Back to Journals » Open Access Emergency Medicine » Volume 14
Lack of Thoracentesis Competencies and Training in Danish Emergency Departments: A Danish Nationwide Study
Authors Langsted ST, Lauridsen KG, Weile JB , Skaarup SH, Kirkegaard H , Løfgren B
Received 2 August 2022
Accepted for publication 20 October 2022
Published 15 November 2022 Volume 2022:14 Pages 609—614
DOI https://doi.org/10.2147/OAEM.S384608
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Sandra Thun Langsted,1– 3 Kasper Glerup Lauridsen,2– 4 Jesper Bo Weile,2,3,5 Søren Helbo Skaarup,6 Hans Kirkegaard,2,3 Bo Løfgren1– 4
1Department of Emergency Medicine, Randers Regional Hospital, Randers, Denmark; 2Research Center for Emergency Medicine, Aarhus University Hospital, Aarhus, Denmark; 3Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 4Department of Internal Medicine, Randers Regional Hospital, Randers, Denmark; 5Department of Emergency Medicine, Horsens Regional Hospital, Horsens, Denmark; 6Department of Respiratory Medicine, Aarhus University Hospital, Aarhus, Denmark
Correspondence: Bo Løfgren, Department of Emergency Medicine, Randers Regional Hospital, Skovlyvej 15, Randers, NE, 8930, Denmark, Tel +457842 0000, Email [email protected]
Background: Dyspnea caused by pleural effusion is a common reason for admission to the emergency department (ED). In such cases, thoracentesis performed in the ED may allow for swift symptom relief, diagnostics, and early patient discharge. However, the competence level of thoracentesis and training in the ED are currently unclear. This study aimed to describe the current competencies and training in thoracentesis in Danish EDs.
Methods: We performed a nationwide cross-sectional study in Denmark. A questionnaire was distributed to all EDs in March 2022 including questions on competencies and thoracentesis training methods. Descriptive statistics were used.
Results: In total, 21 EDs replied (response rate 100%) between March and May 2022. Overall, 50% of consultant and 77% of physicians in emergency medicine specialist training were unable to perform thoracentesis independently. Only 2 of 21 EDs (10%) had a formalized training program. In these 2 EDs, there were no requirements of maintaining these competences. Informal training was reported by 14 out 21 (66%) EDs and consisted of ad-hoc bedside procedural demonstration and/or guidance. Among the 19 EDs without formalized training, 9 (47%) had no intention of establishing a formalized training program.
Conclusion: We found a major lack of thoracentesis competencies in Danish EDs among both consultant and physicians in emergency medicine specialist training. Moreover, the vast majority of EDs had no formalized thoracentesis training program.
Keywords: thoracenteses, training, competencies, emergency medicine
Introduction
Dyspnea is a common reason for admission to the emergency department (ED) and may be caused by pleural effusion.1,2 Pleural effusion develops due to multiple causes and is most frequently associated with congestive heart failure, pleural malignancy or pleural infection.
Drainage of pleural effusion ie, thoracentesis will typically relieve symptoms. Large effusion may contribute to respiratory failure especially if combined with other conditions that impede lung function such as pulmonary edema or infection. Thoracentesis may in these cases be life-saving. Furthermore, thoracentesis serves diagnostic purposes as biochemical, microbiological, and pathological analysis of the effusion are essential in process of establishing the etiology of the effusion.3–5
If pleural effusion is identified in patients who are admitted to the emergency department, thoracentesis may be performed by an emergency medicine physician or the patient may be referred to the radiology department for thoracentesis. Performing thoracentesis in the ED hold a number of possible advantages such as avoiding the need for in-hospital patient transport, reducing treatment delay, and relieving the work load on radiology department which all will improve emergency department efficiency and possible reduce overcrowding.
Consequently, thoracentesis was introduced as a mandatory skill in the 2018 core curriculum for emergency medicine in Denmark.6 However, no national, or international, standards exist for teaching thoracentesis in emergency medicine and there is a lack in knowledge on how many emergency physicians perform thoracentesis, their level of education, organization of training and evaluation of competency.
This study aims to describe the current thoracentesis competence level and thoracentesis training in Danish Emergency Departments.
Methods
Study Design
A nationwide cross-sectional study was performed including all EDs in Denmark. The EDs were identified from the Danish Health Authority.7 A structured questionnaire was emailed to key members in the EDs ie, department chairs or the consultant being head of staff education in the ED.
Questionnaire
The questionnaire inquired the following information: 1) number of physicians (consultants in emergency medicine (combined consultant in emergency medicine and consultant in other specialty working in the ED), physicians in emergency medicine specialist training (combined senior house officer and specialist registrar), house officer or others; definitions are similar to those previously used by Lauridsen et see Box 1)8 employed in the ED and the number of these who were able to perform thoracentesis, 2) whether a formalized training program (defined as structured and scheduled training for physicians in the department) was implemented and/or whether informal training (eg bedside thoracentesis) was used, 3) whether a specific number of supervised procedures were required before a physician was allowed to perform the thoracocentesis independently, and 4) if they had guidelines for thoracentesis procedures.
 |
Box 1 Definition of Medical Titles |
If the respondents replied that they had a formalized training program, additional questions regarding the nature of the training program were inquired: 1) what the training consisted of, 2) the number of hours allocated to training, 3) where the training took place, 4) how theoretical knowledge was being disseminated, 5) what format was used for training, 6) whether any formal assessment of skills was conducted, and 7) any requirements to maintenance of skills. Thoracentesis was defined as the use of a trocar pigtail catheter. For the full questionnaire please see Supplementary Data.
The questionnaire was developed by the authors. The questionnaire was subsequently reviewed for face-validity by 4 emergency physicians to identify any obscurities before distribution of the questionnaire.
Data Collection
The questionnaire was distributed on 8th of marts 2022 by e-mail. After 1 week, 2 weeks, 4 weeks, 6 weeks, and 9 weeks a reminder was sent to the respondents to complete the questionnaire. Study data were collected and managed using REDCap electronic data capture tools hosted at Aarhus University.9,10
In addition to the questionnaire, the EDs who reported to have no formal or informal thoracentesis training, nor had any intentions of establishing training were contacted and inquired about the reasons for this.
Ethics
According to Danish law, no approval from the Danish National Committee on Biomedical Research Ethics was required (Danish Act on Research Ethics, Review of Health Research Projects, Act number 593 of 14 July 2011 section 14). All data on respondents were handled according to European Union general data protection regulation. All respondents gave informed consent to participating when completing the questionnaire.
Data Analysis
Categorical data are presented as number (percentage). Data were analyzed using STATA version 14.1 (StataCorp LP, College Station, TX, USA). As this is a descriptive study, no statistical tests were conducted.
Results
The questionnaires were distributed to all 21 Danish EDs. The questionnaire was answered between March and May 2022. The response rate was 100%.
Procedure Performance
Number of physicians in the ED who can perform thoracentesis independently (yes/no/unknown) is shown in Figure 1.
Formalized Training
In 2 out of 21 (10%) EDs, a formalized training program was implemented. In these two EDs, training took place in a simulation center, lasting 2 and 3 hours, respectively. The theoretical part was taught using e-learning or classroom teaching, respectively, and hands-on training was conducted using manikins. Competences were assessed by continuous observations without the use of a checklist and there were no requirements of maintaining these competences. No formal evaluation ie, individual skill test was performed.
Informal Training
Informal training was performed in 14 out of the 21(66%) EDs. Two EDs reported to have a formalized training program. The informal training consisted of ad-hoc bedside procedural demonstration and/or guidance (n=13 (93%)), while one ED had a skill station set-up once or twice every half year.
No Training
Seven (33%) reported to have no formalized training or informal training.
Future Establishment of Formalized Training
For the 19 EDs that did not have a formalized training program, 10 EDs (53%) reported they intended to establish a formalized training program while the remaining 9 (47%) ED reported they had no intentions. Of the 7 EDs who had no formalized or informal training – 4 EDs had no intentions of establishing a formalized training program (see Table 1).
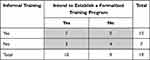 |
Table 1 Description of How Many EDs Intend to Establish a Formalized Training Program Among the EDs Who Have No Formalized Training |
Minimum Skill Requirements and Guidelines
Overall, 19 EDs (90%) reported no minimum requirements to perform thoracentesis independently whereas one ED (5%) required 5 supervised thoracenteses before performing the procedure independently and one ED (5%) reported unknown, meaning they did not know. Overall, 7 EDs (33%) reported to have a guideline on the technical aspect of the procedure and one ED (5%) answered that they used the guideline from the Danish Respiratory Society.
Discussion
In this nationwide study, we found a major lack of thoracentesis competencies among physicians in Danish EDs and that the vast majority of EDs had no formalized thoracentesis training program implemented.
We found that half of the consultants were not able to perform thoracentesis independently. In line with our study, Petrosoniak et al examined the current state of procedural skills training in Canadian physicians in emergency medicine specialist training. They found that 52–78% of specialist registrars had never performed important clinical procedures.11 Although it is unknown how many thoracenteses a physician should perform to be competent, studies have shown a positive association between the number of thoracenteses performed and the perceived competence, actual competence, and the complication rate.1,12–14 Importantly, it may be very difficult to achieve thoracentesis competencies using ad hoc bedside supervision without formalized training when the number of consultants being competent to perform thoracentesis is limited. Therefore, it is likely that a substantial amount of the Danish physicians in emergency medicine specialist training will have difficulties obtaining thoracentesis competencies given the current training efforts. Notably, in the Danish core curriculum for emergency medicine, thoracentesis competencies are mandatory to become board certified. All emergency medicine trainees in Denmark receive one hour of thoracentesis training as part of their mandatory curriculum. However, one hour of training during a five-year long education to become a consultant in emergency medicine is most unlikely to result in insufficient clinical competencies. Thus, it may be a concern that emergency medicine specialist trainees complete training despite lacking procedural skills which has also been reported by others.11
We also found that there currently are no minimum requirements to perform thoracentesis independently, and no requirements of maintenance of skills. This is in line with Bell et al who also found no requirements to maintenance of thoracentesis skills when they examined maintenance of competencies among consultants in US hospitals.15 Similar to our study, no ED program had a formalized process in place to evaluate procedural competencies during employment.15
Our study findings may be explained by the organization of the EDs in Denmark. Emergency medicine was only introduced as a medical specialty in 2017. Therefore, Danish EDs have largely been run by physicians with different medical backgrounds and thoracenteses have mostly been performed by radiologists instead of physicians in the ED. As a result, emergency physicians may have difficulties obtaining and maintaining skills. This challenge is also reported by Bucher et al reporting that physicians in emergency medicine specialist training often did not perform thoracentesis as patients were referred to the radiology department.16
Our study found that only 10% of the EDs had formalized training implemented, whereas the majority seem to use the traditional “see one, do one, teach one”-approach by ad-hoc bedside demonstration/guidance. However, the “see one, do one, teach one” approach may pose severe patient safety issues. Several studies have shown that deliberate practice with simulation training can improve thoracentesis skills and potentially patient outcome.17–19 These studies highlight the importance of structured, simulation-based training in thoracentesis training and indicate that such skills can be transferred to the clinical setting with improved patient outcomes.
The lack of thoracentesis training in Danish EDs may be due to substantial time and resource requirements for simulation-based training courses. Bell et al examined barriers for procedural training for consultants in emergency medicine and found that time and availability of courses were two main barriers for training.15 The two EDs using formalized training reported to use a massed training format of up to 3 hours course duration. This training may not be the most effective way of learning as medical education studies have found that spaced learning may be more effective.20–22 Studies evaluating if thoracentesis skills can be obtained more efficiently with more flexibility in less time- and resource-consuming manner are warranted.
It is known from numerous studies that the use of ultrasound reduces the complication risk.2,3,6 It is paramount for physicians in Emergency Medicine to have basic skills in point-of-care ultrasound before endeavoring into invasive ultrasound guided procedures. These skills are already core competences in the Danish Emergency Medicine curriculum. We have no information on the ultrasound skills among ED physicians, but it is likely that a lack of ultrasound skills may be a contributing factor to the lack of thoracentesis skills.
A number of studies have discussed thoracentesis training frequency, evaluation and maintenance of skill but no uniform agreement exists.11,15,16 This highlights the large knowledge gap on thoracentesis training, calling for a dedicated research effort to facilitate the development of evidence-based international guidelines.
With our result in mind, we recommend that each ED establish an evidence-based formalized thoracentesis training program, which take a position on continuous education and required skill competency.
Strength and Limitations
All EDs in Denmark responded the questionnaire, thus eliminating the risk of selection bias. Staff compositions change over time, and, consequently, only the prevailing status is reported. Furthermore, skill competency was estimated by the consultant being head of staff education in each ED, rather than asking each individual in each ED. Similar, respondents reported intend to establish training programs, but whether this thoracentesis training will be implemented is uncertain. Moreover, this study did not collect any data on ultrasound usability or competencies.
Conclusion
We found a major lack of thoracentesis competencies in Danish EDs among both consultant and physicians in emergency medicine specialist training. Moreover, the vast majority of EDs had no formalized thoracentesis training program.
Acknowledgments
We thank all of the respondents for participating in this study. This study received a grant from Health Research Foundation of Central Denmark Region, “Puljen til styrkelse af sundhedsforskning I Region Midtjylland” Central Denmark Region and a grant from “initiativmidler” Central Denmark Region.
Disclosure
The authors report no conflict of interest in this work.
References
1. Ault MJ, Rosen BT, Scher J, Feinglass J, Barsuk JH. Thoracentesis outcomes: a 12-year experience. Thorax. 2015;70(2):127–132. doi:10.1136/thoraxjnl-2014-206114
2. Dancel R, Schnobrich D, Puri N, et al. Recommendations on the use of ultrasound guidance for adult thoracentesis: a position statement of the society of hospital medicine. J Hospital Med. 2018;13(2):126–135. doi:10.12788/jhm.2940
3. Havelock T, Teoh R, Laws D, Gleeson F. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65(Suppl2):i61–i76. doi:10.1136/thx.2010.137026
4. Armbruster KNM, Clementsen PF. Pleuracentese. Ugeskr Læger. 2014;176:V60468.
5. Thomsen TW, Setnik GS. Thoracentesis. Thorax. 2006;1:12–15.
6. Sundhedsstyrelsen DSfA. Målbeskrivelse for Speciallægeuddannelsen I Akutmedicin [Program Description for Specialist Training in Emergency Medicine]; 2018.
7. Sundhedsstyrelsen. Vurdering af et speciale i akutmedicin i Danmark; 2017.
8. Lauridsen KG, Schmidt AS, Adelborg K, Løfgren B. Organisation of in-hospital cardiac arrest teams – a nationwide study. Resuscitation. 2015;89:123–128. doi:10.1016/j.resuscitation.2015.01.014
9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
10. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
11. Petrosoniak A, Herold J, Woolfrey K. Emergency medicine procedural skills: what are residents missing? Canadian j em med. 2013;15(4):241–248. doi:10.2310/8000.2013.130897
12. Bartter T, Mayo PD, Pratter MR, Santarelli RJ, Leeds WM, Akers SM; Bartter T, Mayo PD, Pratter MR, Santarelli RJ, Leeds WM, Akers SM. Lower Risk and. Higher Yield for Thoracentesis When Performed by Experienced Operators. Chest. 1993;103(6):1873–1876. doi:10.1378/chest.103.6.1873
13. Schonnop R, Stauffer B, Gauri A, Ha D. Procedural skills training in emergency medicine physicians within the Edmonton zone: a needs assessment. AEM Educ Training. 2021;5(2):e10495. doi:10.1002/aet2.10495
14. Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332–339. doi:10.1001/archinternmed.2009.548
15. Bell E, Fischer MA, Sinatro H. Procedural Competency in Academic Emergency Medicine Attending Physicians: how Is Competency Maintained and Evaluated by Academic Institutions in the US? Curēus. 2021;13(7):e16719–e16719. doi:10.7759/cureus.16719
16. Bucher JT, Bryczkowski C, Wei G, et al. Procedure rates performed by emergency medicine residents: a retrospective review. Int J Emerg Med. 2018;11(1):1–5. doi:10.1186/s12245-018-0167-x
17. Barsuk JH, Cohen ER, Williams MV, et al. Simulation-based mastery learning for thoracentesis skills improves patient outcomes: a randomized trial. Acad med. 2018;93(5):729–735. doi:10.1097/ACM.0000000000001965
18. Wayne DB, Barsuk JH, O’Leary KJ, Fudala MJ, McGaghie WC. Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. J Hospital Med. 2008;3(1):48–54. doi:10.1002/jhm.268
19. Duncan DR, Morgenthaler TI, Ryu JH, Daniels CE. Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero-risk environment. Chest. 2009;135(5):1315–1320. doi:10.1378/chest.08-1227
20. Yeung J, Djarv T, Hsieh MJ, et al. Spaced learning versus massed learning in resuscitation — a systematic review. Resuscitation. 2020;156:61–71. doi:10.1016/j.resuscitation.2020.08.132
21. Versteeg M, Hendriks RA, Thomas A, Ommering BWC, Steendijk P. Conceptualising spaced learning in health professions education: a scoping review. Med Edu. 2020;54(3):205–216. doi:10.1111/medu.14025
22. Sullivan A, Elshenawy S, Ades A, Sawyer T. Acquiring and Maintaining Technical Skills Using Simulation: initial, Maintenance, Booster, and Refresher Training. Cureus. 2019;11(9):e5729–e5729. doi:10.7759/cureus.5729
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

