to juggle, that confidence is not something that’s going to be there for you, even if you are generally a very confident person and generally you try to assume leadership positions.
One faculty called for more research to be done on leadership and students’ perceptions, as well as curriculum mapping to answer this question.
The key thing is you need the knowledge and the skills to get your degree and to start practicing…Get a residency. Get that underway. Then leadership comes further down the line.
Is Leadership Training Seen as a Priority by Students? Faculty?
All participants agreed that leadership training is not seen as a priority by either students or faculty. However, there were different explanations for this. Students reported that while leadership is seen as important by some, it is not recognized as important by all, and the fact that leadership training is not implemented as a core curriculum component is suggestive of either a failure to recognize the importance of leadership or an inability to implement effective training. One student’s assumption of the leadership’s efforts is that “what [they’re] doing already is enough in terms of teaching leadership or helping develop leaders”.
Faculty believe that while leadership as a skill is beneficial, the priority for students is to excel on their exams and acquire the knowledge that they need. Leadership training is not seen as a priority by faculty due to the obstacles encountered: packed curriculum, lack of interest and recognition from students, and need for research on ways to optimally implement training methods. Figure 5 provides a summary of students and faculty perceptions of the obstacles to leadership training in the medical curriculum.
Discussion
Students agree that leadership should be a core competency since being a physician comes with the responsibility of patient care and ownership. Faculty on the other hand do not necessarily believe that leadership needs to be separately stated as a core competency since the curriculum already provides implicit training. Also, leadership should be a later priority since the main objective is to provide students with the requisite clinical skills and knowledge to qualify them for residency. Both students and faculty identified the rigorous and dense curriculum as an obstacle to implementing leadership training. Students also mentioned the feasibility of leadership training, especially in clinical settings, as a barrier. But by and large, the most influential obstacle appears to be the lack of recognition. Figure 3 illustrates students’ and faculty perceptions of leadership training at their institution. It is a representation of the relevant codes derived from the focus group and interviews.
We found that the students’ impressions and opinions are largely consistent with previous literature. Most notably, Quince et al conducted focus groups involving 28 participants between 2009 and 2012 in one medical school in the UK to explore students’ attitudes towards leadership education. The authors concluded that students are “more open and accepting of the role of leadership and management education in medical education than thought hitherto”.16 Our students’ thoughts are similar to those reported by the study in terms of the desire to integrate leadership education into a crowded curriculum. Their study also recognized that perceptions that contribute to a lack of recognition, especially “some attitudes held by medical professionals and students and by society as a whole” are barriers to leadership education. Rouhani et al’s study, published more recently in 2018, identified that Quince et al’s study was in parallel with their findings, stating that 63% of the students surveyed would have liked more leadership training in their medical school and that over half of those students rated their training as poor.5 Similar sentiments were also reported in a 2011 systematic review that explored the attitudes of medical students to medical leadership and management. It emphasized students’ agreement with a need for leadership training in an undergraduate medical curriculum while identifying that lack of time as well as disinterest (by both students and faculty) as possible barriers to implementation.17
Qualities such as emotional intelligence, confidence, and humility have been identified as key qualities of leaders and such qualities, in addition to teamwork, communication, management, and other competencies can be taught during medical school.6 As a result of students’ and faculty perceptions, Mayo medical school introduced an explicit core curriculum on leadership with plans to integrate it across the four years of medical school.6 University of Michigan Medical School, for example, integrated leadership training in the form of evaluations, opportunities for personal leadership development reflections with faculty, as well as interactive sessions to improve leadership skills.18 Duke University school of medicine also implemented a Leadership Education and Development (LEAD) curriculum that spans all four years of medical school.19 The curriculum is centered around the competencies that comprise the Duke healthcare leadership model with the aim to not only teach these competencies through certain LEAD activities (such as team based learning sessions) but also intentionally explore and foster leadership skills in the context of experiential learning ie the clinical/hospital setting.
Intention and integration seem to be the consistent themes behind the implementation of an explicit curriculum and framework at the medical schools mentioned above. Specifically, an intention to actively incorporate and look for leadership skills and competencies that can be observed and taught in a natural way that is integrated into the curriculum. Implementing training with such principles in mind would be far better against the obstacles of teaching in a packed curriculum and increasing recognition, or at the very least, curbing disinterest in leadership training.
Making changes based on a curricular framework such as MLCF would fare quite well since it was described as one of the most comprehensive models for leadership education. But as faculty interviewees stated, leadership training is implicit and the requisite skills (interpersonal communication, patient care, professionalism) that fall under leadership are indeed assessed and developed in students. Given the perceptions of the students, however, perhaps it would be prudent to incorporate leadership as a core objective, construct or adapt a conceptual framework, and make additions to the four-year medical curriculum in a similar fashion to the examples mentioned above. As stated in previous literature and by the student participants, incorporation of such training would be most effective if done through experiential learning, although additional small group sessions and interactive classroom seminars can be employed as well. The students in our focus group alluded to the level of responsibility assigned to them during clerkships as a starting point to build upon leadership skills. To that effect, Uniformed Services University employed a reflective essay assignment at the end of its internal medical clerkship rotation to assess for reflection of leadership as a theme.20 Based on the aspects of leadership that the students implicitly or explicitly reflected on in their essays, the study concluded that such an assignment can be conducive to personal leadership development since they were given the opportunity to reflect on others and themselves while building upon the leadership model that they were taught in pre-clerkship years. Their leadership curriculum in the pre-clerkship years is based on their leadership conceptual framework and includes plenary sessions, flipped classrooms, and applied clinical and field settings.20 Additionally, the authors argue that such essays can be used to guide further curriculum development.
Lastly, methods used in residency training to foster leadership development can be carried down to medical school. Hadley et al’s study demonstrated that junior doctors who received formative feedback on their leadership skills felt that their skills improved as a result of said feedback.21 Rouhani et al, as result, cited this study and suggested that this practice be transferable to medical schools. Ultimately, training must be integrated and in line with the education rather than separated and isolated from clinical instruction. Abbas et al’s systematic review therefore calls for curriculum planners to be flexible and “win the hearts and minds of clinicians” who come in contact with students and have them act as role models that can emphasize the importance of such a skill.17
Strengths and Limitations
This study expands on prior literature in terms of recency, a different location with a US-based curriculum, essentially offering perspectives from a unique setting. It contributes to the literature with a small-scale study of US medical students’ and builds upon several past studies that employed either mixed method studies, interviews, or focus groups.6,13,16
This study does have some limitations, however. The participants in this study are a select small group, and the focus was on the medical school that they are enrolled in. The qualitative data analysis and the approach to analysis are also subject to researcher bias. We understand that the sample size and study are small, which may have impacted the strength of our findings. To put it in perspective, however, the fourth-year medical students are a cohort of 45 students and the third-year medical students are also around the same. This was deemed to be the most realistic and attainable number given the student population and timeline.
Conclusion
Given the well-known need for leadership training and the students’ consistent views with prior literature elicited from this small-scale study that took place in a setting with unique a curricular context, institutions should focus on fostering interest in leadership at the faculty level and demonstrate flexibility in their approach to integrating and improving their training after first employing or adapting a suitable framework. While there have been studies13 that have highlighted the importance of leadership skills and leadership curricula from the perspective of faculty and physicians, continuing to elicit students’ perspectives is essential to inform effective curriculum development since it can highlight the obstacles as well as areas that are beneficial in one’s curriculum. This study hopes to advance mixed methods methodology to elicit a comprehensive and deep understanding of students’ perspectives as well as discuss literature about the barriers to implementing leadership training and ways to address them.
Exploring the perceptions of medical alumni could strengthen the claims made in this paper as well as enhance the information at our disposal to best implement a leadership curriculum. This study could also serve as a foundation for improved quantitative and qualitative phases for evaluation of leadership curriculum in medical education after implementation.
Acknowledgments
This study is the result of a report that emerged from the Area of Concentration (AOC) program for medical students at Weill Cornell Medicine-Qatar. The authors would like to thank the Medical Education Division for funding this study. The authors are also grateful to the AOC faculty and staff; Reya Saliba, Education and Research Librarian; Dr. Ziyad Mahfoud, Professor of Statistics; medical students and faculty; and the IRB team for their valuable support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chen T. Medical leadership: an important and required competency for medical students. Tzu-Chi Med J. 2018;30(2):66. doi:10.4103/tcmj.tcmj_26_18
2. Sarto F, Veronesi G. Clinical leadership and hospital performance: assessing the evidence base. BMC Health Serv Res. 2016;16(2):85–97. doi:10.1186/s12913-016-1395-5
3. Sonsale A, Bharamgoudar R. Equipping future doctors: incorporating management and leadership into medical curriculums in the United Kingdom. Perspect Med Educ. 2017;6(2):71–75. doi:10.1007/s40037-017-0327-3
4. Cabell GH, Anjorin A, Price M, Biswas S, Doty JP. How the COVID-19 Pandemic Has Demonstrated a Need for Increased Leadership Education in Medicine. J Healthcare Leadership. 2021;13:137. doi:10.2147/JHL.S317847
5. Rouhani MJ, Burleigh EJ, Hobbis C, et al. UK medical students’ perceptions, attitudes, and interest toward medical leadership and clinician managers. Adv Med Educ Pract. 2018;9:119–124. doi:10.2147/AMEP.S151436
6. Varkey P, Peloquin J, Reed D, Lindor K, Harris I. Leadership curriculum in undergraduate medical education: a study of student and faculty perspectives. Med Teach. 2009;31(3):244–250. doi:10.1080/01421590802144278
7. Lyons O, Sua B, Locke M, Hill A. A systematic review of leadership training for medical students. N Zealand Med J. 2018;131(1468):75–84.
8. Neeley SM, Clyne B, Resnick-Ault D. The state of leadership education in US medical schools: results of a national survey. Med Educ Online. 2017;22(1):1301697. doi:10.1080/10872981.2017.1301697
9. Webb AM, Tsipis NE, McClellan TR, et al. A first step toward understanding best practices in leadership training in undergraduate medical education: a systematic review. Acad Med. 2014;89(11):
10. Hackman JR. Leading Teams: Setting the Stage for Great Performances. Boston, Mass: Harvard Business Press; 2002.
11. Matsas B, Goralnick E, Bass M, Barnett E, Nagle B, Sullivan EE. Leadership Development in U.S. Undergraduate Medical Education: a Scoping Review of Curricular Content and Competency Frameworks. Acad Med. 2022;97(6):899–908. doi:10.1097/ACM.0000000000004632
12. Richard K, Noujaim M, Thorndyke LE, Fischer MA. Preparing medical students to be physician leaders: a leadership training program for students designed and led by students. MedEdPORTAL. 2019;15:10863. doi:10.15766/mep_2374-8265.10863
13. Omar A, Shrestha A, Fernandes R, Shah A. Perceived barriers to medical leadership training and methods to mitigate them in the undergraduate medical curriculum: a mixed-methods study of final-year medical students at two medical schools. Future Healthcare J. 2020;7(3):e11. doi:10.7861/fhj.2019-0075
14. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Sage publications; 2017.
15. Wilkinson S. Focus group methodology: a review. Int J Soc Res Methodol. 1998;1(3):181–203. doi:10.1080/13645579.1998.10846874
16. Quince T, Abbas M, Murugesu S, et al. Leadership and management in the undergraduate medical curriculum: a qualitative study of students’ attitudes and opinions at one UK medical school. BMJ Open. 2014;4(6):e005353. doi:10.1136/bmjopen-2014-005353
17. Abbas MR, Quince TA, Wood DF, Benson JA. Attitudes of medical students to medical leadership and management: a systematic review to inform curriculum development. BMC Med Educ. 2011;11:93. doi:10.1186/1472-6920-11-93
18. Leadership Program [homepage on the Internet]. University of Michigan Medical School; 2022. Available from: https://medicine.umich.edu/medschool/education/md-program/curriculum/impact-curriculum/leadership-program.
19. Leadership Education and Development (LEAD) Curriculum [homepage on the Internet]. Duke University School of Medicine; 2022. Available from: https://medschool.duke.edu/education/health-professions-education/doctor-medicine-md-program/curriculum/longitudinal-0.
20. Barry ES, Grunberg NE, Kleber HG, McManigle JE, Schoomaker EB. A four-year medical school leader and leadership education and development program. Int J Med Educ. 2018;16(9):99–100. doi:10.5116/ijme.5abe.12d2
21. Hadley L, Black D, Welch J, Reynolds P, Penlington C. Encouraging formative assessments of leadership for foundation doctors. Clin Teach. 2015;12(4):231–235. doi:10.1111/tct.12289
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.