Back to Journals » Nature and Science of Sleep » Volume 11
Laser-assisted uvulopalatoplasty (LAUP) complications and side effects: a systematic review
Authors Wischhusen J , Qureshi U, Camacho M
Received 28 January 2019
Accepted for publication 7 April 2019
Published 27 May 2019 Volume 2019:11 Pages 59—67
DOI https://doi.org/10.2147/NSS.S178540
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sutapa Mukherjee
Jeffrey Wischhusen,1 Uneeb Qureshi,2 Macario Camacho3
1School of Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD, USA; 2United States Public Health Service, Indian Health Service, Uniformed Services University, Bethesda, MD, USA; 3Department of Otolaryngology, Tripler Army Medical Center, Honolulu, HI, USA
Objective: Laser-assisted uvulopalatoplasty (LAUP) has been used as a treatment option for snoring and obstructive sleep apnea for almost three decades. It has been previously reported that some patient’s sleep-disordered breathing worsened following surgery. The aim of this paper is to further elucidate the specific complications of LAUP.
Data sources: A systematic search of the electronic databases MEDLINE/PubMed, Google Scholar, and Embase.
Review methods: The PRISMA statement was followed. Databases were searched from inception through September 2, 2018. The following search was applied to MEDLINE/PubMed ((laser AND uvul*) OR (LAUP) OR (LAVP) OR (laser AND (apnea OR apnoea OR sleep))).
Results: Forty-two studies with a mean follow-up of 16.1 months reported complications on 3,093 total patients who underwent LAUP. The percentages and associated complications of LAUP are as follows: bleeding (2.6%), candidiasis (0.3%), dryness (7.2%), dysgeusia (0.3%), dysosmia (0.2%), globus sensation (8.2%), surgical site infection (1.3%), velopharyngeal (VP) insufficiency (3.9%), and VP stenosis (1.6%). The mean duration of patient-reported pain in studies that reported pain was 11.65 days. Only globus and VP insufficiency had a significant incidence compared with either the general population or the post-oropharyngeal surgery population with relative risks of 1.48 and 2.25, respectively. Overall, there were approximately 26 complications per 100 patients who underwent LAUP.
Conclusion: LAUP is associated with a statistically significant rate of VP insufficiency and globus sensation; however, studies lack details of surgical approaches, suggesting that in a population identified as good candidates, a tissue-sparing approach may result in fewer complications.
Keywords: LAUP, uvulopalatoplasty, outcomes, complications
Introduction
Laser-assisted uvulopalatoplasty (LAUP) is a method of treatment for snoring and obstructive sleep apnea (OSA) that was first described in 1990 by Dr Kamami. The procedure was based on progressive widening of the oropharynx by “successive vaporizations of the vibrating soft palate, wide posterior tonsil pillars, and redundant posterior pharyngeal mucosa” to prevent obstructions during sleep.1 While evaluating this technique, he reported that the use of the carbon dioxide (CO2) laser for uvulopalatoplasty had many advantages to conventional uvulopalatoplasty, including avoidance of hospitalization and general anesthesia, and the idea that it is a procedure that can be performed reliably, in-clinic, and is both hemostatic and relatively painless.1 The disadvantages were cited as cost, multiple treatment sessions, and technical setup.1 In a follow-up study, he reported 40 of 46 patients had >50% reduction in respiratory disturbance index (RDI) but only half of those 40 (43.5%) had a significant reduction in apnea-hypopnea index (AHI) or snoring. The six remaining patients were reported as relative failures who did not have any reduction in RDI or AHI.2
In 1994, the use of LAUP for treatment of snoring and OSA had been recommended against by the American Sleep Disorders Association for inadequate data and controlled studies in peer-reviewed journals.3 A 1999 meta-analysis on LAUP by Verse and Pirsig upheld the recommendation that “LAUP and its related procedures presently should not be recommended for the treatment of any severity of OSA” because long-term results were lacking; however, “short-term results are promising.”4
A 2017 metanalysis and review of the literature, by Camacho et al, reported on the effects of LAUP on AHI and lowest oxygen saturation (LSAT). It found that LAUP had a minimal effect on LSAT and reduced the overall AHI by 32% among all patients; however, LAUP was successful for only 23% of patients.5 On an individual basis, 44% of patients reportedly had worsening of the AHI. In light of this new long-term information, this systematic review aims to report the complications and side effects of LAUP to supplement long-term outcome data.
Materials and methods
During the investigation for this systematic review, the PRISMA statement and checklist were followed as closely as possible.6 The articles were reviewed for relevance and had the number and types of complications compiled for analysis. Complications were recorded as an average number of that specific complication per person per study and a standard error of the means was calculated to create the 95% confidence interval (CI) and extrapolate the data to a larger population for simplistic interpretation. The variability is reported as either standard deviation or standard error of the mean where applicable.
Relative risk (RR, or risk ratio) was computed by taking the ratio of complications (eg, rate of complication X for LAUP divided by the rate of complication X in the general population). The point estimate is the RR obtained from our literature review. Unfortunately, the RR does not follow a normal distribution. However, the natural log (ln) of the RR values are approximately normalized and was used to produce the CIs presented. The antilog of the upper and lower limits of the CI for ln(RR) provided the published CIs.
Search parameters and study selection
A systematic search of the electronic databases MEDLINE/PubMed and Embase was conducted before September 2, 2018 using the following search parameters: ((laser AND uvul*) OR (LAUP) OR (LAVP) OR (laser AND (apnea OR apnoea OR sleep))).
The literature search was performed independently by the authors. Study titles and abstracts were screened and eligible studies were identified as those that reported outcomes, complications, or side effects of LAUP. Complications and side effects of LAUP included bleeding, candidiasis, dehiscence, dryness, dysgeusia, dysosmia, globus sensation, surgical site infection (SSI), velopharyngeal (VP) insufficiency [reported as VP insufficiency, hypernasal voice, or pharyngonasal reflux], and VP stenosis [reported as VP stenosis or posterior pillar narrowing]. The references of the initial articles were evaluated and used for searching for additional literature. Our search yielded 42 articles that included detailed information about LAUP complications or outcomes.
Protocol approval
Tripler Army Medical Center was contacted and Protocol 16N14 was approved and used for this study. Formal consent was not required.
Results
Forty-two articles evaluated LAUP complications with a mean duration of patient follow-up of 16.1 months, a median of 6 months, and a range of 0.5–134 months. The total number of patients involved was 3,093. The studies pertinent to this systematic review are listed in Table 1 with their sample size and mean follow-up time. A common side effect of surgery is pain; however, only 15 studies commented on pain as a side effect. The mean duration of patient-reported pain for the 975 patients in these studies was 11.65 (s=2.56) days. Ferguson et al did not report a duration of patient-reported pain but instead reported that 2 of 21 patients refused further procedures due to severe pain that occurred after the primary surgery, even though the pain resolved within several days.7 Of the studies that commented on pain, only two of those reported the mean duration of narcotic usage. The mean duration of narcotic usage was 5.56 days among the 25 patients in the two studies.
The LAUP research found in this review reported the following pertinent complications: bleeding, candidiasis, dehiscence, dryness, dysgeusia, dysosmia, globus sensation, SSI, VP insufficiency, and VP stenosis. The values in Table 2 represent the specific complications per 1,000 patients in those 42 combined studies. The total number of LAUP complications based on a population of 1,000 patients with a 95% CI is 255.71±23.33 There were no reported cases of dehiscence or VP fistulas. Globus and dryness occurred in about 7–8% of cases. Bleeding and VP insufficiency each occurred in 2–4% of cases. SSI and VP stenosis occurred in 1–2% of cases. Candidiasis, dysgeusia, and dysosmia occurred in fewer than 1% of cases. Reviewing the literature revealed four studies that explicitly reported no complications occurred for the 174 patients in those studies.8,14,20,34 Another study reported that the only complication or side effect was pain.9
 | Table 2 Compiled statistics of the specific complications of laser-assisted uvulopalatoplasty that were reported by all 42 studies |
To understand the true risk of LAUP complications, the incidence rates reported in Table 2 were compared to selected population studies. These studies were selected based on the following: recent publication, study type (with reviews and meta-analyses favored over cohort studies), demographic matching (eg, gender), and those matching for oral surgical or outpatients. Relative risk was calculated using standard 2×2 tables and using the same error analysis described in the methods section. Not all incidence rates are published in the literature, but the rates we were able to obtain from the literature review were compared to reference surgical populations if available.
The only significant complications based on RR are globus sensation49 and VP insufficiency50 with 95% CI of 1.07–2.06 and 1.29–3.94, respectively. The risks of post-operative bleeding,51–54 dysgeusia,49 dysosmia,49 and oral dryness49 were not significantly elevated as compared to the referred populations. Candidiasis,55 SSI,56 and VP stenosis57 rates did not significantly correlate as LAUP complications.
Discussion
It was previously reported by Camacho et al in their 2017 meta-analysis and review of the literature that LAUP had a minimal effect on LSAT and caused worsening of the AHI in 44% of patients.5 Due to these seemingly poor outcomes, the concern is now whether or not the procedure should be performed at all and if so, what potential complications could be anticipated. Fortunately, there are many publications that reported on these specific complications of LAUP; however, there are some significant limitations with these studies that have an impact on the interpretation of the data. The most important is that some of the complications were not commented on as transient or long term. There are obvious transient complications like bleeding, candidiasis, dehiscence, and SSI; however, it is unclear if dryness, globus, dysgeusia, dysosmia, and VP insufficiency were related to post-operative inflammation or if they are persistent complications. This is an important aspect of determining the weight the complications should have when weighing the potential benefits of a procedure against the risks.
When evaluating the rates of complications, it is important to not only look at the RR but the average complications reported per person per study because the number of reported complications reflects actual outcomes of the procedure whereas RR will provide a basis of how this data relates to the general or post-oropharyngeal surgery populations. Overall, there was an average of about 0.256±0.023 complications per patient reported in the 42 studies which extrapolates to a 95% CI of about 256±23 complications in every 1,000 patients who undergo LAUP. A single patient may develop multiple complications from the procedure.
The most common complications, aside from pain, were globus sensation and dryness which were reported with an incidence of about 8.2% and 7.2% of patients, respectively. In the four studies with the longest follow-up duration with a mean of 100.5 months, these two complications were reported at a rate of 12.2% and 10.8%, respectively.19,22,29,43 This suggests that these may be long-term complications as they are reported more frequently in studies that followed patients for a longer period of time. Globus sensation and VP insufficiency are the only complications identified that had a statistically significant RR >1 based on the 95% CI, which suggests a correlation with LAUP. The absolute risk of acquiring globus sensation in the general population is 5.5% whereas post-LAUP it is 8.2%.49 For VP insufficiency, the oropharyngeal surgery patient population has an incidence of about 1.7% versus the post-LAUP risk of 3.9%.50
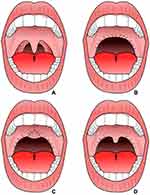
One drawback to these studies is the lack of detailed information on the extent of how these surgeries were performed. Perhaps one of the most important items for clinicians is identifying patients that may benefit from the procedure. A good candidate for the surgery will have mild OSA, large tonsils, a normal tongue, an enlarged uvula, and a posteriorly displaced soft palate.58 Figure 1 shows various surgical approaches for uvulopalatoplasty (UPPP) that correlate with approaches to LAUP in patients that are presumably good candidates for the procedure. Figure 1B shows a more radical form of surgery that was classically used in UPPP and was likely used in the older studies found in this systematic review. This large circumferential area is capable of scarring inward and causing VP stenosis or scarring outward causing VP insufficiency, hypernasal speech, and pharyngonasal regurgitation.58 Any of these structural changes are capable of causing globus sensation. As complication rates were higher with this more radical approach, the procedure progressed to a modified UPPP which involved denuding the anterior-inferior portion of the soft palate and sparing the uvula by suturing it to the soft palate as shown in Figure 1C.58 This modified approach limited the structural change caused by scarring by creating a soft tissue barrier at the midline. A newer proposed approach is a tissue-sparing approach as seen in Figure 1D which involves a bilateral tonsillectomy and plication of the anterior and posterior tonsillar pillars.58 By suturing the palatoglossus muscles to the palatopharyngeus muscles, this procedure reduces the risk of surgical complications by limiting the extent of tissue retraction from scarring. More information is needed about the complications related to specific surgical techniques and approaches; however, we recommend this tissue-sparing approach that spares the medial portion and is either performed on post-tonsillectomy patients or with a concurrent bilateral tonsillectomy, whether it be for a UPPP or LAUP, in order to reduce the risk of long-term complications to patients.
Although the RRs of the various other complications are not statistically significant, it is worth noting that all of the complications reported were likely the outcome of the surgery given the time frame of follow-up for the procedure being less than an average of 16.1 months and median of 6 months. This means that the mean number of complications represented in this review should reflect outcomes of the surgery more closely than health concerns within the general or oropharyngeal surgery populations.
Pain is the most common side effect of the surgery; however, it is underreported in the literature likely because it is an expected outcome. Patients should be counseled on the potential for pain to last up to 2 weeks based on the available data. More information is needed to better quantify and understand the expected level of pain from the procedure and the need for narcotics. Based on the short duration of narcotic usage lasting between 3 and 7 days in the two studies that reported on pain management, minimal narcotics may be required to allow patients to recover comfortably.
None of the 42 studies reported complications of wound dehiscence or VP fistula formation which are complications that have been associated with the UPPP in previous studies.34,39,59 This is one difference that may be further explored to compare differences in complication rates between UPPP and LAUP. While several studies reported 0 complications, others reported as many complications as patients. This may be due to provider skill at performing the procedure, differences in techniques for identifying complications, and differences in thresholds for reporting information. The presence of any of these differences between studies will likely lead to an underestimation of the overall number of complications. Given that complications are unwanted, a reporting bias within various papers may also result in a significant underreporting of complications.
This systematic review shows that LAUP has a notable volume of complications even though it likely underestimates the actual number. The effectiveness of the procedure has been brought into question after a meta-analysis revealed a minimal change in the LSAT and the AHI increased in a large subset of patients.5 Complications are not uncommon and may be expected to occur in a quarter of patients who undergo the procedure. For providers who continue to use LAUP as a means of treating patients, additional reporting of complications, including the timing and duration of those complications would greatly improve future risk-benefit analysis. Identifying those complications that are persistent will improve patient safety and satisfaction and reduce morbidity by limiting a procedure where risks may outweigh benefits. Additionally, a lack of information on techniques or extent of surgery associated with complications may reveal an opportunity to improve the procedure itself. For those who continue to perform LAUP, performing the procedure in a manner that reduces risk as well as reporting this information with regards to how it relates to complications will allow providers to educate other providers on how to perform the procedure in a manner to reduce complications and to appropriately identify a patient population that may be at a reduced risk of complications.
Conclusion
LAUP has been shown to have a large number of complications in patients undergoing treatment for sleep-disordered breathing. In this systematic review, there were an average of 256±23 complications per 1,000 procedures performed. The most common complications reported were globus and dryness and there were no reported cases of dehiscence or VP fistula formation which are reported in UPPP literature. Though dryness and globus were reported more often in studies with longer follow-up, there is limited information on transience or persistence of any of the reported complications. Globus and VP insufficiency are the only complications assessed with a statistically significant RR compared to the general or oropharyngeal surgery populations. It is important to remember that the duration of follow-up in each study strongly suggests that these complications were the result of the procedure, and the numbers presented should resemble the expected complications from the procedure.
Based on the findings of this systematic review, we recommend that LAUP be performed with caution using the tissue-sparing approach or avoided altogether, given the potential for complications identified in the current literature.58 Additionally, if performed, the procedure should only be performed in patients who are clearly identified as strong candidates that will likely benefit. Providers that continue to perform LAUP should do so with a secondary goal of improving the procedure by the means of gathering more information about complications including the timing and duration of the problem, surgical technique, and extent of surgery. Collecting more information may benefit patients by allowing providers who continue to perform LAUP to better assess the risks versus benefits and identify patients who are better candidates for LAUP.
Author contributions
All authors met the criteria for authorship established by the International Committee of Medical Journal Editors. Specifically, Jeffrey Wischhusen and Macario Camacho were responsible for substantial contributions to the conception, design, analysis, drafting the work, revising the work, and reviewing of the manuscript. Uneeb Qureshi assisted with the data gathering, revising the work and reviewing of the manuscript. Additionally, all authors provided final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring the accuracy and/or integrity of the work.
Disclosure
No financial or material support was received for this research and work. Authors have no financial interests in any companies or other entities that have an interest in the information in the contribution (eg, grants, advisory boards, employment, consultancies, contracts, honoraria, royalties, expert testimony, partnerships, or stock ownership in medically related fields). The views expressed in this manuscript are those of the author(s) and do not reflect the official policy or position of the Department of the Army, Department of Defense, the Uniformed Services University of the Health Sciences or the US Government. The authors report no conflicts of interest in this work.
References
1. Kamami YV. Laser CO2 for snoring. Preliminary results. Acta Otorhinolaryngol Belg. 1990;44(4):451–456.
2. Kamami YV. Outpatient treatment of sleep apnea syndrome with CO 2 laser, LAUP: laser-assisted UPPP results on 46 patients. J Clin Laser Med Surg. 1994;12(4):215–219. doi:10.1089/clm.1994.12.215
3.
4. Verse T, Pirsig W. [Meta-analysis of laser-assisted uvulopalatopharyngoplasty. What is clinically relevant up to now?]. Laryngorhinootologie. 2000;79(5):273–284. doi:10.1055/s-2000-8805
5. Camacho M, Nesbitt NB, Lambert E, et al. Laser-Assisted uvulopalatoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2017;40:3. doi:10.1093/sleep/zsx004
6. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b2651
7. Ferguson KA, Heighway K, Ruby RR. A randomized trial of laser-assisted uvulopalatoplasty in the treatment of mild obstructive sleep apnea. Am J Respir Crit Care Med. 2003;167(1):15–19. doi:10.1164/rccm.2108050
8. Abdullah B, Othman NA, Daud MK. Outcome of Laser-Assisted Uvulopalatoplasty (LAUP) in the management of snoring in hospital Universiti Sains Malaysia (USM). Malays J Med Sci. 2008;15(2):29–32.
9. Astor FC, Hanft KL, Benson C, Amaranath A. Analysis of short-term outcome after office-based laser-assisted uvulopalatoplasty. Otolaryngol Head Neck Surg. 1998;118(4):478–480. doi:10.1177/019459989811800408
10. Belloso A, Morar P, Tahery J, Saravanan K, Nigam A, Timms MS. Randomized-controlled study comparing post-operative pain between coblation palatoplasty and laser palatoplasty. Clin Otolaryngol. 2006;31(2):138–143. doi:10.1111/j.1749-4486.2006.01174.x
11. Berger G, Stein G, Ophir D, Finkelstein Y. Is there a better way to do laser-assisted uvulopalatoplasty? Arch Otolaryngol Head Neck Surg. 2003;129(4):447–453. doi:10.1001/archotol.129.4.447
12. Carenfelt C. Laser uvulopalatoplasty in treatment of habitual snoring. Ann Otol Rhinol Laryngol. 1991;100(6):451–454. doi:10.1177/000348949110000604
13. Cheng DS, Weng JC, Yang PW, Cheng LH. Carbon dioxide laser surgery for snoring: results in 192 patients. Otolaryngol Head Neck Surg. 1998;118(4):486–489. doi:10.1177/019459989811800410
14. Chisholm E, Kotecha B. Oropharyngeal surgery for obstructive sleep apnoea in CPAP failures. Eur Arch Otorhinolaryngol. 2007;264(1):51–55. doi:10.1007/s00405-006-0139-2
15. Cincik H, Cekin E, Cetin B, Gungor A, Poyrazoglu E. Comparison of uvulopalatopharyngoplasty, laser-assisted uvulopalatoplasty and cautery-assisted uvulopalatoplasty in the treatment of primary snoring. ORL J Otorhinolaryngol Relat Spec. 2006;68(3):149–155. doi:10.1159/000091313
16. Coleman JA
17. Finkelstein Y, Stein G, Ophir D, Berger R, Berger G. Laser-assisted uvulopalatoplasty for the management of obstructive sleep apnea: myths and facts. Arch Otolaryngol Head Neck Surg. 2002;128(4):429–434. doi:10.1001/archotol.128.4.429
18. Godoy LBM, Pinto JA, Colombini N, Bogaz EA, Faller GJ. Complications in obstructive sleep apnea: analyses of 694 procedures. Sleep Med. 2009;10:S69. doi:10.1016/S1389-9457(09)70259-X
19. Goktas O, Solmaz M, Goktas G, Olze H. Long-term results in obstructive sleep apnea syndrome (OSAS) after laser-assisted uvulopalatoplasty (LAUP). PLoS One. 2014;9(6):e100211. doi:10.1371/journal.pone.0100211
20. Hanada T, Furuta S, Tateyama T, Uchizono A, Seki D, Ohyama M. Laser-assisted uvulopalatoplasty with Nd: yAGlaser for sleep disorders. Laryngoscope. 1996;106(12):1531–1533.
21. Haraldsson PO, Carenfelt C. Laser uvulopalatoplasty in local anaesthesia. A safe approach in the treatment of habitual snoring. Rhinology. 1990;28(1):65–66.
22. Iyngkaran T, Kanagalingam J, Rajeswaran R, Georgalas C, Kotecha B. Long-term outcomes of laser-assisted uvulopalatoplasty in 168 patients with snoring. J Laryngol Otol. 2006;120(11):932–938. doi:10.1017/S002221510600209X
23. Klozar J, Plzák J. Laser uvuloplasty in the therapy of primary ronchopathy. Otolaryngol Foniatrie. 2004;53(4):200–204.
24. Klozar J, Plzak J, Zabrodsky M, Betka J. Effectiveness and side effects of one-stage laser-assisted uvuloplasty in primary rhonchopathy. ORL J Otorhinolaryngol Relat Spec. 2007;69(5):316–321. doi:10.1159/000107574
25. Kotecha B, Paun S, Leong P, Croft CB. Laser Assisted Uvulopalatoplasty: an objective evaluation of the technique and results. Clin Otolaryngol Allied Sci. 1998;23(4):354–359.
26. Kyrmizakis DE, Chimona TS, Papadakis CE, et al. Laser-assisted uvulopalatoplasty for the treatment of snoring and mild obstructive sleep apnea syndrome. J Otolaryngol. 2003;32(3):174–179.
27. Larrosa F, Hernandez L, Morello A, Ballester E, Quinto L, Montserrat JM. Laser-assisted uvulopalatoplasty for snoring: does it meet the expectations? Eur Respir J. 2004;24(1):66–70.
28. Lim DJ, Kang SH, Kim BH, Kim HG. Treatment of primary snoring using radiofrequency-assisted uvulopalatoplasty. Eur Arch Otorhinolaryngol. 2007;264(7):761–767. doi:10.1007/s00405-007-0252-x
29. Lysdahl M, Haraldsson PO. Uvulopalatopharyngoplasty versus laser uvulopalatoplasty: prospective long-term follow-up of self-reported symptoms. Acta Otolaryngol. 2002;122(7):752–757.
30. Maheshwar AA, Gomez KG, Obilanade M, Evans RA. Efficacy of laser palatoplasty: four-year results. Int J Clin Pract. 2002;56(7):501–503.
31. Mickelson SA, Ahuja A. Short-term objective and long-term subjective results of laser-assisted uvulopalatoplasty for obstructive sleep apnea. Laryngoscope. 1999;109(3):362–367.
32. Negm H, Elkharbotly A. Laser-assisted uvulopalatoplasty: post operative complications (NILES, preliminary experience). J Photochem Photobiol B. 2001;62(3):153–157.
33. Neruntarat C. Laser-assisted uvulopalatoplasty: short-term and long-term results. Otolaryngol Head Neck Surg. 2001;124(1):90–93. doi:10.1067/mhn.2001.112203
34. Osman EZ, Osborne JE, Hill PD, Lee BWV, Hammad Z. Uvulopalatopharyngoplasty versus laser assisted uvulopalatoplasty for the treatment of snoring: an objective randomised clinical trial. Clin Otolaryngol Allied Sci. 2000;25(4):305–310.
35. Papadakis CE, Skoulakis CE, Nikolidakis AA, Velegrakis GA, Bizakis JG, Helidonis ES. Swiftlase inferior turbinoplasty. Am J Rhinol. 1999;13(6):479–482.
36. Pavelec V, Polenik P. Use of Er,Cr: YSGGversus standard lasers in laser assisted uvulopalatoplasty for treatment of snoring. Laryngoscope. 2006;116(8):1512–1516. doi:10.1097/01.mlg.0000227958.81725.f4
37. Pinczower EF. Globus sensation after laser-assisted uvulopalatoplasty. Am J Otolaryngol. 1998;19(2):107–108.
38. Pribitkin EA, Schutte SL, Keane WM, et al. Efficacy of laser-assisted uvulopalatoplasty in obstructive sleep apnea. Otolaryngol Head Neck Surg. 1998;119(6):643–647. doi:10.1016/S0194-5998(98)70026-9
39. Rombaux P, Hamoir M, Bertrand B, Aubert G, Liistro G, Rodenstein D. Postoperative pain and side effects after uvulopalatopharyngoplasty, laser-assisted uvulopalatoplasty, and radiofrequency tissue volume reduction in primary snoring. Laryngoscope. 2003;113(12):2169–2173. doi:10.1097/00005537-200312000-00023
40. Ryan CF, Love LL. Unpredictable results of laser assisted uvulopalatoplasty in the treatment of obstructive sleep apnoea. Thorax. 2000;55(5):399–404.
41. Scierski W, Namysłowski G, Urbaniec N, Misiołek M, Namysłowska K, Pilch J. Complication after laser assisted uvulopalatoplasty in the treatment of snoring and obstructive sleep apnea syndrome. Otolaryngol Pol. 2003;57(5):675–678.
42. Seemann RP, DiToppa JC, Holm MA, Hanson J. Does laser-assisted uvulopalatoplasty work? An objective analysis using pre- and postoperative polysomnographic studies. J Otolaryngol. 2001;30(4):212–215.
43. Sharp HR, Mitchell DB. Long-term results of laser-assisted uvulopalatoplasty for snoring. J Laryngol Otol. 2001;115(11):897–900.
44. Skatvedt O. Laser-assisted uvulopalatoplasty: description of the technique and pre- and postoperative evaluation of subjective symptoms. ORL J Otorhinolaryngol Relat Spec. 1996;58(5):243–247. doi:10.1159/000276846
45. Terris DJ, Coker JF, Thomas AJ, Chavoya M. Preliminary findings from a prospective, randomized trial of two palatal operations for sleep-disordered breathing. Otolaryngol Head Neck Surg. 2002;127(4):315–323. doi:10.1067/mhn.2002.128345
46. Troell RJ, Powell NB, Riley RW, Li KK, Guilleminault C. Comparison of postoperative pain between laser-assisted uvulopalatoplasty, uvulopalatopharyngoplasty, and radiofrequency volumetric tissue reduction of the palate. Otolaryngol Head Neck Surg. 2000;122(3):402–409. doi:10.1016/S0194-5998(00)70056-8
47. Walker RP, Grigg-Damberger MM, Gopalsami C. Uvulopala-topharyngoplasty versus laser-assisted uvulopalatoplasty for the treatment of obstructive sleep apnea. Laryngoscope. 1997;107(1):76–82.
48. Wareing M, Mitchell D. Laser-assisted uvulopalatoplasty: an assessment of a technique. J Laryngol Otol. 1996;110(3):232–236.
49.
50. Milczuk HA. Effects of oropharyngeal surgery on velopharyngeal competence. Curr Opin Otolaryngol Head Neck Surg. 2012;20(6):522–526. doi:10.1097/MOO.0b013e32835873cc
51. Khanna S, Dagum AB. A critical review of the literature and an evidence-based approach for life-threatening hemorrhage in maxillofacial surgery. Ann Plast Surg. 2012;69(4):474–478. doi:10.1097/SAP.0b013e31824a2171
52. Kubik M, Mandal R, Albergotti W, Duvvuri U, Ferris RL, Kim S. Effect of transcervical arterial ligation on the severity of postoperative hemorrhage after transoral robotic surgery. Head Neck. 2017;39(8):1510–1515. doi:10.1002/hed.24677
53. Reich W, Kriwalsky MS, Wolf HH, Schubert J. Bleeding complications after oral surgery in outpatients with compromised haemostasis: incidence and management. Oral Maxillofac Surg. 2009;13(2):73–77. doi:10.1007/s10006-009-0154-8
54. Zenga J, Suko J, Kallogjeri D, Pipkorn P, Nussenbaum B, Jackson RS. Postoperative hemorrhage and hospital revisit after transoral robotic surgery. Laryngoscope. 2017;127(10):2287–2292. doi:10.1002/lary.26626
55. Denning DW. Calling upon all public health mycologists : to accompany the country burden papers from 14 countries. Eur J Clin Microbiol Infect Dis. 2017;36(6):923–924. doi:10.1007/s10096-017-2909-8
56. Stulberg JJ, Delaney CP, Neuhauser DV, Aron DC, Fu P, Koroukian SM. Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303(24):2479–2485. doi:10.1001/jama.2010.841
57. Santos NS, Scoralick AC, Figueiredo F, de Moraes LL, Da Cunha Viana Jr.A, Mendes DL. Case report: restorative palatopharyngoplasty in velo-pharyngeal stenosis. Int Arch Otorhinolaryngol. 14th Congress of Otorhinolaryngology Foundation. Official Program Abstracts - oral presentations and posters. 2015;19 (Suppl 2 #A351).
58. Camacho M, Certal V, Modi R, Capasso R. Tissue-sparing uvulopalatopharyngoplasty for OSA: conservative, compassionate and possibly just as effective. Indian J Otolaryngol Head Neck Surg. 2019;71(1):5–6. doi:10.1007/s12070-015-0915-7
59. Walker RP, Garrity T, Gopalsami C. Early polysomnographic findings and long-term subjective results in sleep apnea patients treated with laser-assisted uvulopalatoplasty. Laryngoscope. 1999;109(9):1438–1441. doi:10.1097/00005537-199909000-00015
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.