Back to Journals » Therapeutics and Clinical Risk Management » Volume 20
LASSO-Based Identification of Risk Factors and Development of a Prediction Model for Sepsis Patients
Authors Hong C, Xiong Y, Xia J, Huang W , Xia A, Xu S, Chen Y, Xu Z, Chen H, Zhang Z
Received 8 August 2023
Accepted for publication 17 January 2024
Published 7 February 2024 Volume 2024:20 Pages 47—58
DOI https://doi.org/10.2147/TCRM.S434397
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Chengying Hong,1 Yihan Xiong,2 Jinquan Xia,3 Wei Huang,4 Andi Xia,1 Shunyao Xu,1 Yuting Chen,1 Zhikun Xu,1 Huaisheng Chen,1 Zhongwei Zhang5
1Department of Critical Care Medicine, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, Guangdong, 518020, People’s Republic of China; 2Neurology Department, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, Guangdong, 518020, People’s Republic of China; 3Department of Clinical Medical Research Center, The Second Clinical Medical College, Jinan University (Shenzhen People’s Hospital), The First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, Guangdong, 518020, People’s Republic of China; 4Department of Clinical Microbiology, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, Guangdong, 518020, People’s Republic of China; 5Department of Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China
Correspondence: Huaisheng Chen, Department of Critical Care Medicine, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, Guangdong, 518020, People’s Republic of China, Email [email protected] Zhongwei Zhang, Department of Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China, Email [email protected]
Objective: The objective of this study was to utilize LASSO regression (Least Absolute Shrinkage and Selection Operator Regression) to identify key variables in septic patients and develop a predictive model for intensive care unit (ICU) mortality.
Methods: We conducted a cohort consisting of septic patients admitted to the ICU between December 2016 and July 2019. The disease severity and laboratory index were analyzed using LASSO regression. The selected variables were then used to develop a model for predicting ICU mortality. AUCs of ROCs were applied to assess the prediction model, and the accuracy, sensitivity and specificity were calculated. Calibration were also used to assess the actual and predicted values of the predictive model.
Results: A total of 1733 septic patients were included, among of whom 382 (22%) died during ICU stay. Ten variables, namely mechanical ventilation (MV) requirement, hemofiltration (HF) requirement, norepinephrine (NE) requirement, septicemia, multiple drug-resistance infection (MDR), thrombocytopenia, hematocrit, red-cell deviation width coefficient of variation (RDW-CV), C-reactive protein (CRP), and antithrombin (AT) III, showed the strongest association with sepsis-related mortality according to LASSO regression. When these variables were combined into a predictive model, the area under the curve (AUC) was found to be 0.801. The AUC of the validation group was 0.791. The specificity of the model was as high as 0.953. Within the probability range of 0.25 to 0.90, the predictive performance of the model surpassed that of individual predictors within the cohort.
Conclusion: Our findings suggest that a predictive model incorporating the variables of MV requirement, HF requirement, NE requirement, septicemia, MDR, thrombocytopenia, HCT, RDW-CV, CRP, and AT III exhibiting an 80% likelihood of predicting ICU mortality in sepsis and demonstrates high accuracy.
Keywords: sepsis, mortality, LASSO regression, predictive model, ICU
Background
Sepsis is a pathological state characterized by an aberrant immune response triggered by an infection, leading to impaired organ function or failure.1,2 This condition poses a significant threat to life and demands immediate identification and treatment.1 The mortality rate associated with sepsis is estimated to be approximately 30%, with severe sepsis and septic shock demonstrating even higher rates of mortality.3
In recent years, the PubMed database has seen an abundance of over 500 models dedicated to predicting sepsis mortality. In principle, variations in individual indicators have the potential to introduce new models, as these approaches heavily rely on data-driven algorithms.4 The application of computer-based technologies, which have demonstrated considerable success in the industrial sector, has now permeated the field of medicine, becoming an essential component across all its domains. Artificial intelligence has unlocked novel avenues for addressing and resolving both theoretical and practical challenges in healthcare.5 While logistic regression models incorporating specific factors exhibit a similar area under the curve (AUC) in the receiver operating characteristic (ROC) analysis compared to machine learning approaches,6 the latter has the ability to identify factors influencing the clinical outcomes of sepsis, thereby contributing to prediction and enhancement of these outcomes.7
The least absolute shrinkage and selection operator (LASSO) regression is a statistical technique employed for variable selection and regularization in the context of linear regression analysis.8 The primary goal of LASSO regression is to minimize the sum of squared residuals while adhering to the constraint that the sum of the absolute values of regression coefficients remains below or equal to a predefined constant. By imposing this constraint, the coefficients are effectively shrunk towards zero, facilitating variable selection by setting certain coefficients exactly to zero. This mechanism mitigates overfitting and enhances the accuracy and interpretability of the model.9 In our study, we utilized LASSO regression to identify the minimal set of predictive indicators for ICU mortality in sepsis patients admitted to the intensive care unit.
Method
Inclusion Criteria
Sepsis is now defined as life-threatening organ dysfunction caused by a dysregulated host response to infection.1 The inclusion criteria are as follows: 1) Patients were diagnosed with infection, 2) The patient has organ dysfunction due to infection. Following the Sepsis-3.0 diagnostic criteria, patients were screened for sepsis. To ensure comprehensive screening, chest X-ray and lung CT scans were employed to identify pulmonary infections, while evidence of abdominal, biliary, urinary tract, and bloodstream infections was also taken into consideration. Additionally, a white blood cell count exceeding 12 × 109/L or falling below 4 × 109/L served as a supplementary diagnostic criterion for sepsis. Clinical and laboratory findings were evaluated to assess organ function, including the following: 1) respiratory rate exceeding 20 breaths per minute or the requirement for mechanical ventilation (MV). Patients requiring mechanical ventilation due to respiratory failure were categorized as “MV requirement”. 2) serum creatinine levels surpassing 144 μmol/L or the need for blood purification therapy. Patients undergoing hemofiltration (HF) were classified as “HF requirement”. 3) total bilirubin levels surpassing 34.1 μmol/L. 4) mean arterial pressure (MAP) falling below 60 mmHg or the necessity of norepinephrine (NE) as a vasopressor to maintain blood pressure in cases of circulatory failure. Patients receiving norepinephrine treatment were identified as “NE requirement”. 5) platelet count lower than 100 × 109/L. Patients with documented infections, along with organ dysfunction, were considered to have sepsis and were included in the study.
Exclusion Criteria
Patients will be excluded if they meet the following criteria:
- Patients were diagnosed without infection.
- Patients suffered infectious diseases without sign of organ failure.
- Age less than eighteen.
Intervention Measures and Observation Indicators
Upon admission to the intensive care unit (ICU), blood cultures were collected, and patients received empirical antimicrobial therapy. Mechanical ventilation and blood purification were implemented based on the severity of organ failure. Subsequently, adjustments were made to the administration of antibiotics, other medications, and organ support strategies in response to changes in the patient’s condition and microbial cultures. The Sequential Organ Failure Assessment (SOFA) score was calculated using extracted data, and various parameters were recorded, including lactate elevations (≥1.5 mmol/L), positive cultures for multidrug-resistant microorganisms, length of stay in the ICU (LOS, measured in days), duration of mechanical ventilation (in hours), and final clinical outcomes (improvement or death). Additionally, other laboratory indicators upon admission to the ICU were also documented.
Statistical Analysis
The patients were categorized into survival and non-survival groups based on their outcomes, and a comparison of baseline characteristics was performed between the two groups. Normally distributed continuous variables were presented as mean ± standard deviation (M±SD) and analyzed using the Student’s t-test. Non-normally distributed continuous variables were reported as the median and interquartile range and analyzed using the Mann–Whitney U-test.
The LASSO method was employed to investigate the clinical and laboratory indicators that exhibited differences between the two groups. It aimed to identify significant prognostic risk factors for sepsis, construct a prediction model, and assess the model’s predictive performance using the receiver operating characteristic (ROC) curve analysis. The area under the curve (AUC) of the risk factor model for mortality prediction was calculated, along with the confidence interval and significance test using non-parametric bootstrap resampling (resampling times = 500). The optimal threshold was determined to evaluate diagnostic specificity, sensitivity, accuracy, positive and negative likelihood ratios, as well as positive and negative predictive values. Discrimination and calibration analyses were conducted to assess the predictive capability of the developed model. Additionally, decision curve analyses (DCA) were employed to validate the clinical utility of the nomograph. Statistical significance was defined as p < 0.05. The data analysis and statistical procedures were performed using EmpowerStats software 4.0 (R language) and R Studio 4.0.4 software for Windows.
Results
Baseline Characteristics of the Patients
A total of 1996 cases were admitted to the intensive care unit (ICU) between December 2016 and July 2019. Among them, 1733 cases met the inclusion criteria and were diagnosed with sepsis. In the ICU, 382 cases resulted in death, corresponding to a mortality rate of 22.04%. Of these patients, 1013 were male and 720 were female. The mean age was 61.11 ± 19.62 years. The most common sites of infection were the lungs (1098 cases), bloodstream (220 cases), abdomen (41 cases), biliary tract (26 cases), and urinary tract (8 cases). The remaining patients were diagnosed with sepsis based on significant increases in inflammatory indicators, even though the specific infection sites were unclear upon admission to the ICU. A total of 666 patients experienced significant shock and required the administration of norepinephrine (NE) to maintain blood pressure. Additionally, 483 cases exhibited lactacidosis, indicating microcirculation dysfunction. The study included 1067 patients with respiratory failure who required mechanical ventilation, 345 patients with acute kidney injury (AKI) necessitating blood purification treatment, 612 patients with thrombocytopenia, and 321 patients with elevated bilirubin levels. The patients were divided into survival and non-survival groups. There was a notable difference in the incidence of organ failure between the two groups, with the mortality group demonstrating a significantly higher incidence compared to the survival group (p < 0.001 for both). The mortality group also had a higher Sequential Organ Failure Assessment (SOFA) score compared to the non-mortality group (11.07 ± 4.52 vs 10.46 ± 4.38, p < 0.001). Table 1 presents the demographic characteristics of the patients.
 |
Table 1 Demographic Characteristics of the Patients |
The survival group of patients exhibited a significantly shorter length of stay (LOS) in the intensive care unit (ICU) compared to the non-survival group (4 days vs 8 days, p < 0.0001). Among the cases, 1067 experienced severe respiratory failure and required mechanical ventilation for support. The duration of mechanical ventilation in the survival group was also significantly shorter than that in the non-survival group (34 hours vs 99.5 hours, p < 0.001). The comparisons of ICU LOS and mechanical ventilation duration are presented in Table 2.
 |
Table 2 Comparisons of Clinical Outcomes Between Survival and Non-Survival Groups |
Predictive Indicators Selected from LASSO Regression
From the LASSO regression analysis, a total of 10 variables were identified as potential predictors of sepsis-related mortality (Figure 1A and B). These variables included the need for mechanical ventilation (MV requirement), the need for hemofiltration (HF requirement), the need for norepinephrine support (NE requirement), septicemia, multidrug resistance (MDR), thrombocytopenia, red cell distribution width coefficient of variation (RDW-CV), hematocrit (HCT), C-reactive protein (CRP), and antithrombin III (AT III). (refer to Table 3).
 |
Table 3 Predicting Indicators Screened from LASSO Regression |
Discrimination and Validation of the Predictive Model
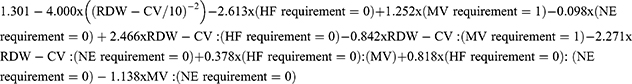
The predictive model for ICU mortality in sepsis incorporated the ten variables selected by LASSO regression. The algorithm of the model is presented as follows:
Within the cohort, approximately 7% of the data were missing, predominantly in the index of AT III (Figure 2A). The area under the curve (AUC) of the model was calculated as 0.801, indicating excellent predictive performance (Figure 2B). To validate the model, 25% of the patients from this cohort were randomly selected as the validation set (V set). The AUC of the V set in the model was determined to be 0.791 (Figure 2B). The predictive model demonstrated an accuracy of 0.819, a sensitivity of 0.348, and a specificity of 0.953.
Calibration of the Predictive Model
Based on the predicted probabilities, the data was stratified into ten groups using deciles. The observed values and predicted values for each group were represented in a coordinate form. Line graphs were utilized to depict the observed values and predicted values separately. This graphical representation effectively showcased the disparities between the actual observed values and the model-predicted values for each group. Furthermore, it facilitated an overall assessment of the model’s calibration performance. The close alignment between the actual values and predicted values across the groups indicated a well-calibrated predictive model (Figure 2C and D).
Clinical Use of the Models
To validate the findings of this study, decision curve analysis (DCA) was employed. The analysis demonstrated that the models developed using the primary cohorts exhibited a threshold probability ranging from 0.25 to 0.90 (Figure 2E). Within this probability range, the predictive performance of the model surpassed that of individual predictors within the cohort. The DCA curve of the validation data resembled that of the training data, further confirming the model’s favorable predictive effect (Figure 2F).
Discussion
Sepsis is a severe systemic infection that leads to fetal multiple organ dysfunction syndrome (MODS).10 The mortality rate associated with sepsis is alarmingly high.11 A large observational study conducted in the United States revealed a relatively stable overall mortality rate of sepsis over the past decade, with an estimated 1 in 4 patients succumbing to the condition during hospitalization.12 Despite being a leading cause of death worldwide, sepsis continues to pose significant challenges in terms of high mortality rates. Consequently, researchers are actively investigating novel therapies and interventions to enhance patient outcomes.11
While medical scientists and clinical experts agree that certain key factors can serve as prognostic indicators for sepsis,13 different studies have identified varying high-risk factors.14,15 In our study, we examined data from a cohort of 1733 septic patients and identified ten variables (MV requirement, HF requirement, NE requirement, Septicemia, MDR, thrombocytopenia, RDW-CV, CRP, AT III, and APTT) that exhibited the strongest associations with sepsis-related mortality using Lasso regression. When combined to form a predictive model, these variables yielded an AUC of 0.801. The validation group demonstrated an AUC of 0.791. Although the predictive model exhibited low sensitivity (0.348), it demonstrated favorable accuracy (0.819) and a high specificity of 0.953.
Results of a recent study revealed several autonomous predictors of mortality in sepsis, including serum cholinesterase, total bilirubin, respiratory failure, lactic acid, creatinine, and pro-brain natriuretic peptide. The area under the ROC curve was 0.847 in the modeling group and 0.826 in the validation group.16 Given the heterogeneity observed in sepsis research, with patients presenting at various stages of the disease course, predicting outcomes in sepsis has produced diverse findings.17 One study identified age, Sequential Organ Failure Assessment (SOFA) score, serum myoglobin (MYO), use of vasopressors, and mechanical ventilation as independent risk factors for one-year mortality. Combining these variables in a model improved the AUC of the predictive curve.18 However, the inclusion of the SOFA score, which assesses multiple organ systems simultaneously, may introduce overlap and potentially yield inaccurate results. Other studies have also demonstrated successful prognostic predictions by excluding the SOFA score.19,20 Another study proposed peritonitis, respiratory failure, cardiac insufficiency, consciousness disturbance, tumor history, albumin level, and creatinine level at ICU admission as predictive factors for 30-day mortality. The predictive model combining these factors yielded an AUC of 0.834, which closely aligns with our results. These models encompassed microcirculation, respiratory function, renal function, and cardiac function as relevant factors.21
In the intensive care unit (ICU), critically ill patients necessitate increased equipment or medication support, indicating a more severe condition.22 Patients with sepsis-induced acute kidney injury (AKI) often require blood purification therapy.23 The primary indications for renal replacement therapy (RRT) were oligo-anuria (57.4%), metabolic acidosis (52.1%), and elevated plasma urea levels (47.9%).24 Existing literature indicates no significant differences in mortality among different RRT modalities.25 While continuous renal replacement therapy (CRRT) is considered a promising clinical technology that can potentially reduce ICU and hospital stays, decrease medical costs, provide long-term benefits to patients, and alleviate social and personal burdens, it is important to note that further research is required to fully assess its effectiveness and safety.26 Whether renal replacement therapy has an effect on mortality in critically ill patients remains a topic of debate.27 The effectiveness of relood purification therapy signifies a critical stage in the patient’s condition.28
Another crucial variable, the need for norepinephrine (NE), signifies patients with severe shock requiring NE support for circulatory function.29 Shock, particularly septic shock, is associated with unfavorable clinical outcomes.29 Norepinephrine is the primary vasoactive medication used for septic shock.30 Maintaining mean arterial pressure (MAP) above 65 mmHg with norepinephrine is a common practice and serves as an indicator of the severity of circulatory shock. Patients with septic shock tend to have prolonged ICU length of stay (LOS).31 The administration of norepinephrine in patients with severe sepsis can enhance their clinical outcomes. Utilizing norepinephrine to maintain blood pressure is correlated with improved clinical outcomes, particularly in patients requiring intensified infection control strategies.32 Evidently, patients with septic shock exhibit a higher mortality rate compared to those without shock, emphasizing shock as an independent predictor of unfavorable clinical outcomes.2
Other variables can serve as predictors of sepsis mortality. Hematocrit (Hct) is a blood test that measures the proportion of red blood cells in the total blood volume, expressed as a percentage.33 A low HCT level independently increases the risk of 30-day mortality in sepsis patients and can be used as a significant predictor of clinical outcomes.34 Combining HCT with albumin (ALB) can also predict the prognosis of sepsis.35 Recently, red cell distribution width (RDW) has been recognized for its correlation with disease severity and prognostic potential.36 RDW, whether used alone or in combination with other clinical and laboratory parameters, has demonstrated prognostic value in predicting clinical outcomes in sepsis.37 However, there are limited studies utilizing the coefficient of variation (RDW-CV) of RDW to predict clinical outcomes in sepsis. On the other hand, sepsis often leads to significant coagulation dysfunction.38 APTT, in combination with other factors, has been used to predict the mortality rate in septic patients.39 Indicators related to organ dysfunction, such as acute physiology and chronic health assessment II (APACHE II) score, APTT, total bilirubin, creatinine, hypotension, chronic kidney disease, and the need for continuous renal replacement therapy (CRRT), are associated with microcirculatory impairment and increased sepsis mortality.40 Overall, reduced HCT and prolonged APTT are important indicators for predicting the prognosis of sepsis. It is worth noting that inflammation and coagulation often interact in the pathophysiological process of sepsis. C-reactive protein (CRP) is an inflammatory marker that has limited value in predicting 30-day ICU mortality.41 The predictive indicators mentioned in previous studies largely overlap with those in our study. By employing LASSO regression, our study identified simple clinical and laboratory indicators for predicting ICU mortality in sepsis and achieved a higher prediction AUC, underscoring the significance of these ten indicators. Indicators reflecting inflammation, coagulation, and important organ functions play critical roles in the model.
Limitation
Despite identifying four significant prediction indicators in the sepsis cohort and validating the models’ predictive function using internal data, this study is retrospective in nature and unable to establish definitive causal relationships. The reliance on past records and data limits our ability to fully control variables or interventions, thereby precluding the confirmation of causal relationships. Nevertheless, the findings offer valuable insights and hypotheses for future prospective studies to investigate and ascertain the causal nature of these relationships.
Conclusion
By incorporating the variables of MV requirement, HF requirement, NE requirement, Septicemia, MDR, thrombocytopenia, RDW-CV, CRP, AT III, and APTT, a predictive model may indicate enhanced prognostic capability for sepsis mortality. The model exhibits an 80% probability of accurately predicting ICU mortality in sepsis cases, thus demonstrating high accuracy.
Ethics Approval and Consent to Participate
This study was approved by the Medical Department and its affiliated institution, the Medical Research Ethics Committee of Shenzhen People’s Hospital. Serial number: LL-KY-2019508.
Ethical Statement
The study of LASSO-based identification of risk factors and development of a prediction model for sepsis patients was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and complied with relevant Chinese regulations. The research protocol was approved by the Medical Department and its affiliated institution, the Medical Research Ethics Committee of Shenzhen People’s Hospital, with the serial number LL-KY-2019508. To ensure the privacy and confidentiality of the subjects, all data used in this study have been encrypted. The encrypted data can only be accessed and decrypted by authorized personnel from the Ethics Committee and Information Department. Both the researchers involved in the study and the subjects themselves are unable to trace or identify any individual participants without going through the proper decryption process.
The protection of privacy and personally identifiable information is of utmost importance in this study, and all necessary measures have been taken to safeguard the confidentiality and anonymity of the subjects. Any potential risks or harms to the participants have been minimized, and their rights and welfare have been prioritized throughout the research process.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2016. Crit Care Med. 2017;45(3):486–552. doi:10.1097/CCM.0000000000002255
2. Shankar-Hari M, Phillips GS, Levy ML, et al. Sepsis definitions task force. developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):775–787. doi:10.1001/jama.2016.0289
3. Singer M, S DC, W SC, et al. The third international consensus definitions for sepsis and septic shock. JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
4. Alanazi HO, Abdullah AH, Qureshi KN. A critical review for developing accurate and dynamic predictive models using machine learning methods in medicine and health care. J Med Syst. 2017;41(4):69. doi:10.1007/s10916-017-0715-6
5. Brdička R. Artificial intelligence and modern information and communication technologies entering medicine. Cas Lek Cesk. 2019;158(2):87–91.
6. Chiu YM, Courteau J, Dufour I, Vanasse A, Hudon C. Machine learning to improve frequent emergency department use prediction: a retrospective cohort study. Sci Rep. 2023;13(1):1981. doi:10.1038/s41598-023-27568-6
7. Long J, Wang M, Li W, et al. The risk assessment tool for intensive care unit readmission: a systematic review and meta-analysis. Intensive Crit Care Nurs. 2023;76:103378. doi:10.1016/j.iccn.2022.103378
8. Tibshirani R. Regression shrinkage and selection via the lasso. J Royal Statistical Soc. 1996;58(1):267–288.
9. Zou H, Hastie T. Regularization and variable selection via the elastic net. J Royal Statistical Soc. 2005;67(2):301–320. doi:10.1111/j.1467-9868.2005.00503.x
10. Gupta S, Hayek SS. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2021;181(4):509–515. doi:10.1001/jamainternmed.2020.8587
11. Rudd KE, Kissoon N, Limmathurotsakul D, et al. The global burden of sepsis: barriers and potential solutions. Crit Care. 2021;25(1):348. doi:10.1186/s13054-021-03767-3
12. Kadri SS, Rhee C, Strich JR, et al. Estimating ten-year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest. 2017;151(2):278–285. doi:10.1016/j.chest.2016.07.010
13. Rech MA, Bennett S, Chaney W, Sterk E. Risk factors for mortality in septic patients who received etomidate. Am J Emerg Med. 2015;33(10):1340–1343. doi:10.1016/j.ajem.2015.07.062
14. Pansiritanachot W, Ruangsomboon O, Limsuwat C, Chakorn T. Independent risk factors of mortality in patients with sepsis receiving single-dose etomidate as an induction agent during rapid sequence intubation in a large tertiary emergency department in Thailand. BMC Emerg Med. 2022;22(1):94. doi:10.1186/s12873-022-00658-w
15. Wang YX, Li XL, Zhang LH, et al. Machine learning algorithms assist early evaluation of enteral nutrition in ICU patients. Front Nutr. 2023;10:1060398. doi:10.3389/fnut.2023.1060398
16. Lu B, Pan X, Wang B, et al. Development of a nomogram for predicting mortality risk in sepsis patients during hospitalization: a retrospective study. Infect Drug Resist. 2023;16:2311–2320. doi:10.2147/IDR.S407202
17. Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–2244. doi:10.1056/NEJMoa1703058
18. Liu Y, Zhang Y, Zhang X, et al. Nomogram and machine learning models predict 1-year mortality risk in patients with sepsis-induced cardiorenal syndrome. Front Med Lausanne. 2022;9:792238. doi:10.3389/fmed.2022.792238
19. Liu H, Zhang L, Xu F, et al. Establishment of a prognostic model for patients with sepsis based on SOFA: a retrospective cohort study. J Int Med Res. 2021;49(9):3000605211044892. doi:10.1177/03000605211044892
20. Ren Y, Zhang L, Xu F, et al. Risk factor analysis and nomogram for predicting in-hospital mortality in ICU patients with sepsis and lung infection. BMC Pulm Med. 2022;22(1):17. doi:10.1186/s12890-021-01809-8
21. Wang B, Chen J. Establishment and validation of a predictive model for mortality within 30 days in patients with sepsis-induced blood pressure drop: a retrospective analysis. PLoS One. 2021;16(5):1.
22. Frank CE, Buchman TG, Simpson SQ, et al. Sepsis among medicare beneficiaries: 4. precoronavirus disease 2019. Crit Care Med. 2021;49(12):2058–2069. doi:10.1097/CCM.0000000000005332
23. Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–1964. doi:10.1016/S0140-6736(19)32563-2
24. Jolly F, Jacquier M, Pecqueur D, et al;READIAL Study group. Management of renal replacement therapy among adults in French intensive care units: a bedside practice evaluation. J Intensive Med. 2023;3(2):147–154. doi:10.1016/j.jointm.2022.10.005
25. Wang AY, Bellomo R. Renal replacement therapy in the ICU: intermittent hemodialysis, sustained low-efficiency dialysis or continuous renal replacement therapy? Curr Opin Crit Care. 2018;24(6):437–442. doi:10.1097/MCC.0000000000000541
26. Ma H, Liu H, Liu Y, Wang Y, He J, Yang Q. Efficacy of continuous renal replacement therapy and intermittent hemodialysis in patients with renal failure in intensive care unit: a systemic review and meta-analysis. Evid Based Complement Alternat Med. 2023;2023:8688974. doi:10.1155/2023/8688974
27. Klingele M, Baerens L. Impact of renal replacement therapy on mortality in critically ill patients-the nephrologist’s view within an interdisciplinary intensive care team. J Clin Med. 2021;10(15):3379. doi:10.3390/jcm10153379
28. Bateman RM, Sharpe MD, Jagger JE, et al. 36th international symposium on intensive care and emergency medicine: Brussels, Belgium. Crit Care. 2016;20(Suppl 2):94. doi:10.1186/s13054-016-1208-6
29. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–e1143. doi:10.1097/CCM.0000000000005337
30. Bitton E, Zimmerman S, Azevedo LCP, et al. An international survey of adherence to surviving sepsis Campaign guidelines 2016 regarding fluid resuscitation and vasopressors in the initial management of septic shock. J Crit Care. 2022;68:144–154. doi:10.1016/j.jcrc.2021.11.016
31. Tuttle E, Wang X, Modrykamien A. Sepsis mortality and ICU length of stay after the implementation of an intensive care team in the emergency department. Intern Emerg Med. 2023;2023:1–8.
32. Petros S. Volumen- und vasoaktive therapie bei sepsis [fluid and vasopressor therapy in sepsis]. Med Klin Intensivmed Notfmed. 2023;118(2):163–171. doi:10.1007/s00063-022-00976-8
33. Qaseem A, Humphrey LL, Fitterman N, Starkey M, Shekelle P. Clinical guidelines committee of the American college of physicians. Treatment of anemia in patients with heart disease: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2013;159(11):770–779. doi:10.7326/0003-4819-159-11-201312030-00009
34. Luo M, Chen Y, Cheng Y, Li N, Qing H. Association between hematocrit and the 30-day mortality of patients with sepsis: a retrospective analysis based on the large-scale clinical database MIMIC-IV. PLoS One. 2022;17(3):1.
35. Wang Z, Zhang L, Li S, et al. The relationship between hematocrit and serum albumin levels difference and mortality in elderly sepsis patients in intensive care units-A retrospective study based on two large database. BMC Infect Dis. 2022;22(1):629. doi:10.1186/s12879-022-07609-7
36. Zhang FX, Li ZL, Zhang ZD, Ma XC. Prognostic value of red blood cell distribution width for severe acute pancreatitis. World J Gastroenterol. 2019;25(32):4739–4748. doi:10.3748/wjg.v25.i32.4739
37. Wu H, Liao B, Cao T, Ji T, Huang J, Ma K. Diagnostic value of RDW for the prediction of mortality in adult sepsis patients: a systematic review and meta-analysis. Front Immunol. 2022;13:997853. doi:10.3389/fimmu.2022.997853
38. Yu SH, Ma YT, Li X. The correlation between coagulation function and prognosis in patients with acute respiratory distress syndrome caused by extrapulmonary sepsis or pulmonary infection. Zhonghua Nei Ke Za Zhi. 2021;60(7):650–655. doi:10.3760/cma.j.cn112138-20201217-01017
39. Chen R, Zhou X, Rui Q, Wang X. Combined predictive value of the risk factors influencing the short-term prognosis of sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32(3):307–312. doi:10.3760/cma.j.cn121430-20200306-00218
40. He M, Huang J, Li X, Liang S, Wang Q, Zhang H. Risk factors for mortality in sepsis patients without lactate levels increasing early. Emerg Med Int. 2023;2023:6620157. doi:10.1155/2023/6620157
41. Schupp T, Weidner K, Rusnak J, et al. C-reactive protein and procalcitonin during course of sepsis and septic shock. Ir J Med Sci. 2023; 1–12. doi:10.1007/s11845-023-03385-8
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.