Back to Journals » Clinical Ophthalmology » Volume 14
Lateral Rectus Muscle Tendon Elongation by an Auto Graft from the Resected Medial Rectus Muscle as a Monocular Surgery for Large-Angle Sensory Exotropia
Authors Shafik HM , Eldesouky MA , Tadros D
Received 20 March 2020
Accepted for publication 26 June 2020
Published 24 July 2020 Volume 2020:14 Pages 2135—2142
DOI https://doi.org/10.2147/OPTH.S253628
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Heba M Shafik, Mohamed Ashraf Eldesouky, Dina Tadros
Department of Ophthalmology, Faculty of Medicine, Tanta University, Tanta, Egypt
Correspondence: Heba M Shafik
Tanta University Hospital, El-Geish Street, Tanta, Egypt
Tel +00201227440829
Fax +0020403274005
Email [email protected]
Purpose: To evaluate using the resected medial rectus muscle for elongation of the lateral rectus tendon in monocular surgery for large-angle sensory exotropia.
Patients and Methods: A prospective case series was carried out in Tanta University hospital from January 2017 to June 2018 including 16 patients with large-angle sensory exotropia ≥ 50PD. The near and distance angles of exotropia were measured; any restrictions in adduction or abduction were recorded and scaled from − 4 to 0. Resection of the medial rectus muscle was done first; the resected segment was attached to the lateral rectus muscle after dissection by mattress sutures, and the muscle was recessed after elongation according to the preoperative distance angles. Successful motor alignment was considered if the angle measurement was within 10 PD of orthotropia at distance after 6 months. The stability of the alignment, any motility restrictions, and patient satisfaction were recorded at each follow-up visit until the 6th month.
Results: The mean age of the study patients was 30.68± 13.30 years. The best-corrected visual acuity of the exotropic eyes by logMAR was 1.2± 0.3; the mean of the preoperative distance angle of deviation was − 72.19 ± 14.26 PD. The mean preoperative adduction and abduction restrictions were − 1.19 ± 1.52 and − 1.13 ± 1.09, respectively. There was significant improvement in the distance angle of deviation at the last follow-up after 6 months (p=0.001*). Also, there was improvement in both adduction and abduction restriction from the first to last follow-up. Thirteen patients (81.2%) were satisfied at the 6-month follow-up.
Conclusion: Elongation of the lateral rectus muscle by an autograft from the resected medial rectus muscle is an easy, effective procedure for large-angle sensory exotropia. Patients achieve good postoperative alignment with minimal restriction of ocular motility.
Keywords: sensory exotropia, autograft, lateral rectus elongation
Introduction
Sensory exotropia is exodeviation of one eye with longstanding poor vision. The angle is characteristically large, ranging from 30 to 100 prism diopters (PD), and it may gradually increase as the cause of visual deficit remains active.1 Combined recession-resection is the preferred procedure on the eye with poorer visual acuity and a large angle. Some surgeons prefer to do an additional one- or two-muscle surgery in the better seeing eye if the angle of deviation is ≥50PD. Others prefer to do extra surgery on the visually poorer eye alone without interfering with the other eye and they leave it intact for a second intervention in the case of recurrence.2–4 Although the stability of alignment is a significant benefit of supermaximum recession-resection surgery, the possibility of disfigurement caused by limited abduction, excessive adduction, narrowing of the palpebral fissure, and enophthalmos has to be considered.5,6
As an alternate for supermaximal recession resection surgery, elongation of the muscle using bovine pericardium7 or artificial materials such as Gore-Tex® have been used,8,9 where the possibility of extrusion, infection, and globe erosion cannot be excluded.10–12 However, using the resected part of the muscle as an alternate to allograft has proven to show fewer complications and better results regarding biocompatibility, availability, safety, and cost.13–15
In the current study, we evaluated the outcomes when using the resected part of the medial rectus (MR) muscle to elongate the lateral rectus (LR) in patients with large-angle exotropia, in which a recession was necessary beyond the possibilities of a conventional recession, and we evaluated the results after 6 months of follow-up in terms of stability of the graft, eye alignment, and motility.
Patients and Methods
This is an institutional, prospective case series that was carried out in Tanta University hospital, Tanta, Egypt between January 2017 and June 2018. The research was approved by the Medical Ethics Review Committee at Tanta University. All procedures were carried out under the tenets of the Helsinki Declaration. Written consent was provided by all participants after discussing the procedure, alternative treatment plans, follow-up schedules, and possible benefits and risks.
Patients with monocular low vision or loss of vision due to a congenital or acquired cause withexodeviation of the poorly seeing eye ≥50PD were included in the study. Patients with exotropia other than sensory type (alternating exotropia, intermittent exotropia), an angle of deviation less than 50 PD, visual acuity better than 0.6 by logMar in the affected eye, and an A or V pattern ornystagmus were excluded. Also, the adult patients or caregivers of children who refused surgery or did not complete follow-up, were excluded.
The full history examination included previous surgeries, if any, and their timing, and the etiology of visual affection. Visual acuity in decimals were converted to logMar for statistical analysis. A cycloplegic refraction and fundus examination of both eyes was performed prior to surgery. Strabismus angles were measured at near and distance with an alternate prism cover test when possible and Krimsky’s test with a prism put in front of the better seeing eye was performed with poorer visual acuities. The manifest exotropia angle at 6m was the angle used for dosage of surgery.
Any restrictions of adduction or abduction were scaled from −4 to 0; with-4 implying no adduction beyond midline, −3 implying a 75% deficit,-2 indicating a 50% deficit,-1 indicating a 25% deficit, and 0 for full ductions. Successful motor alignment was considered within 10 PD of orthotropia at a 6 m distance with spectacle correction worn at 6 months.
Surgical Procedure
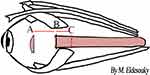
All surgeries were performed under general anesthesia by the first author. The MR muscle was dissected through a limbal incision. Two single armed 6–0 Vicryl sutures (Ethicon Inc., Somerville, NJ, USA) were placed anteriorly at the insertion and another pair was placed posteriorly at the desired distance from the insertion as the routine resection of rectus muscles. The muscle was then incised in front of the preplaced anterior and posterior sutures. The previously placed posterior sutures were passed through the original insertion. The resected segment with a pair of vicryl sutures tied to its anterior borders was put in saline. Two single armed vicryl 6–0 sutures were placed at the LR muscle insertion after isolation through a limbal incision. Next, the anterior border of the resected segment was sutured to the sclera at the desired position measured by the strabismus caliber according to the surgical dosage sufficient to correct the premeasured distance angle and the posterior border was sutured with the LR muscle with the 6–0 Vicryl already placed on the LR muscle by mattress sutures. Now the elongated muscle was sutured at the desired distance from the insertion. The conjunctiva was sutured with 7/0 Vicryl (Ethicon Inc.) Figure 1 shows diagrammatic representation of the recession of the LR muscle after elongation by autograft of the resected MR muscle.
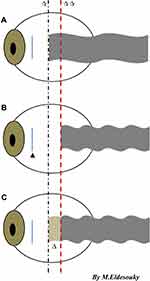
The amount of resection of the MR muscle was 6 mm for angles from50–65 PD, 7 mm for angles from 70–85PD, and 8 mm for angles > 85PD. There was shrinkage from 1–2 mm in the transplantation segment after cutting from the MR. The amount of recession of the LR muscle after elongation was set according to the preoperative distance angle (5.7±1.9; based on surgeon experience and previous recommendations) and did not exceed 7 mm resection and 8 mm recession to avoid limitations of movement as recommended by previous studies.16,18 Each 1mm elongation of the LR by the transplanted segment causes weakening and is considered to be 1.5 mm added to the amount of recession of the LR muscle without the need for further recession behind the equator. (See Figure 2, which shows diagrammatic representation for the difference between maximum recession, supermaximum recession, and muscle elongation.). This dosage scheme was developed by trial in the first few cases and it was maintained in subsequent patients.
The patients were followed at 1 day, 1 month, 3months, and 6months postoperatively.
At each visit, the distance angle of deviation was measured with a prism cover test whenever possible and with Krimsky’s test when not possible, any limitation of adduction and abduction was scaled, and all results were recorded and tabulated.
Subjective assessment of postoperative satisfaction was judged by a satisfaction score. The patients were asked to complete a satisfaction assessment questionnaire at the 6-month follow-up, which comprised three questions based on satisfaction with degree of alignment, aesthetic appearance, and limitation of adduction and abduction. The patients were asked to classify their postoperative level of satisfaction as 0: I am not satisfied, 1: I am moderately satisfied, 2: I am satisfied, 3: I am very satisfied, and I would recommend it to another. Figure 3 shows the questionnaire presented to the patients at 6 months after surgery.
 |
Figure 3 The patient satisfaction questionnaire at the 6th month. |
Three distinctive groups were created based on the score of the questionnaire (0–3 unsatisfied, 4–6 moderately satisfied, 7–9 very satisfied). The supplementary material file shows the pre- and post- operative photos of a sample of the cases with successfully maintained alignment postoperatively and improved adduction and abduction.
Statistical Analysis
A paired t-test was used to compare continuous variables for the mean angle of deviation before and after surgical correction. Data are summarized as mean and standard deviation. A P value of ≤0.05 was considered significant.
Results
The present study was carried out on 16 patients with large-angle sensory exotropia, including nine males (56.3%) and seven females (43.8%). The mean age of the patients in years was 30.68±13.30 (range: 12–56), the best-corrected visual acuity of the exotropic eyes by logMar was 1.2±0.3 (range: 1.0–1.5), and the mean of the preoperative distance angle of deviation by PD was −72.19±14.26 (range: −100 Δ– −50 Δ). The mean of the preoperative adduction restriction was −1.19±1.52 (range: −4–0) and the mean of preoperative abduction restriction was −1.13±1.09 (range: −3–0). The amount of MR resection ranged from (6–8mm), while the amount of LR recession ranged from (4–8 mm). There was significant improvement in the distant angle of deviation at the last follow-up after 6months (p=0.001*; Table 1). There was improvement in adduction restriction, as shown in Table 2 and Figure 4. Also, there was significant improvement in abduction restriction at that last follow-up, as shown in Table 3 and Figure 5.
 |
Table 1 Preoperative Distant Angle and Postoperative Distance Angles from First Day Till Last Follow-Up Showing Significant Improvement |
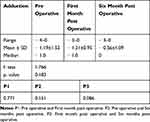 |
Table 2 Improvement of Adduction Restriction from Preoperative Till Last Follow-Up at the 6th Month |
 |
Table 3 Improvement of Abduction Restriction from Preoperative Till Last Follow-Up at the 6th Month |
 |
Figure 4 A graph showing post operative improvement of adduction restriction. |
 |
Figure 5 A graph showing post operative improvement of abduction restriction. |
Regarding patient satisfaction with the procedure, seven patients were moderately satisfied (43.8%), six were very satisfied (37.5%), and only three patients were not satisfied (18.8%).
The success rate was80% and only two cases failed. One of these patients was not satisfied and had secondary surgery for correction of the residual angle after 6 months, while the other patient was satisfied with the result.
Observations after the second surgery: In the patient who had residual exotropia of 20 PD, which increased at the last follow-up to 30PD. The patient underwent revision surgery with re-resection of MR 3 mm and re-recession of the elongated LR an additional 5 mm. This required exploration in the region of the LR muscle. During surgery, no severe adhesions were encountered. Exploration was not difficult. The transplanted segment showed excellent healing to the stump of the LR muscle as if it was a part of the LR muscle tendon. Figure 6 shows the elongated recessed LR muscle after 6 months during exploration for re-recession to correct residual exotropia.
 |
Figure 6 Intra operative photo showing the autograft segment of resected medial rectus to the recessed lateral rectus muscle showing no adhesions or reactions after six months from the first surgery. |
Discussion
Some patients with large-angle sensory exotropia refuse or may not meet the criteria for binocular surgical correction.16 With such large angles, extra-large recessions are required.17 Furthermore, in patients with thin scleras, such as in glaucoma or high myopia, or patients with a history of previous surgery on the same eye, an extra-large recession or resection may be difficult. Therefore, monocular surgery is required to weaken the extraocular muscle and improve motility of the globe at the same time.8,9
An excessive amount of recession or resection may cause severe disfigurements. When large MR resection is performed, significant resistance to abduction, narrowing of the palpebral fissure, and enophthalmos can occur.2 Rayner and Jampolsky4 advocated the use of large MR resection and maximum LR recession on the amblyopic eye with large-angle exotropia. In this study, 22 patients were included, six patients underwent MR resections of more than 9 mm, while the amount of LR recession was 7 mm to 8 mm. They asserted that the disadvantage of deficient abduction is considered an advantage for the prevention of exotropia recurrence. In addition, other studies reported that LR recession exceeding the equator may also reduce abduction significantly and it causes lateral incomitancy and late overcorrection.9,18 In our study, patients were able to achieve good postoperative alignment with minimal limitation of ocular motility after 6 months postoperatively. In 2011, Chang19 published a case report of four patients with sensory exotropia who had a mean deviation of 82.3 PD and had a MR muscle resection with a mean of 10.3 mm and a LR muscle recession with a mean of 12.8 mm. The mean postoperative angle of exodeviation was 2.0 PD. He stated that limitation of abduction and noncomitancy were present but were not disfiguring. In our study, noncomitancy and disfigurement, such as narrowing of the palpebral fissure or enophthalmos, were present.
The other option is using marginal myotomies, such as botox injection, to augment recession with unpredictable results or hang-back sutures. However, the efficacy of large hang-back recessions beyond the equator has not yet been proven.20–22 Moreover, in cases of VI nerve palsy, Focosi et al,23 and Boschi et al,24 reported the results of elongation of the tendon of the MR muscle by fascia lata. However, the success rate of this technique was diminished because the material shrank by about one third of its length. Also, muscle elongation with allograft material, such as a silicone band or non-absorbable sutures, has been reported.9,25 It has been used successfully in Brown’s syndrome for muscle elongation as well as chicken sutures,26,27 but it is still a challenging procedure with a long learning curve and with the possibility of postoperative inflammatory reactions, adhesions, and extrusion.28 Artificial materials such as Gore-Tex® have been used recently in restrictive strabismus cases with fibrosis or repeated operations to improve duction movement, residual deviation, and diplopia. The results were promising for restriction improvement and the authors stated that the material is enclosed by a layer of connective tissue, undistinguishable from normal tendon, and that the extraocular muscle would grow into the structure of the polytetrafluoroethylene patch. The studies, however, were conducted on a small number of patients with restrictive strabismus only.8,9
Moreover, using xenograft material in the form of bovine pericardium has been reported in a retrospective study conducted by van Rijn and colleagues.12 The study included 38patients with recurrent strabismus and it was reported that most of the study patients had some duction limitation in the direction of the elongated muscle and that there was a small but nonsignificant regression of the exodeviation. Another study was conducted on thyroid orbitopathy patients with esotropia that used the bovine pericardium for MR elongation. It was concluded that the limitation that was present preoperatively improved but was still present postoperatively and most of the patients needed a second surgery with a variable dose effect.26 Although success was reported with the use of these materials, the availability, cost, and the fear of inflammatory reactions and extrusion could not be excluded.29
Muscle transplantation effectively provides an opportunity to correct very large angle cases and preserve comitancy with a single eye surgery.13–15,29
The transplantation of a portion of extraocular muscle was first attempted in an experimental trial on rabbits by transplanting a portion of the inferior rectus muscle to the superior rectus muscle. Cyanoacrylate adhesive was used instead of suturing. The procedure was then abandoned for two reasons: first, the fragility of the tendon of muscle and its small size interfered with handling and, second, the presence of an excessive amount of reaction around the adhesive and recipient muscle tended to fragment as well.30
Following the experimentation with the rabbits, a standard protocol was then developed and extensive studies were done on transplantation using various muscles and their mode of healing. One of the most important of these studies was conducted by Hiatt.13 This study reported that extraocular muscle tissue was transplanted, survived, and remained viable in three patients with large-angle esotropia. He stated that it is a feasible procedure that gives good results similar to artificial implants such as silicone but with the advantage of being performed easily with no tissue reaction or extrusion.
He recommended using this procedure in paralyzed extraocular muscles, thyroid orbitopathy, and amblyopic esotropia or exotropia. However, it has also been shown that the transplanted segment does not maintain its normal muscular characteristics. The rate of healing of extraocular muscles, as shown by Ingram and others, closely parallels the rate of replacement of transplanted extraocular muscle by fibrous tissue.13,31-34
Furthermore, the general reaction of tenon’s capsule was mild with some gross and microscopic adherence to the underlying sclera, but not severe enough to produce marked restrictions.13
The true muscle transplantation was studied later for large-angle esotropia correction with transplantation of the resected LR muscle by Diamond 15 and Amitava.14 However, the number of patients was limited. In 2017, Jitendra et al,29 conducted a study on 22 patients with large-angle esotropia and extended the follow-up for 2 years to study long term results. They stated that true muscle transplantation is a safe procedure. The results were stable long-term. They asserted that it is a simple yet innovative procedure that should be considered for large-angle strabismus.29
In the present study, patients had good outcomes with respect to eye alignment and motility with a follow-up of 6 months in most of the study cases and up to 1 year in two cases. No adverse effects were observed.
Moreover, the only case with residual exotropia was operated on again 6 months later for more resection of the MR and recession of the elongated LR muscle. It was noticed that there were minimal adhesions compared to all re-operated residual misaligned cases with minimal adhesions to the underlying sclera. The transplanted segment was taken into the recipient muscle, but it had more fibrous tissue content.
The limitations of our study are the small sample size and the need to re-operate on more cases that had tendon elongation to draw solid conclusions on its viability and reaction.
Conclusion
Elongation of the LR muscle by an autograft from resected MR muscle is an easy, effective procedure, especially in amblyopic eyes with large-angle sensory exotropia, especially if extraocular muscle surgery was performed previously. It has an advantage over artificial synthetic material with the absence of extrusion and less reaction. Patients achieve good post-operative alignment with minimal limitation of ocular motility and the extraocular muscle tissue that was transplanted remains viable.
Acknowledgments
Thanks for the support of Tanta University hospitals and for allowing me to collect patients, perform surgery and follow-ups and finish this research. Also I want to thank Charlesworth Author service for helping me in the final editing of the manuscript.
Disclosure
There is no conflict of interest in this research and no source of funding.
References
1. Kraft SP. Selected exotropia entities and principles of management. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia: W. B. Saunders; 1999:193–199.
2. Santiago AP, Ing MR, Kushner BJ, et al. Intermittent exotropia. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia: W.B. Saunders; 1999:163–173.
3. Parks MM, Parker JE, editors, Atlas of Strabismus Surgery. Philadelphia: Harper & Row; 1983:6–23.
4. Rayner JW, Jampolsky A. Management of adult patients with large angle amblyopic exotropia. Ann Ophthalmol. 1983;5:95–99.
5. Raab EL. Unilateral four-muscle surgery for large-angle exotropia. Ophthalmology. 1979;86:1441–1450. doi:10.1016/S0161-6420(79)35377-5
6. Rathod D, Goyal R, Watts P. A survey of the management of globe perforation during strabismus surgery in the United Kingdom. Strabismus. 2011;1963–1966.
7. Oeverhaus M, Fischer M, Hirche H, et al. TendonElongation with bovine pericardium in patients with severe esotropia after decompression in graves’ orbitopathy-efficacy and long-term stability. Strabismus. 2018;26:62–70. doi:10.1080/09273972.2018.1450430
8. Harrer S, Stangler-Zuschrott E, Rossmann M, et al. Polytetrafluoroethylene in the surgery of cases with severe limitation of abduction; long-term results. Neuro-Ophthalmol. 1999;22:177–185. doi:10.1076/noph.22.3.177.3729
9. Langmann A, Lindner S, Wackernagel W, et al. Polytetrafluoroethylene (Goretex) for muscle elongation in the surgical treatment of strabismus with restricted motility. Acta Ophthalmol Scand. 2006;84:250–253.
10. Hedergott AM, Fricke J, Neugebauer A. Medial rectus tendon elongation with bovine pericardium for type 1 Duane’s retraction syndrome. Klin Monatsbl Augenheilkd. 2014;23:980–987.
11. TsuiI. Scleral buckle removal; indications and outcomes. Surv Ophthalmol. 2012;57:53–63.
12. van Rijn LJ, van De Ven SN, et al. Tendon elongation with bovine pericardium (Tutopatch®) when conventional strabismus surgery is not possible. Eur J Ophthalmol. 2016;26:193–202. doi:10.5301/ejo.5000689
13. Hiatt RL. Extraocular muscle transplantation. Trans Am Ophthalmol Soc. 1973;71:426–458.
14. Amitava AK, Goswami AK, Mishra A. Large-angle strabismus and primary true muscle transplantation. J Pediatr Ophthalmol Strabismus. 2005;42:211–215. doi:10.3928/01913913-20050701-02
15. Diamond GR. True transposition procedures. J Pediatr Ophthalmol Strabismus. 1990;27:153–156.
16. Millan T, De Carvalho KM, Minguini N. Results of monocularsurgeryunderperibulbaranaesthesiafor large-anglehorizontalstrabismus. Clinics. 2009;64:303–308. doi:10.1590/s1807-59322009000400006
17. Damanakis AG, Arvanitis PG, LadasI D, et al. 8-mm bimedial rectus recession in infantile esotropia of 8090 prism dioptres. Br J Ophthalmol. 1994;78:842. doi:10.1136/bjo.78.11.842
18. Prieto-Díaz J, Souza-Diaz C. Esotropias. Prieto D, Souza-Dias C, editors. Estrabismo.SãoPaulo: Livraria Santos Editora; 2002:149–199.
19. Chang JH, Kim HD, Lee JB, et al. Supermaximal recession and resection in large-angle sensory exotropia. Korean J Ophthalmol. 2011;25:139–141. doi:10.3341/kjo.2011.25.2.139
20. Repeka MX, Gyton DL. Comparison of hang-back medial rectus recession with conventional recession. Ophthalmology. 1988;95:782–787. doi:10.1016/S0161-6420(88)33107-6
21. Heede S, Salchow D. Comparison of hang-back medial rectus recession with conventional recession for the correction of esotropia in children. Klin Monatsbl Augenheilkd. 2014;231:988–993.
22. Repka MX, Fisherman PJ, Guyton DL. The site of reattachment of the extraocular muscle following hang-back recession. J Pediatr Ophthalmol Strabismus. 1990;27:286–290.
23. Focosi M, Salvi G, Frosini R Tendon lengthening by fascia lata graft to weaken the action of extraocular muscles. Tsamparkalils J, editor.
24. Boschi MC, Salvi G, Dal Pozzo G. Démonstration par la tomodensitométrie des effets de l’allongement du tendon selonFocosi. Bull Mem Soc Fr Ophthalmol. 1985;96:83–88.
25. Wright KW. Superior oblique silicone expander for Brown syndrome and superior oblique overaction. J Pediatr Ophthalmol Strabismus. 1991;28:101–107.
26. Esser J, Eckstein A. Tendon elongation; a new surgical technique for convergent squint after three wall orbital decompression in thyroid associated ophthalmopathy. Exp Clin Endocrinol Diab. 2006;114:13.
27. Wright KW. Results of superior oblique tendon elongation procedure for sever Brown syndrome. Trans Am Ophthalmol Soc. 2000;98:41–48.
28. Kadircan H. Long-term outcome of a silicone expander for brown syndrome. J Pediatr Ophthalmol Strabismus. 2007;44:164–169.
29. Jitendra N, Nirzari S, Sonal A, et al. Stability and effects of muscle transplantation for very large angle esotropia: A study of 22 patients. Indian J Ophthalmol. 2017;65:607–609. doi:10.4103/ijo.IJO_54_17
30. Dunlap EA, Dunn M, Rossomonda R. Observations on the use of plastic adhesives in muscle surgery with two new potential applications. Trans Am OphthalmolSoc. 1969;67:283–303.
31. Ingram RM. Tissue repair after the operations of recession and resection. Brit J Ophthalmol. 1965;49:18–28. doi:10.1136/bjo.49.1.18
32. Ingram RM. Rate at which muscle becomes joined to sclera after operations of recession resection. Brit J Ophthalmol. 1965;48:235–245. doi:10.1136/bjo.49.5.235
33. Ingram RM. Wound healing after operations on the extraocular muscles on monkeys. Brit J Ophthalmol. 1966;50:185–208. doi:10.1136/bjo.50.4.186
34. Truhlsen SM. The recession operation: histopathologic response and suture reaction and absorption. Trans Am OphthalmolSoc. 1965;63:626–677.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.