Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Laparoscopic versus Open Inguinal Hernia Repair in Aging Patients: A Propensity Score Matching-Based Retrospective Study
Authors Xu Z, Zhao Y, Fu X, Hu W, Zhao C , Ge C, Ye H, Chen C
Received 29 May 2023
Accepted for publication 2 August 2023
Published 8 August 2023 Volume 2023:19 Pages 657—666
DOI https://doi.org/10.2147/TCRM.S423307
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Zipeng Xu,1,* Yong Zhao,2,* Xu Fu,3,* Weidong Hu,1 Chunlong Zhao,1 Chen Ge,1 Hui Ye,4,5 Chaobo Chen1,3,5
1Department of General Surgery, Xishan People’s Hospital of Wuxi City, Wuxi, 214105, People’s Republic of China; 2Department of General Surgery, Wuxi Rehabilitation Hospital, Wuxi, 214007, People’s Republic of China; 3Department of General Surgery, the Affiliated Drum Tower Hospital of Nanjing University Medical school, Nanjing, 210008, People’s Republic of China; 4Department of Anesthesiology, ZhongDa Hospital, Southeast University, Nanjing, 210009, People’s Republic of China; 5Department of Immunology, Ophthalmology & ORL, Complutense University School of Medicine, Madrid, 28040, Spain
*These authors contributed equally to this work
Correspondence: Chaobo Chen; Hui Ye, Email [email protected]; [email protected]
Objective: Although laparoscopic repair has been widely carried out and promoted due to its minimally invasive advantages, open surgery is still popular compared to elderly patients. This study aims to compare the outcomes of laparoscopic (LIHR) vs open repair of inguinal hernias (OIHR) in elderly patients.
Methods: A retrospective analysis of the database was performed to identify elderly patients, from January 2021 through December 2022, who underwent surgery for an inguinal hernia. After a 1:1 propensity score matching (PSM) with a caliper of 0.1 was conducted to balance potential bias, binary logistic regressions were used for categorical and continuous outcomes.
Results: After PSM, 78 pairs of elderly patients were enrolled in this study, and there were no significant differences in baseline between LIHR and OIHR groups. Compared to OIHR, univariable and multivariable logistic regression analysis showed that LIHR was independently affected for reducing intraoperative hemorrhage (OR = 0.06, 95% CI: 0.02– 0.18, P < 0.001) and shortening postoperative hospitalization time (OR = 0.29, 95% CI: 0.15– 0.57, P < 0.001) in elderly patients. Furthermore, LIHR (OR = 0.28, 95% CI: 0.14– 0.57, P < 0.001) and age (OR = 0.89, 95% CI: 0.82– 0.96, P = 0.002) were independent affecting factors for relieving postoperative pain. Meanwhile, no obvious differences were detected in postoperative complications [LIHR 7.7% (6/78) vs OIHR 14.1% (11/78), P = 0.199].
Conclusion: LIHR was closely associated with reducing intraoperative hemorrhage and shortening postoperative hospitalization time. Whilst LIHR and age were independently affecting factors for relieving postoperative pain.
Keywords: inguinal hernia, propensity score matching, elderly patient, laparoscopy, retrospective study
Introduction
Primary inguinal hernia is a common surgical disease arising from a defect in the abdominal wall of the inguinal region. Approximately 20 million patients worldwide undergo surgical treatment every year.1 From 1990 to 2019, India (2.45 million), China (1.95 million), and Brazil (0.71 million) accounted for more than one-third (39%) of the incident hernias worldwide while still increasing in China.2 Surgical treatment of inguinal hernia is the most effective method.3 The more common surgical method is Lichtenstein’s tension-free repair (LTFR). However, with the development of minimally invasive surgery, the application of minimally invasive technology has benefited much more patients. For example, the emergence of transabdominal preperitoneal prosthetic (TAPP), totally extraperitoneal repair (TEP), and the robotic TAPP (rTAPP) has diversified the minimally invasive surgical treatment of inguinal hernia.4,5
Laparoscopic inguinal hernia repair (LIHR) and open inguinal hernia repair (OIHR) procedures are often compared during the 20 years.4,6–9 Importantly, with the advantages of minimally invasive technology, such as reduced wound complications, less recurrence rate, and faster recovery, which is highly favored by not only surgeons but also patients.10 However, no prospective studies have reported the correlation between age, surgical methods (LIHR and OIHR), and surgical outcomes. A retrospective study found that in the treatment of inguinal hernia repair in elderly patients, LIHR also showed similar advantages.11 Likewise, another study suggested that LIHR was safe and feasible and was also considered more advantageous for the intraoperative detection of contralateral hernia in elderly patients.12
In fact, the decision to use an open or laparoscopic approach to non-emergency inguinal hernia surgery is multifactorial, including the patient’s individualized medical history and anatomical structure, surgeon preferences, and resource availability at the patient’s attending hospital.1 For example, patients with coagulopathy, extensive preperitoneal adhesions, and local extraperitoneal hematoma may force surgeons to adopt open surgery.13 Similarly, in elderly patients, because of poor cardiopulmonary function, anesthetic allergy, or other reasons for intolerance of general anesthesia, LIHR cannot be performed and OIHR can only be performed under regional anesthesia.12,14 These matters were also reviewed by Perez15 who focused on which patients should be repaired, the optimal timing of surgery, what is the best anesthesia, and how the repair should be performed in the elderly patients (age ≥65 years).
Although, many randomized controlled trials (RCTs) have been published in the early stage,16–18 but they are fewer related research reports based on propensity score matching (PSM)-paired in elderly patients.19,20 At present, China’s aging process is accelerating, and the number of elderly patients increasing year by year has put unprecedented pressure on the current medical system. How to better diagnose and treat elderly patients with inguinal hernia has put forward new requirements for medical workers.21,22 Therefore, this research report focused on the single-center elderly patients with an inguinal hernia who received LIHR or OIHR treatment, compared the outcomes of these two groups based on PSM, and shared the experience in diagnosing and treatment of elderly inguinal hernia patients.
Method
Study Design and Patients
This retrospective cohort study included patients with inguinal hernia admitted at the Xishan People’s Hospital of Wuxi City between Jan 2021 and Dec 2022.
Inclusion criteria: (1) underwent either LIHR or OIHR, (2) aged elder than 65, (3) unilateral inguinal hernias.
Exclusion criteria: (1) undergoing surgery were converted from LIHR to OIHR, (2) with complexed hernias (such as, obstructive or/and strangulated hernias), (3) uncorrectable coagulation disorders, (4) pregnant women, (5) recurrent inguinal hernia. The study complied with the Declaration of Helsinki and was approved by the Ethics Committee of the Xishan People’s Hospital of Wuxi City (No. xs2023ky002). The requirement for informed consent was waived.
Surgical Technique
All surgeries were completed by the same surgical team. Surgical procedures for LIHR and OIHR were performed as previously described.23–25 In this study, we performed LIHR via transabdominal preperitoneal procedure (TAPP), and OIHR adopted the approach of Lichtenstein’s tension-free repair (LTFR).
Data Collection
Data collection and follow-up were carried out for both LIHR and OIHR groups, including: Age, Hernia sac diameter, Gender (M/F), Hypertension, Diabetes, Type of hernia (Indirect/direct hernia), ASA (American Society of Anesthesiologists) Grade,26 Postoperative 12-hour Pain score, Operation time, Intraoperative hemorrhage, Postoperative hospitalization, and Postoperative complications. Patients in both groups were regularly followed up for at least 3 months via telephone or outpatient clinic.
Statistical Analysis
SPSS 22.0 (IBM, Armonk, NY, USA) was used for data analysis. The continuous data were expressed as means ± standard deviations and analyzed via Student’s t-test. Categorical data were presented as frequencies and scores and were analyzed using Chi-squared test or Fisher’s exact test. Non-normally distributed variables were presented as medians with interquartile ranges (IQR) and were tested by using the Mann–Whitney U-test. Propensity score matching (PSM) was performed to correct patients´ baseline date. In the PSM, one‐to‐one matching between the groups was performed using the nearest neighbor matching method with a caliper width of 0.1. Binary logistic regressions were used for categorical and continuous outcomes, respectively. Meanwhile, postoperative 12-hour pain score was classified into mild pain and moderate pain based on median numerical rating scale (NRS) score. P-value <0.05 was considered statistically significant.
Results
Characteristics of the Patients
A total of 319 elderly patients (more than 65-year) with primary unilateral inguinal hernias diagnosed as inguinal hernia at Xishan people’s Hospital of Wuxi City was initially identified. Among these patients, 7 were excluded due to anesthesia intolerance, 39 were excluded due to recurrent hernia combined with second surgery treatment, and 6 cases of abdominal wall hernia were also excluded. A total of 81 patients were treated with LIHR; 3 were excluded because they converted from LIHR to OIHR. Finally, 264 patients, 78 treated with LIHR and 186 treated with OIHR, were included in this study (Figure 1). Significant differences were observed in age between OIHR and LIHR groups (P < 0.001, Table 1), also combined with obvious differences in the type of hernia, especially high-rate indirect hernia (P < 0.05, Table 1).
 |
Table 1 Comparison of Clinical Baseline Data Between LIHR and OIHR Group Before Propensity Score Matching |
 |
Figure 1 Detailed surgery flow diagram. |
Therefore, a 1:1 PSM with a caliper 0.1 was conducted to balance potential bias, based on Age, Hernia sac diameter, Gender, Hypertension, Diabetes, Type of hernia, and ASA Grade, and then 78 comparable pairs of patients from LIHR and OIHR groups were matched (Figure 1). There were no significant differences in Age, Hernia sac diameter, Gender (M/F), Hypertension, Diabetes, Type of hernia and ASA Grade, between LIHR and OIHR groups (P > 0.05, Table 2).
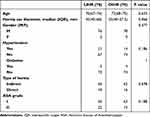 |
Table 2 Comparison of Clinical Baseline Data Between LIHR and OIHR Group After Propensity Score Matching |
Comparisons of Intraoperative and Postoperative Outcomes
The operation time was similar, compared LIHR group to OIHR group, and no differences was observed [LIHR 80 (70–90) vs OIHR 80 (61.25–93.75), P = 0.997]. However, compared to OIHR group, LIHR group performed less intraoperative hemorrhage [LIHR 10 (10–10) mL vs OIHR 20 (10–20) mL, P < 0.001], and less postoperative pain (12 hours) [LIHR 2 (1–3) vs OIHR 3 (2–4), P < 0.001], combined with shorter postoperative hospitalization [LIHR 2 (2–4) Day vs OIHR 4 (3–5) Day, P < 0.001] (Table 3).
 |
Table 3 Comparison of Intraoperative and Postoperative Outcomes Between LIHR and OIHR Group |
While there’s no significant differences in the postoperative complications of uroschesis, hematoma and incision infection compare LIHR group with OIHR group (P > 0.05). Moreover, no obvious differences were detected in the total postoperative complications between these two groups of patients [LIHR 7.7% (6/78) vs OIHR 14.1% (11/78), P = 0.199] (Table 3).
LIHR Associated with Reducing Intraoperative Hemorrhage
In order to explore the factors affecting intraoperative hemorrhage, we performed a binary logistic regression analysis. Univariable logistic regression analysis showed that LIHR was positively related to reduce intraoperative hemorrhage (OR = 0.06, 95% CI: 0.02–0.17, P < 0.001), whilst elderly patients were more prone to bleeding (OR = 1.09, 95% CI: 1.01–1.18, P = 0.029). Multivariable logistic regression analysis conducted to identify independent predictors affecting intraoperative hemorrhage suggested LIHR as an independent factor (OR = 0.06, 95% CI:0.02–0.18, P < 0.001) for reducing intraoperative hemorrhage (Table 4).
 |
Table 4 Regression Analysis of Intraoperative Hemorrhage |
LIHR Associated with Relieving Postoperative Pain
Inguinal hernia surgery is relatively less traumatic. Therefore, we chose the postoperative 12-hour pain score for statistical analysis. As shown in Table 5, univariable and multivariate logistic regression analysis indicated that LIHR (OR = 0.28, 95% CI: 0.14–0.57, P < 0.001) and age (OR = 0.89, 95% CI: 0.82–0.96, P = 0.002) were independent risk factors for relieving postoperative 12-hour pain.
 |
Table 5 Regression Analysis of Postoperative 12-Hour Pain Scores |
Potential Influence Factors Related to Postoperative Hospitalization Time
Univariable logistic regression analysis suggested that LIHR was closely related to postoperative hospitalization time (OR = 0.31, 95CI%: 0.16–0.6, P < 0.001). Although multivariate logistic regression analysis indicated that diabetes would prolong postoperative hospitalization time (OR = 6.12, 95% CI: 1.16–32.28, P = 0.033), LIHR was still an independent factor for shortening the postoperative hospitalization time (OR = 0.29, 95% CI: 0.15 −0.57, P < 0.001) (Table 6).
 |
Table 6 Regression Analysis of Postoperative Hospitalization Time |
Discussion
Inguinal hernia is a common defect in the abdominal wall, which may occur in all ages, from children to the elderly. Hernia repair surgery is the most common treatment procedure.27 As reported, China has the second highest incidence rate and prevalence in the world, and the age-standardized incidence rate (ASIR) is on the rise.2 Inguinal hernia repair represents a huge burden on the local healthcare system in a country with a large population. Due to the aging of the global population, the incidence of inguinal hernia is also expected to be a rise in the next few years.28 Therefore, what we concerned is that China may become the country with the heaviest burden of inguinal hernia in the world in the near future,15 and the need for hernia management, especially in elderly patients, has become an important socioeconomic issue that may affect the public healthcare system in China.
Herein, based on the diagnosis and treatment situation in our medical center, after PSM, we analyzed and compared the outcomes of 78 pairs of patients who received LIHR or OIHR treatment and shared the experience of inguinal hernia treatment for elderly patients in our medical center. There was no mortality in both groups. As described, compared to OIHR (LTFR), LIHR has the advantages of lower incidence of hematoma, lower rates of seroma, less postoperative pain, faster recovery and less wound infection rate,4,29 which are also applicable to elderly patients.11,12 After PSM, there were no significant differences in baseline between LIHR and OIHR groups (Table 1 and Table 2).
Relatively, an update RCT network meta-analysis showed that minimally invasive surgical repair of inguinal hernia has many advantages, but the operation time is relatively long, and no significant difference was found between TAPP and TEP.4 However, the operation time was similar in this study, there’s no significant differences between LIHR and OIHR groups (Table 3). Previous studies have shown that surgeons need to go through a special learning curve from basic operations to proficiency in mastering LIHR techniques.30 Other medical centers have reported a range of 50 to 250 cases,31 while our center recently reported 54 cases as well.9 All patients in this study were completed by the same group of senior and professional surgeons. Perhaps, the LIHR approach could be performed easier by exerted surgeons after overcoming the laparoscopic technical learning curve, thereby significantly shortening the operative time, which in this study was similar to that of the OIHR group. Additionally, there was no recurrence of hernias after short-term following-up in this study.
In recent years, with the acceleration of China’s aging process, many elderly patients need oral antiplatelet drugs because of cardiac dysfunction, coronary atherosclerosis, cardiovascular stent surgery, etc., which may increase the risk of postoperative bleeding, wound hematoma, and/or other postoperative complications when undergone inguinal hernia surgery. According to the guideline recommendation, before undergoing inguinal hernia repair surgery, patients discontinue warfarin 5 days before surgery and take anticoagulants orally 2 days before surgery (if renal function normal). Non-aspirin antiplatelet drugs were withheld for 5 to 7 days before surgery after the risk of postoperative bleeding had decreased, while warfarin was resumed within 24 hours of surgery.32 Previous studies have shown that patients who receive antithrombotic therapy or with coagulation disorders have a 4-fold higher risk of secondary bleeding after inguinal hernia surgery, but LIHR surgery appears to reduce the risk of bleeding complications and complication-related reoperations.33 In another cohort study, non-aspirin antiplatelet therapy or anticoagulant therapy was found to be an independent predictor of OIHR; but LIHR approach was safe for this subset of elderly patients, with no significant differences in hemorrhage and cardiovascular complications.13 In this study, those elderly patients who were treated with antiplatelet or anticoagulant drugs before surgery would be adjusted according to the time of surgery and anesthesia. Indeed, drugs such as aspirin and warfarin were stopped for three days preoperatively but switched to low-molecular-weight heparin bridging therapy. After PSM, there was also no significant difference in the postoperative complication of hematoma between these two groups in our study. Moreover, LIHR was independently affected for reducing intraoperative hemorrhage and shortening postoperative hospitalization time in elderly patients.
Actually, numerous studies have shown the potential advantages of LIHR, such as faster recovery, reduced pain, and so on.30,34–37 Specifically, LIHR and age were independent risk factors for relieving postoperative pain compared to OIHR, as presented in our study. In fact, patients also need to undergo general anesthesia if performed with LIHR, which may importantly affect the postoperative pain of the patient. However, more data from the real world need to be collected for clinical validation. Unlike LIHR, OIHR was usually performed under local or spinal anesthesia (especially for those who cannot tolerate general anesthesia), and occasionally also under general anesthesia. Therefore, there may be a bias in the parameters obtained for inguinal hernia repair under different anesthesia states. However, after PSM, the parameter bias of the two groups of patients could be obviously reduced, making the results of this study more convincing. Although no cardiovascular-related postoperative complications were found in this study. Particularly, a previous study has shown that regional anesthesia in elderly patients (65 years and older) is closely related to more frequent complications of cardiac and thromboembolism.1 This may be related to the effective evaluation of cardiac function in elderly patients before operation (both LIHR and OIHR), and the use of preoperative medication to improve cardiac function in elderly patients with poor cardiac function before surgery.
In contrast, the incidence of diabetes in the elderly is relatively high.38 Therefore, we also analyzed the impact of diabetes on the surgical treatment of elderly patients with inguinal hernia. Although multivariate logistic regression analysis indicated that diabetes would prolong postoperative hospitalization time, LIHR was still independently affected for shortening postoperative hospitalization time.
Although based on the PSM-paired analysis, we have known the advantages of LIHR compared with OIHR, as well as the impact on elderly patients with inguinal hernia. However, there are also some limitations in this study. The data from our single medical center is relatively limited, and the heterogeneity of patients is also limited to residents from Wuxi and/or surrounding areas. Although the sample size was presented as not so small, it is still a larger distance compared to the overall Chinese resident base. Multi-center cooperation may make up for this deficiency. Moreover, we only conducted short-term follow-ups and lacked long-term follow-up data, including long-term recurrence, incisional hernia, scar contracture, etc., which requires a more rigorous research plan to obtain better reports.
Conclusions
With the global aging process today, the number of elderly patients with inguinal hernias in China has been on the rise, and the healthcare care system for elderly patients requires more attention. The LIHR approach has the advantages of reducing intraoperative bleeding, shortening postoperative hospital stay, and independently affecting in relieving postoperative pain in elderly inguinal hernia patients. This treatment approach may better care for and benefit more elderly patients.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author (Chaobo Chen) upon reasonable request. For any queries, kindly contact [email protected].
Ethics Approval and Consent to Participate
The need for written informed consent was waived by the Xishan People’s Hospital of Wuxi City Ethics Committee (No. xs2023ky002). This article was a retrospective study, there are no commercial interests involved, patient parental consent to review their medical records was not required by the ethics Committee of Xishan People’s Hospital of Wuxi City. This study strictly kept the patients’ information confidential. The study complied with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the scientific research projects of the Wuxi Municipal Health Commission (Project, No. M202160).
Disclosure
The authors report no conflicts of interest in this work.
References
1. HerniaSurge G. International guidelines for groin hernia management. Hernia. 2018;22(1):1–165.
2. Ma Q, Jing W, Liu X, Liu J, Liu M, Chen J. The global, regional, and national burden and its trends of inguinal, femoral, and abdominal hernia from 1990 to 2019: findings from the 2019 Global Burden of Disease Study - a cross-sectional study. Int J Surg. 2023;109(3):333–342. doi:10.1097/JS9.0000000000000217
3. Hammoud M, Gerken J. Inguinal Hernia. In: StatPearls. Treasure Island (FL): StatPearls; 2023.
4. Aiolfi A, Cavalli M, Ferraro SD, et al. Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg. 2021;274(6):954–961. doi:10.1097/SLA.0000000000004735
5. Reinhorn M, Fullington N, Agarwal D, et al. Posterior mesh inguinal hernia repairs: a propensity score matched analysis of laparoscopic and robotic versus open approaches. Hernia. 2023;27(1):93–104. doi:10.1007/s10029-022-02680-0
6. Anadol ZA, Ersoy E, Taneri F, Tekin E. Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus Open Lichtenstein technique. J Laparoendosc Adv Surg Tech A. 2004;14(3):159–163. doi:10.1089/1092642041255414
7. Howard R, Ehlers A, Delaney L, et al. Incidence and trends of decision regret following elective hernia repair. Surg Endosc. 2022;36(9):6609–6616. doi:10.1007/s00464-021-08766-7
8. Sehat AJ, Oliver JB, Yu Y, Kunac A, Anjaria DJ. Increasing volume but declining resident autonomy in laparoscopic inguinal hernia repair: an inverse relationship. Surg Endosc. 2023;37(4):3119–3126. doi:10.1007/s00464-022-09476-4
9. Zhao Y, Xu Z, Wang T, et al. The impact of laparoscopic versus open inguinal hernia repair for inguinal hernia treatment: a retrospective cohort study. Health Sci Rep. 2023;6(4):e1194. doi:10.1002/hsr2.1194
10. Aiolfi A, Cavalli M, Micheletto G, et al. Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia. 2019;23(3):473–484. doi:10.1007/s10029-019-01964-2
11. Pang NQ, Ng CSY, Wong CJH. Laparoscopic versus open groin hernia repair in older adults: a systematic review and meta-analysis. ANZ J Surg. 2022;92(10):2457–2463. doi:10.1111/ans.18032
12. Kohga A, Kawabe A, Makino A, et al. Safety and feasibility of laparoscopic transabdominal preperitoneal hernia repair for octo- and nonagenarians. J Laparoendosc Adv Surg Tech A. 2022;32(8):848–853. doi:10.1089/lap.2021.0616
13. Balch JA, Neal D, Crippen C, et al. Safety of laparoscopic inguinal hernia repair in the setting of antithrombotic therapy. Surg Endosc. 2022;36(12):9011–9018. doi:10.1007/s00464-022-09360-1
14. Ryu T, Song SY. Perioperative management of left ventricular diastolic dysfunction and heart failure: an anesthesiologist’s perspective. Korean J Anesthesiol. 2017;70(1):3–12. doi:10.4097/kjae.2017.70.1.3
15. Perez AJ, Campbell S. Inguinal hernia repair in older persons. J Am Med Dir Assoc. 2022;23(4):563–567. doi:10.1016/j.jamda.2022.02.008
16. Bobo Z, Nan W, Qin Q, Tao W, Jianguo L, Xianli H. Meta-analysis of randomized controlled trials comparing Lichtenstein and totally extraperitoneal laparoscopic hernioplasty in treatment of inguinal hernias. J Surg Res. 2014;192(2):409–420. doi:10.1016/j.jss.2014.05.082
17. Gavriilidis P, Davies RJ, Wheeler J, de’Angelis N, Di Saverio S. Total extraperitoneal endoscopic hernioplasty (TEP) versus Lichtenstein hernioplasty: a systematic review by updated traditional and cumulative meta-analysis of randomised-controlled trials. Hernia. 2019;23(6):1093–1103. doi:10.1007/s10029-019-02049-w
18. Chen LS, Chen WC, Kang YN, Wu CC, Tsai LW, Liu MZ. Effects of transabdominal preperitoneal and totally extraperitoneal inguinal hernia repair: an update systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2019;33(2):418–428. doi:10.1007/s00464-018-6314-x
19. Philipp M, Leuchter M, Lorenz R, Grambow E, Schafmayer C, Wiessner R. Quality of life after desarda technique for inguinal hernia repair-a comparative retrospective multicenter study of 120 patients. J Clin Med. 2023;12(3):1001. doi:10.3390/jcm12031001
20. Aly S, de Geus SWL, Carter CO, Hess DT, Tseng JF, Pernar LIM. Laparoscopic versus open ventral hernia repair in the elderly: a propensity score-matched analysis. Hernia. 2021;25(3):673–677. doi:10.1007/s10029-020-02243-1
21. Li L, Du T, Zeng S. The different classification of hospitals impact on medical outcomes of patients in China. Front Public Health. 2022;10:855323. doi:10.3389/fpubh.2022.855323
22. Lomanto D, Cheah WK, Faylona JM, et al. Inguinal hernia repair: toward Asian guidelines. Asian J Endosc Surg. 2015;8(1):16–23. doi:10.1111/ases.12141
23. Fafaj A, Lo Menzo E, Alaedeen D, et al. Effect of intraoperative urinary catheter use on postoperative urinary retention after laparoscopic inguinal hernia repair: a randomized clinical trial. JAMA Surg. 2022;157:667. doi:10.1001/jamasurg.2022.2205
24. Fernandez-Alberti J, Iriarte F, Croceri RE, Medina P, Porto EA, Pirchi DE. Laparoscopic treatment (reTAPP) for recurrence after laparoscopic inguinal hernia repair. Hernia. 2021;25(5):1301–1307. doi:10.1007/s10029-020-02357-6
25. Sofi J, Nazir F, Kar I, Qayum K. Comparison between TAPP & Lichtenstein techniques for inguinal hernia repair: a retrospective cohort study. Ann Med Surg. 2021;72:103054. doi:10.1016/j.amsu.2021.103054
26. Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth. 2011;55(2):111–115. doi:10.4103/0019-5049.79879
27. Itani KMF, Fitzgibbons R. Approach to Groin Hernias. JAMA Surg. 2019;154(6):551–552. doi:10.1001/jamasurg.2018.5564
28. Williams ML, Hutchinson AG, Oh DD, Young CJ. Trends in Australian inguinal hernia repair rates: a 15-year population study. ANZ J Surg. 2020;90(11):2242–2247. doi:10.1111/ans.16192
29. Dedemadi G, Sgourakis G, Radtke A, et al. Laparoscopic versus open mesh repair for recurrent inguinal hernia: a meta-analysis of outcomes. Am J Surg. 2010;200(2):291–297. doi:10.1016/j.amjsurg.2009.12.009
30. Zhu X, Liu Z, Shen J, Liu J, Tang R. Comparison of open and laparoscopic inguinal-hernia repair in octogenarians. Asian J Surg. 2023;46(2):738–741. doi:10.1016/j.asjsur.2022.06.149
31. Zhu X, Liu Z, Shen J, Liu J, Tang R. Comparison of open and laparoscopic inguinal hernia repair in octogenarians. Asian J Surg. 2022;46(2):738–741.
32. Hornor MA, Duane TM, Ehlers AP, et al. American college of surgeons’ guidelines for the perioperative management of antithrombotic medication. J Am Coll Surg. 2018;227(5):521–536 e521. doi:10.1016/j.jamcollsurg.2018.08.183
33. Kockerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D. Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the herniamed registry. Surg Endosc. 2016;30(5):2073–2081. doi:10.1007/s00464-015-4456-7
34. Pan Z, Zhang M, Wang L. Efficacy of laparoscopic totally extraperitoneal repair for inguinal hernia. Dis Markers. 2022;2022:2970257. doi:10.1155/2022/2970257
35. Amato G, Agrusa A, Calo PG, et al. Fixation free laparoscopic obliteration of inguinal hernia defects with the 3D dynamic responsive scaffold ProFlor. Sci Rep. 2022;12(1):18971. doi:10.1038/s41598-022-23128-6
36. Wu G, Shi D, Chen M, et al. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair with preperitoneal closed-suction drainage reduced postoperative complications. BMC Surg. 2023;23(1):14. doi:10.1186/s12893-022-01900-9
37. Chen L, Liu S, Cao Y, Yan L, Shen Y. Rectus sheath block versus local anesthetic infiltration in pediatric laparoscopic inguinal hernia repair: a randomized controlled trial. Int J Surg. 2023;109(4):716–722. doi:10.1097/JS9.0000000000000265
38. Conrad N, Verbeke G, Molenberghs G, et al. Autoimmune diseases and cardiovascular risk: a population-based study on 19 autoimmune diseases and 12 cardiovascular diseases in 22 million individuals in the UK. Lancet. 2022;400(10354):733–743. doi:10.1016/S0140-6736(22)01349-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
