Back to Journals » Infection and Drug Resistance » Volume 14
Knowledge, Attitudes, and Practices of Antimicrobial Uses and Resistance Among Public University Students in Bangladesh
Authors Marzan M , Islam DZ , Lugova H , Krishnapillai A, Haque M , Islam S
Received 2 November 2020
Accepted for publication 13 January 2021
Published 11 February 2021 Volume 2021:14 Pages 519—533
DOI https://doi.org/10.2147/IDR.S289964
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Mahfuza Marzan,1 Dewan Zubaer Islam,1 Halyna Lugova,2 Ambigga Krishnapillai,3 Mainul Haque,4 Salequl Islam1
1Department of Microbiology, Jahangirnagar University, Savar, Dhaka, 1342, Bangladesh; 2The Unit of Community Medicine, Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kuala Lumpur, 57000, Malaysia; 3The Unit of Family Medicine, Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kuala Lumpur, 57000, Malaysia; 4The Unit of Pharmacology, Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kuala Lumpur, 57000, Malaysia
Correspondence: Salequl Islam
Department of Microbiology, Jahangirnagar University, Savar, Dhaka, 1342, Bangladesh
Tel +880-1715029136
Fax +880-2-7791052
Email [email protected]
Mainul Haque
Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kem Perdana Sungai Besi, 57000, Kuala Lumpur, Malaysia
, +60109265543
Email [email protected]
Background: Antibiotics are lifesaving drugs, and inappropriate uses lead to the resistance that renders them ineffective. This study aims to understand knowledge, attitude, and practice (KAP) concerning antibiotic use and resistance among university students in Bangladesh.
Methods: A cross-sectional study was performed from January to April 2020 among students at Jahangirnagar University (JU), Bangladesh. Purposive sampling was conducted through an in-person interview using a structured questionnaire. Students from the faculties of biological sciences and non-biology background were included. The univariate ordinal regression technique was used to analyze the relationship between predictors and good knowledge about the antibiotics. A two-tailed p-value was calculated to determine statistical association.
Results: Out of 205 study participants, 92 and 113 responders were from biological science faculty and non-biology disciplines, respectively. Less than half of the students (42.4%) showed a good knowledge level (scores higher than 80%). Biology-background students possess better knowledge than non-biology students [odds ratio (OR) = 4.44, 95% confidence level (CL) (2.56, 7.70), p < 0.001]. A better attitude was noticed among all students. The self-medication rate was quite low, and more than 90% of students were found to consume antibiotics according to the physician’s prescription. Lack of treatment adherence was recorded, and students admitted to stop-taking antibiotics when symptoms disappeared (48.67% biology and 36.26% non-biology). Multivariate regression analysis was unable to detect any significant association between self-medication and gender, student category or the level of knowledge about antibiotics.
Conclusion: Students of biological science background possessed better knowledge indicating the importance of appropriate curriculum imparted in knowledge buildup. Introducing a short course about the risk and development of antibiotic resistance will grow the students’ awareness to avoid the resistance phenomenon.
Keywords: knowledge, anti-bacterial agents, antibiotic, drug resistance, state-owned, university students, Bangladesh
Introduction
The emergence and spread of antibiotic resistant pathogens pose a big challenge to policy-makers, … …. transformation of health systems that evolved to provide easy access to these drugs into ones that encourage appropriate use of antimicrobials, whilst reducing the risk of resistance.1
Antimicrobials have saved millions of lives and expanded humans’ average life expectancy since penicillin’s breakthrough in 1928 and other subsequent discovery of antimicrobial classes.2 Besides treating infectious diseases, antibiotics ensured the safety of numerous emergency medical procedures, including surgery and organ transplant. However, the drugs’ success is evaluated by the drugs’ capacities to encounter the emergence of resistance in pathogenic bacteria. The resistance of bacteria to almost all antibiotic types is a worldwide public health problem.3,4 It is estimated that around ten million deaths can occur every year by 2050 due to antibiotic-resistant bacteria.5 Antimicrobial resistance (AMR) is responsible for thousands of deaths worldwide and economic loss due to the increased hospital stays, unnecessary drug consumption, and increased burden with diagnostic costs. The resistance of bacteria to antibiotics is a natural phenomenon, often caused by genetic mutations in chromosomes under selective pressure, and most importantly, this phenomenon can be transferred horizontally to other bacteria through the exchange of extrachromosomal resistant plasmids.6 As the resistant bacteria have no “evolutionary disadvantage,” it is unlikely that the bacteria will lose its resistance over time; therefore, scientists warn the appropriate use of antibiotics to prevent the emergence of primary resistance.7 Availability of antibiotics from pharmacies without authorized prescription and overuse or misuse of antibiotics such as self-medication practice, non-adherence to the prescription, inappropriate prescribing, and lack of antibiotic susceptibility testing can play a vital role in the evolvement of antibiotic resistance.8–10 Moreover, the uncontrolled antibiotics applications in animal husbandry as therapeutic, prophylactic, and growth enhancers can contribute to the emergence of resistant bacteria that enter humans through the food chain.11 A study indicated that South East Asia is at the highest risk of developing and spreading antibiotic resistance, and it suggested One Health approach to address this problem.12 A systematic review has identified a very high resistance to common antibiotics in Bangladesh with the prevalence of extended-spectrum beta-lactamase (ESBL) producing E. coli and methicillin-resistant Staphylococcus aureus (MRSA).13 The presence of antibiotic-resistant bacteria has been reported in different sources, including hospital waste, poultry, and environmental samples.14–16 Inappropriate and incomplete prescription by physicians, non-compliance to the prescribed antibiotics, availability of antibiotics as non-prescription drugs in the pharmacies have been reported in Bangladesh.17,18
Antimicrobial self-medication is frequently observed in low-and middle-income countries (LMICs), including Bangladesh.19–21 It has been reported that although Bangladesh has possessed national drug22 and health23 policy, additionally, access to public healthcare reasonably good.20 Nevertheless, a large portion of antimicrobials consumption in Bangladesh remains without a licensed medical doctor prescription.24,25 Antimicrobials principally consumed in Bangladesh as self-purchased from community pharmacy snubbing national guiding principle.19,26,27 Antimicrobials consumption as self-purchased or imprudently prescribed frequently correlated with increased drug interactions, hiding symptoms of primary disease and expanding microbial resistance.28–30 It has been reported that self-medication frequently correlated to unnecessary expenditure in both the public healthcare budget and individual and community.31 Although any use of antimicrobials still rational and prudent contributes to the development of microbial resistance as the process of evolution,3 extensive superfluous, irrational, and imprudent use frequently contribute to treatment challenges.10,32,33 Multiple studies reported that poor knowledge regarding use of antibiotics frequently correlated with irrational consumption of antimicrobials even among medical students.34–36 The causes of self-medication with antimicrobials were identified as trivial illness, time-saving, possessing old prescriptions and high consultation fees.37,38
The biggest challenge for the healthcare sector is to educate people about antibiotics, its side effects, and to encourage them to stop the misuse of antibiotics. The lack of knowledge about self-medication is the prime reason for mass scale antibiotic resistance tragedy.31
Public awareness of antibiotic resistance is indispensable to mitigate this insidious problem.39–41 As the World Health Organization (WHO) emphasized, the behavioral change towards the irrational use of antibiotics, otherwise any new addition to the antibiotic will become ineffective.42 To understand the current public perception and habits, KAP-based studies on antibiotic prescribing, consumption, and antibiotic resistance are conducted in different countries on diverse groups, including medical students, university students, health workers, and common public.36,43,44 Continuation of such studies is necessary to understand common cultural beliefs, knowledge gaps, and practice behavior of a particular social group. In Bangladesh, the young population plays a vital role in different societal movements. However, KAP on antibiotic use and antibiotic resistance of this group of people, especially among university students, are yet to be explored. Therefore, we aimed to conduct a cross-sectional study among the leading public university in Bangladesh to understand KAP concerning antibiotic uses and resistance. We also sought to know whether the students of biological science faculty have better KAP than other faculties.
Methods and Materials
Study Design
A cross-sectional design was used in this study to collect information on knowledge and attitude regarding antibiotics among public university biology and non-biology students.
Sample Size
JU is a public university of Bangladesh that accommodates over 16,000 students. JU covers a broad range of disciplines, such as mathematical and physical sciences, biological sciences, arts and humanities, social sciences, business studies, and law. Sample size was calculated utilizing online sample size calculator Raosoft (http://www.raosoft.com/samplesize.html). The margin of error was 5% and CL 95%. After that the sample size was 376 as the total population was 16,000. We expect there will be drop out and noise data around 5%. Thereafter, this research firstly planned for 396 were sample population size.
Study Population
Mostly undergraduates’ students approached through an in-person interview where answers were inscribed in a printed questionnaire (Figure 3). A previously validated printed study instrument was used to gather data in the most time and cost-efficient way.
Sampling Method
Although this study group initially planned for random sampling, nevertheless, purposive sampling (mostly snowball technique) method was adopted for the current study because of the COVID-19 pandemic. Furthermore, to avoid selection bias this study we included all 16 residential halls.
Study Period
This cross-sectional study was performed from January to April 2020 among undergraduate and graduate JU university students during initial day of the COVID-19.
Preparation of Questionnaire
The questionnaire was prepared based on a literature review of similar studies conducted in different parts of the world,36,45 with some modifications in the questions based on common practice knowledge in Bangladesh. The questionnaire was separated into four sections. The first section included the demographical information. The second section included seven questions to measure students’ level of knowledge regarding antibiotics and antibiotic resistance. This section contained seven questions, evaluated using “true,” “false,” and “uncertain” responses. The third section was designed to understand the students’ attitudes towards some common philosophy about preventing antibiotic resistance. In the third part, a three-point response scale by “agree,” “disagree” and “uncertain” was used to determine the attitudes. The fourth section was created to understand the common practice among students related to antibiotic intake strategy, clinical phenomena when the antibiotic is used, and the failure to complete the course of antibiotics. The practices part further evaluated the student participants’ habitude about antibiotic use and their adherence to dosing and treatment courses. The study instrument was pre-tested and validated in the local context involving 48 [16X3=48 (3 from each hall)] students. These students did not participate in the subsequent principal study. The questionnaire sections demonstrated acceptable values, with a range between 0.672 and 0.882, which indicated that both instruments possessed good internal consistency and reliability. Convergent validity was shown by the significant correlations between the items of each section and the total mean in each part (rs=0.332–0.718; p=0.05). The study pretested result corresponds with earlier studies.46,47
Data Collection
To increase the survey’s response rate, questionnaires were sent to students beforehand and collected through face-to-face interviews. The interviewers were introduced to the questionnaire’s aim and were instructed about how to ask these questions. Before the interview, written informed consent was taken from the responders. The aims of our study were explained to the participants before written consent was obtained. Attempts were made to include male and female students from the biological sciences faculty, including Microbiology, Pharmacy, Biochemistry & Molecular Biology, Public Health and Informatics, Botany, Zoology, and other non-biological disciplines. The personal information of the respondents was made anonymous by coding.
Data Analysis
The completed questionnaire data were verified and subsequently analyzed using IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. The parameters from the knowledge, attitudes, perceptions, and practice sections were evaluated by calculating each response percentage among all the participants. In the questions relating to knowledge, correct responses to the knowledge parameters were “wrong” for Q2, and Q3 and the remaining were “right.” The levels of knowledge were further estimated using a scoring system, where a score of 1 was considered for a correct response and 0 for an incorrect or uncertain response. For quantitative analysis, an obtained score higher than 80% was considered acceptable, between 60% and 80% was considered moderate, and less than 60% was considered low.48 Questions relating to attitudes and perceptions were assessed using the three-point Likert scales with options of “agree,” “disagree,” and “uncertain.” Similar Likert scales evaluation was used to assess the study participants’ practices and habits. Response frequencies and percentages for each question were calculated to compare the KAP of biology and non-biology background students. Missing data were excluded from the bivariate analysis. Pearson’s chi-square test was used to test any association between categorical data. The univariate ordinal regression technique was used to analyze the relationship between predictors and good knowledge about antibiotics. Explanatory variables, including gender (male and female) and student category (biology and non-biology), were regressed onto the knowledge level (low, moderate, and good) as a response variable. An OR greater than 1 (or less than 1) indicated a more significant probability (or lower probability) of having higher levels of knowledge about antibiotics compared to the reference category. Finally, a multiple ordinal regression model was introduced to identify the independent effects of explanatory variables, defined by univariate analysis, on the level of knowledge about antimicrobial use and resistance. Similarly, multivariate logistic regression analysis was performed to identify the predictors of self-medication with antibiotics. Explanatory variables included gender, student category and the level of knowledge about antibiotics. 95% confidence intervals (CI) were used as OR estimates. A two-tailed p-value was calculated to check statistical significance.
Ethics Statement
The Ethics and Research Review Committee of the Faculty of Biological Sciences, Jahangirnagar University, Savar, Dhaka-1342, Bangladesh approved this study [Reference No.: BBEC, JU/M 2020 11(1) dated 01.11.2020]. Written informed consent was obtained from all the study participants for collecting their knowledge, opinion, and recent practices of antimicrobial consumption. The personal identities of the participants were strictly anonymized to protect their privacy. Author six obtained verbal permission from the chairman of the ethical committee to collect the data before ethical approval certificate was obtained. It was granted because there is human intervention the study. It is because of COVID-19 respective office was closed and it took long time to get certificate.
Results
Study Participants
Out of 396 potential respondents, 210 responded completed the questionnaires (53% response rate). Then, we excluded five questionnaires from the analyses because of incomplete data, and the final response rate became 51.77% (205⁄396). The final completed questionnaires encompass 106 collected from male respondents and 99 from female respondents. Ninety-two students studied in the different biological science faculty departments and 113 students in other non-biology disciplines. Over 90% of the students (186/205) participated in the study were undergraduate students. Current study response rates were at the same line with earlier studies.49–52
Levels of Knowledge
Most biology-background students had markedly better knowledge in the knowledge part of the questionnaire than non-biology students about antibiotics uses and antibiotic resistance. In six out of seven questions, biology students selected a higher percentage of correct answers. Very significant higher knowledge was observed in biological students in responses for three questions (No. 1, 2, and 3), and the other responses were higher but non-significant (#5, 6, and 7) (Table 1). Unlikely, in one question (No. 4), non-biology students selected more percentage of the correct answer. Many students (44.4%, 91/205) held misconceptions that antibiotics could prevent viral infections. This knowledge gap was more prevalent in non-biology students (62.8%, 71/113) than biology students (32.6%, 30/92). In knowledge level regarding antibiotic resistance, most students reported that antibiotic consumption without a physician’s prescription (91.7%, 188/205) and overuse (82.0%, 168/205) could promote antibiotic resistance emergence (Table 1).
 |
Table 1 Knowledge of Antibiotics, Their Uses, and Antibiotic Resistance in Biology-Background (n=92) and Non-Biology (n=113) University Students |
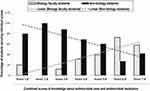
In the combined score of knowledge, a median score of 5 (IQR: 4–6) was obtained from a maximum of 7. Less than half of students had good knowledge (42.4%) and over one-third had poor knowledge (34.1%) (Table 2). This demonstrated an overall sub-standard knowledge of the uses and effects of antibiotics. The lower scores were observed in non-biology students compared to biology-background students (Figure 1). A linear downtrend was towards higher scores (1 to 7) for non-biological students; however, the reverse was noticed for biological students regarding antibiotics knowledge-scores (Figure 1).
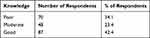 |
Table 2 Levels of Knowledge About Antibiotics, Their Uses, and Antibiotic Resistance |
In a univariate analysis, gender and student category showed a statistically significant association with higher knowledge levels about antibiotics at p ≤ 0.05 and were included in a multiple regression analysis. In a multivariate analysis, the final model was a significant improvement in fit over the null [χ2(2) = 34.026, p<0.001]. The student category was a significant predictor in the model. Biology students were more than four times as likely to have higher levels of knowledge about antibiotics than non-biology students [OR = 4.44, 95% CI (2.56, 7.70), p < 0.001]. Males were more likely to have higher levels of knowledge than females. However, gender was only marginally significant predictor in the model [OR = 1.69, 95% CI (0.99, 2.88), p = 0.052] (Table 3).
 |
Table 3 Predictors of Knowledge About Antibiotics, Their Uses, and Antibiotic Resistance Based on Multivariate Regression Analysis |
Levels of Attitudes and Beliefs
Most of the students accepted the recommendation and action plan that should be taken to prevent antibiotic resistance. Overall, about 91.7% of students believe that antibiotic resistance increases; the correct beliefs were found more in biology students than non-biology backgrounds (99.0% and 89%, respectively, p=0.019). Overall, 97.5% of students think we should be more cautious regarding the intake of antibiotics. The levels of this belief were recorded similarly in biology- and non-biology students (p=0.284). About 96.6% of students think the government should create more awareness to prevent antibiotic resistance and other 3.4% of respondents perceive the vital roles of other stakeholders than the government to generate awareness for preventing antibiotic resistance. Most of them (89.8%) agreed that antibiotics in the dairy and poultry industry should be regulated strictly. More percentage of biological students (95.6%) than non-biology students (87.5%) believed that regulation of inappropriate use of antibiotics in animal husbandry played an essential role in preventing the emergence of antibiotic resistance (Table 4). Respondents were divided into almost equal groups regarding their beliefs, whether physicians often prescribe antibiotics unnecessarily (Table 4).
 |
Table 4 Attitudes and Beliefs of Antibiotic Selections and Uses in Biology-Background (n=92) and Non-Biology (n=113) University Students |
Levels of Practices
The survey identified that 93.47% of biological students and 92% of non-biological students used to take antibiotics according to authorized physicians’ prescriptions (Table 5). Of the 205 respondents, 21 (10.2%) had self-medicated with antibiotics over the study period. The wrongdoing was found slightly higher in non-biology students (11.5%) than in biology students (8.7%, p=0.509).
 |
Table 5 Frequencies of Students Based on Their Everyday Practice of Taking Antibiotic |
To recover from the fever, 49.8% of the students reported taking antibiotics. Using antibiotics to prevent the cough and common cold was documented in 36.1% of students. Other clinical episodes for which students took antibiotics included surgery (28.3%), pustules (22.9%), urine infection (21%), ear infection (19.5%), any kind of pain (17.1%), gastroenteritis (13.7%), and for other undisclosed reasons (6.8%). However, students have reported that they often fail to complete the dose of antibiotics, and for this failure, they have provided some reasons shown in Figure 2. The most reported reason is to stop taking antibiotics when they feel better.
 |
Figure 3a Continue. |
 |
Figure 3b Questionnaire knowledge, attitude and practice about antibiotic use and antibiotic resistance among students of a public university of Bangladesh. |
About 31.7% (n=65) of the students were found to take antibiotics in the last six months, of which 77.2% of students stated they had completed the course of antibiotics. The most common antibiotics consumed are, azithromycin (n=9), ciprofloxacin (n=5), cephalosporin (n=5), flucloxacillin (n=4) and amoxicillin (n=3). Among those who took antibiotics in the last six months, 36.8% had experienced different side effects during their medication course. The most common side effects were weakness, diarrhea, vomiting, loss of appetite, allergic reaction, and dizziness. In a multivariate regression analysis, there was no significant association between self-medication and gender, student category or the level of knowledge about antibiotics (Table 6).
 |
Table 6 Predictors of Self-Medication with Antibiotics Based on Multivariate Regression Analysis |
Discussion
There is a need to tackle antibiotic resistance emergence and containment on levels ranging from individuals, households, and the communities, to health care facilities, the entire health sector, and finally to national and global levels.53
Antibiotic resistance causes around 50,000 deaths each year in Europe and the USA alone; scientists warn that antibiotics resistance can lead us to an era where antibiotics no longer will work.5 Unfortunately, not many natural or synthetic antibiotics are in the pipeline to combat pathogenic bacteria, and primary prevention is one of the best ways to lessen this problem. In this study, a total of 205 responses (68.3% response rate) were considered, of which 92 responders were from biological faculty, and 113 responders were from non-biological faculty. Less than half of the students demonstrated good knowledge regarding antibiotic resistance; however, students of biological faculty were four times [OR = 4.44, 95% CI (2.56, 7.70), p < 0.001] as likely to have better knowledge than non-biology students. The self-medication rate (10.2%) was appreciably lower, though some students also reported failure to complete the antibiotic course.
In the knowledge section, the questions were to identify students’ understanding of antibiotic resistance and the proper use of antibiotics. Less than half of the students (42.4%) showed the right knowledge level (scores higher than 80%), and about one-third of students (34.1%) indicated poor knowledge level (scores lower than 60%). In a study in Ethiopia, a substandard level of knowledge was found (54.8%) among the final year paramedical undergraduate students.45 Two studies conducted in Malaysia showed different results regarding the knowledge level of medical students. In one study, 63.3% of medical students showed a moderate level of knowledge, whereas, in another study, 68% of medical students had a high level of knowledge.54,55 One of the frequent misconceptions in the knowledge section was the effectiveness of antibiotics to treat viral diseases. Over 67.0% of biology students recognized this statement as false, while only 37.2% of non-biology students selected the correct statement. A similar misconception was documented in a study in China, where 64.52% of the medical students chose “antibiotics cannot treat a viral infection,” compared to only 43.44% of non-medical students (p < 0.0001).56 In another study in Nepal, 73.7% of medical students understood that antibiotics could not treat viral diseases, but only 34.2% of non-medical students agreed to this.57 Most students (95.7% biology, 88.5% non-biology) believed that antibiotics consumption without a physician’s prescription could cause antibiotic resistance. We found that 79.6% of non-biology students understood that overuse of antibiotics could lead to antibiotic-resistant; this rate is much higher for non-biological background students, as reported previously in Nepal.57 Comparing knowledge score with the previously conducted studies is not always appropriate as there are variations in the type of questions asked, and educational background is also disparate. The educational background seems essential in most reported data as students of biological background and medical students were found to have better knowledge. Nonetheless, researchers believe that proper knowledge is often associated with better attitude and practice.58
Students of both backgrounds showed a better attitude towards the understanding of antibiotic resistance. Most of the students (99% biology, 89.1% non-biology) believed that antibiotic resistance is increasing, and we should be more concerned regarding antibiotic consumption (99% biology, 96.4% non-biology). A similar attitude has been observed in earlier studies.59 More than 95% of students thought that the government is responsible for generating more awareness about antibiotic resistance. In a study in Iran, 41.02% of medical students believed that developing educational workshops about antibiotic administration rationale is necessary to create knowledge.43 Students were alarmed about the use of antibiotics in animal husbandry, and most of them were in favor of strict monitoring of this practice (95.6% biology, 87.5% non-biology). Indeed, this is an area of concern as numerous studies conducted in Bangladesh showed antibiotics in consumable meats, eggs, and fishes.60,61 Respondents were divided into almost equal groups regarding their beliefs, whether physicians often prescribe antibiotics unnecessarily. Previous studies reported that physicians often prescribed two or more antibiotics, frequently with the higher generation; however, no study could depict that physicians prescribe antibiotics unnecessarily.62–64
The majority of the students (93.47% biology, 92% non-biology) were found to take antibiotics only when prescribed by physicians; this practice coincides with the high level of knowledge that consuming antibiotics without a physician’s prescription can lead to antibiotic resistance. In appropriate antibiotic practice, only 8.7% of biology students and 11.5% of non-biology students tended to self-medicate; the number is lower than those reported in previous Bangladesh studies. Two previous studies conducted in Bangladesh reported self-medication of antibiotics 23.5% and 26.7, respectively, and the self-chosen antibiotics were metronidazole, azithromycin, ciprofloxacin, and amoxicillin.9,65 Compared to other countries, this lower self-medication rate is appreciative, as 70% of Indian medical students and 27% of Chinese medical students were found to self-medicate with antibiotics.36,44 A study conducted in Malaysia showed more than 89% of students accepted self-medication with antibiotics.66 In comparison to other countries, the lower self-medication rate that we found in our study is appreciative. Participants of the previously mentioned study were mainly medical students that might encourage them to self-medicate with confidence. A similar concept can be obtained from the study in Sri Lanka that indicated the rate of self-medication was higher in “pharmacology education group” students than in “non-pharmacology education group” students.67 Moreover, the students of this study have access to free medical consultation; this provision might influence them to visit the doctor before buying antibiotics by themselves. However, the suggestion of drug sellers comes next to the physician’s prescription. This is a matter of concern as drug sellers do not perceive enough knowledge regarding antibiotic resistance and its rational use. Unfortunately, antibiotics are easily available in Bangladesh in most pharmacies without prescription because of weak legislative regulations on the issue.24 Students in the study reported incomplete doses of antibiotics sometimes, especially when they feel well (48.67% biology and 36.26% non-biology). Non-compliance to prescription is common in Bangladesh; one study indicated that a substantial portion of patients stop taking antibiotics when the symptoms alleviate.68 A similar result was observed in the study conducted in Jordan, where 59.1% of students admitted that they stop taking antibiotics when they feel better.69 However, non-compliance is a widespread practice among patients, which may cause pathogens to be resistant to antibiotics. WHO always encourages antibiotic course completion, even if the patient feels well. Hence, seeking a physician’s suggestion was recommended strongly before withdrawing the medicine course when symptoms no longer persist.70 Students also reported stopping taking antibiotics when they face side effects such as gastrointestinal disturbance or allergic reaction. Adverse drug reactions (ARDs) are common with antibiotics as the medicines can disrupt the gut’s normal flora and increase the chance of infection with opportunistic pathogens such as Clostridium difficile,71 and around 1 in 15 people consuming antibiotics face allergic reaction.72
Despite rigorous screening and research, the continuous discovery of new natural and synthetic antibiotics seems scarce. Therefore, there is no alternative to increasing knowledge, perceive a better attitude, and practice accordingly. Our survey indicates that students of biological faculty have better knowledge about antibiotic application and resistance, though overall knowledge level is unsatisfactory with a chance of improvement. It is often found that educational background plays a crucial role in developing knowledge, and educational campaigns can improve antibiotic use and prescribing practice.73 There are currently 46 public universities in Bangladesh, with around 3 million students. Thus, students can play a vital role in preventing antibiotic resistance if proper knowledge can be delivered to them. Enhanced educational training is often recommended for knowledge generation. Furthermore, a better attitude is observed when people are knowledgeable about the attitude object.74 Therefore, introducing short courses or workshops for all tertiary level students can positively impact creating awareness of antibiotics’ proper use. The current study did not find any significant co-relation between self-medication and gender, student category or the level of knowledge about antimicrobials. Current study findings were similar to earlier overseas studies.75–78
Limitation of the Survey
This survey was conducted in a single public university in Bangladesh; therefore, it may not represent the overall scenario of the Bangladeshi student community. The data set is small, consisting of data of 205 respondents. The study had the intrinsic limitations of the knowledge, attitude, practice survey. Students might face recall bias when answering the questions of antibiotic consumption in the last six months. The current study is cross-sectional type of known as observational study often utilize to determine prevalence and to infer causation.79 Only describe the snap-shot of the research issue not a video picture.80 Additionally, this is a cross-sectional study with its inherent the primary limitation. The cross-sectional study design assessed both the exposure and outcome simultaneously, there is generally no evidence of a temporal relationship between exposure and outcome.81 Furthermore, the current study utilizes three point likert scale. The likert scale questionnaire had predetermined answer, thereby, if any research-respondent differs with mentioned answer that can not be determined.82,83 Moreover, likert scale only gathers numerical data which unable to offer a comprehensive representation, especially of educational portents.84
Conclusions
Students of biological backgrounds possessed better knowledge indicating the importance of curriculum in knowledge buildup. In this study, nearly half of the students of a public university in Bangladesh demonstrated the right knowledge level. Students were found to perceive a better attitude regarding antibiotic resistance and its misuse in different sectors. Although their self-medication rate was low, non-compliance to prescribed treatment was reported.
Recommendations
We recommend introducing a short course or workshop for university students of all faculties describing the importance of proper use of antibiotics, the adverse effect of improper use, and antibiotic resistance dangers. We also recommend performing more KAP-based studies in different social groups in Bangladesh to understand the overall scenario. Based on these studies, the government may create robust laws to restrain the selling and purchasing of antibiotics without an authorized physician’s prescription. Awareness should be created among the physicians and consumers of all economic classes about antibiotic resistance through mass media (TV, Radio, Newspaper), workshops, and social media where applicable. There is an urgent need for inter and intra-sectoral collaboration and cooperation among all health-related stakeholders of both national and international level-based primary health care concept to minimize the risk of antimicrobial resistance.85–89
Key Messages
- Nearly half of the university students possessed a good knowledge of antibiotic resistance.
- Students studying in departments of biological sciences perceived knowledge four times better than the students of non-biological faculty.
- The majority of students demonstrated a better attitude in the prevention of antibiotic resistance.
- Non-adherence to prescribed treatment was observed.
- Educational intervention and social awareness are necessary to improve the KAP regarding proper antibiotics use.
Acknowledgment
The authors would like to thank the study participants for their active support and all data collectors. This work was partially supported by a research grant from University Grants Commission awarded to Mahfuza Marzan. The research grant had funded the workshop, data collection cost, questionnaire administration. It did not secure any part for publication of manuscripts. The authors are grateful to Professor (Dr.) M. S. Razzaque, MBBS, Ph.D. of Lake Erie College of Osteopathic Medicine, Pennsylvania, USA, carefully read the manuscript and provided useful suggestions.
Authorship Contribution
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work. Consent for Publication: all authors reviewed and approved the final version and have agreed to be accountable for all aspects of the work, including any issues related to accuracy or integrity.
Funding
This study was partially financed by the grant of University Grants Commission Bangladesh, 2019–2020 fiscal year.
Disclosure
The authors report no conflicts of interest for this work and declare that they do not have any financial involvement or affiliations with any organization, association, or entity directly or indirectly with the subject matter or materials presented in this article. This also includes honoraria, expert testimony, employment, ownership of stocks or options, patents or grants received or pending, or royalties.
References
1. Merrett GLB, Bloom G, Wilkinson A, MacGregor H. Towards the just and sustainable use of antibiotics. J Pharm Policy Practice. 2016;9(1):1–10. doi:10.1186/s40545-016-0083-5
2. Hutchings MI, Truman AW, Wilkinson B. Antibiotics: past, present and future. Curr Opin Microbiol. 2019;51:72–80. doi:10.1016/j.mib.2019.10.008
3. Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74(3):417–433. doi:10.1128/MMBR.00016-10
4. Rossolini GM, Arena F, Pecile P, Pollini S. Update on the antibiotic resistance crisis. Curr Opin Pharmacol. 2014;18:56–60. doi:10.1016/j.coph.2014.09.006
5. Belkaid Y, Segre JA. Dialogue between skin microbiota and immunity. Science. 2014;346(6212):954–959. doi:10.1126/science.1260144
6. San Millan A. Evolution of plasmid-mediated antibiotic resistance in the clinical context. Trends Microbiol. 2018;26(12):978–985. doi:10.1016/j.tim.2018.06.007
7. Gillespie SH. Antibiotic resistance in the absence of selective pressure. Int J Antimicrob Agents. 2001;17(3):171–176. doi:10.1016/S0924-8579(00)00340-X
8. Chowdhury F, Sturm-Ramirez K, Mamun AA, et al. Effectiveness of an educational intervention to improve antibiotic dispensing practices for acute respiratory illness among drug sellers in pharmacies, a pilot study in Bangladesh. BMC Health Serv Res. 2018;18(1):676. doi:10.1186/s12913-018-3486-y
9. Biswas M, Roy MN, Manik MI, et al. Self medicated antibiotics in Bangladesh: a cross-sectional health survey conducted in the Rajshahi City. BMC Public Health. 2014;14:847. doi:10.1186/1471-2458-14-847
10. Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40(4):277–283.
11. Landers TF, Cohen B, Wittum TE, Larson EL. A review of antibiotic use in food animals: perspective, policy, and potential. Public Health Rep. 2012;127(1):4–22. doi:10.1177/003335491212700103
12. Chereau F, Opatowski L, Tourdjman M, Vong S. Risk assessment for antibiotic resistance in South East Asia. BMJ. 2017;358:j3393. doi:10.1136/bmj.j3393
13. Ahmed I, Rabbi MB, Sultana S. Antibiotic resistance in Bangladesh: A systematic review. Int j Infectious Diseases. 2019;80:54–61. doi:10.1016/j.ijid.2018.12.017
14. Arifatun Nahar MM, Siddiquee M, Nahar S, Islam K. Multidrug resistant providencia stuartii in chicken droppings: public health implications for poultry workers and associated communities in nearby dhaka metropolis, Bangladesh. British Microbiol Res J. 2016;14(5):1–9. doi:10.9734/BMRJ/2016/25883
15. Nihad Adnan MS, Islam OK, Shuvro Prokash NM, Hossain A. Characterization of ciprofloxacin resistant extended spectrum β-Lactamase (ESBL) producing Escherichia spp. from clinical waste water in Bangladesh. Adv Biosci Biotechnol. 2013;4:15–23. doi:10.4236/abb.2013.47A2003
16. Rahman M, Shoma S, Rashid H, Siddique AK, Nair GB, Sack DA. Extended-spectrum beta-lactamase-mediated third-generation cephalosporin resistance in Shigella isolates in Bangladesh. J Antimicrob Chemother. 2004;54(4):846–847. doi:10.1093/jac/dkh413
17. Chouduri AUBM, Haque MU, Arman MS, et al. Cephalosporin-3g, highly prescribed antibiotic to outpatients in rajshahi, bangladesh: prescription errors, carelessness, irrational uses are the triggering causes of antibiotic resistance. J Appl Pharm Sci. 2018;8(06):105–112.
18. Sutradhar KBSA, Huda NH, Uddin R. Irrational use of antibiotics and antibiotic resistance in southern rural Bangladesh: perspectives from both the physicians and patients. Annu Res Rev Biol. 2014;4(9):1421–1430.
19. Lucas PJ, Uddin MR, Khisa N, et al. Pathways to antibiotics in Bangladesh: A qualitative study investigating how and when households access medicine including antibiotics for humans or animals when they are ill. PLoS One. 2019;14(11):e0225270. doi:10.1371/journal.pone.0225270
20. Chowdhury M, Stewart Williams J, Wertheim H, Khan WA, Matin A, Kinsman J. Rural community perceptions of antibiotic access and understanding of antimicrobial resistance: qualitative evidence from the health and demographic surveillance system site in matlab, Bangladesh. Glob Health Action. 2019;12(sup1):1824383. doi:10.1080/16549716.2020.1824383
21. Ateshim Y, Bereket B, Major F, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health. 2019;19(1):726. doi:10.1186/s12889-019-7020-x
22. Murshid ME, Haque M. Bangladesh national drug policy 1982–2016 and recommendations in policy aspects. Eurasian J Emergency Med. 2019;18(2):104. doi:10.4274/eajem.galenos.2019.43765
23. Haque M, Haque M. Hits and misses of bangladesh national health policy 2011. J Pharmacy Bioallied Sci. 2020;12(2):83. doi:10.4103/jpbs.JPBS_236_19
24. Hoque R, Ahmed SM, Naher N, et al. Tackling antimicrobial resistance in Bangladesh: A scoping review of policy and practice in human, animal and environment sectors. PLoS One. 2020;15(1):e0227947. doi:10.1371/journal.pone.0227947
25. Nahar P, Unicomb L, Lucas PJ, et al. What contributes to inappropriate antibiotic dispensing among qualified and unqualified healthcare providers in Bangladesh? A qualitative study. BMC Health Serv Res. 2020;20(1):1–11. doi:10.1186/s12913-020-05512-y
26. Matin MA, Khan WA, Karim MM, et al. What influences antibiotic sales in rural Bangladesh? A drug dispensers’ perspective. J Pharm Policy Practice. 2020;13(1):1–12. doi:10.1186/s40545-020-00212-8
27. Saha S, Hossain MT. Evaluation of medicines dispensing pattern of private pharmacies in Rajshahi, Bangladesh. BMC Health Serv Res. 2017;17(1):136. doi:10.1186/s12913-017-2072-z
28. Ocan M, Obuku EA, Bwanga F, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health. 2015;15(1):742. doi:10.1186/s12889-015-2109-3
29. Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017;6(1):47. doi:10.1186/s13756-017-0208-x
30. Torres N, Chibi B, Middleton L, Solomon V, Mashamba-Thompson T. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. 2019;168:92–101. doi:10.1016/j.puhe.2018.11.018
31. Rather IA, Kim B-C, Bajpai VK, Park Y-H. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi j Biol Sci. 2017;24(4):808–812. doi:10.1016/j.sjbs.2017.01.004
32. Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi:10.1016/S1473-3099(13)70318-9
33. Sakeena M, Bennett AA, McLachlan AJ. Non-prescription sales of antimicrobial agents at community pharmacies in developing countries: a systematic review. Int J Antimicrob Agents. 2018;52(6):771–782. doi:10.1016/j.ijantimicag.2018.09.022
34. Chen J, Sidibi AM, Shen X. et al. Lack of antibiotic knowledge and misuse of antibiotics by medical students in Mali: A cross-sectional study. Expert Rev Anti Infect Ther;2020. 1–8. doi: 10.1080/14787210.2021.1857731
35. Higuita-Gutiérrez LF, Villamil GER, Quiceno JNJ. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: a cross-sectional descriptive study. BMC Public Health. 2020;20(1):1–12. doi:10.1186/s12889-020-09971-0
36. Hu Y, Wang X, Tucker JD, et al. Knowledge, attitude, and practice with respect to antibiotic use among chinese medical students: a multicentre cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1165. doi:10.3390/ijerph15061165
37. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. 2019;12:1333.
38. Niwandinda F, Lukyamuzi EJ, Ainebyona C, Ssebunya VN, Murungi G, Atukunda EC. Patterns and practices of self-medication among students enrolled at Mbarara University of Science and Technology in Uganda. Integrated Pharmacy Res Practice. 2020;9:41. doi:10.2147/IPRP.S237940
39. Mason T, Trochez C, Thomas R, Babar M, Hesso I, Kayyali R. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health. 2018;18(1):711. doi:10.1186/s12889-018-5614-3
40. Abdel-Qader DH, Albassam A, Ismael NS, et al. Awareness of antibiotic use and resistance in Jordanian Community. J Prim Care Community Health. 2020;11:2150132720961255. doi:10.1177/2150132720961255
41. Mazińska B, Strużycka I, Hryniewicz W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: did the European antibiotic awareness day campaigns change attitudes? PLoS One. 2017;12(2):e0172146. doi:10.1371/journal.pone.0172146
42. World Health Organization. Antibiotic resistance; 2020. Available from https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.
43. Abdolghafour Jorak FK, Saeidinia A, Heidarzadeh A, Saeidinia F. A cross sectional study on knowledge, attitude and practice of medical students toward antibiotic resistance and its prescription, Iran. Adv Environmental Biol. 2014;8(17):675–681.
44. Mosmi Lomi VKJ, Srinivasan SV, Jonathan Daniel M. Assessment of knowledge, attitude and practice of antibiotic usage amongst undergraduate, intern and postgraduate dental students - a questionnaire based study. Int J Sci Healthcare Res. 2019;4:2.
45. Seid MA, Hussen MS. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect Dis. 2018;18(1):312. doi:10.1186/s12879-018-3199-1
46. Nunnally JC. Psychometric Theory 3E. Tata McGraw-hill education; 1994.
47. Barman MP, Hazarika J, Kalita A. Reliability and validity of Assamese version of EORTC QLQ-C30 questionnaire for studying the quality of life of cancer patients of Assam. World Appl Sci J. 2012;17(5):672–678.
48. Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Social Administrative Pharmacy. 2008;4(2):164–172. doi:10.1016/j.sapharm.2007.04.004
49. Fincham JE. Response rates and responsiveness for surveys, standards, and the Journal. Am J Pharm Educ. 2008;72:2. doi:10.5688/aj720243
50. Harrison S, Henderson J, Alderdice F, Quigley MA. Methods to increase response rates to a population-based maternity survey: a comparison of two pilot studies. BMC Med Res Methodol. 2019;19(1):65. doi:10.1186/s12874-019-0702-3
51. Weaver L, Beebe TJ, Rockwood T. The impact of survey mode on the response rate in a survey of the factors that influence Minnesota physicians’ disclosure practices. BMC Med Res Methodol. 2019;19(1):73. doi:10.1186/s12874-019-0719-7
52. Beebe TJ, Locke III GR, Barnes SA, Davern ME, Anderson KJ. Mixing web and mail methods in a survey of physicians. Health Serv Res. 2007;42(3p1):1219–1234. doi:10.1111/j.1475-6773.2006.00652.x
53. Tomson G, Vlad I. The need to look at antibiotic resistance from a health systems perspective. Ups J Med Sci. 2014;119(2):117–124. doi:10.3109/03009734.2014.902879
54. Haque M, Rahman NAA, McKimm J, et al. A cross-sectional study evaluating the knowledge and beliefs about, and the use of antibiotics amongst Malaysian university students. Expert Rev Anti Infect Ther. 2019;17(4):275–284. doi:10.1080/14787210.2019.1581607
55. Haque M, Rahman NAA, McKimm J, et al. Antibiotic use: a cross-sectional study evaluating the understanding, usage and perspectives of medical students and pathfinders of a public defence University in Malaysia. Antibiotics. 2019;8(3). doi:10.3390/antibiotics8030154.
56. Huang Y, Gu J, Zhang M, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13:163. doi:10.1186/1472-6920-13-163
57. Shah P, Shrestha R, Mao Z, et al. Knowledge, attitude, and practice associated with antibiotic use among university students: a survey in Nepal. Int J Environ Res Public Health. 2019;16:20. doi:10.3390/ijerph16203996
58. Khalili H, Mohebbi N, Hendoiee N, Keshtkar AA, Dashti-Khavidaki S. Improvement of knowledge, attitude and perception of healthcare workers about ADR, a pre- and post-clinical pharmacists’ interventional study. BMJ Open. 2012;2:e000367. doi:10.1136/bmjopen-2011-000367
59. Thriemer K, Katuala Y, Batoko B, et al. Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS One. 2013;8(2):e55495. doi:10.1371/journal.pone.0055495
60. Islam ASA, Al Faruq A, Islam S, et al. Antimicrobial residues in tissues and eggs of laying hens at Chittagong, Bangladesh. Int J One Health. 2016;2(11):75–80. doi:10.14202/IJOH.2016.75-80
61. Sattar SHM, Islam S, Alam M, et al. Antibiotic residues in broiler and layer meat in Chittagong district of Bangladesh. Veterinary World. 2014;7:9. doi:10.14202/vetworld.2014.738-743
62. Fahad BMA, Shill M, Asish K. Antibiotic usage at a primary health care unit in Bangladesh. Australasian Med J. 2010;3(7):414. doi:10.4066/AMJ.2010.32
63. Sayeed MAIN, Ali MS, Rahman MM, Islam MR, Jakaria M. Survey on antibiotic practices in chittagong city of Bangladesh. Bangladesh Pharmaceutical J. 2015;18(2):174–178. doi:10.3329/bpj.v18i2.24318
64. Abdulrahman JA, Saleh A-HS JM. Antibiotics dispensing between legal idealism and implementation: closing the implementation gap between local regulation and practice. Res Social Administrative Pharmacy. 2020;16:1328–1329. doi:10.1016/j.sapharm.2020.05.001
65. Md. Uzzal HAK, Barik SMA, Islam MAU. Prevalence, practice and irrationality of self-medicated antibiotics among people in Northern and Southern Region of Bangladesh. Int J Res Pharm Biosci. 2017;4(10):17–24.
66. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. 2019;12:1333–1351.
67. Rathish D, Wijerathne B, Bandara S, et al. Pharmacology education and antibiotic self-medication among medical students: a cross-sectional study. BMC Res Notes. 2017;10(1):337. doi:10.1186/s13104-017-2688-4
68. Sutradhar KB, Saha A, Huda NH, Uddin R. Irrational use of antibiotics and antibiotic resistance in southern rural Bangladesh: perspectives from both the physicians and patients. Annual Res Rev Biol. 2014;4:1421–1430.
69. Ghadeer ARY, Suaifan MS, Darwish DA, Al-Ijel H, Darwish A-M. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. African J Pharm Pharmacol. 2012;6(10):763–770.
70. Langford BJ, Morris AM. Is it time to stop counselling patients to “finish the course of antibiotics”?. Canadian pharmacists J. 2017;150(6):349–350.
71. Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4554–4561. doi:10.1073/pnas.1000087107
72. Blumenthal KG, Peter JG, Trubiano JA, Phillips EJ. Antibiotic allergy. Lancet. 2019;393(10167):183–198.
73. Kandeel A, Palms DL, Afifi S, et al. An educational intervention to promote appropriate antibiotic use for acute respiratory infections in a district in Egypt- pilot study. BMC Public Health. 2019;19(Suppl 3):498. doi:10.1186/s12889-019-6779-0
74. Holbrook AL, Berent MK, Krosnick JA, Visser PS, Boninger DS. Attitude importance and the accumulation of attitude-relevant knowledge in memory. J Pers Soc Psychol. 2005;88(5):749–769. doi:10.1037/0022-3514.88.5.749
75. Gyawali S, Shankar PR, Poudel PP, Saha A. Knowledge, attitude and practice of self-medication among basic science undergraduate medical students in a medical school in western Nepal. J Clin Diagnostic Res. 2015;9(12):FC17. doi:10.7860/JCDR/2015/16553.6988
76. Alex IO. Knowledge of antibiotic use and resistance among students of a medical school in Nigeria. Malawi Med J. 2019;31(2):133–137. doi:10.4314/mmj.v31i2.5
77. Elong Ekambi G-A, Okalla Ebongue C, Penda IC, Nnanga Nga E, Mpondo Mpondo E, Eboumbou Moukoko CE. Knowledge, practices and attitudes on antibiotics use in Cameroon: self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS One. 2019;14(2):e0212875. doi:10.1371/journal.pone.0212875
78. Jairoun A, Hassan N, Ali A, Jairoun O, Shahwan M. Knowledge, attitude and practice of antibiotic use among university students: a cross sectional study in UAE. BMC Public Health. 2019;19(1):518. doi:10.1186/s12889-019-6878-y
79. Mann C. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emergency Med j. 2003;20(1):54–60. doi:10.1136/emj.20.1.54
80. Setia MS. Methodology series module 3: cross-sectional studies. Indian J Dermatol. 2016;61(3):261. doi:10.4103/0019-5154.182410
81. Carlson MD, Morrison RS. Study design, precision, and validity in observational studies. J Palliat Med. 2009;12(1):77–82. doi:10.1089/jpm.2008.9690
82. Voutilainen A, Pitkäaho T, Kvist T, Vehviläinen‐Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72(4):946–957. doi:10.1111/jan.12875
83. Kuhlmann T, Dantlgraber M, Reips U-D. Investigating measurement equivalence of visual analogue scales and Likert-type scales in Internet-based personality questionnaires. Behav Res Methods. 2017;49(6):2173–2181. doi:10.3758/s13428-016-0850-x
84. Nemoto T, Beglar D (2014). Developing Likert-scale questionnaires. In Sonda N, Krause A (Eds.),
85. Bordier M, Binot A, Pauchard Q, et al. Antibiotic resistance in Vietnam: moving towards a One Health surveillance system. BMC Public Health. 2018;18(1):1136. doi:10.1186/s12889-018-6022-4
86. Razzaque MS. Exacerbation of antimicrobial resistance: another casualty of the covid-19 pandemic? Expert Rev Anti Infect Ther. 2020;1–5. doi:10.1080/14787210.2021.1865802
87. Dhingra S, Rahman NAA, Peile E, et al. Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Front Public Health. 2020;8:8. doi:10.3389/fpubh.2020.535668
88. van Dale D, Lemmens L, Hendriksen M, et al. Recommendations for effective intersectoral collaboration in health promotion interventions: results from joint action CHRODIS-PLUS work package 5 activities. Int J Environ Res Public Health. 2020;17(18):6474. doi:10.3390/ijerph17186474
89. Haque M, Islam T, Rahman NAA, McKimm J, Abdullah A, Dhingra S. Strengthening primary health-care services to help prevent and control long-term (chronic) non-communicable diseases in low-and middle-income countries. Risk Manag Healthc Policy. 2020;13:409–426. doi:10.2147/RMHP.S239074
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.