Back to Journals » Research and Reports in Urology » Volume 14
Late Distal Ureteral Stricture in Internal Hemipelvectomy Without Bone Reconstruction: A Case Report
Authors Asavamongkolkul A , Chotikawanich E
Received 11 April 2022
Accepted for publication 12 July 2022
Published 26 July 2022 Volume 2022:14 Pages 275—280
DOI https://doi.org/10.2147/RRU.S370265
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Apichat Asavamongkolkul,1 Ekkarin Chotikawanich2
1Department of Orthopaedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand; 2Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Apichat Asavamongkolkul, Department of Orthopaedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, 10700, Thailand, Tel/Fax +66 2-419-7968, Email [email protected]
Abstract: We report the case of a patient with Ewing sarcoma involving the right pelvis in a 14-year-old girl who had multicycles of neo-adjuvant chemotherapy and preoperative radiation therapy. She underwent an internal hemipelvectomy type I resection, according to Enneking and Dunham’s classification without bony reconstruction. There was no intra- and perioperative complication. The patient has good function and needs no gait aids. She can walk with equinus foot compensated for leg shortening 5 centimeters and without a shoe-lift. There is no sign of disease relapse. However, she developed late ureteral stricture at 8-year postoperatively and was successfully treated with a ureteral stent.
Keywords: internal hemipelvectomy, Ewing sarcoma, ureteric stricture, limb-sparing surgery, radiation therapy, mesh graft
Background
Malignant bone tumor involving the pelvis accounts for 5–10%.1,2 External hemipelvectomy (hindquarter amputation) is used as the mainstay surgery for unremoved tumors of the pelvis.3 With the advances in imaging, chemotherapy, radiation therapy, and surgical techniques have allowed more patients to be managed with limb-sparing surgery. An internal hemipelvectomy technique was introduced to remove the tumor with limb preservation in these particular patients.4 Many alternative bone reconstructions following internal hemipelvectomy have been reported by using non-vascularized autograft, free-vascularized autograft, allograft, recycling bone (autoclaved, pasteurized, and extracorporeal radiation), allograft-prosthetic composite (APC), saddle prosthesis, custom prosthesis, arthrodesis and no bone reconstruction.5–17 Complications following internal hemipelvectomy with or without bone reconstruction are reported at around 50–80%. Most complications are related to wound problems, infection, vascular and visceral injury, structural failure, and local recurrence.15,18,19 Although urethral stricture is not a rare complication of pelvic tumors that received radiotherapy, there were a limited amount of literature that reported this particular complication in a patient receiving internal hemipelvectomy. In addition to radiation-related injuries, we believe that repetitive mechanical injuries from altered hip anatomy resulting from internal hemipelvectomy could increase the risk of the late urethral stricture. Herein, we report a case of late distal ureteral stricture following internal hemipelvectomy without bone reconstruction and radiotherapy in a patient with Ewing sarcoma of the right pelvic bone.
Case Presentation
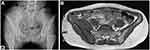
A 14-year-old student girl presented with a painful growing mass around her right flank for three months. She had fever and pain at night around the mass. She walked limping recently. She loose appetite and body weight by three kilograms in the last three months. Plain radiographs of the right pelvis revealed a mixed permeative osteolytic and osteoblastic lesion at the ilium and periacetabulum (Figure 1A). Magnetic resonance imaging (MRI) of the pelvis demonstrated bony destruction at the right ilium extending close to the sacroiliac joint and acetabulum with soft-tissue involvement in iliopsoas and gluteus muscles (Figure 1B).
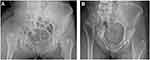
Chest radiograph and computed tomography (CT) chest revealed no active lung lesion. Bone scintigraphy showed increased uptake lesion at right pelvis involving ilium and close to the periacetabulum. Open biopsy confirmed Ewing sarcoma. The patient was administered multicycles of neoadjuvant chemotherapy with vincristine, adriamycin, and cyclophosphamide (VAC) regimen. She had preoperative radiation therapy with a dose of 45 Gy. A preoperative MRI of the pelvis revealed tumor shrinkage from an excellent response to the neoadjuvant therapies. Internal hemipelvectomy with type I resection, according to Enneking and Dunham’s classification of pelvic tumor resection, was performed by making osteotomy at the sacroiliac joint and above the acetabulum20 (Figure 2A). The piece of the iliac bone and pelvic bone tissue was measured at 16.5 x 13 x 5 centimeters. The patient had no bone reconstruction following tumor resection. Operative time was 3 hours, and intraoperative blood loss was recorded at around 1500 mL. The patient had a blood transfusion with pack red cells five units. She was placed in balanced skeletal traction at the tibial tuberosity at a weight of 15 pounds for three weeks after surgery. The final pathological report confirmed 100% tumor necrosis with adequate tumor margins. She had another two cycles of adjuvant chemotherapy postoperatively. An immediate postoperative rehabilitation program was started by strengthening exercise of the psoas, gluteus, hamstring, and quadriceps muscles. Progressive partial weight-bearing with axillary crutches was allowed after eight weeks, and full weight-bearing at 12 weeks. With a regular follow-up at 8-year, she had no signs of local recurrence or distant metastasis. She could walk with Trendelenburg gait without using gait support. She had 5 centimeters leg length discrepancy, and her foot was compensated at a slightly equinus pace. A recent plain radiograph of the pelvis revealed no bone destruction and more inner-upward migration of the head of the femur (Figure 2B). She developed gross hematuria with pain in her right flank. CT scan of the lower abdomen revealed a long segmental diffuse ureteric thickening with enhancement at the right distal ureter, causing mild dilatation of the right proximal ureter and mild right hydronephrosis. There was no bony destruction or soft-tissue mass around the remaining right pelvic bone (Figure 3). She was diagnosed with distal ureteral injury and stricture. She successfully underwent ureteroscopy and ureteric stricture dilation and maintained a ureteric stent. After ureteral dilation, the stent can easily pass through the stricture site. The fluoroscopic and KUB radiographs revealed upward, and inner migration of the head of the femur close to the ureteric-vesical junction within the deformed right pelvic ring (Figure 4A and B). The patient recovered and urinated normally without difficulty and hematuria. The radiation-induced ureteral stricture etiology is generally ureteral ischemia. Thus, the management of this condition is challenging. Previous literature has revealed that endoureterotomy is less effective in ischemic ureteral stricture, with only a 65% to 69% success rate compared to non-ischemic stricture. Accordingly, endoureterotomy is not a treatment of choice for radiation-induced ureteral stricture, and reconstruction was planned instead. Nevertheless, after an extensive discussion on the risk and benefits of the reconstruction procedure, the patient and her family decided not to undergo the operation and continue using a ureteric stent.
 |
Figure 3 CT scan of the lower abdomen illustrated right ureteric stricture (arrow). |
Discussion
Internal hemipelvectomy was accepted for limb-sparing surgery in patients with malignant bone and soft-tissue tumors of the pelvis. Bone reconstruction techniques following internal hemipelvectomy were introduced to maintain the patients’ hip stability, leg length, and function.5–17,21 Internal hemipelvectomy without bone reconstruction or flail hip was reported in the literature with accepted functional outcomes.16,17 Peri- and postoperative complications of internal hemipelvectomy were not uncommon in this challenging surgery due to the relatively large size of the tumor, extensive surgery, and the complexity of pelvic anatomy with major viscera and vessels. Most complications were wound complications, deep infection, structural failure of bone reconstruction, and local recurrence.15,18,19 Campanacci and Capanna reported 56% of complications in 105 patients following internal hemipelvectomy, including infection in 29% and vascular and visceral problems in 19%.2
This patient was treated with multicycles of neoadjuvant chemotherapy and preoperative radiation therapy before definitive surgery with internal hemipelvectomy without bone reconstruction. Guder et al recommended a combined treatment approach for pelvic Ewing sarcoma by tumor resection, and radiation therapy led to local control and overall survival rates compared with those of extremity locations.22 The postoperative management and rehabilitation program of the patient was uneventful. The patient could participate in the class with good recovery and graduated with her bachelor’s later. Even though the patient had 5-centimeter leg length discrepancy, she could compensate by walking with an equinus foot without gait support.
Intra- and perioperative urogenital injury existed in internal hemipelvectomy, including urinary incontinence, ureter stenosis, urethra injury, and bladder injury.2,22 A late incision hernia of the urinary bladder following internal hemipelvectomy was reported in the literature, especially in type III resection according to Enneking and Dunham's classification.23 There was no peri- and postoperative complication in this patient. However, she was diagnosed with distal ureteral stricture following an internal hemipelvectomy of the patient with Ewing sarcoma of the right pelvis. The patient developed this symptom eight years after the index treatments. The primary cause of late ureteral stricture in this patient should be from radiation therapy preoperatively. As we know, radiotherapy is widely used as a curative treatment for pelvic malignancies. Many organs in this location were inevitably exposed to radiation and subsequently developed radiation cystitis, fistulae, strictures, and secondary malignancy. Ureteral criticisms were reported following radiotherapy for pelvic malignancies, especially cervical cancer. The overall incidence of radiation-induced ureteral stricture was 1.0%, 1.2%, 2.2%, 2.5%, and 3.3% at 5, 10, 15, 20, and 25 years, respectively, with a mean latency period of 16.8 years.24 This patient’s associated cause of ureteral stricture might be related to her body weight during standing and walking. The recent plain and fluoroscopic KUB radiographs showed upward and inner migration of the head of the femur close to the ureteric-vesical junction within the deformed right pelvic ring. Previous literature reported the intrapelvic organ compression, including the ureter, by the medial migration of the hip prosthesis.25 Likewise, we believed that the axial loading of the head of the femur during weight-bearing repetitively injured the surrounding structure, especially the right ureter and bladder wall. This effect might worsen the stricture of the distal ureter from previous radiation therapy. Therefore, we recommended using polypropylene mesh as an anchoring material to re-approximate all the muscles attached to the pelvis to gain optimal function. In addition, this anchoring material can also improve the remaining hip stability to prevent upward migration and maintain the leg length equality of the patient who underwent internal hemipelvectomy.26
Conclusions
Internal hemipelvectomy is the mainstay of surgical treatment for Ewing pelvic sarcoma to allow good oncological outcomes. High complications following this extensive surgery and other adjuvant treatment must be a concern. In addition to radiation-induced ureteral ischemia, the repetitive mechanical compression from superomedial migration of the femoral head caused by internal hemipelvectomy might increase the risk of late ureteral stricture. Preventing the femoral head migration might reduce the risk of late ureteral stricture following internal hemipelvectomy.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. Copies of the written consent form are available for review upon request.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shin K-H, Rougraff BT, Simon MA. Oncologic outcomes of primary bone sarcomas of the pelvis. Clin Orthop Relat Res. 1994;304:207–217. doi:10.1097/00003086-199407000-00033
2. Campanacci M, Capanna R. Pelvic resections: the Rizzoli Institute experience. Orthop Clin North Am. 1991;22:65–86. doi:10.1016/S0030-5898(20)31632-1
3. Sugarbaker PH, Chretien PA. Hemipelvectomy for buttock tumors utilizing an anterior myocutaneous flap of quadriceps femoris muscle. Ann Surg. 1983;197:106–115. doi:10.1097/00000658-198301001-00017
4. Eilber FR, Grant TT, Sakai D, Morton DL. Internal hemipelvectomy-excision of the hemipelvis with limb preservation. An alternative to hemipelvectomy. Cancer. 1979;43:806–809. doi:10.1002/1097-0142(197903)43:3<806::AID-CNCR2820430305>3.0.CO;2-Y
5. Akiyama T, Clark JCM, Miki Y, Choong PFM. The non-vascularized fibular graft: a simple and successful method of reconstruction of the pelvic ring after internal hemipelvectomy. J Bone Joint Surg. 2010;92-B:999–1005. doi:10.1302/0301-620X.92B7.23497
6. Chao AH, Neimanis SA, Chang DW, Lewis VO, Hanasano MM. Reconstruction after internal hemipelvectomy: outcomes and reconstruction algorithm. Ann Plast Surg. 2015;74:342–349. doi:10.1097/SAP.0b013e31829778e1
7. Ogura K, Sakuraba M, Miyamoto S, Fujiwara T, Chuman H, Kawai A. Pelvic ring reconstruction with a double-barreled free vascularized fibula graft after resection of malignant pelvic bone tumor. Arch Orthop Trauma Surg. 2015;135:619–625. doi:10.1007/s00402-015-2197-7
8. Langlais F, Lambotte JC, Thomazeau H. Long-term results of hemipelvis reconstruction with allografts. Clin Orthop Relat Res. 2001;388:178–186. doi:10.1097/00003086-200107000-00025
9. Harrington KD. The use of hemipelvis allografts or autoclaved grafts for reconstruction after wide resection of malignant tumors of the pelvis. J Bone Joint Surg. 1992;74-A:331–341. doi:10.2106/00004623-199274030-00003
10. Guo X, Li X, Liu T, Shuai C, Zhang Q. Pasteurized autograft reconstruction after resection of periacetabular malignant bone tumours. World J Surg Oncol. 2017;15:13. doi:10.1186/s12957-016-1065-4
11. Wafa H, Grimer RJ, Jeys L, Abudu AT, Carter SR, Tillman RM. The use of extracorporeally irradiated autografts in pelvic reconstruction following tumour resection. Bone Joint J. 2014;96-B:1404–1410. doi:10.1302/0301-620X.96B10.33470
12. Aljassir F, Beadel GP, Turcotte RE, et al. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin Orthop Relat Res. 2005;438:36–41. doi:10.1097/00003086-200509000-00009
13. Guo W, Li D, Tang X, Ji T. Surgical treatment of pelvic chondrosarcoma involving periacetabulum. J Surg Onco. 2010;101:160–165. doi:10.1002/jso.21442
14. Sun W, Li J, Li Q, Li G, Cai Z. Clinical effectiveness of hemipelvic reconstruction using computer-aided custom-made prostheses after resection of malignant pelvic tumors. J Arthroplasty. 2011;26:1508–1513. doi:10.1016/j.arth.2011.02.018
15. Pant R, Moreau P, Ilyas I, Paramasivan ON, Younge D. Pelvic limb-salvage surgery for malignant tumors. Int Orthop. 2001;24:311–315. doi:10.1007/s002640000197
16. Asavamongkolkul A, Pimolsanri R, Waikakul S, Kiatsevee P. Periacetabular limb salvage for malignant bone tumours. J Orthop Surg. 2005;13:273–279. doi:10.1177/230949900501300310
17. Schwartz AJ, Kiatsevi P, Eilber FC, Eilber FR, Eckardt JJ. The Friedman-Eilber resection arthroplasty of the pelvis. Clin Orthop Relat Res. 2009;467:2825–2830. doi:10.1007/s11999-009-0844-4
18. Griesser MJ, Gellette B, Crist M, et al. Internal and external hemipelvectomy or flail Hip in patients with sarcomas: quality-of-life and functional outcomes. Am J Phys Med Rehabil. 2012;91:24–32. doi:10.1097/PHM.0b013e318232885a
19. Shao QD, Yan X, Sun JY, Xu TM. Internal hemipelvectomy with reconstruction for primary pelvic neoplasm: a systematic review. ANZ J Surg. 2015;85:553–560. doi:10.1111/ans.12895
20. Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg. 1978;60-A:731–746. doi:10.2106/00004623-197860060-00002
21. Angelini A, Drago G, Trovarelli G, Calabro T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: an analysis of 270 patients from one institution. Clin Orthop Relat Res. 2014;472:349–359. doi:10.1007/s11999-013-3250-x
22. Guder WK, Hardes J, Nottrott M, Steffen AJ, Dirksen U, Streitburger A. Pelvic Ewing sarcoma: a retrospective outcome analysis of 104 patients underwent pelvic tumor resection at a single supra-regional center. J Orthop Surg Res. 2020;15(1):534. doi:10.1186/s13018-020-02028-3
23. Jamshidi K, Zandrmhimi F, Bagherifard A, Mohammadi F, Mirzaei A. Type III internal hemipelvectomy for primary bone tumours with and without allograft reconstruction: a comparison of outcomes. Bone Joint J. 2021;103-B:1155–1159. doi:10.1302/0301-620X.103B6.BJJ-2020-2149.R1
24. Gellrich J, Hakenberg OW, Oeshlschlager S, et al. Manifestation, latency and management of late urological complications after curative radiotherapy for cervical carcinoma. Onkologie. 2003;26:334–340. doi:10.1159/000072091
25. Stiehl JB. Acetabular prosthetic protrusion and sepsis: case report and review of the literature. J Arthroplasty. 2007;22(2):283–288. doi:10.1016/j.arth.2006.02.170
26. Asavamongkolkul A, Waikakul S. Using polypropylene mesh graft for soft-tissue reconstruction in internal hemipelvectomy: a case report. World J Surg Oncol. 2012;10:124. doi:10.1186/1477-7819-10-124
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.