Back to Journals » Clinical Epidemiology » Volume 10
Labor augmentation during birth and later cognitive ability in young adulthood
Authors Stokholm L, Talge NM, Christensen GT , Juhl M, Mortensen LH , Strandberg-Larsen K
Received 21 July 2018
Accepted for publication 25 October 2018
Published 26 November 2018 Volume 2018:10 Pages 1765—1772
DOI https://doi.org/10.2147/CLEP.S181012
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Henrik Sørensen
Lonny Stokholm,1 Nicole M Talge,2 Gunhild Tidemann Christensen,3–5 Mette Juhl,6 Laust Hvas Mortensen,1,7Katrine Strandberg-Larsen1
1Section of Epidemiology, Department of Public Health, University of Copenhagen, Copenhagen, Denmark; 2Department of Epidemiology and Biostatistics, Michigan State University, Michigan, USA; 3Department of Public Health, University of Southern Denmark, Danish Aging Research Center, Odense, Denmark; 4Center for Clinical Research and Prevention, Bispebjerg and Frederiksberg Hospital, Capital Region, Copenhagen, Denmark; 5Department of Public Health, University of Copenhagen, Copenhagen, Denmark; 6Department of Midwifery, Copenhagen University College, Copenhagen, Denmark; 7Methods and Analysis, Statistics Denmark, Copenhagen, Denmark
Purpose: Synthetic oxytocin for labor augmentation during birth has been linked to negative neurodevelopment effects in children. We examined whether maternal labor augmentation was associated with lower cognitive ability in young adulthoods.
Patients and methods: We identified 330,107 individuals (96.6% were men), with noninduced labor and with a cognitive ability test score, the Børge Priens Prøve (BPP) score, from draft board examinations in 1995–2015 (mean age, 18.8 years). Information on maternal labor augmentation was ascertained from the Danish Medical Birth Register, and we calculated mean differences in the BPP score according to maternal labor augmentation. We repeated our analyses in a sub-sample of siblings to control for unmeasured familial confounding.
Results: Maternal labor augmentation was not associated with any noticeable decline in cognitive ability. However, the difference in the mean BPP score for exposure to maternal labor augmentation varied according to maternal parity, as the mean difference in BPP scores increased with increasing parity, in nulliparous: mean difference=–0.14 (95% CI=–0.23 to –0.04); in maternal parity 4+: mean difference=–1.21 (95% CI=–2.905 to –0.37). The sibling analysis showed little influence of shared familial factors on the association.
Conclusion: The mean BPP was slightly lower among labor augmented compared to nonaugmented and with an increasing difference with increasing parity. However, the differences were small and could not be considered of any clinical relevance. Furthermore, the sibling analyses suggested little confounding by familial factors.
Keywords: Børge Priens Prøve, dystocia, neurodevelopment, oxytocin, siblings
Introduction
Labor augmentation with synthetic oxytocin is the primary medical treatment for dystocia,1,2 that is the most common birth complication among nulliparous women.3 Estimates from the beginning of this millennium suggest that 51% of deliveries by nulliparous women in USA4 and 43%–58% of all deliveries in Europe included treatment with synthetic oxytocin for labor augmentation. Synthetic oxytocin for labor augmentation has also been associated with several adverse effects, including uterine hyperstimulation, uterine rupture, cesarean section, neonatal distress, and neonatal intensive care unit admission.5–7 Therefore, the US Institute for Safe Medication Practices has designated synthetic oxytocin as a high-alert drug, bearing a heightened risk of harm when used inappropriately.8
In addition, possible long-term adverse effects, such as a potentially harmful influence on neurodevelopment, have been suggested. Although it is unclear whether oxytocin can cross the fetal blood–brain barrier, effects on the developing brain may exist given association of synthetic oxytocin with neonatal distress and hypoxia.5,9 Currently, the full scope of the potential impact of synthetic oxytocin during delivery on child neurodevelopment has not yet been clarified, as studies to date suggest inconsistent links with various neurodevelopmental outcomes, including autism spectrum disorder (ASD),10 attention deficit hyperactivity disorder (ADHD),11–13 gross motor development, and cognitive performance in childhood and young adults.14–16 Sex differences were considered in some of the studies.10,12,15 These associations may be driven by unobserved maternal confounding, but to our knowledge, sibling comparisons with control for familial factors have not been used in this field, although there is a considerable variation in the use of synthetic oxytocin across births. We hypothesized that maternal labor augmentation with oxytocin is associated with lower cognitive ability in a cohort of young men and women who were evaluated for military service. Moreover, we also examined the association in a sub-sample of siblings, which allowed us to adjust for confounding due to unmeasured familial factors that are shared among siblings.
Materials and methods
Individuals registered in either the Danish Defence Personnel Organisations Database (1995–2005: n=219,824) or the Danish Conscription Registry17,18 (2006–2015: n=335,244) were eligible for inclusion. From the registers, information on the draft board examination score (Børge Priens Prøve [BPP]) was available. Some individuals (n=1481) had completed the test more than once because they had been called more than once due to, eg, postponement for educational reasons or need for re-evaluation due to health problems. In these cases, we used the first (ie, earliest) BPP score for the analysis. The individuals were evaluated for military service between the age of 18 and 26 years (compulsory for men and optional for women). We restricted the sample to draft board attendees born between 1980 and 1996 with a valid record of a singleton birth and a noninduced delivery registered in the Danish Medical Birth Register19 (n=406,051). We excluded individuals with missing BPP test scores, (n=52,414). We then linked this database to Statistics Denmark20 and the Danish National Patient Register21 and further excluded individuals with missing information on maternal labor augmentation (n=4,333), maternal education, gestational age, or intrauterine growth (n=19,197). This resulted in a study population of 330,107 individuals. Some mothers contributed with more than one child to the cohort, and by using the unique ID number of the mothers, we identified 109,448 siblings for sub-analyses.
We are aware that the study population included pregnancies that ended with a planned cesarean section, even though they are not at risk of being exposed to labor augmentation. They are included in this study population because the data in the Medical Birth Register, from 1980 to 1991, did not allow differentiating between planned and acute cesarean sections.
Labor augmentation
We used information on maternal labor augmentation (yes and no) from the Danish Medical Birth Register as a proxy for oxytocin exposure. At this time, register data did not include information on the medication used for augmentation, but according to textbooks22 from this time period, synthetic oxytocin was the first choice of medication when medical treatment for dystocia was required. Synthetic oxytocin can potentially have been used for labor induction, and therefore, we excluded deliveries where the labor was induced. Furthermore, augmentation and artificial rupture of membranes were registered separately. This means that the code “augmentation” can be regarded as referring to medical augmentation alone.23
Cognitive ability
Cognitive ability was assessed using the BPP, which consists of four subtests designed to assess logical, verbal, numerical, and spatial reasoning.24 The total BPP score is the sum of correct answers across these four subtests (range, 0–78), with higher scores representing higher levels of cognitive ability.
Covariates
The selection of potential confounders for the association between labor augmentation and cognitive ability was guided by Directed Acyclic Graphs (DAGs)25,26 and prior knowledge from existing literature. From the Danish Medical Birth Register, we abstracted the following information: birth year as 1-year intervals in the adjusted model (1980–1996), maternal age at delivery in years (<20, 20–24, 25–29, 30–34, 35–39, and 40+), maternal parity (0, 1, 2, 3, and 4+), maternal smoking (yes/no, only available from 1991 onward), gestational age in completed weeks (<37, 37–41, and 42+), and intrauterine growth (small for gestational age [SGA], ≤10th percentile; appropriate for gestational age [AGA]; large for gestational age [LGA], >90th percentile).27
From the Danish National Patient Register, we abstracted information on maternal preeclampsia (yes/no) registered by diagnostic codes (ICD-8: 637.03, 637.04, 637.09; ICD-10: O14.0, O14.1, O14.9)28 and maternal diabetes (yes, no) registered by diagnostic codes (ICD-8: 240, 250; ICD-10: E10-14, O24).29 From Statistics Denmark, we retrieved the highest maternal educational level attained in the year corresponding to the index individual’s birth. We then categorized this information according to the International Standard Classification of Education guidelines30 (ISCED 2011): low, level 0–2 (lower secondary education or lower); middle, level 3–4 (upper secondary education); and high, level 5–6 (postsecondary education).
Information on sex was available in both the Danish Defence Personnel Organisations database and the Danish Conscription Registry, but information on height and weight, from which we calculated the individual’s body mass index (BMI; <18.5, 18.5–24.9, 25.0–29.9, and 30+ kg/m2), was only available in the Danish Conscription Registry.31
Missing data
Implausible combinations of birth weight and gestational age were identified using predefined cut points32 and were coded as missing (n=689). Heights and weights beyond 4.5 SDs (standardized for age and sex)33 were also replaced with missing values (n=367).
Statistical modeling
By using Generalized Estimating Equations (GEE) model, we examined whether the mean BPP scores differed between individuals exposed to maternal labor augmentation and individuals who were not exposed. To account for the presence of siblings in the data set, we used the GEE model with robust standard error.
We then repeated the analysis with adjustment for birth year, maternal age, maternal education, maternal parity, preeclampsia, diabetes, gestational age, intrauterine growth, and sex.
Since the military draft board examination is voluntary for women, they likely represent a selected subgroup; thus, we examined the association for interaction with sex. Gestational age has been found to be associated with cognitive functioning and impaired cognitive ability,34 and therefore, we examined the interaction with preterm delivery (<37 weeks). Finally, since nulliparous women are more likely to be exposed to labor augmentation and research have shown that later-born children have lower intelligence on average than the first-born child,35 we examined the interaction with maternal parity. We assessed the interaction based on a P-value <0.05, and in case of interactions, we stratified the analyses and modeled the joint effect.
Sensitivity analyses
To examine the robustness of our findings, we performed four sensitivity analyses.
First, in a study population containing deliveries with an induced (medical and mechanical) and noninduced onset of labor, we examined if adjusting for labor induction changed the results.
Second, we examined the association in a sub-sample of children born 1991–1996 where we excluded pregnancies that ended with a planned cesarean section (available from 1991 to 1996) since these mothers were not at risk of being exposed to labor augmentation. Third, we analyzed the association in a sub-sample where information on maternal smoking was available (available from 1991 to 1996). Fourth, almost one-third (n=102,172) had missing BMI data, and we re-ran the analyses in the sub-sample with the complete BMI data, modeling BMI as a confounder.
Sibling analyses
In the sub-sample restricted to siblings, we initially examined the association between maternal labor augmentation and cognitive ability using a general linear regression model (unpaired model). In addition, we analyzed the association using a family fixed effect that compared siblings within the same family with one another in paired (families with two siblings) and clustered (families with more than two siblings) data. We then repeated these analyses following adjustment for the covariates that vary within families: birth year, maternal age, maternal education, maternal parity at birth, preeclampsia, diabetes, gestational age, intrauterine growth, and sex.
The difference between the unpaired model and the family fixed effect model was used as an indication of familial confounding, where attenuation of the association in the family fixed effect model will reflect confounding from shared familial factors.
This study was approved by the Faculty of Health Science, the University of Copenhagen (j.no. 2015-57-0121). According to Danish legislation, no informed consent or ethical approval is required when using register data.
Results
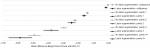
In the full sample, more than one of five (22%) individuals had been exposed to maternal labor augmentation, with the rates of maternal labor augmentation increasing across the birth year. Mean age at draft board examination was 18.8 years (SD=1.1) with a majority of men (96.6%). Women who received medical labor augmentation were more likely to be in their twenties than nonaugmented women, have an education at the upper secondary level or postsecondary level, be nulliparous, and were slightly less likely to give birth at term. For the grown-up children, there was no difference in sex ratio or age of draft board attendees, but those who had been exposed to labor augmentation at birth were more likely to have a BMI above 18.5 kg/m2 at the draft board examination (Table 1). Prior to adjustment for covariates we found a slightly increased BPP score (mean difference, 0.18 [95% CI=0.11–0.26]). Adjustment changed the direction of the association to a slightly lowered BPP score among individuals exposed to maternal labor augmentation, (mean difference, –0.19 [95% CI=–0.26 to –0.12]) compared to nonexposed individuals (Table 2). The reversed direction of the association was foremost driven by maternal parity; the mean differences in BPP scores increased with advancing parity for those exposed to maternal labor augmentation. Furthermore, maternal parity itself (independent of oxytocin) is associated with a lower BPP (Figure 1).
For individuals born to mothers with parity 4+, the (mean difference, –1.21 [95% CI=–2.05 to –0.37]) in maternal labor augmentation exposed vs nonexposed, whereas this (mean difference, –0.14 [95% CI=–0.23 to –0.03]) in nulliparous women (Table 2). Modeling the joint effect of maternal labor augmentation and maternal parity showed that an increase in parity had the most effect on the mean difference in BPP scores, but also that the mean differences in BPP scores between the maternal labor augmented and nonaugmented increased in the higher parity groups (Figure 1).
In the sub-sample of siblings, 29% were discordant on exposure to maternal labor augmentation. The estimates from the unpaired model was for the model not stratified on parity, in the opposite direction than for the total sample (mean difference, –0.09 [95% CI=–0.22 to –0.04]) Comparing the results from the unpaired model with the results from the family fixed effect model suggested little confounding by familial factors shared by siblings. Again, adjustment for especially maternal parity attenuated the association in both the unpaired and the family fixed effect model (Table 3).
Overall, the sensitivity analyses showed findings similar to those of the full study population; however, in the adjusted analyses, the effect of maternal parity on maternal labor augmentation attenuated (Tables S1–S4). Furthermore, there was no evidence for statistical interaction between sex and maternal labor augmentation or between gestational age and maternal labor augmentation (data not shown). Despite the interaction with sex was insignificant, which could be due to the limited number of females, we present the results restricted to a female population in Table S5.
Discussion
In this large cohort study, we found a slightly reduced BPP score among individuals exposed to maternal labor augmentation compared to nonexposed individuals. However, the difference was small, and the significance was likely driven by our large sample size; hence, we do not consider these overall findings to be clinically relevant. Data revealed an interaction with maternal parity, showing stronger associations among multiparous women as the mean difference in BPP increased with increasing parity. Finally, the analyses among siblings did not indicate any strong confounding by shared familial factors.
Our findings are much in line with previous findings from a smaller Danish study on men evaluated for military service in 2003–2004 in a geographically restricted part of Denmark, in which no association between labor augmentation and cognitive performance was observed.16 Our findings do not support a previously published study indicating lower performance on the Raven’s instruments among children who have been exposed to synthetic oxytocin at birth.14 This study included oxytocin for labor induction and did not have parity in the analyses, which may explain why the findings differ from our study. Our findings add to the existing literature by demonstrating parity differences in the effect of labor augmentation on cognitive ability. This interaction effect could be explained by the competing risk of maternal age since advanced maternal age has been associated with pregnancy-related complications36 and adverse perinatal outcomes37 or a neonatal risk due to a grand multipara mother.38 Furthermore, since labor augmentation is less common among multiparous mothers than among nulliparous mothers,36 labor augmentation in the context of multiparity may be a proxy for less optimal pregnancy, antepartum, and/or postnatal factors that may have impact on neurodevelopment.
The population-based design enabled us to restrict to a sub-sample of individuals who shared the same mother and who also attended the draft board examination. Thus, we were able to perform a family fixed effect analyses within sibling pairs to examine a potential influence of unmeasured familial factors such as maternal intelligence or socioeconomic position. We found that siblings exposed to maternal labor augmentation generally scored higher on the BPP than their nonexposed siblings in the crude analyses. However, this was driven by the in-built parity difference in sibling pairs and that it was most often the earliest born who was exposed to labor argumentation. In the sub-sample of siblings, 59% of the firstborn and 27% of the second-born siblings were exposed to maternal labor augmentation, and in the adjusted analyses, there was no association between labor argumentation and BPP score. Furthermore, research has indicated higher intelligence among firstborn men when measured within the family.35 In the sibling analyses, we specifically included siblings differently exposed to maternal labor augmentation, since those are the only siblings who contribute to the estimate. Furthermore, we adjusted for confounding by birth year, maternal age, maternal education, maternal parity, preeclampsia, diabetes, gestational age, intrauterine growth, and sex where siblings were likely to differ from each other. In the sibling analyses, we have, therefore, reinforced the confounding by maternal parity per design. The properties of sibling analyses to amplify confounding from nonshared confounders have been described in detail elsewhere.39,40 Future studies might benefit from examining the association in a sub-sample of cousins. This would make it possible to match on parity in order to remove the effect of parity, which is not possible when comparing siblings. However, we have no reason to believe that such a design will alter our conclusions, as there is no indication that unmeasured familial confounding is a serious concern.
Strengths and limitations
This study was based on long follow-up with little risk of selection bias since we used the data from national registers in Denmark and exploited the set-up that draft board is mandatory for men, and this examination includes a test for cognitive ability. Our data sets primarily contained men and approximately 3% women, and therefore, you can discuss to what degree our results can be generalized to women. However, there was no sign of interaction, which potentially could be a power issue, and the conclusions were similar in the sub-sample of women despite the slight change in estimates.
This study was restricted to deliveries with a noninduced onset of labor, because induced deliveries from the early years of our study period may have involved oxytocin as a induction agent. Even though prostaglandins were introduced as a induction agent during the late 1960s,41 several studies conducted from the 1980s and early 1990s42,43 on prostaglandins (oral or vaginal application) vs oxytocin (intravenous infusion) indicated that the general shift from oxytocin to prostaglandins as the first choice of drug for labor induction has taken place at some point during our study period. In a sensitivity analysis, we included deliveries with an induced onset of labor to the study population and examined if the results would change if we adjusted for labor induction. The results did not change our conclusion.
Pregnancies that end in a planned cesarean section are not at the risk of maternal labor augmentation. Thus, our findings could be underestimated due to information bias. We were only able to identify planned cesarean section for a sub-sample of individuals born 1991–1996, thus, we performed a sensitivity analyses where we excluded pregnancies that ended in a planned cesarean section. The analyses revealed an attenuated effect of maternal labor augmentation, most likely due to the smaller sub-sample. Potential nondifferential misclassification of labor augmentation may exist in the Danish Medical Birth Register since pregnancy and birth-related information until 1996 were reported by the medical staff to the register in a paper form and since registration error when inputting data and lack of knowledge for the purpose of registration is possible.44 We have not been able to find any studies that explicitly validated the registration of labor augmentation in the Danish Medical Birth Register from the time period in question, but pregnancy complications such as placenta previa, abruption placenta, hydramnios, hypertensive disorders in the Danish Medical Birth Register have been validated with good agreement.19
The BPP has been used in Denmark for the draft board examination since its incorporation in 1957. The constructions of the test and the four subtests have remained unchanged. The test is not available to the public, and it has a correlation of 0.82 with the Wechsler Adult Intelligence Scale (WAIS) full-scale IQ score. This indicates that the BPP is closely related to this standard measure of general intelligence and that it is a useful indicator of cognitive ability.45 It is possible that some young adults with little motivation for serving in the military purposefully underperformed on the draft board examination test in an attempt to appear unqualified for military service. However, studies suggest that negative attitudes toward military service are associated with higher BPP scores and higher educational levels.46 Moreover, on suspicion of cheating, the Danish Military registered the code 99, and a new BPP test was made. In this study, we considered BPP score values of 99 as invalid, and together with the missing BPP score, they were excluded. Therefore, we have no reason to believe that individuals in our sample deliberately scored lower on the BPP or that our findings should be biased due to an attempt to appear unqualified and re-examination.
Conclusion
Our results showed a slightly reduced BPP score among individuals registered with noninduced labor and exposed to maternal labor augmentation and born by a multiparous mother, but we considered the effect to be small and of no clinical relevance. The interaction between maternal labor augmentation and maternal parity may be explained by advanced maternal age or less optimal pregnancy and delivery that may impact cognitive ability, and if replicated, maternal age and complication during pregnancy may be next step for future research. Furthermore, the sibling analyses showed little influence of shared familial factors on the association.
Author contributions
KS-L and LS developed the study idea. KS-L, GTC, NMT, MJ, and LS initiated the study and developed the analytic strategy. Data management and statistical analyses were performed by LS. KS-L and LS had full access to all data in the study, but LS takes responsibility for the integrity of the data and the accuracy of the analyses. LHM participated in performing the sibling analyses. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Owen J, Hauth JC. Oxytocin for the induction or augmentation of labor. Clin Obstet Gynecol. 1992;35(3):464–475. | ||
Kjaergaard H, Olsen J, Ottesen B, Dykes AK. Incidence and outcomes of dystocia in the active phase of labor in term nulliparous women with spontaneous labor onset. Acta Obstet Gynecol Scand. 2009;88(4):402–407. | ||
ACOG Practice Bulletin Number 49, December 2003. Dystocia and augmentation of labor. Obstet Gynecol. 2003;102(6):1445–1454. | ||
Zhang J, Branch DW, Ramirez MM, et al. Oxytocin regimen for labor augmentation, labor progression, and perinatal outcomes. Obstet Gynecol. 2011;118(2 Pt 1):249–256. | ||
Oscarsson ME, Amer-Wåhlin I, Rydhstroem H, Källén K. Outcome in obstetric care related to oxytocin use. A population-based study. Acta Obstet Gynecol Scand. 2006;85(9):1094–1098. | ||
Selo-Ojeme D, Rogers C, Mohanty A, Zaidi N, Villar R, Shangaris P. Is induced labour in the nullipara associated with more maternal and perinatal morbidity? Arch Gynecol Obstet. 2011;284(2):337–341. | ||
Bernitz S, Øian P, Rolland R, Sandvik L, Blix E. Oxytocin and dystocia as risk factors for adverse birth outcomes: a cohort of low-risk nulliparous women. Midwifery. 2014;30(3):364–370. | ||
Clark SL, Simpson KR, Knox GE, Garite TJ. Oxytocin: new perspectives on an old drug. Am J Obstet Gynecol. 2009;200(1):35.e1–3535. | ||
Wahl RU. Could oxytocin administration during labor contribute to autism and related behavioral disorders?--A look at the literature. Med Hypotheses. 2004;63(3):456–460. | ||
Weisman O, Agerbo E, Carter CS, et al. Oxytocin-augmented labor and risk for autism in males. Behav Brain Res. 2015;284:207–212. | ||
Kurth L, Haussmann R. Perinatal Pitocin as an early ADHD biomarker: neurodevelopmental risk? J Atten Disord. 2011;15(5):423–431. | ||
Silva D, Colvin L, Hagemann E, Bower C. Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133(1):e14–e22. | ||
Henriksen L, Wu CS, Secher NJ, Obel C, Juhl M. Medical augmentation of labor and the risk of ADHD in offspring: a population-based study. Pediatrics. 2015;135(3):e672–e677. | ||
Freedman D, Brown AS, Shen L, Schaefer CA. Perinatal oxytocin increases the risk of offspring bipolar disorder and childhood cognitive impairment. J Affect Disord. 2015;173:65–72. | ||
González-Valenzuela MJ, López-Montiel D, González-Mesa ES. Exposure to synthetic oxytocin during delivery and its effect on psychomotor development. Dev Psychobiol. 2015;57(8):908–920. | ||
Sørensen HT, Steffensen FH, Sabroe S, Rothman KJ, Gillman MW, Fischer P. Historical cohort study of in utero exposure to uterotonic drugs and cognitive function in young adult life. West J Med. 1999;170(5):433–434. | ||
Green A. The Danish Conscription Registry: a resource for epidemiological research. Dan Med Bull. 1996;43(5):464–467. | ||
Christensen GT, Skogstad S, Nissen LR, Osler M. Data resource profile: Danish Conscription Registry Data (DCRD). Int J Epidemiol. 2018;47(4):1023–1024. | ||
Kristensen J, Langhoff-Roos J, Skovgaard LT, Kristensen FB. Validation of the danish birth registration. J Clin Epidemiol. 1996;49(8):893–897. | ||
Denmark S [homepage on the Internet]. Documentation of Statistics Denmark. Available from: http://www.dst.dk/en/Statistik/dokumentation/documentationofstatistics. Accessed April 9, 2017. | ||
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. | ||
Falck Larsen JTS. Obstetrik/gynækologi, Basisbog. Vol. 4. udgave, 2. oplag: Munksgaard; 1983. | ||
Sundhedsstyrelsen. Medicinsk Fødselsstatistik 1985. The National Board of Health; 1985. | ||
Teasdale TW. The Danish draft board’s intelligence test, Børge Priens Prøve: psychometric properties and research applications through 50 years. Scand J Psychol. 2009;50(6):633–638. | ||
Hernán M, Robins J. Graphical Representation of Causal Effects in Causal Inference. Boca Raton: Chapman & Hall/CRC, forthcoming. | ||
Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22(5):745. | ||
Marsál K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 1996;85(7):843–848. | ||
Wu CS, Nohr EA, Bech BH, Vestergaard M, Catov JM, Olsen J. Health of children born to mothers who had preeclampsia: a population-based cohort study. Am J Obstet Gynecol. 2009;201(3):269.e261–269.269. | ||
Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K, Steering Group of the National Diabetes Register. The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia. 2008;51(12):2187–2196. | ||
Unesco Statistics. International Standard Classification of Educatio, Isced 2011. 2012; http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf, 2012. | ||
World Health Organization. WHO Global database on Body Mass Index. BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. | ||
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87(2):163–168. | ||
Aarestrup J, Bjerregaard LG, Gamborg M, et al. Tracking of body mass index from 7 to 69 years of age. Int J Obes. 2016;40(9):1376–1383. | ||
Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Preterm cognitive function into adulthood. Pediatrics. 2015;136(3):415–423. | ||
Black SE, Devereux PJ, Salvanes KG. Older and wiser? birth order and IQ of young men. CESifo Econ Stud. 2011;57(1):103–120. | ||
Waldenström U, Ekéus C. Risk of labor dystocia increases with maternal age irrespective of parity: a population-based register study. Acta Obstet Gynecol Scand. 2017;96(9):1063–1069. | ||
Kenny LC, Lavender T, Mcnamee R, O’Neill SM, Mills T, Khashan AS. Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PLoS One. 2013;8(2):e56583. | ||
Bai J, Wong FW, Bauman A, Mohsin M. Parity and pregnancy outcomes. Am J Obstet Gynecol. 2002;186(2):274–278. | ||
Frisell T, Öberg S, Kuja-Halkola R, Sjölander A. Sibling comparison designs: bias from non-shared confounders and measurement error. Epidemiology. 2012;23(5):713–720. | ||
Mortensen LH, Torssander J. Family of origin and educational inequalities in mortality: Results from 1.7 million Swedish siblings. SSM Popul Health. 2017;3:192–200. | ||
Osler M. Fødselshjælpens historie. Medicinsk-Historisk Museum, Københavns Universitet; 2002. | ||
O’Brien WF. The role of prostaglandins in labor and delivery. Clin Perinatol. 1995;22(4):973–984. | ||
Lyndrup J, Legarth J, Dahl C, Philipsen T, Eriksen PS, Weber T. Induction of labour: the effect of vaginal prostaglandin or i.v. oxytocin--a matter of time only? Eur J Obstet Gynecol Reprod Biol. 1990;37(2):111–119. | ||
Hemminki E, Teperi J, Tuominen K. Need for and influence of feedback from the Finnish birth register to data providers. Qual Assur Health Care. 1992;4(2):133–139. | ||
Mortensen EL, Reinisch JM, Teasdale TW. Intelligence as measured by the WAIS and a military draft board group test. Scand J Psychol. 1989;30(4):315–318. | ||
Teasdale TW, Hartmann PV, Pedersen CH, Bertelsen M. The reliability and validity of the Danish Draft Board Cognitive Ability Test: Børge Prien’s Prøve. Scand J Psychol. 2011;52(2):126–130. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.